Professional Documents
Culture Documents
Peak Flow Meter
Uploaded by
tetiCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Peak Flow Meter
Uploaded by
tetiCopyright:
Available Formats
Review Article
The peak flow meter and its use
in clinical practice
B O Adeniyi and G E Erhabor
Introduction parallel with the channel. Each indicator presents to view,
Bronchial asthma is a disease that causes significant two visually distinguishable areas defining a boundary
morbidity and mortality. It is projected to increase at an that can be set at a point along the path of the pointer
alarming rate with an estimated prevalence of 400million to indicate limit positions relating to lung function. This
by the year 2025, as contrasted to 300million at present. indicates to the user when to take remedial action.
Monitoring this disease involves both subjective and
objective modalities. The peak flow meter is the one of Types of peak flow meters
the means of objectively assessing and monitoring the There are several brands of peak flow meters available
airway function of the patient with bronchial asthma. which all perform the same function. However, there
It has been said that the peak flow meter is to the are two major types: the low-range peak flow meter
asthmatics, what the sphygmomanometer is to the hy- for small children between 4 and 9 years of age, and
pertensive. Most clinicians are, however, not skilled in for adults with severely impaired lung function; and
the use of this simple instrument and its in partnership the standard-range peak flow meter for older children,
with the asthmatic, to develop a personalised asthma teenagers, and adults.
management plan in order to achieve effective control. It is important that the doctor or healthcare provider
This article thus seeks to highlight the importance of the prescribes the appropriate device for each individual.
peak flow meter and its use in clinical practice. Adults have larger airways than children. If given a
A peak flow meter is a small hand-held device that low-range peak flow meter, they will continually have
measures how fast a person can blow air out of the maximum peak flow rates even when having severe short-
lungs when there is forceful exhalation, after maximum ness of breath. This may jeopardise proper management;
inhalation. This measurement is called the peak expira- they therefore need the much larger standard range.
tory flow (PEF). The peak flow meter helps to assess the
airflow through the airways and thus help to determine What is a normal peak flow rate?
the degree of obstruction along them. Normal peak flow rates vary according to age, height,
The measurement of PEF was pioneered by Dr Martin and sex. However, a patients normal score should
Wright who produced the first meter specifically designed be within 20% of a person of the same age, sex, and
to measure this index of lung function. Since the original height who does not have asthma. There are published
design was introduced in the late 1950s, and the subse- standardised normal values which were calculated by
quent development of a more portable, lower-cost version comparing asthmatics
(the Mini-Wright peak flow meter), other designs and with a set of age- and
copies have become available across the world. Brands sex-matched controls.
of electronic peak flow meters are also being marketed. The normal peak
flow or personal best
Description is the highest consistent Measuring
A peak flow meter (Figure 1) consists of a housing which peak flow reading over scale
has within it a channel along which a pointer is movable a 2 3-week period when
to a distance dependent on the lung function of the pa- the patient does not have Cursor
tient using the meter. Positioned adjacent to the channel, asthma symptoms. It
are two or more indicators which move along an axis serves as a standard
against which other
Dr B O Adeniyi, Consultant Physician (Respiratory) readings are meas-
Federal Medical Centre, Owo, Ondo State, Nigeria; and ured. By checking the
Professor G E Erhabor, Consultant Chest Physician and Mouthpiece
patients personal best
Professor of Medicine, Obafemi Awolowo University,
Ile-Ife, Nigeria, and when he does not have
President of the Nigerian Thoracic Society. symptoms, changes
Correspondence to Dr B O Adeniyi. can be recognised and
Email: delbis2003@yahoo.com reduced PEF can be Figure 1 A peak flow meter
March 2011 African Journal of Respiratory Medicine 5
Review Article
Exercise testing
Exercise is known to induce bronchospasm in over 80%
of asthma patients. Exercise challenge has been in use
for several years in the diagnosis of asthma, especially in
children. The standard technique is to exercise the asthma
patient for about 68 minutes on a treadmill, or in some
cases free running on an open field; a fall of PEFrate
greater than 15% is indicative of asthma (see Figure 3).
