Professional Documents
Culture Documents
Uti Pedia
Uploaded by
Neenya SisonOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Uti Pedia
Uploaded by
Neenya SisonCopyright:
Available Formats
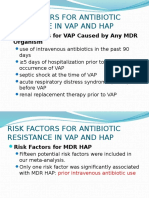
PIDSP Journal 2010 Vol 11 No.
1 10
Copyright 2010
CLINICAL AND LABORATORY PROFILE OF URINARY TRACT INFECTION
AMONG CHILDREN AT THE OUTPATIENT CLINIC OF A TERTIARY HOSPITAL
AUTHORS: April Gamier Bay, MD, Francisco Anacleto, Jr., MD
University of the Philippines College of Medicine- Philippine General Hospital
KEYWORDS
urinary tract infection, children, incidence, clinical profile, diagnosis
ABSTRACT
Introduction: Urinary tract infection (UTI) is a common reason for outpatient consults. It is almost always
in the Top Ten consults at the sick-child clinic of a tertiary hospital. However, a study concerning the
incidence and clinical and laboratory profiles of UTI in the Philippines has yet to be documented.
Objectives: To determine the incidence rate and clinical and laboratory profiles of UTI among patients
who consulted at the pediatric outpatient clinic of a tertiary hospital.
Methods: All patients 0 to 12 years, who were UTI suspects and consulted at the Sick-Child Clinic of a
tertiary hospital from January to December 2006 were included in the study. Patients who had recurrent
UTI or history of previous UTI and those with co-morbidities such as anatomic and/or functional
problems involving the urinary tract were excluded. Chart review was done and the following were noted:
demographics and clinical and laboratory characteristics.
Results: Four hundred twenty three patients were included in the study. The incidence rate was 30 per
1000 persons (95% CI). 54% percent were female. The majority of the patients were between 7 to 12 years
of age. The most common presenting symptoms were fever, abdominal pain, vomiting, and dysuria. Only
25 patients had urine culture done and only 8 had positive results, mostly with E. coli. The most common
antibiotics used were Cotrimoxazole, Cefuroxime, and Amoxicillin.
Conclusion: The incidence rate is higher compared to other studies done in general practice. The
presenting signs and symptoms were however similar. Important to note is the high incidence of patients
who did not follow up. It is also noted that the gold standard for the diagnosis of UTI, which is the urine
culture is very seldom requested. This may lead to the over- or maybe under-diagnosis of UTI and its
eventual mismanagement. Therefore, it is recommended that the approach to the diagnosis and
management of UTI in children should be reviewed.
is reversed, with majority of UTI occurring in
INTRODUCTION females.3
A urinary tract infection (UTI) is a bacterial Although UTI is infrequently associated with
infection that affects any part of the urinary mortality, it is still a significant cause for
tract. It is one of the most common bacterial morbidity. Delay in the treatment of UTI can
infections among children. However, the lead to vesicoureteral reflux and renal scarring.
epidemiology of UTI is confounded by the Renal scarring has been cited as one of the
variability and non-specificity of signs and most common causes of end stage renal
symptoms of infection in infants and young disease in both adults and children.4
children.1 The incidence of UTI and its clinical UTI is a common cause for a significant
impact are very different for both sexes and at number of out patient visits.3 In the pediatric
different stages of life.2 It is known that UTI is outpatient clinic of a tertiary hospital in the
more frequent in boys in the first 3 months of Philippines, it remains in the Top Ten Consults
life, with sex distribution of 5:1 (male almost every year. Keeping in view the high
predominance). By preschool age, the sex ratio incidence of UTI in children and its associated
Downloaded from www.pidsphil.org
PIDSP Journal 2010 Vol 11 No.1 11
Copyright 2010
morbidity, it is imperative to diagnose UTI early In 2005, a study was done at Ayub Teaching
and to treat the infection promptly. This study Hospital in Pakistan to look into the clinical
proposed to look into the clinical profile of UTI profile of UTI in children admitted at the
in children presenting at the pediatric pediatric wards. Said study showed that the
outpatient clinic of a Tertiary Hospital. majority of UTI patients (46%) belonged to the
age group 13 to 60 months: The number of UTI
REVIEW OF RELATED LITERATURE cases was less among neonates; the number of
Urinary tract infection is defined as the cases increased in the older age group, but it
presence of bacteria in urine along with declined in the thirteen to fifteen age group.
