Professional Documents
Culture Documents
Treatment of Acute Otitis Media in Children
Uploaded by
Ramza Shiddiq As'AryCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Treatment of Acute Otitis Media in Children
Uploaded by
Ramza Shiddiq As'AryCopyright:
Available Formats
new england
The
journal of medicine
established in 1812 january 13, 2011 vol. 364 no. 2
Treatment of Acute Otitis Media in Children
under 2 Years of Age
Alejandro Hoberman, M.D., Jack L. Paradise, M.D., Howard E. Rockette, Ph.D., Nader Shaikh, M.D., M.P.H.,
Ellen R. Wald, M.D., Diana H. Kearney, R.N., C.C.R.C., D. Kathleen Colborn, B.S., Marcia Kurs-Lasky, M.S.,
Sonika Bhatnagar, M.D., M.P.H., Mary Ann Haralam, C.R.N.P., Lisa M. Zoffel, C.R.N.P., Carly Jenkins, R.N.,
Marcia A. Pope, R.N., Tracy L. Balentine, R.N., and Karen A. Barbadora, M.T.
A BS T R AC T
Background
Recommendations vary regarding immediate antimicrobial treatment versus watch- From the Department of Pediatrics, Uni-
ful waiting for children younger than 2 years of age with acute otitis media. versity of Pittsburgh School of Medicine,
Childrens Hospital of Pittsburgh of the
University of Pittsburgh Medical Center
Methods (A.H., J.L.P., N.S., E.R.W., D.H.K., D.K.C.,
We randomly assigned 291 children 6 to 23 months of age, with acute otitis media S.B., M.A.H., L.M.Z., C.J., M.A.P., T.L.B.,
diagnosed with the use of stringent criteria, to receive amoxicillinclavulanate or K.A.B.), and the Department of Biostatis-
tics, Graduate School of Public Health,
placebo for 10 days. We measured symptomatic response and rates of clinical failure. University of Pittsburgh (H.E.R., M.K.-L.)
both in Pittsburgh. Address reprint re-
Results quests to Dr. Hoberman at the Division
of General Academic Pediatrics, Chil-
Among the children who received amoxicillinclavulanate, 35% had initial resolu- drens Hospital of Pittsburgh of UPMC,
tion of symptoms by day 2, 61% by day 4, and 80% by day 7; among children who Childrens Hospital Office Bldg., 3rd Fl.,
received placebo, 28% had initial resolution of symptoms by day 2, 54% by day 4, and 4401 Penn Ave., Pittsburgh, PA 15224, or
at hoberman@chp.edu.
74% by day 7 (P=0.14 for the overall comparison). For sustained resolution of symp-
toms, the corresponding values were 20%, 41%, and 67% with amoxicillinclavula- N Engl J Med 2011;364:105-15.
nate, as compared with 14%, 36%, and 53% with placebo (P=0.04 for the overall Copyright 2011 Massachusetts Medical Society.
comparison). Mean symptom scores over the first 7 days were lower for the children
treated with amoxicillinclavulanate than for those who received placebo (P=0.02).
The rate of clinical failure defined as the persistence of signs of acute infection
on otoscopic examination was also lower among the children treated with
amoxicillinclavulanate than among those who received placebo: 4% versus 23% at
or before the visit on day 4 or 5 (P<0.001) and 16% versus 51% at or before the visit on
day 10 to 12 (P<0.001). Mastoiditis developed in one child who received placebo. Diar-
rhea and diaper-area dermatitis were more common among children who received
amoxicillinclavulanate. There were no significant changes in either group in the
rates of nasopharyngeal colonization with nonsusceptible Streptococcus pneumoniae.
Conclusions
Among children 6 to 23 months of age with acute otitis media, treatment with amoxi-
cillinclavulanate for 10 days tended to reduce the time to resolution of symptoms
and reduced the overall symptom burden and the rate of persistent signs of acute
infection on otoscopic examination. (Funded by the National Institute of Allergy and
Infectious Diseases; ClinicalTrials.gov number, NCT00377260.)
n engl j med 364;2 nejm.org january 13, 2011 105
The New England Journal of Medicine
Downloaded from nejm.org by Ramza As'Ary on January 31, 2017. For personal use only. No other uses without permission.
Copyright 2011 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
A
cute otitis media is the most fre- most effective treatment for acute otitis media, we
quently diagnosed illness in children in the chose it as the active treatment in our study.7,10
United States1 and the most commonly cit-
ed indication for antimicrobial therapy in chil- Me thods
dren2; in the United States, most children with
acute otitis media have routinely been treated Eligibility and Enrollment
Comment on with antimicrobial drugs. However, a watchful- We conducted this trial between November 2006
this article at waiting strategy, in which treatment is reserved and March 2009 at the Childrens Hospital of Pitts-
NEJM.org for children whose condition does not improve burgh and Armstrong Pediatrics, an affiliated pri-
without medication, has long been applied in sev- vate practice in Kittanning, Pennsylvania. The study
eral European countries in the interest of mini- protocol was approved by the institutional review
mizing the use of antimicrobial drugs.3 In the board at the University of Pittsburgh; written in-
Netherlands and Scotland, that strategy has been formed consent was obtained from a parent of
recommended officially for children as young as each enrolled child. The protocol, including the
6 months of age.4,5 In 2004, a clinical practice statistical analysis plan, is available with the full
guideline issued by the American Academy of text of this article at NEJM.org. The authors at-
Pediatrics and the American Academy of Family test that the study was performed in accordance
Physicians endorsed watchful waiting as an op- with the protocol and the statistical analysis plan.
tion for children 6 to 23 months of age in whom To be eligible for enrollment in the study, chil-
illness is nonsevere (defined, in an adaptation dren were required to have received at least two
of an earlier definition,6 by the presence of mild doses of pneumococcal conjugate vaccine and to
otalgia and a temperature of less than 39C dur- have acute otitis media that was diagnosed on the
ing the preceding 24 hours) and in whom the basis of three criteria: the onset, within the pre-
diagnosis of acute otitis media is uncertain.7 A ceding 48 hours, of symptoms that parents rated
similar recommendation, but without reference with a score of at least 3 on the Acute Otitis
to diagnostic certainty, was issued recently by Media Severity of Symptoms (AOM-SOS) scale11,12
the Infectious Diseases and Immunization Com- (on which scores range from 0 to 14, with higher
mittee of the Canadian Paediatric Society.8 scores indicating greater severity of symptoms),
The adoption of a strategy of watchful waiting the presence of middle-ear effusion, and moder-
has been based on the results of clinical trials3 ate or marked bulging of the tympanic mem-
that showed relatively high rates of spontaneous brane or slight bulging accompanied by either
improvement in children with acute otitis media. otalgia or marked erythema of the membrane.