Peak expiratory flow rate (l/min)
600
500
400
300
200
100
Time (min)
Figure 2 Normal values for PEF (EN 13826 or EU scale)
0
monitored. In addition, when the PEF remains at a high- * 0 5 10 15 20 25
level, it helps to reassure the individual that the asthma
is under control. Pre-exercise Post-exercise
It is good to note that every asthma patients personal
Figure 3 Exercise testing showing a 40% decrease in
best or normal PEF is unique to them. It is the duty of PEF after 15 minutes of exercise
the physician to assist the patient to determine what
their personal best is. Figure 2 shows an example of a Occupational asthma
nomogram which can assist in estimating the best peak Demonstration of work-related asthma can be done
flow reading of the subject. by frequent readings of the peak flow every 2 hours
throughout the day or when the patient is awake, for
Clinical use of the peak flow meter about 4 weeks. However, a reasonable diagnosis can be
Diagnosis of asthma made by having patients record their peak flow reading
Variability
One of the hallmarks of asthma is varia-
tion in airflow obstruction. Considerable
variations in PEF over short periods can be
recorded by measuring the peak flow twice
daily preferably mornings and evenings.
Patients with asthma often show diurnal
variation with readings falling sharply in
the night or early mornings, the so-called
early morning dips. Variation of at least
15% of established maximum is assumed
to be indicative of asthma.
Bronchodilator response
Another characteristic of asthma is revers-
ibility with inhaled bronchodilators. If the
patient inhales a shortacting b2 agonist
such as salbutamol, terbutaline sulfate, or
anticholinergics, a bronchodilator response
greater than 15% in PEF is indicative of Figure 4 Peak flow meter reading of a foam worker with
asthma. occupational asthma from toluene diisocyanate (TDI)
6 African Journal of Respiratory Medicine March 2011
Review Article
three or four times daily, preferably before the first shift, evening for at least 2 weeks and thus know his estimated
after a break, at the end of a shift, and before reporting best PEF values.
for work the next day. In occupational asthma there is a Usually the traffic light colour code is used. Figure 5
progressive fall in peak flow rates over several days and summarises what each code indicates and the required
failure to return fully to normal. There is also progressive action by the patient.
recovery on work cessation over several days, with or
without medication (see Figure 4). How to use the peak flow meter
The patient must be well instructed and if possibe have
Monitoring disease progress a practical demonstration so as to get the correct read-
The peak flow measurement can be used to decide the ing. Table 1 highlights the steps involved in using the
suitability of patients for discharge after an acute severe peak flow meter.
attack. Large dips in readings are an indication that their Table 1 How to use the peak flow meter
asthma is not yet under control, and calls for continued
modification of therapy. The diurnal variation should 1. Set the cursor to zero. NB Do not touch the cursor
also be less than 25%. Patients should be discharged if when breathing out.
their PEFR has returned to normal or at least 75% of the 2. Stand up and hold the peak flow meter horizontally
predicted or best value. in front of the mouth.
3. Take a deep breath in and close the lips firmly
Self-management plan around the mouthpiece, making sure there is no
Asthma is an unpredictable disease, and this is espe- air leak around the lips.
cially so with those whose asthma is severe or unstable. 4. Breathe out as hard and as fast as possible.
These patients are better managed with an asthma self- 5. Note the number indicated by the cursor.
management plan using a diary and a peak flow meter. 6. Return cursor to zero and repeat this sequence
A simple plan is to stick coloured tape on the peak flow twice more, thus obtaining three readings.
meter to correspond to agreed zones or levels, with spe- The highest or best reading of all three measurements
cific instruction of what to do at each level. Before the is the peak flow at that time. The highest reading
asthma patient can use this guide, he/she would have should be recorded in the patients daily asthma diary
recorded his peak flow reading consistently morning and or recorded on a peak flow chart. To ensure results
of the peak flow meter are comparable, the patient is
Green zone: The peak flow reading is between advised to use the meter in the same way each time
80100% of the patients personal best. This is the and at the same time each day.