symptoms of infection. The first and most Fever was the most common presentation; 92%
critical step in establishing the diagnosis of UTI of the patients had history of fever. Dysuria is a
is the method by which urine is collected. In common presentation in older children (4% to
young patients, care must be taken in preparing 60.8%).3
the perineum and periurethral area for Also in 2005, the profile of children with UTI
placement of the sterile plastic receptacle, who consulted at a Chilean pediatric
which will be used for collection of urine. In emergency institution/clinic showed that UTI
infants, the best way to obtain urine for culture was 1.78 times more frequent in girls. The
aseptically is by urethral percutaneous supra- most common clinical presentations were fever
pubic bladder aspiration or by catheterization. and urinary tract symptoms. For patients who
These procedures avoid the potential problem are more than 2 years old, urinary tract
of contaminated urine cultures that often result symptoms and previous UTI, were risk factors
from bag specimens. Older children and for UTI. The most frequent organism isolated
adolescents can be instructed to collect a was Escherichia coli (86%).8 Based on the
midstream urine specimen after proper previous studies, reported incidence rates of
cleansing of the urethral area. Demonstration childhood UTI vary. For boys the reported
of bacteria microscopically is the most reliable incidence rates range from 0.17 to 18 per 1000
and fastest mean to establish the diagnosis of person years and for girls from 0.4 to 66 per
UTI before results of urine cultures are 1000 person years. This variation may be
available. The presence of 105 colony forming explained by differences in setting, health care
units (CFU) of a single organism per mil of urine system, age range, case definition, or study
is diagnostic of UTI.5 period. The range of occurrence rates is found
Studies conducted at Parkland Memorial to be much smaller in studies carried out in
Hospital in Dallas demonstrated that the general practice. From 2000 to 2002, a national
incidence rate of UTI in infants (6 months of survey was conducted in Sweden involving
age and younger) was 1.65 cases/1000 live general practice and involving patients 0 to 18
births from (in) 1972 to 1975, and 2.04 years old; it was published in 2006. The results
cases/1000 live births from (in) 1977 to 1980. showed an overall incidence rate of 19.0
The male: female ratios were 2.7:1 and 5:1, in episodes of UTI presented in general practice
the two time periods.6 per 1000 person years for children under the
Boys are more susceptible to UTI before the age of 18 years (95% CI: 18.1 to 19.9). In other
age of 3 months; thereafter, the incidence is words, if 1000 children, who are 0 to 18 years
substantially higher in girls. Estimates of the old, are monitored/checked on for one year,
true incidence of UTI (urinary tract infection) their general practitioner would have made 19
depend on rates of diagnosis and investigation. times more diagnoses of UTI. The incidence
At least 8% of girls and 2% of boys will have UTI rate in girls was almost 8 times higher than in
(a urinary tract infection) in childhood. boys (respectively, 34.4 episodes per 1000
Downloaded from www.pidsphil.org
PIDSP Journal 2010 Vol 11 No.1 12
Copyright 2010
person years vs. 4.4 episodes per 1000 person Recurrent UTI occurrence of the disease at
years, p < 0.001). 9 least twice a year
In the local setting, a study was done in Pyuria urinalysis with 5WBC/hpf
1997 at the Pediatric Emergency room of the Positive urine culture with 100,000CFU/ml
Philippine General Hospital among subjects less of urine of a single pathogen
than 2 years old. This study was conducted to
determine the prevalence of UTI among febrile RESULTS
infants and young children with or without A total of 457 charts were reviewed for the
apparent source of fever. A total of 40 patients study period of January to December 2006.
were included in the study. Results showed Thirty four patients were excluded: 11 patients
that the prevalence of UTI was 7.5% (95%CI: had recurrent UTI, 7 had Acute
15.7%-20.7%): all were males and with Glomerulonephritis, 3 had Nephrotic
apparent sources of fever. However, due to the Syndrome, 1 had Lupus nephritis, 1 had
limited number of subjects, the results were diabetic nephropathy, 5 had phimosis, 1 had
inconclusive. 4 hypospadia, 1 had epispadia, and 3 had
neurogenic bladder. Four hundred twenty
OBJECTIVES three UTI suspects were included in the study.