However, in those trials, as in earlier trials in- The AOM-SOS scale consists of seven discrete
volving children with otitis media, there were items: tugging of ears, crying, irritability, diffi-
substantial limitations most notably, the lack culty sleeping, diminished activity, diminished
of stringent diagnostic criteria, the inclusion of appetite, and fever. Parents are asked to rate
few very young children, and the use of an anti- these symptoms, in comparison with the childs
microbial drug that had limited efficacy or that usual state, as none, a little, or a lot, with
was administered in suboptimal doses.9 Moreover, corresponding scores of 0, 1, and 2 (see Fig. 1 in
rates of spontaneous improvement similar to the the Supplementary Appendix, available at NEJM
rates seen in those studies among children re- .org). Children were excluded if they had an-
ceiving placebo have not been found uniformly.6 other acute illness (e.g., pneumonia) or a chron-
Therefore, for children with acute otitis media, the ic illness (e.g., cystic fibrosis), were allergic to
circumstances in which immediate antimicrobial amoxicillin, had received more than one dose of
treatment is the preferred strategy have remained an antimicrobial drug within the previous 96
unclear. We undertook this clinical trial to de- hours, had had otalgia for longer than 48 hours,
termine the extent to which antimicrobial treat- or had perforation of the tympanic membrane.
ment affects the course of both symptoms and
signs of acute otitis media, irrespective of the Randomization
apparent severity of the disease, among children We stratified children according to whether they
6 to 23 months of age in whom the diagnosis of had a history of recurrent acute otitis media (de-
acute otitis media is quite certain. Because amox- fined as three or more episodes in the preceding
icillinclavulanate has been shown to be the 6 months or four or more episodes over the course
106 n engl j med 364;2 nejm.org january 13, 2011
The New England Journal of Medicine
Downloaded from nejm.org by Ramza As'Ary on January 31, 2017. For personal use only. No other uses without permission.
Copyright 2011 Massachusetts Medical Society. All rights reserved.
Treatment of Acute Otitis Media in Young Children
of 12 months) and according to their exposure or visit, we categorized the children as having met
nonexposure to three or more children for at least the criteria for either clinical success or clinical
10 hours per week. At each study site, within each failure. We defined clinical failure at or before the
stratum, we randomly assigned children in blocks day 45 visit as either a lack of substantial im-
of four, in a 1:1 ratio, to receive a 10-day course provement in symptoms, a worsening of signs on
of either amoxicillinclavulanate (Augmentin ES, otoscopic examination, or both, and clinical fail-
GlaxoSmithKline), at a daily dose of 90 mg of ure at the day 1012 visit as the failure to achieve
amoxicillin per kilogram of body weight com- complete or nearly complete resolution of symp-
bined with 6.4 mg of clavulanate per kilogram, toms and of otoscopic signs, without regard to the
or placebo; each study drug was administered in persistence or resolution of middle-ear effusion.
two doses per day. The placebo was prepared by We treated children who met the criteria for clin-
the research pharmacy at the Childrens Hospital ical failure with a standardized 10-day regimen of
of Pittsburgh according to the formula for pla- orally administered amoxicillin, at a dose of 90 mg
cebo specified in the application to the Food and per kilogram per day, and cefixime, at a dose of
Drug Administration for the labeling information 8 mg per kilogram per day. Once a child had met
for Augmentin ES and was similar to that prod- the criteria for clinical failure, he or she remained
uct in appearance and taste. The parents, the re- in that category for the analyses. At the day 2125
search personnel, and the health care providers visit, the reappearance of acute otitis media in a
who were not associated with the study remained child who had previously been categorized as hav-
unaware of the childrens group assignments ing met the criteria for clinical success was consid-
throughout the study. Parents were advised to ad- ered to be a relapse. When feasible, we obtained
minister acetaminophen as needed for the relief nasopharyngeal specimens from the children for
of symptoms. culturing, at study entry and at the day 1012 and
day 2125 visits.
Assessment of Symptoms
We assessed symptoms with the use of a struc- Outcomes
tured interview of one of the childs parents; as- All outcome measures were prespecified. The pri-
sessments were performed by telephone every day mary outcome measures were the time to resolu-
until the first follow-up visit and in person at each tion of symptoms and the symptom burden over
visit. We also asked the parents about loss of time time. The time to resolution of symptoms was
at work or the need for alternative day-care ar- measured in two ways: the time to the first re-
rangements because of the childs illness. Parents cording of an AOM-SOS score of 0 or 1 and the
were asked to record their childs AOM-SOS scores time to the second of two successive recordings
and other pertinent clinical information in a diary of that score. The symptom burden over time was
twice a day for 3 days and once a day thereafter. measured by calculating the mean AOM-SOS score
in the two groups each day over the first 7 days
Otoscopic Examination, Overall Assessment, of follow-up and the groups weighted mean scores
and Management for that period. The secondary outcomes were
All the study clinicians were otoscopists who had overall clinical efficacy, the use of acetaminophen,
successfully completed an otoscopic validation the occurrence of adverse events, nasopharyngeal
program,13 and their findings on otoscopic exami- colonization rates, and the use of health care re-
nation determined the diagnoses for the study; sources.
whenever possible, however, we also obtained oto-
endoscopic photographs of the childrens tym- Statistical Analysis
panic membranes (see Fig. 2, 3, and 4 in the We estimated that with a sample of 120 children
Supplementary Appendix). The children received who could be evaluated in each study group, the
the study drug on day 1; thereafter, we assessed study would have 80% power to detect a 66% low-
them during the course of therapy, usually on day er rate of resolution of symptoms in the placebo
4 or 5; at the end of therapy, usually on day 10 to group as compared with the amoxicillinclavula-
12; and at a follow-up visit, usually on day 21 to nate group. All the analyses were based on the
25. Hereinafter, we use those days to designate intention-to-treat principle, were performed with
the three types of visit, irrespective of individual the use of two-sided tests, and included adjust-
variations in the actual days of the visits. At each ment for the study stratification variables. We com-
n engl j med 364;2 nejm.org january 13, 2011 107
The New England Journal of Medicine
Downloaded from nejm.org by Ramza As'Ary on January 31, 2017. For personal use only. No other uses without permission.