all-clear zone. There are no symptoms, he can
do normal activities and have a sound sleep. He How to chart the peak flow readings
should continue his usual treatments (bronchodilators The peak flow rates should be recorded on a peak flow
when needed with or without regular inhaled seroids. chart. The patient is required to chart the highest of
three readings. This is the best for the period. A typical
Yellow zone: Peak flow reading is between 50 chart has dates with AM and PM, a left margin with a
79% of patients personal best. This is the caution scale starting from 0l/min at the bottom and ending
zone. Asthma may be getting wrose. The patient with 600l/min at the top. It should also contain space at
may be coughing, wheezing, sleeping poorly, or the bottom to record symptoms, possible triggers, and
having restricted activities. He should take action to medications used. Figure 6 is an example of a peak flow
gain control and needs to adjust his medications, as chart showing the progression in the peak flow rates of
recommended by the doctor. an asthmatic before and after treatment.
Red zone: Peak flow reading is less than 50% of When to use the peak flow meter
the patients best. This is an asthma emergency! A peak flow meter should be used regularly to moni-
Patients may be coughing, dyspnoeic and having tor asthma control. It is also a valuable tool to monitor
sleep disturbances with frequent awakenings in the effectiveness of short-term bronchodilators (rescue
one night and most nights. He may be unable to com- medications) during an acute episode of asthma. It is
plete sentences in one breath. The patient is advised to therefore recommended for use:
take a reliever medication such as the short-acting b-2 every morning before the patient takes his asthma
agonist medication and start an oral dose of steroids. medications and in the evenings. It is preferable to
He should call the doctor or go to hospital immediately use the peak flow meter at the same time every day
if these symptoms persist or he develops blue lips or and record symptoms;
fingers, or if the peak flow is still in the Red Zone 30 when having asthma symptoms that either wake the
minutes later. patient at night or are increased during the day, or
Figure 5 An example of a self-management plan for asthma when the patient needs rescue medication;
March 2011 African Journal of Respiratory Medicine 7
Review Article
during an attack of asthma;
after taking medication for
an asthma attack.
as recommended by the
health practitioner.
What are the advantages
of a peak flow meter?
The peak flow meter is useful
in that it is small, inexpen-
sive, easy to use, portable,
and hand-held, and does not
need to be plugged in. Once a
patient has been taught how
to use it he does not need
supervision.
It is useful for diagnosing
asthma.
It helps to monitor the
progress of disease, and is
useful in self-management
of asthma. When properly
used it can recognise early
changes and reveal narrow-
Figure 6 An example of a peak flow chart
ing of the airways well in
advance (hours or even days) doctor before obtaining a peak flow meter, this will ensure
of an asthma attack. This helps the patient to take his that he is getting the right type and the physician will
rescue medications and pre-empt an attack. be able to give step-by-step instructions on how to use
It enables the asthma patient to measure the day-to- the device for maximum effect.
day variation in his breathing accurately. It is good to know that measuring the peak flow is
It helps to identify what is going on in the lungs rather just one step in gaining control of asthma. It should
than guessing by how the patient feels. not be a substitute for regular medical care and clinic
It shows the effectiveness of the asthma medication visits. The patient must work in partnership with his
and management plan. physician to develop an effective self-management plan,
It keeps a record of how the patients have been between learn to avoid his asthma triggers and use his asthma
clinic attendance. medication as prescribed. It is pertinent, therefore, for
It helps the doctor know when to adjust, add to, reduce, the physician to be familiar with the peak flow meter
or stop asthma medications. and its appropriate use.
It could help the patient learn what triggers his asthma.
Further reading
Global strategy for asthma management and prevention (updated
Limitations of a peak flow meter 2009): Global Initiative for Asthma (GINA). URL:http://www.
ginasthma.org; 2009.
The peak flow meter has some limitations. Results are Sawyer G, Miles J, Lewis S, et al. Classification of asthma severity:
sometimes not reproducible over a long period and there should the international guidelines be changed? Clin Ex Allergy
may be inter-model variation in the values of readings 1998; 28(12): 156570.
Erhabor GE. Pulmonary function tests: spirometry and peak
obtained. It is also effort dependent. It primarily assesses flow in clinical practice. Waltodany Publishing Press, 2010.
the airflow in the larger airways and not in the medium Eid N, Yandell B, Howell L, Eddy M, Sheikh S. Can peak expira-
and smaller airways and thus can underestimate the tory flow predict airflow obstruction in children with asthma?