The aim of the study was to determine the Of the 423 patients included in the study,
clinical and laboratory profile of UTI in children 228 (53.9%) were females and 195 (46.1%)
presented at the pediatric outpatient clinic of a were males (Table 1). Table 1 also shows that
tertiary hospital. the majority of patients belong to the 7-to-12-
years-old group or the school-age group,
MATERIALS AND METHODS showing a total of 180 patients or 42.6% of the
This study is retrospective and descriptive. population. This is closely followed by the 3-to-
Subjects (included) were patients, who 6-years-old age group, with a total of 166
were 0 to 12 years old, were suspected of patients or 39.2%.
having UTI and consulting at the Sick-Child Fever was the most common presenting
Clinic of a tertiary hospital from January to symptom, accounting for 63.6% of patients. It
December 2006. Excluded from the study were was the most common symptom for all age
patients who had previous histories of UTI or groups. This was followed by abdominal pain
with recurrent UTI and those with co- (57%), vomiting (35.9), and dysuria (30.7%).
morbidities such as anatomic and/or functional For the age group of 0 to 3 mos, diarrhea,
problems involving the urinary tract (i.e. those irritability, and staining were the other
that would cause neurogenic bladder, symptoms noted. For the 4 to 12mos age
vesicoureteral reflux, etc). Charts of all eligible group, vomiting and irritability were second
subjects were reviewed and the following only to fever. For the rest of the age groups,
information were collected: age, sex, signs and other symptoms noted were anorexia, diarrhea
symptoms, urinalysis results, urine culture and frequency.
results, antibiotics used, other workups done, Among the subjects of the study, 44.4% did
and the patients disposition upon follow up. not come back for a follow-up, hence no
Definition of Terms urinalysis was recorded. Only 35.2% of the UTI
UTI suspect with signs and symptoms that are suspects had pyuria, therefore had presumptive
associated with UTI UTI. In terms of urine culture, 94.1% of the
Presumptive UTI positive for pyuria on subjects had no urine culture done. Only 1.9%
urinalysis of the subjects had bacteriuria.
Confirmed UTI positive for pyuria Among those who had urine culture done, 7
documented by positive urine culture showed no growth after 2 days of incubation;
Downloaded from www.pidsphil.org
PIDSP Journal 2010 Vol 11 No.1 13
Copyright 2010
Table 1. Distribution of UTI suspects according to age and sex.
Age Male Female TOTAL
No. (%) No. (%) No. (%)
0-3mos 4 (1.0) 2 (0.5) 6 (1.4)
4mos- 12mos 15 (3.5) 8 (1.9) 23 (5.4)
13mos 2yrs 21 (5.0) 27 (6.4) 48 (11.4)
3yrs 6yrs 83 (19.6) 83 (19.6) 166 (39.2)
7yrs 12yrs 72 (17.0) 108 225.5) 180 (42.6)
TOTAL 195 (46.1) 228 (53.9) 423 (100)
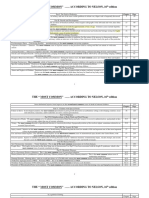
Table 2. Clinical Manifestations according to age group.
Signs and 0-3m 4 13mos 3years 7years TOTAL %
symptoms 12mos 2years 6years 12years
Abdominal 11 111 119 241 57.0
pain
Abdominal 2 11 17 30 7.1
tenderness
Anorexia 4 43 29 76 18.0
Constipation 2 3 2 7 1.7
CVA 2 3 5 1.2
tenderness
Diarrhea 1 2 6 11 23 43 10.2
Dribbling 2 1 5 8 1.9
Dysuria 8 61 61 130 30.7
Fever 6 18 36 107 102 269 63.6
Flank pain 1 25 26 6.1
Frequency 4 25 22 51 12.1
Genital 11 1 12 2.8
discharge
Genital pain 6 1 7 1.7
Hematuria 2 7 16 27 6.4
Intermit-tency 4 3 7 1.7
Irritability 1 2 3 0.7
Nausea 1 6 15 22 5.2
Oliguria 1 1 8 3 13 3.1
Staining 1 1 2 0.5
Straining 1 4 9 2 16 3.8
on urination
Urgency 4 5 9 2.1
Vomiting 9 15 62 66 152 35.9
* Patient may present with one or more signs and symptoms
* Legend: Years y; Months m
Downloaded from www.pidsphil.org
PIDSP Journal 2010 Vol 11 No.1 14
Copyright 2010
10 showed growth of pathogens, but were persistent UTI. However, 88.2% of our subjects
<100,000CFU/ml of urine. Among those who were eventually lost to follow up.
showed positive for bacteriuria, Escherichia coli
(44.4%) was the most common organism found, Table 6. Antibiotics used.
followed by Enterobacter spp. (16.7%), and Antibiotics No. (%)
Pseudomonas aeruginosa (11.1%). Amoxicillin 39 (9.2)
The most common antibiotic used among Cefaclor 1 (0.2)
our subjects was Cotrimoxazole (26%); this is Cefalexin 9 (2.1)
followed by Cefuroxime (13.2%) and Amoxicillin Cefixime 1 (0.2)
(9.2%). Some of our subjects were untreated Cefuroxime 56 (13.2)
(44.7%). Chloramphenicol 3 (0.7)
Ciprofloxacin 1 (0.2)
Table 3. Results of Urinalysis and Urine Culture Co-Amoxiclav 9 (2.1)
Urine WBC No. (%) Cotrimoxazole 110 (26.0)
WBC < 5/hpf 86 (20.3) Nitrofurantoin 3 (0.7)
WBC 5/hpf 149 (35.2) Ofloxacin 1 (0.2)
Urinalysis not done 188 (44.4) Penicillin 1 (0.2)
Urine Culture No treatment 189 (44.7)
Positive 8 (1.9)
Table 7. Other laboratory examinations done.