Copyright 2011 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
pared the time to the resolution of symptoms be- 54%, and 74% (P=0.14 for the overall compari-
tween the study groups using life-table plots, and son). The resolution of symptoms as defined by
we conducted tests of equal hazard functions us- two successive recordings of an AOM-SOS score
ing a proportional-hazards model. We compared of 0 or 1 occurred by day 2 in 20% of the children
the mean AOM-SOS scores in the two groups at who were treated with amoxicillinclavulanate,
individual assessments each day over the first by day 4 in 41%, and by day 7 in 67%; the corre-
7 days of follow-up using generalized estimating sponding values for children who received placebo
equations, and the groups weighted mean scores were 14%, 36%, and 53% (P=0.04 for the overall
for that period (taking into account that observa- comparison).
tions were made twice daily during the first 3 days The mean AOM-SOS scores in the two treat-
of follow-up) using regression analysis. For analy ment groups over the first 7 days (Fig. 2C) were
ses of clinical success or failure, we used logistic lower in the amoxicillinclavulanate group than
regression. To determine whether variables were in the placebo group at each time point (P=0.02)
prognostic or effect modifiers, we used the pro- and at the 1012 day visit (1.590.21 vs. 2.460.20;
portional-hazards model or logistic-regression difference, 0.87; 95% confidence interval [CI],
models, as appropriate. We used McNemars test 0.29 to 1.45; P=0.003). The 7-day weighted mean
for analyses of nasopharyngeal colonization rates. (SE) score was also significantly lower in the
amoxicillinclavulanate group than in the pla-
R e sult s cebo group (2.790.16 vs. 3.420.18; difference,
0.63; 95% CI, 0.15 to 1.10; P=0.01). The degree
Study Population of difference between the two treatment groups
A total of 1385 children were screened; 498 of the varied according to the severity of the childrens
children were eligible for the clinical trial and symptoms at trial entry; among children whose
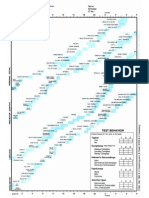
291 were enrolled (Fig. 1). Selected demographic initial AOM-SOS score was 8 or less, the scores
and clinical characteristics of the children are were 2.210.16 vs. 2.580.19 (difference, 0.37;
shown in Table 1. There were no significant dif- 95% CI, 0.13 to 0.87; P=0.14), and among chil-
ferences between enrolled children and children dren whose initial score was higher than 8, the
whose parents withheld consent or between the values were 3.590.27 vs. 4.500.28 (difference,
children in the two study groups. We found no 0.91; 95% CI, 0.13 to 1.68; P=0.02).
significant correlation between childrens AOM-
SOS scores at entry and the degree of bulging of Clinical Failure
their affected tympanic membranes. A total of 96% Children who received amoxicillinclavulanate
of the children completed all scheduled study vis- were less likely than children receiving placebo
its, and 85% reportedly received all scheduled med- to have evidence of clinical failure at or before
ication doses during days 1 through 3 and at least the day 45 visit (4% vs. 23%; difference, 19%;
80% of doses overall. 95% CI, 12 to 27; P<0.001) and at or before the
day 1012 visit (16% vs. 51%; difference, 35%;
Efficacy of Treatment 95% CI, 25 to 45; P<0.001). In the two groups
Symptomatic Response combined, AOM-SOS scores at the time of clini-
The childrens symptomatic response during the cal failure were 2 or higher in 33 of 39 children
first 7 days of follow-up is summarized in Figure 2. (85%) who met the criteria for clinical failure at or
The time to resolution of symptoms is shown ac- before the day 45 visit and in 60 of 95 children
cording to two criteria: the time to the first re- (63%) who met the criteria for clinical failure at or
cording of an AOM-SOS score of 0 or 1 (Fig. 2A) before the day 1012 visit; the proportions did not
and the time to the second of two successive re- differ significantly between the two study groups.
cordings of that score (Fig. 2B). (In 54% of the The mean (SD) scores at the day 45 visit were
instances in which scores fell to 0 or 1, a subse- 5.03.2 among children who met the criteria for
quent score was higher than 1.) Among the chil- clinical failure at that visit and 2.22.3 among
dren who were treated with amoxicillinclavula- children who did not meet the criteria for clinical
nate, the initial resolution of symptoms occurred failure at that visit; the corresponding values at
by day 2 in 35% of the children, by day 4 in 61%, the day 1012 visit were 3.73.3 and 1.21.8. No
and by day 7 in 80%; the corresponding values child was categorized as having met the criteria for
among children who received placebo were 28%, clinical failure on the basis of symptoms alone.
108 n engl j med 364;2 nejm.org january 13, 2011
The New England Journal of Medicine
Downloaded from nejm.org by Ramza As'Ary on January 31, 2017. For personal use only. No other uses without permission.
Copyright 2011 Massachusetts Medical Society. All rights reserved.
Treatment of Acute Otitis Media in Young Children
1385 Children were assessed for eligibility
887 Were not eligible
397 Did not have acute otitis media
138 Had AOM-SOS score <3
28 Had onset of illness >48 hr earlier
57 Had otorrhea or tympanostomy tubes
267 Met other exclusion criteria
125 Did not have available parent, were
not examined, or could not be
followed up
86 Were prescribed or received anti-
biotic or had other acute or chronic
illness
28 Had inadequate immunization with
pneumococcal conjugate vaccine
28 Had a history of penicillin allergy
498 Were eligible
207 Had parent who declined participation
291 Underwent randomization
144 Were assigned to and received
147 Were assigned to and received placebo
amoxicillinclavulanate
1 Had parent who withdrew consent 1 Had parent who withdrew consent
139 Were assessed at or near day 45 142 Were assessed at or near day 45
(during therapy) (during therapy)
140 Were assessed at or near day 1012 141 Were assessed at or near day 1012
(end of therapy) (end of therapy)
141 Were assessed at or near day 2125 139 Were assessed at or near day 2125
(follow-up) (follow-up)
7 Discontinued intervention 2 Discontinued intervention
1 Had a rash 1 Had urticaria
6 Had protocol-defined diarrhea 1 Had protocol-defined diarrhea
144 Were included in analysis 147 Were included in analysis
Figure 1. Enrollment, Randomization, and Follow-up of Children in the Study.