Paediatrics 2000; 105(2): 3548.
degree of airflow limitation, particularly as airflow Reddel HK, Marks GB, Jenkins CR. When can personal best
limitation and gas trapping worsen. peak flow be determined for asthma action plans? Thorax 2004;
It is good to note that measurement of PEF is not inter- 59(11): 9224.
Reddel HK, Salome CM, Peat JK, Woolcock AJ. Which index of
changeable with other measurements of lung function peak expiratory flow is most useful in the management of stable
such as FEV1 (forced expiratory volume in 1 second). asthma? Am J Respir Crit Care Med 1995; 151(5): 13205.
Dekker FW, Schrier AC, Sterk PJ, Dijkman JH. Validity of peak
expiratory flow measurement in assessing reversibility of airflow
Conclusion obstruction. Thorax 1992; 47(3): 1626.
Peak flow meters are available in medical equipment Boezen HM, Schouten JP, Postma DS, Rijcken B. Distribution
of peak expiratory flow variability by age, gender and smoking
and drug stores worldwide and can be acquired without habits in a random population sample aged 20-70 yrs. Eur Respir
prescription. It is advisable for the patient to consult his J 1994; 7(10): 181420.
8 African Journal of Respiratory Medicine March 2011
You might also like
- 2023 - MHA-MABHS State Agency Involved Pediatric Patients - FinalDocument11 pages2023 - MHA-MABHS State Agency Involved Pediatric Patients - FinalBoston 25 DeskNo ratings yet
- Medicare Correct Coding GD PDFDocument58 pagesMedicare Correct Coding GD PDFvrushgangNo ratings yet
- Admission, Transfer, and DischargeDocument28 pagesAdmission, Transfer, and DischargeydtrgnNo ratings yet
- Vasopressors and Inotropes in ShockDocument8 pagesVasopressors and Inotropes in ShockRiska PashaNo ratings yet
- Benign Prostatic HyperplasiaDocument18 pagesBenign Prostatic HyperplasiaGunawan SadewoNo ratings yet
- A Simple Guide to Circulatory Shock, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Circulatory Shock, Diagnosis, Treatment and Related ConditionsNo ratings yet
- Ich-Gcp & Schedule yDocument38 pagesIch-Gcp & Schedule ySahiti PendyalaNo ratings yet
- Nov 2017 Infantile Spasms WebinarDocument22 pagesNov 2017 Infantile Spasms WebinartetiNo ratings yet
- Functional Dyspepsia in ChildrenDocument13 pagesFunctional Dyspepsia in ChildrenTimothy Eduard A. SupitNo ratings yet
- Z Score Girls PDFDocument15 pagesZ Score Girls PDFDio Pratama0% (1)
- Continuing Education in Nursing - EditedDocument7 pagesContinuing Education in Nursing - EditedOnkwani DavidNo ratings yet
- Management of Status Asthmatic Us in ChildrenDocument7 pagesManagement of Status Asthmatic Us in Childrenjshq1971No ratings yet
- Managing Mechanical VentilationDocument7 pagesManaging Mechanical VentilationArden QuiambaoNo ratings yet
- Pulmonary Physiology of The NewbornDocument39 pagesPulmonary Physiology of The NewbornADNo ratings yet
- Critical Appraisal for Therapy ArticlesDocument4 pagesCritical Appraisal for Therapy ArticlesMahardhika AcintyaNo ratings yet
- Code of Professional Conduct and EthicsDocument36 pagesCode of Professional Conduct and EthicsAgnieszka Waligóra100% (1)
- An Introduction To Evidence-Based NursinDocument8 pagesAn Introduction To Evidence-Based NursinAli MaqsudiNo ratings yet
- Ventilator, Weaning, SuctioningDocument81 pagesVentilator, Weaning, SuctioningwaqarNo ratings yet
- Icu Initial Ventilator SettingsDocument40 pagesIcu Initial Ventilator SettingsantreaspetsasNo ratings yet