Negative 17 (4.0)
Other laboratory exams No. (%)
Not done 398 (94.1)
KUB IVP 7 (1.7)
Table 5. Organisms obtained from the urine KUB UTZ 49 (11.5)
culture. VCUG 4 (0.9)
Organisms <100,000 100,000 TOTAL
CFU/ml CFU/ml Table 8. Disposition on follow up.
No. (%) No. (%) No. (%) Disposition No. (%)
Klebsiella - 1 (5.6) 1 (5.6) Cystolithiasis 1 (0.2)
pneumoniae - Hydronephrosis 1 (0.2)
Escherichia 3 (16.7) 5 (27.8) 8 (44.4) Nephrolithiasis 1 (0.2)
coli Persistent UTI 7 (1.7)
Acinetobacter 1 (5.6) - 1 (5.6) Recurrent UTI 7 (1.7)
baumanii
Renal agenesis 1 (0.2)
Staph. aureus 1 (5.6) - 1(5.6)
Staph. spp. 1 (5.6) - 1 (5.6) Renal parenchymal 1 (0.2)
Enterobacter 2 (11.1) 1(5.6) 3(16.7) disease
Pseudo 1 (5.6) 1 (5.6) 2 (11.1) VUR 1 (0.2)
aeruginosa Improved 30 (7.1)
Strep 1 (5.6) -- 1(5.6) Lost to follow up 373 (88.2)
pyogenes TOTAL 423 (100)
TOTAL 10 (55.5) 8 (44.4) 18 100
DISCUSSION
Other laboratory workups requested for our In this study, 423 UTI suspects were
subjects were KUB-UTZ (10.6%), KUB-IVP identified with a computed incidence rate of 30
(1.7%), and VCUG (0.9%). On follow up, 7.1% of per 1000 persons (95% CI). This value is much
our subjects were found to have improved, higher than in the study done in Sweden,
1.7% had recurrent UTI, and another 1.7% had where the incidence rate was only 19 per 1000
Downloaded from www.pidsphil.org
PIDSP Journal 2010 Vol 11 No.1 15
Copyright 2010
persons.9 The value we got for the present These statements were verified in this study.
study may be an over estimation since a large Among the 423 UTI suspects, only 235 had
percentage of these UTI suspects (44.4%) were urinalysis done and a mere 149 had pyuria.
actually lost to follow up and diagnosis was not Disappointingly, only 25 had urine culture done
supported by a urinalysis. If we look at the and only 8 were confirmed to have bacteuria.
incidence rate of patients with presumptive Among those that showed positive for urine
UTI, which is 10.5 per 1000, this is closer to the culture, Escherichia coli was the most frequent
reported incidence rate from previous studies. organism isolated. This is in complete
The present study showed that the majority agreement to the findings in a study done in
of patients belonged to the age group 7 to 12 Chile.
years. However, if we combined the age The most common antibiotics used for the
groups 13 mos to 2 years and 3 to 6 years, they subjects in this study were Cotrimoxazole,
accounted for 214 patients or 50.6% of the Cefuroxime, and Amoxicillin. According to the
population. These combined values will 2004 Clinical Practice Guideline as regards the
approximate the findings of the study in approach and treatment of UTI in children in
Pakistan where it was showed that 46% of their the Philippine setting, Amoxicillin and
subjects belonged to the age group 13 to 60 Cotrimoxazole are in the list of antibiotics for
months.3 This could be because, as reported by oral treatment of UTI. Cefuroxime is not in the
other studies, those who belong in the age said list.