Mean scores on the Acute Otitis Media Severity of Symptoms (AOM-SOS) scale range from 0 to 14, with higher
scores indicating greater severity of symptoms.
Prognostic Factors and Effect Modifiers per week than among children who were not
At day 10 to 12, the clinical results were less (P=0.007), among children with higher AOM-
favorable among children who were exposed SOS scores at entry than among those with lower
to three or more children for at least 10 hours scores (P=0.004), among children with bilateral
n engl j med 364;2 nejm.org january 13, 2011 109
The New England Journal of Medicine
Downloaded from nejm.org by Ramza As'Ary on January 31, 2017. For personal use only. No other uses without permission.
Copyright 2011 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
Table 1. Selected Demographic and Clinical Characteristics, According to Study Group.*
AmoxicillinClavulanate Placebo Group All Children
Characteristic Group (N=144) (N=147) (N=291)
Age at entry no. (%)
611 mo 83 (58) 78 (53) 161 (55)
1217 mo 35 (24) 42 (29) 77 (26)
1823 mo 26 (18) 27 (18) 53 (18)
Sex no. (%)
Male 75 (52) 80 (54) 155 (53)
Female 69 (48) 67 (46) 136 (47)
Race no. (%)
White 66 (46) 65 (44) 131 (45)
Black 62 (43) 58 (39) 120 (41)
Other 16 (11) 24 (16) 40 (14)
Maternal level of education no./total no. (%)
Less than high school 24/144 (17) 16/146 (11) 40/290 (14)
High-school graduate 90/144 (62) 95/146 (65) 185/290 (64)
College graduate 30/144 (21) 35/146 (24) 65/290 (22)
Type of health insurance no./total no. (%)
Private 43/141 (30) 42/145 (29) 85/286 (30)
Medicaid 98/141 (70) 103/145 (71) 201/286 (70)
Exposure to other children no. (%)
Yes 69 (48) 72 (49) 141 (48)
No 75 (52) 75 (51) 150 (52)
AOM-SOS score
Baseline score no. (%)
35 37 (26) 33 (22) 70 (24)
68 46 (32) 51 (35) 97 (33)
911 46 (32) 44 (30) 90 (31)
1214 15 (10) 19 (13) 34 (12)
Mean baseline score 7.692.85 7.902.87 7.802.86
Laterality of acute otitis media no. (%)
Bilateral 75 (52) 77 (52) 152 (52)
Unilateral 69 (48) 70 (48) 139 (48)
Degree of tympanic membrane bulging in worse ear
no. (%)
Slight 42 (29) 39 (27) 81 (28)
Moderate 63 (44) 70 (48) 133 (46)
Marked 39 (27) 38 (26) 77 (26)
* There were no significant differences in characteristics between the two study groups.
Race was reported by the parents.
Exposure to other children was defined as exposure to at least three children for at least 10 hours per week.
The Acute Otitis Media Severity of Symptoms (AOM-SOS) scale measures seven discrete items: tugging of ears, crying,
irritability, difficulty sleeping, diminished activity, diminished appetite, and fever. Parents are asked to rate these symp-
toms, in comparison with the childs usual state, as none, a little, or a lot, with corresponding scores of 0, 1, and
2. Thus, total scores range from 0 to 14, with higher scores indicating greater severity of symptoms.
110 n engl j med 364;2 nejm.org january 13, 2011
The New England Journal of Medicine
Downloaded from nejm.org by Ramza As'Ary on January 31, 2017. For personal use only. No other uses without permission.
Copyright 2011 Massachusetts Medical Society. All rights reserved.
Treatment of Acute Otitis Media in Young Children
Figure 2. Resolution of Childrens Symptoms A First Recording of AOM-SOS Score of 0 or 1
during the First 7 Days of Follow-up.
100
Children with Continuing Symptoms (%)
During the first 3 days, the Acute Otitis Media Severity
90
of Symptoms (AOM-SOS) scale11,12 was administered
twice daily; thereafter, it was administered once daily. 80
Panels A and B show the proportion of children in 70
whom symptoms had not resolved. Resolution of
60
symptoms is defined in Panel A as the first recording
of an AOM-SOS score of 0 or 1 and in Panel B as the 50
second of two successive recordings of a score of 0 or 1. 40 Placebo group
Panel C shows the mean scores on the AOM-SOS scale 30 Amoxicillinclavulanate group
over the course of the first 7 days of the study treat-
20
ment. Since multiple assessments were made on the
first 3 study days, numbers on the x axis in all three 10 P=0.14
panels indicate the end of a study day. 0
1 2 3 4 5 6 7
Study Day
acute otitis media than among children with uni-
lateral acute otitis media (P=0.002), and among B Second Recording of AOM-SOS Score of 0 or 1
children with more bulging of the tympanic mem- 100
Children with Continuing Symptoms (%)
brane than among children with less bulging 90
(P<0.001) (Table 2; and see Table 2 in the Supple- 80
mentary Appendix for the multiple logistic-regres- 70
sion analysis). Among children in the trial whose 60 Placebo group
illness would have been considered severe (as in- 50
Amoxicillinclavulanate group
dicated by moderate or severe otalgia or a body 40
temperature of more than 39C during the pre- 30
ceding 24 hours), the rates of clinical failure at 20
or before the day 1012 visit were 19% (12 of 63 10 P=0.04
children) among those receiving amoxicillinclav
0
ulanate and 61% (40 of 66) among those receiv- 1 2 3 4 5 6 7
ing placebo. Corresponding rates among children Study Day
whose illness would have been considered nonse-
vere were 14% (11 of 79) and 43% (33 of 77). C Mean AOM-SOS Score
Among the 17 interactions that we tested between 8
a demographic or clinical variable and the assigned 7
study treatment, one was significant: children 18
6
Mean AOM-SOS Score
to 23 months of age who received amoxicillin
clavulanate had a higher rate of clinical failure 5
than did children 12 to 17 months of age and 4
children 6 to 11 months of age (38% vs. 12% and
3
11%, respectively) (see Table 1 in the Supplemen- Placebo group
tary Appendix for additional details). 2
Amoxicillinclavulanate group
1 P=0.02
Relapse and Residual Middle-Ear Effusion
0
Among children who met the criteria for clinical 1 2 3 4 5 6 7
success at the day 1012 visit, the rate of relapse Study Day
noted at or before the day 2125 visit was 16% (19
of 119 children) in the amoxicillinclavulanate
group and 19% (13 of 70) in the placebo group
(P=0.56). At the day 2125 visit, 71 of the 141 chil- lateral) and 87 of 139 in the placebo group (63%)
dren in the amoxicillinclavulanate group (50%) had middle-ear effusion (32 unilateral and 55 bi-
had middle-ear effusion (29 unilateral and 42 bi- lateral) (P=0.05).