- Acute Respiratory Distress Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandAcute Respiratory Distress Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Reading and Vocabulary Proficiency As Predictors of Productive Language Skills of College of Teacher Education StudentsDocument4 pagesReading and Vocabulary Proficiency As Predictors of Productive Language Skills of College of Teacher Education StudentsAcademiPHNo ratings yet
- Suctioning Artificial Airways - AdultsDocument27 pagesSuctioning Artificial Airways - AdultssdaNo ratings yet
- Epid COPDDocument9 pagesEpid COPDAgung WistaraNo ratings yet
- Effects of HypoxiaDocument6 pagesEffects of HypoxiaMaria TelloNo ratings yet
- Management of Vacuum Assisted Closure TherapyDocument14 pagesManagement of Vacuum Assisted Closure TherapyVoiculescu MihaelaNo ratings yet
- Top 10 Care Essentials in Ventilated PtsDocument3 pagesTop 10 Care Essentials in Ventilated PtsAdel HamadaNo ratings yet
- Presus Interactive Lecture Handout - September 2015Document4 pagesPresus Interactive Lecture Handout - September 2015api-317814049No ratings yet
- Ventricular Septal DefectDocument9 pagesVentricular Septal DefectpepotchNo ratings yet
- Pediatric Fluid and Electrolyte TherapyDocument8 pagesPediatric Fluid and Electrolyte TherapyWildan Wisnu WardayaNo ratings yet
- Anaesthesia For Patients With COPD: University College of Medical Sciences & GTB Hospital, DelhiDocument76 pagesAnaesthesia For Patients With COPD: University College of Medical Sciences & GTB Hospital, DelhiRINI100% (1)
- Mechanical Ventilation Dyssynchrony Types and ManagementDocument17 pagesMechanical Ventilation Dyssynchrony Types and ManagementjuanNo ratings yet
- Use of Vasopressors and InotropesDocument14 pagesUse of Vasopressors and InotropesEdwin VargasNo ratings yet
- Aerosoltherapy Nebu 120503115712 Phpapp01Document65 pagesAerosoltherapy Nebu 120503115712 Phpapp01Aan Ika SugathotNo ratings yet
- Advanced Practice NursingDocument11 pagesAdvanced Practice NursingSaher Kamal100% (2)
- Standardized Nursing Terminology AssignmentDocument6 pagesStandardized Nursing Terminology Assignmentapi-3284480220% (1)
- 2020 Neonata Lcare PDFDocument20 pages2020 Neonata Lcare PDFserigne badianeNo ratings yet
- Basic Principles of Pediatric Mechanical VentilationDocument39 pagesBasic Principles of Pediatric Mechanical VentilationNav KovNo ratings yet
- Thesis (Noridja's Group)Document31 pagesThesis (Noridja's Group)DenMarkSolivenMacniNo ratings yet
- The WHO Health Promotion Glossary PDFDocument17 pagesThe WHO Health Promotion Glossary PDFfirda FibrilaNo ratings yet
- Respiratory Failure Nursing Care and ManagementDocument19 pagesRespiratory Failure Nursing Care and ManagementYudionoNo ratings yet
- Quality of Nursing DocomentationDocument19 pagesQuality of Nursing DocomentationEKA TRISNAWATINo ratings yet
- Lec 2, Congenital Heart DiseasesDocument61 pagesLec 2, Congenital Heart DiseasesAlexandrescuNo ratings yet
- Chest Pain: Jean J. Chatham, MDDocument40 pagesChest Pain: Jean J. Chatham, MDYermia RashaquatNo ratings yet
- Patient Safety and Quality Care MovementDocument9 pagesPatient Safety and Quality Care Movementapi-300362983No ratings yet
- Vital Sign Instr 2-10Document51 pagesVital Sign Instr 2-10Katrina AzeezNo ratings yet
- Final EssayDocument9 pagesFinal Essayapi-383024083No ratings yet
- Admitting A Patient To The Hospital PDFDocument40 pagesAdmitting A Patient To The Hospital PDFMarc Imhotep Cray, M.D.No ratings yet