group of 13 to 60 months are having toilet
training problems, and thus, more susceptible CONCLUSIONS/RECOMMENDATIONS
to infections. The incidence rate of UTI in a tertiary
It is known that UTI is more frequent in Hospital Outpatient Clinic is higher compared
boys in the first 3 months of life. In the present to other studies done in general practice. This
study, this was also true; male to female ratio may be attributed to over estimation due to a
of 2:1. The sex ratio is equal, instead of high incidence of patients being lost to follow
reversed by the preschool age (1:1). The up. UTI is more common among patient the age
reversal of the sex ratio was more apparent in group of 13 months-6years. UTI is generally
the pre-adolescent age (1:1.5) with majority of more common in females than in males. In
UTIs occurring in females. Overall, in terms of early infancy though, males are more
gender distribution, our study showed that UTI susceptible but as the age increases the gender
was 1.5 times more frequent in girls. This is ratio is reversed. The presenting signs and
very close to the value arrived at in the study symptoms were however similar, fever being
done at a Chilean Hospital which showed that the most common presentation in all age
UTI was 1.78 times more frequent in girls. 8 groups. This study confirmed that in the local
Similar to previous studies, fever was the setting, the diagnosis of UTI is based on clinical
most common presentation for all age groups. presentation of the patient, often times
It accounted for 63.6% of the study population supported by urinalysis, rarely confirmed by
which is comparable to the proportion reported urine culture and sensitivity. Most UTIs were
by the study done in Pakistan which was 92%. presumptive since bacterial growth was never
In the Philippines, the diagnosis of UTI is documented.
based on the clinical presentation of the RECOMMENDATIONS
patient; it is often times supported by It is recommended that dipstick test should
urinalysis, but rarely confirmed by urine culture be made available at the outpatient clinic in
and sensitivity. That is why most UTIs were order to lessen the incidence of patients being
presumptive, because bacterial growth was lost to follow up and, at the same time, to
never documented; to do so is very costly.4 ensure the appropriate management of the
Downloaded from www.pidsphil.org
PIDSP Journal 2010 Vol 11 No.1 16
Copyright 2010
patients. Another recommendation is that the 11. Clinical practice guidelines in the approach and
approach to the diagnosis and management of treatment of urinary tract infection in children in the
Philippine setting. Philippine Pediatric Society. 2004.
UTI in children should be reviewed and these
guidelines should be followed as much as
possible. Urine culture should be done more
often, if not all the time, in order for us to be
sure that we are using the correct antibiotic.
Also we recommend that ultrasound and
cystogram be requested as proposed by
acceptable guidelines.
REFERENCES
1. Alinea MCD, Mantaring JBV III. A single blind,
randomized controlled trial on the effect of
cranberry juice as adjunct to antibiotics in the
treatment of recurrent urinary tract infection in
children. PIDSP J. 2002 July-Dec; 6(3):45-52.
2. Jose PA. Acute urinary tract infection in children. Phil
J Pediatr Proceedings of the 34th PPS Annual
Convention and Golden Anniversary. 1997 Special
Issue: 29-31.
3. Qureshi AM. Clinical presentation of urinary tract
infection among children at Ayub Teaching Hospital.
Abbottabad. J Ayub Med Coll Abbottabad. 2005 Apr-
Jun; 7(2):79-81.
4. De Leon MAB. Prevalence of urinary tract infection
in febrile infants and young children. Phil J Pediatr.
1997 July-Sep; 46(3):185-187.
5. McCracken GH. Options in antimicrobial
management of urinary tract infections in infant and
young children. Ped Inf Dis Newslett. 1989 Aug;
8(8):552-555.
6. Nelson J, McCracken GH. Circumcision and UTI. Ped
Inf Dis Newslett. 1984; 10:6.
7. Stark H. Urinary tract infections in girls: the cost-
effectiveness of currently recommended
investigative routines. Pediatr Nephrol. 1997;
11:174-77 [Medline].
8. Lizama CM, Luco IM, Reichhard TC, Hirsch BT.
Urinary tract infection in a pediatrics emergency
department: frequency and clinical parameters. Rev
Chilena Infectol. 2005 Sep; 22(3):235-41. Epub 2005
Aug 2.
9. Wing-Yeh Kwok, et. al. Incidence rates and
management of urinary tract infections among
children in Dutch general practice: results from a
nationwide registration study. BMC Pediatr.
2006;6:10.
10. Evidence-based care guideline for medical
management of first urinary tract infection in
children 12 years of age or less. Cincinnati (OH):
Cincinnati Children's Hospital Medical Center; 2006
Nov. 23 p. [70 references].