n engl j med 364;2 nejm.org january 13, 2011 111
The New England Journal of Medicine
Downloaded from nejm.org by Ramza As'Ary on January 31, 2017. For personal use only. No other uses without permission.
Copyright 2011 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
Table 2. Clinical Failure Rates at or before the Day 1012 Visit, According to Study Group and Demographic
and Clinical Characteristics at Entry.*
AmoxicillinClavulanate Placebo Group All Children
Characteristic at Entry Group (N=144) (N=147) (N=291) P Value
no. of children with clinical failure/total no. (%)
Exposure to other children 0.007
No 10/73 (14) 29/73 (40) 39/146 (27)
Yes 13/69 (19) 44/70 (63) 57/139 (41)
AOM-SOS score 0.004
8 9/82 (11) 35/81 (43) 44/163 (27)
>8 14/60 (23) 38/62 (61) 52/122 (43)
Laterality of acute otitis media 0.002
Unilateral 6/68 (9) 29/70 (41) 35/138 (25)
Bilateral 17/74 (23) 44/73 (60) 61/147 (41)
Degree of tympanic membrane bulging <0.001
in worse ear
Slight or moderate 12/103 (12) 46/106 (43) 58/209 (28)
Marked 11/39 (28) 27/37 (73) 38/76 (50)
No. of unfavorable characteristics <0.001
0 1/19 (5) 4/15 (27) 5/34 (15)
1 4/42 (10) 14/46 (30) 18/88 (20)
2 6/44 (14) 27/46 (59) 33/90 (37)
3 8/26 (31) 20/28 (71) 28/54 (52)
4 4/11 (36) 8/8 (100) 12/19 (63)
* For each characteristic, the favorable category is listed first and the unfavorable second. All the tests for interactions be-
tween study group and the individual characteristics were nonsignificant. The odds ratios for the individual unfavorable
characteristics, adjusted for study group and for the remaining three characteristics, ranged from 2.0 to 2.3 (see Table
2 in the Supplementary Appendix for additional details). AOM-SOS denotes the Acute Otitis Media Severity of
Symptoms scale.
For the individual characteristics, P values are for the comparison, in the study groups combined, between children
with the favorable characteristic and children with the unfavorable characteristic. For the number of unfavorable charac-
teristics, the P value is for the test for linear trend from none to four.
Data were not available for some children because of missed visits.
Exposure to other children was defined as exposure to at least three children for at least 10 hours per week.
Nasopharyngeal Colonization and Other Complications and Adverse Events
Outcomes Mastoiditis developed in one child in the placebo
From day 1 to the day 2125 visit, no significant group on day 5. Dermatitis in the diaper area and
changes occurred in either group in the rate of protocol-defined diarrhea occurred commonly, and
colonization with nonsusceptible strains of Strep- often together, among children receiving antimi-
tococcus pneumoniae (minimum inhibitory concen- crobial agents. Details concerning complications
tration, 0.1 g per milliliter) (see Table 3 in the and adverse events are summarized in Table 3.
Supplementary Appendix for details). The rates
of clinical failure had no apparent relationship to Discussion
the childrens initial colonization status in either
group. We found no significant differences be- In this clinical trial involving children 6 to 23
tween the amoxicillinclavulanate group and the months of age with acute otitis media, children
placebo group in either the mean daily number who were treated with amoxicillinclavulanate,
of doses of acetaminophen administered (0.37 as compared with those who received placebo,
and 0.43, respectively; P=0.35) or the use of had consistently more favorable short-term out-
health care resources. comes, including a sustained symptomatic re-
112 n engl j med 364;2 nejm.org january 13, 2011
The New England Journal of Medicine
Downloaded from nejm.org by Ramza As'Ary on January 31, 2017. For personal use only. No other uses without permission.
Copyright 2011 Massachusetts Medical Society. All rights reserved.
Treatment of Acute Otitis Media in Young Children
Table 3. Complications and Adverse Events According to Study Group and Treatment Received at the Time of Occurrence.*
Adverse Event AmoxicillinClavulanate Group (N=144) Placebo Group (N=147)
During Receipt of
Amoxicillin During Receipt of During Receipt of During Receipt of
Clavulanate Rescue Therapy Total Placebo Rescue Therapy Total
number of children (percent)
Mastoiditis 0 0 0 1 (1) 0 1 (1)
Perforation of tympanic membrane 1 (1) 0 1 (1) 6 (4) 1 (1) 7 (5)
Protocol-defined diarrhea 34 (24) 2 (1) 36 (25) 11 (7) 11 (7) 22 (15)
Diaper-area dermatitis 67 (47) 6 (4) 73 (51) 24 (16) 27 (18) 51 (35)
Oral thrush 7 (5) 0 7 (5) 0 1 (1) 1 (1)
Vomiting 12 (8) 0 12 (8) 11 (7) 1 (1) 12 (8)
Rash** 1 (1) 0 1 (1) 1 (1) 1 (1) 2 (1)
* In each study group, one child was not followed beyond enrollment. Comparisons were adjusted for study site, history or no history of re-
current acute otitis media, and exposure or no exposure to other children.
Mastoiditis developed on day 5 in an 11-month-old child with unilateral acute otitis media and a score on the Acute Otitis Media Severity
of Symptoms (AOM-SOS) scale of 14 at entry and of 7 on day 5. A culture of middle-ear aspirate yielded serotype 19A Streptococcus pneu-
moniae with a penicillin minimum inhibitory concentration of 2 g per milliliter. The child was hospitalized for 41 hours and treated initial-
ly with parenteral antibiotics and subsequently with oral antibiotics; he recovered uneventfully.