Downloaded from www.pidsphil.org
You might also like
- TB CPG (PPS)Document28 pagesTB CPG (PPS)Chandice CuaNo ratings yet
- Acog Practice BulletinDocument10 pagesAcog Practice BulletinCristian AranibarNo ratings yet
- Pediatrics PerpetualDocument20 pagesPediatrics PerpetualHazel Fernandez VillarNo ratings yet
- TransfusionPractices Compendium 3rdeditionDocument81 pagesTransfusionPractices Compendium 3rdeditionIngrid GamboaNo ratings yet
- MC NelsonsDocument31 pagesMC NelsonsNiñoTanNo ratings yet
- Oral Cases Study Guide - PediatricsDocument68 pagesOral Cases Study Guide - PediatricsJohn100% (1)
- Nasal Cavity and Paranasal Sinuses AnatomyDocument19 pagesNasal Cavity and Paranasal Sinuses AnatomyLicensed to HealNo ratings yet
- Bartter Syndrome Vs Gitelman SyndromeDocument1 pageBartter Syndrome Vs Gitelman SyndromeBobet ReñaNo ratings yet
- IM Revalida Review 2019Document75 pagesIM Revalida Review 2019Nathaniel CamangonNo ratings yet
- Fever and Rash Mnemonic Based Approach Epomed 2Document1 pageFever and Rash Mnemonic Based Approach Epomed 2KC Dela RosaNo ratings yet
- Neonatal PneumoniaDocument2 pagesNeonatal PneumoniaJustin EduardoNo ratings yet
- Acrodermatitis EnteropathicaDocument4 pagesAcrodermatitis EnteropathicaIntan FajrinNo ratings yet
- Complaint Scenarios TrainingDocument8 pagesComplaint Scenarios TrainingJaypee Fabros EdraNo ratings yet
- Pediatric Gastritis, Gastropathy, and Peptic Ulcer Disease: Education GapDocument10 pagesPediatric Gastritis, Gastropathy, and Peptic Ulcer Disease: Education GapvgmanjunathNo ratings yet
- Preventive Pediatrics Part 1Document6 pagesPreventive Pediatrics Part 1mkct111No ratings yet
- Practical Management of AsthmaDocument13 pagesPractical Management of AsthmaAmi LuNo ratings yet
- Reviewer For Pedia Osce: 10.5 KG 45.16 CM / 17.8 in 75 CM SixDocument10 pagesReviewer For Pedia Osce: 10.5 KG 45.16 CM / 17.8 in 75 CM SixJamora ManilynNo ratings yet
- 1.acute Respiratory Disease: DDX: Kawasaki, Strep. InfectionDocument5 pages1.acute Respiratory Disease: DDX: Kawasaki, Strep. InfectionSheryl Layne Lao-SebrioNo ratings yet
- Pedia - CNS Infection, Seizures, NMD (Agrava)Document30 pagesPedia - CNS Infection, Seizures, NMD (Agrava)Ivy Grace LimNo ratings yet
- March 2022 Hybrid Full Course OFFICIAL Lecture Schedule - NOV-DEC UPLOADDocument3 pagesMarch 2022 Hybrid Full Course OFFICIAL Lecture Schedule - NOV-DEC UPLOADJhon PauloNo ratings yet
- PSGNDocument23 pagesPSGNalpha mae beltranNo ratings yet
- Finals QuestionsDocument10 pagesFinals QuestionsBobet ReñaNo ratings yet
- Philippines TB CP Guidelines 2006Document151 pagesPhilippines TB CP Guidelines 2006wiltechworksNo ratings yet
- Pedia ReviewDocument22 pagesPedia ReviewDebbie LanceroNo ratings yet
- FLUID MANAGEMENT IN MALNUTRITIONDocument30 pagesFLUID MANAGEMENT IN MALNUTRITIONCHALIE MEQUNo ratings yet
- PEDIA - Cardio (Esguerra) PDFDocument9 pagesPEDIA - Cardio (Esguerra) PDFMedisina101No ratings yet
- Pediatrics:: History Taking and Physical Examination of AdolescentsDocument14 pagesPediatrics:: History Taking and Physical Examination of AdolescentsJüdith Marie Reyes BauntoNo ratings yet
- Pedia TicklersDocument24 pagesPedia Ticklersjoshua espirituNo ratings yet
- Sepsis in ChildrenDocument10 pagesSepsis in ChildrenMario FloresNo ratings yet
- Rabies Lay ForumDocument40 pagesRabies Lay ForumCarlos H. AcuñaNo ratings yet
- Pediatrics in ReviewDocument16 pagesPediatrics in ReviewMaria3 Juliao3No ratings yet
- Childhood Asthma Etiology and EpidemiologyDocument24 pagesChildhood Asthma Etiology and EpidemiologyEstella100% (1)
- Fluminant Pertussis PDFDocument11 pagesFluminant Pertussis PDFDooriitha Pérez Peralta100% (1)
- Pediatrics - Michael GrantDocument78 pagesPediatrics - Michael GrantPappitha RajaNo ratings yet
- CHNDocument26 pagesCHNJen PanganibanNo ratings yet
- Medical History Form and Physicians Report For SHS and College StudentsDocument2 pagesMedical History Form and Physicians Report For SHS and College StudentsKimNo ratings yet
- Chronic Kidney Disease in PregnancyDocument64 pagesChronic Kidney Disease in PregnancyRemelou Garchitorena AlfelorNo ratings yet
- WHO - Haemoglobin Level For Anemia 2011Document6 pagesWHO - Haemoglobin Level For Anemia 2011Adhi SanjayaNo ratings yet
- Session11-Premalignant Lesions of The Cervix, CX CADocument68 pagesSession11-Premalignant Lesions of The Cervix, CX CACHALIE MEQU100% (2)
- Pediatric Cervical LymphadenopathyDocument13 pagesPediatric Cervical LymphadenopathyShaira Aquino VerzosaNo ratings yet
- Hap VapDocument18 pagesHap VapAgita GintingNo ratings yet
- Most Common Nelsons 16th EdDocument32 pagesMost Common Nelsons 16th EdRegine PanaliganNo ratings yet
- Care of the Well NewbornDocument10 pagesCare of the Well NewbornAntonio ValleNo ratings yet
- PDFDocument70 pagesPDFPaul Benjomin AgregadoNo ratings yet
- SLMC GC Ipch Osoe (Age) Oct 2019Document4 pagesSLMC GC Ipch Osoe (Age) Oct 2019Alvin FlorentinoNo ratings yet
- Immunodeficiency DisordersDocument8 pagesImmunodeficiency DisordersMutya XDNo ratings yet
- Nac 2017Document18 pagesNac 2017Nataly CortesNo ratings yet
- Physio Ob ReviewDocument368 pagesPhysio Ob ReviewMark LopezNo ratings yet
- Vitamin K deficiency causes and treatmentDocument22 pagesVitamin K deficiency causes and treatmentKatrin Marcelina SihombingNo ratings yet
- CPG Managment of Neonatal Jaundice (Second Edition) NewDocument62 pagesCPG Managment of Neonatal Jaundice (Second Edition) NewHafiz HamidiNo ratings yet
- Bronchiolitis: Practice GapsDocument11 pagesBronchiolitis: Practice GapsMichelleHanNo ratings yet
- Prep Id 2017 FainalDocument81 pagesPrep Id 2017 Fainala alrabiaahNo ratings yet
- HAB ManualDocument102 pagesHAB ManualSven OrdanzaNo ratings yet
- Platelet Disorders: Practice GapsDocument14 pagesPlatelet Disorders: Practice GapsMichelleHanNo ratings yet
- Pedia HXDocument3 pagesPedia HXeyakoyNo ratings yet
- Very Update Information About MedicineDocument13 pagesVery Update Information About MedicinetriNo ratings yet
- Acute Malnutrition - Roxas City 100214Document70 pagesAcute Malnutrition - Roxas City 100214Geline Joy D. SamillanoNo ratings yet
- Essentials for Practice of Medicine in the Frontline: From Tropical Africa; Pleasantly Different Volume 2From EverandEssentials for Practice of Medicine in the Frontline: From Tropical Africa; Pleasantly Different Volume 2No ratings yet
- Alzheimer Disease New TreatmentsDocument22 pagesAlzheimer Disease New TreatmentsDaniela BlancoNo ratings yet
- Nat Scie 2Document1 pageNat Scie 2Neenya SisonNo ratings yet
- Name: Baby Incredible Age/Sex: 4months, Male Date Issued: Dec. 10, 2010Document2 pagesName: Baby Incredible Age/Sex: 4months, Male Date Issued: Dec. 10, 2010Neenya SisonNo ratings yet
- Nursing Practice I - Foundation of Professional NursingDocument9 pagesNursing Practice I - Foundation of Professional NursingNeenya SisonNo ratings yet
- Eyes and EarsDocument7 pagesEyes and EarsNeenya SisonNo ratings yet
- Ipc 2018Document6 pagesIpc 2018abdullah sahibNo ratings yet
- Conjunctivitis (Inclusion) Vs Acute Bacterial ConjunctivitisDocument13 pagesConjunctivitis (Inclusion) Vs Acute Bacterial ConjunctivitisJayricDepalobosNo ratings yet
- Pediatric Case Studies of Bacterial ConjunctivitisDocument16 pagesPediatric Case Studies of Bacterial ConjunctivitisOana PaladeNo ratings yet