Diarrhea was defined in the protocol as three or more watery stools in 1 day or two watery stools daily for at least 2 days. Treatment was
discontinued because of diarrhea in six children in the amoxicillinclavulanate group and one child in the placebo group, in whom
Clostridium difficile enteritis developed.
P=0.05 for the difference between the amoxicillinclavulanate group and the placebo group.
P=0.008 for the difference between the amoxicillinclavulanate group and the placebo group.
In the amoxicillinclavulanate group, treatment was discontinued in one child because of vomiting.
** In each group, treatment was discontinued in one child because of rash.
sponse, an absence of otoscopic evidence of per- with amoxicillinclavulanate was not associated
sistent middle-ear infection, and a reduced rate with a detectable increase in nasopharyngeal colo-
of residual middle-ear effusion. There were no nization with nonsusceptible strains of S. pneu-
suggestive or significant between-group differ- moniae, although the power to detect such emer-
ences in the use of analgesic drugs or health care gent resistance was limited.
resources. The interaction that we found between In keeping with recent recommendations,15
age and treatment is probably attributable to we chose the resolution of symptoms as the pri-
chance, since it involves small numbers of chil- mary outcome of interest. Because we had previ-
dren and runs counter to other findings.14 In both ously noted that symptoms often recurred after
study groups, the rates of clinical failure were having seemingly resolved, we defined the time
greatest among children who were most severely of resolution in two ways: the time at which an
affected initially. Nonetheless, the relative reduc- AOM-SOS score of 0 or 1 was first recorded and
tion in the risk of clinical failure at day 10 to 12 the time of the second of two successive record-
with amoxicillinclavulanate treatment, as com- ings of an AOM-SOS score of 0 or 1. We also
pared with placebo, was as large among the chil- measured the symptom burden over time, and
dren who were least severely affected those we used a combination of symptomatic response
whose illnesses would have been considered non- and middle-ear findings to categorize overall out-
severe as previously defined as it was among comes as either clinical success or clinical fail-
children whose illnesses would have been con- ure. The differences in symptom scores between
sidered severe. The principal side effects of treat- the two study groups were modest but consistent
ment both with amoxicillinclavulanate and with through the first 10 days of follow-up; the dif-
rescue antimicrobial agents were diarrhea and ferences were observed mainly among the chil-
dermatitis in the diaper area, but the side effects dren with the most severe symptoms initially. In
were usually not severe enough to result in dis- contrast, between-group differences in the over-
continuation of the offending drug. Treatment all clinical response, which included the symptom-
n engl j med 364;2 nejm.org january 13, 2011 113
The New England Journal of Medicine
Downloaded from nejm.org by Ramza As'Ary on January 31, 2017. For personal use only. No other uses without permission.
Copyright 2011 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
atic response and findings on otoscopic exami- of higher rates of clinical failure among the
nation, were substantial and were observed not children who received placebo. This finding, in
only among the children who had the most severe turn, seems to be attributable to the stringent
symptoms initially but also among the children diagnostic criteria that we used to ensure that
who had the least severe symptoms. To our knowl- we would study only children in whom the diag-
edge, a disparity of this nature has not been re- nosis of acute otitis media was quite certain.20
ported previously. These observations, together In conclusion, among children 6 to 23 months
with the fact that among infants and young chil- of age with acute otitis media, treatment with
dren, acute otitis media may be entirely asymp- amoxicillinclavulanate for 10 days affords a mea-
tomatic16,17 and the fact that symptoms may not surable short-term benefit, irrespective of the ap-
differentiate acute otitis media from other respi- parent severity of the illness. The benefit must be
ratory illnesses,18 suggest that overall clinical re- weighed against concern not only about the side
sponse constitutes the more telling measure of effects of the medication but also about the con-
outcome. Regardless of the initial severity of tribution of antimicrobial treatment to the emer-
symptoms, however, it is uncertain whether chil- gence of bacterial resistance. These considerations
dren who have become asymptomatic but have underscore the need to restrict treatment to chil-
otoscopic findings that suggest persistent infec- dren whose illness is diagnosed with the use of
tion are thereby at increased risk for illness later. stringent criteria.
Also uncertain is the clinical significance of per- Supported by a grant (3U01AI066007-02S1) from the National
Institute of Allergy and Infectious Diseases.
sistent middle-ear effusion in the apparent ab- Dr. Hoberman reports receiving honoraria and travel-expense
sence of infection. Because in young children otitis reimbursement from GlaxoSmithKline, and Dr. Wald, grant
media with effusion is often a forerunner of acute support from Merck and GlaxoSmithKline. No other potential
otitis media,19 it is possible that the higher preva- conflict of interest relevant to this article was reported.
Disclosure forms provided by the authors are available with
lence of persistent effusion among the children the full text of this article at NEJM.org.
in the placebo group than among children in the We thank all the families who participated in this study; the
amoxicillinclavulanate group might have placed many house officers at the Childrens Hospital of Pittsburgh; the
faculty and nurses at General Academic Pediatrics; Dr. Thomas
the children in the placebo group at greater risk G. Lynch, who facilitated onsite study-related activities at Arm-
for recurrent infection. strong Pediatrics in Kittanning, PA; the many Pittsburgh-area
The differences in outcome in this trial be- practitioners who referred children to the study; and, in particu-
lar, Dr. Michael D. Green, director of the Infectious Diseases
tween the children who were treated with amox- Research Laboratory; Dr. Judith M. Martin, independent safety
icillinclavulanate and the children who received monitor; members of the data and safety monitoring board
placebo were greater than the differences seen in (Drs. Eugene D. Shapiro, Stephen I. Pelton, Margaret A. Kenna,
most previous trials of antimicrobial agents Howard S. Faden, and George H. McCracken, Jr.); and Drs. Fa-
rukh M. Khambaty and Linda C. Lambert at the Division of Mi-
not because of better outcomes among the chil- crobiology and Infectious Diseases at the National Institute of
dren treated with antimicrobial agents but because Allergy and Infectious Diseases for administrative support.
References
1. Freid VM, Makuc DM, Rooks RN. Am- Network. Diagnosis and management of bial treatment for acute otitis media: not
bulatory health care visits by children: childhood otitis media in primary care. best for infants and young children. JAMA
principal diagnosis and place of visit. Vi- Guideline no. 66. Edinburgh: Royal Col- 1997;278:1640-2.
tal Health Stat 1998;13:1-23. lege of Physicians in Edinburgh, 2003. 10. Hoberman A, Dagan R, Leibovitz E, et
2. Finkelstein JA, Metlay JP, Davis RL, (http://www.sign.ac.uk/guidelines/fulltext/ al. Large dosage amoxicillin/clavulanate,
Rifas-Shiman SL, Dowell SF, Platt R. An- 66/index.html.) compared with azithromycin, for the
timicrobial use in defined populations of 6. Kaleida PH, Casselbrant ML, Rockette treatment of bacterial acute otitis media
infants and young children. Arch Pediatr HE, et al. Amoxicillin or myringotomy or in children. Pediatr Infect Dis J 2005;24:
Adolesc Med 2000;154:395-400. both for acute otitis media: results of a 525-32.
3. Rosenfeld RM, Vertrees JE, Carr J, et randomized clinical trial. Pediatrics 11. Shaikh N, Hoberman A, Paradise JL,
al. Clinical efficacy of antimicrobial 1991;87:466-74. et al. Development and preliminary evalu-
drugs for acute otitis media: metaanalysis 7. American Academy of Pediatrics Sub- ation of a parent-reported outcome in-
of 5400 children from thirty-three ran- committee on Management of Acute Oti- strument for clinical trials in acute otitis
domized trials. J Pediatr 1994;124:355-67. tis Media. Diagnosis and management of media. Pediatr Infect Dis J 2009;28:5-8.
4. Appelman CL, van Balen FA, van de acute otitis media. Pediatrics 2004;113: 12. Shaikh N, Hoberman A, Paradise JL,
Lisdonk EH, van Weert HC, Eizenga WH. 1451-65. et al. Responsiveness and construct valid-
Otitis media acuta: NHG-standaard (eerste 8. Forgie S, Zhanel G, Robinson J. Man- ity of a symptom scale for acute otitis me-
herziening). Huisarts Wet 1999;42:362-6. agement of acute otitis media. Paediatr dia. Pediatr Infect Dis J 2009;28:9-12.
(In Dutch.) Child Health (Oxford) 2009;14:457-64. 13. Kaleida PH, Stool SE. Assessment of
5. Scottish Intercollegiate Guidelines 9. Paradise JL. Short-course antimicro- otoscopists accuracy regarding middle-
114 n engl j med 364;2 nejm.org january 13, 2011
The New England Journal of Medicine
Downloaded from nejm.org by Ramza As'Ary on January 31, 2017. For personal use only. No other uses without permission.
Copyright 2011 Massachusetts Medical Society. All rights reserved.
Treatment of Acute Otitis Media in Young Children
ear effusion: otoscopic validation. Am J (http://www.fda.gov/downloads/Drugs/ symptom-based scores cannot predict
Dis Child 1992;146:433-5. GuidanceComplianceRegulatory acute otitis media at otitis-prone age. Pe-
14. Hoberman A, Paradise JL, Burch DJ, et Information/Guidances/ucm070947.pdf.) diatrics 2010;125(5):e1154-e1161.
al. Equivalent efficacy and reduced occur- 16. Hayden GF, Schwartz RH. Character- 19. Paradise JL, Bernard BS, Colborn DK,
rence of diarrhea from a new formulation istics of earache among children with Smith CG, Rockette HE. Otitis media
of amoxicillin/clavulanate potassium (Aug- acute otitis media. Am J Dis Child 1985; with effusion (OME): highly prevalent and
mentin) for treatment of acute otitis me- 139:721-3. often the forerunner of acute otitis media
dia in children. Pediatr Infect Dis J 1997; 17. Niemela M, Uhari M, Jounio-Ervasti (AOM) during the first year of life. Pediatr
16:463-70. K, Luotonen J, Alho OP, Vierimaa E. Lack Res 1993;33:121A. abstract.
15. Guidance for industry acute bacte- of specific symptomatology in children 20. Paradise JL. On classifying otitis me-
rial otitis media: developing drugs for with acute otitis media. Pediatr Infect Dis dia as suppurative or nonsuppurative, with
treatment. Revision 1. Rockville, MD: J 1994;13:765-8. a suggested clinical schema. J Pediatr
Food and Drug Administration, Center 18. Laine MK, Thtinen PA, Ruuskanen 1987;111:948-51.
for Drug Evaluation and Research, 2008. O, Huovinen P, Ruohola A. Symptoms or Copyright 2011 Massachusetts Medical Society.
n engl j med 364;2 nejm.org january 13, 2011 115
The New England Journal of Medicine
Downloaded from nejm.org by Ramza As'Ary on January 31, 2017. For personal use only. No other uses without permission.