- BMIDocument20 pagesBMIMichael Dulza BaculantaNo ratings yet
- Fneur 12 800605Document15 pagesFneur 12 800605yasmine fadhilahNo ratings yet
- Counselling in HIV/AIDSDocument34 pagesCounselling in HIV/AIDSBhawna JoshiNo ratings yet
- The Top 10 Most Common Chronic Diseases For Older AdultsDocument9 pagesThe Top 10 Most Common Chronic Diseases For Older AdultstessahurintNo ratings yet
- TESDA COVID-19 Test (Answer Keys)Document12 pagesTESDA COVID-19 Test (Answer Keys)ash mizushiNo ratings yet
- Exam Patient Safety AwarenessDocument5 pagesExam Patient Safety AwarenessidzniNo ratings yet
- Prenatal Care: Dr. Ruby E Robiso, Fpogs Davao Medical School Foundation, IncDocument33 pagesPrenatal Care: Dr. Ruby E Robiso, Fpogs Davao Medical School Foundation, IncISFAHAN MASULOTNo ratings yet
- Aspectos SocialesDocument4 pagesAspectos SocialesGuru RachellNo ratings yet
- Dengue Hero-PcpDocument27 pagesDengue Hero-PcpRomina Mae FajardoNo ratings yet
- Callo, John Andrei D. (Regarding Kronos)Document3 pagesCallo, John Andrei D. (Regarding Kronos)andrei CalloNo ratings yet
- The Oral-Systemic Disease Connection PDFDocument2 pagesThe Oral-Systemic Disease Connection PDFJing XueNo ratings yet
- Roadside Urination and Public Sanitation Facilities in Dhaka, BangladeshDocument10 pagesRoadside Urination and Public Sanitation Facilities in Dhaka, BangladeshSimanta Kumar SahaNo ratings yet
- Rujukan: Kempen Cara Hidup Sihat 1997. Kementerian Kesihatan MalaysiaDocument1 pageRujukan: Kempen Cara Hidup Sihat 1997. Kementerian Kesihatan MalaysiaArif MuhdNo ratings yet
- Factors associated with urinary tract infections in pregnant women at Hermilio Valdizán Hospital in HuánucoDocument6 pagesFactors associated with urinary tract infections in pregnant women at Hermilio Valdizán Hospital in HuánucoJavier Narvaez SotoNo ratings yet
- FNCPDocument2 pagesFNCPJaylove CastilloNo ratings yet
- Factors Associated with Stunting in Indonesian ChildrenDocument13 pagesFactors Associated with Stunting in Indonesian ChildrenNie AfnyNo ratings yet
- NCP CervicalDocument4 pagesNCP CervicalZaira Kim93% (14)
- Efficacy of The anti-VZV (anti-HSV3) Vaccine in HSV1 and HSV2 Recurrent Herpes Simplex Disease: A Prospective StudyDocument8 pagesEfficacy of The anti-VZV (anti-HSV3) Vaccine in HSV1 and HSV2 Recurrent Herpes Simplex Disease: A Prospective StudymostafaNo ratings yet
- This Study Resource Was: MN577 Unit 5 AssignmentDocument3 pagesThis Study Resource Was: MN577 Unit 5 AssignmentHugsNo ratings yet
- Viruses: Serge Stroobandt and Roland StroobandtDocument3 pagesViruses: Serge Stroobandt and Roland StroobandtPuskesmas selongNo ratings yet
- Strokescenarioinindia Isp 170727022013Document10 pagesStrokescenarioinindia Isp 170727022013Ajjugal SushmajaNo ratings yet
- Washing-Hands SOPDocument3 pagesWashing-Hands SOPNahian SarthakNo ratings yet
- Evidence-Based Medicine: Lucman, Hakeymah Lunag, Tara Jane Magaoay, CheyserineDocument71 pagesEvidence-Based Medicine: Lucman, Hakeymah Lunag, Tara Jane Magaoay, CheyserinereadmeamllionNo ratings yet
- Criminal' - Confidential EU Documents Reveal Thousands of Deaths From Pfizer-BioNTech Shots - Children's Health DefenseDocument27 pagesCriminal' - Confidential EU Documents Reveal Thousands of Deaths From Pfizer-BioNTech Shots - Children's Health DefenseGabriel KeresztélyNo ratings yet
- Infant and Child Nutrition: Key PointsDocument4 pagesInfant and Child Nutrition: Key PointsseptiNo ratings yet
- Menstrual Hygiene Industry in India October 2023Document36 pagesMenstrual Hygiene Industry in India October 2023Avinash GuptaNo ratings yet
- JSA-055 Hydro-TestDocument24 pagesJSA-055 Hydro-TestOmar Dhieb100% (7)