Copyright 2011 Massachusetts Medical Society. All rights reserved.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Journal ReadingDocument8 pagesJournal ReadingRamza Shiddiq As'AryNo ratings yet
- Subtitle What Men Want Project EnglishDocument172 pagesSubtitle What Men Want Project EnglishRamza Shiddiq As'AryNo ratings yet
- Katalog Harga Perawatan My SalonDocument10 pagesKatalog Harga Perawatan My SalonRamza Shiddiq As'AryNo ratings yet
- Subtitle What Men Want Project EnglishDocument172 pagesSubtitle What Men Want Project EnglishRamza Shiddiq As'AryNo ratings yet
- Summoners War Fusion Calculation TableDocument14 pagesSummoners War Fusion Calculation TableRamza Shiddiq As'AryNo ratings yet
- Jornal Reading OtolaryngologyDocument7 pagesJornal Reading OtolaryngologyRamza Shiddiq As'AryNo ratings yet
- EncephalitisDocument25 pagesEncephalitisAndreas IoannouNo ratings yet
- Meta Analisis Deep Brain Stimulation Pada ParkinsonDocument2 pagesMeta Analisis Deep Brain Stimulation Pada ParkinsonRamza Shiddiq As'AryNo ratings yet
- CPAP For The Metabolic SyndromeDocument10 pagesCPAP For The Metabolic SyndromeRamza Shiddiq As'AryNo ratings yet
- Upper-Airway Stimulation For Obstructive Sleep ApneaDocument11 pagesUpper-Airway Stimulation For Obstructive Sleep ApneaRamza Shiddiq As'AryNo ratings yet
- Farmakologi Sistem Reproduksi: Ramza Shiddiq As'Ary, S.KedDocument19 pagesFarmakologi Sistem Reproduksi: Ramza Shiddiq As'Ary, S.KedRamza Shiddiq As'AryNo ratings yet
- EncephalitisDocument25 pagesEncephalitisAndreas IoannouNo ratings yet
- A Placebo-Controlled Trial of AntimicrobialDocument11 pagesA Placebo-Controlled Trial of AntimicrobialRamza Shiddiq As'AryNo ratings yet
- SW - 6 Star Calculator-Critical CalculatorDocument7 pagesSW - 6 Star Calculator-Critical CalculatorRamza Shiddiq As'AryNo ratings yet
- Formato Denver IIDocument1 pageFormato Denver IIMelly AnidaNo ratings yet
- Summoners War Fusion Calculation TableDocument14 pagesSummoners War Fusion Calculation TableRamza Shiddiq As'AryNo ratings yet
- Summoners War Fusion Calculation TableDocument14 pagesSummoners War Fusion Calculation TableRamza Shiddiq As'AryNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- 50 Item Psychiatric Nursing Exam IDocument11 pages50 Item Psychiatric Nursing Exam Iɹǝʍdןnos98% (40)
- 2008 04 Lecture 1 Interface Dermatitis FrishbergDocument6 pages2008 04 Lecture 1 Interface Dermatitis FrishbergYudistra R ShafarlyNo ratings yet
- Peran Perawat KomDocument27 pagesPeran Perawat Komwahyu febriantoNo ratings yet
- Unit - 1 Concepts and Definitions 1.1 Disaster (I)Document25 pagesUnit - 1 Concepts and Definitions 1.1 Disaster (I)RISHITHA LELLANo ratings yet
- PEC in INDIA ExplainationDocument3 pagesPEC in INDIA ExplainationSaumya ChandraNo ratings yet
- Types of PovertyDocument6 pagesTypes of PovertyJacobNo ratings yet
- Nutritional Knowledge Among Malaysian ElderlyDocument12 pagesNutritional Knowledge Among Malaysian ElderlyNoor Khairul AzwanNo ratings yet
- IMCI Chart BookletDocument66 pagesIMCI Chart Bookletnorwin_033875No ratings yet
- Personal Safety With Dance: Worksheet in Health Optimizing Physical Education 3 (HOPE3/PEH3)Document9 pagesPersonal Safety With Dance: Worksheet in Health Optimizing Physical Education 3 (HOPE3/PEH3)Cregie Brillantes QuezaNo ratings yet
- Group DR - Script - Allergic Rhinitis (Peanut Allergy) Health EducationDocument10 pagesGroup DR - Script - Allergic Rhinitis (Peanut Allergy) Health EducationKyra Bianca R. FamacionNo ratings yet
- Notice: Agency Information Collection Activities Proposals, Submissions, and ApprovalsDocument2 pagesNotice: Agency Information Collection Activities Proposals, Submissions, and ApprovalsJustia.comNo ratings yet
- Drug Treatment of AnemiasDocument29 pagesDrug Treatment of AnemiasKashmalaNo ratings yet
- g8 Health q3 LM Disease 130908005904 PDFDocument64 pagesg8 Health q3 LM Disease 130908005904 PDFkenneth cannillNo ratings yet
- J Villanueva Group 2Document22 pagesJ Villanueva Group 2Caryl Jole PaligsaNo ratings yet
- Pro-Oxidant Strategies - Cancer Treatments ResearchDocument71 pagesPro-Oxidant Strategies - Cancer Treatments ResearchSpore FluxNo ratings yet
- Lab Normal Value S&Sof S&Sof : Loma Linda University School of Nursing Accepted Lab Values Adapted From KaplanDocument3 pagesLab Normal Value S&Sof S&Sof : Loma Linda University School of Nursing Accepted Lab Values Adapted From KaplanGiacen100% (3)
- Evidence-Based Practice in Pediatric Physical Therapy by BarryDocument14 pagesEvidence-Based Practice in Pediatric Physical Therapy by BarryFe TusNo ratings yet
- Food Act 1983Document14 pagesFood Act 1983Shahirah Zubir0% (1)
- Fatima's CommissionDocument7 pagesFatima's CommissionSachie Daniela CheungNo ratings yet
- Lista Medicamente OTC Conform Nomenclator ANM 17 Feb2020Document184 pagesLista Medicamente OTC Conform Nomenclator ANM 17 Feb2020Andreea PasolNo ratings yet
- Written Assignment Principles of Applied RehabilitationDocument17 pagesWritten Assignment Principles of Applied RehabilitationRuqaiyah RahmanNo ratings yet
- Misericordia LetterDocument2 pagesMisericordia LetterKatie DangerfieldNo ratings yet
- Week 2 SolutionsDocument4 pagesWeek 2 Solutionsannavarapuanand100% (2)
- Addressing The Gaps in Nutritional Care Before and During PregnancyDocument12 pagesAddressing The Gaps in Nutritional Care Before and During PregnancyBushra KainaatNo ratings yet
- Chapter 2 Lesson 1Document3 pagesChapter 2 Lesson 1John Carldel VivoNo ratings yet
- Disaster Preparedness IntroDocument10 pagesDisaster Preparedness IntroBernadette-Mkandawire MandolomaNo ratings yet
- N4H InvitationLetter - FinalDocument2 pagesN4H InvitationLetter - Finalluis DiazNo ratings yet
- Stress Management WorkbookDocument19 pagesStress Management WorkbookKATHYNo ratings yet
- Helping Your Child With Extreme Picky Eating A Step-by-Step Guide For Overcoming Selective Eating, Food Aversion, and FeedingDocument242 pagesHelping Your Child With Extreme Picky Eating A Step-by-Step Guide For Overcoming Selective Eating, Food Aversion, and FeedingAndrew Wongkar100% (3)
- Introduction To Occupational Therapy PDFDocument291 pagesIntroduction To Occupational Therapy PDFMurat Hasan BaşaranNo ratings yet