- Using Growth Charts to Monitor Child NutritionDocument13 pagesUsing Growth Charts to Monitor Child Nutritionp1843dNo ratings yet
- Drug Compliance Among Hypertensive PatientsDocument5 pagesDrug Compliance Among Hypertensive PatientsSyifa MunawarahNo ratings yet
- Diagnosis and Treatment of Otitis Media in ChildrenDocument19 pagesDiagnosis and Treatment of Otitis Media in ChildrenreyhanrrNo ratings yet
- Jurnal 1 SBAR PDFDocument10 pagesJurnal 1 SBAR PDFIRFA KHIKMATUL KHULUQNo ratings yet
- Status EpilepticusDocument70 pagesStatus Epilepticusfloppyfishh100% (1)
- Managing Angina: AHA Guidelines on Diagnosis and TreatmentDocument96 pagesManaging Angina: AHA Guidelines on Diagnosis and TreatmentJaymica Laggui DacquilNo ratings yet
- Basics Principle and Guidelines To Neonatal VentilationDocument5 pagesBasics Principle and Guidelines To Neonatal VentilationMaria Babette Almazan TalaveraNo ratings yet
- ABG AnalysisDocument7 pagesABG Analysissneha100% (1)
- Asthma Information HandbookDocument50 pagesAsthma Information Handbookahmad kajNo ratings yet
- Mechanical Ventilation TherapyDocument17 pagesMechanical Ventilation TherapyFaizal FlNo ratings yet
- Community Health Paper IIDocument19 pagesCommunity Health Paper IIapi-444056287No ratings yet
- Intravenous InsulinDocument4 pagesIntravenous Insulingiseladelarosa2006No ratings yet
- How Nurses Can Effectively Delegate TasksDocument28 pagesHow Nurses Can Effectively Delegate Tasksahmad rizalNo ratings yet
- Mechanical Ventilation: Standard Weaning Criteria (Respiratory Therapy)Document6 pagesMechanical Ventilation: Standard Weaning Criteria (Respiratory Therapy)S3DOSHA osmanNo ratings yet
- Whitten - 2011 - Case Study - Reduced BiPAP Days - PM-185047373 - A PDFDocument3 pagesWhitten - 2011 - Case Study - Reduced BiPAP Days - PM-185047373 - A PDFdragon66No ratings yet
- Pediatric Respiratory Problems and VentilationDocument4 pagesPediatric Respiratory Problems and VentilationPaul Saquido CapiliNo ratings yet
- Sample Assignment of Nursing LeadershipDocument5 pagesSample Assignment of Nursing LeadershipPrasiddha Parajuli100% (1)
- 21321Document56 pages21321Daniel TabalanzaNo ratings yet
- Intramuscular HemagiomaDocument7 pagesIntramuscular HemagiomatetiNo ratings yet
- Angiolipoma 3Document3 pagesAngiolipoma 3tetiNo ratings yet
- Annals of Neurology Volume 79 Issue 3 2016 (Doi 10.1002/ana.24594) Knupp, Kelly G. Coryell, Jason Nickels, Katherine C. Ryan, Ni - Response To Treatment in A Prospective National Infantile SpasmDocument10 pagesAnnals of Neurology Volume 79 Issue 3 2016 (Doi 10.1002/ana.24594) Knupp, Kelly G. Coryell, Jason Nickels, Katherine C. Ryan, Ni - Response To Treatment in A Prospective National Infantile SpasmtetiNo ratings yet
- 2016 Rickets Consensus HRP PDFDocument24 pages2016 Rickets Consensus HRP PDFtetiNo ratings yet
- Grafik CDCDocument10 pagesGrafik CDCArief Budi LesmanaNo ratings yet
- Fluid Balance in Critically Ill Children With Acute Lung Injury PDFDocument16 pagesFluid Balance in Critically Ill Children With Acute Lung Injury PDFtetiNo ratings yet
- Contoh Jurnal HematoDocument8 pagesContoh Jurnal HematotetiNo ratings yet
- Benchmark OET Writing Case Notes - Naomski Family HealthDocument2 pagesBenchmark OET Writing Case Notes - Naomski Family HealthGourish MNo ratings yet
- Corrected NCP Case 3 Intrapartum NCPDocument2 pagesCorrected NCP Case 3 Intrapartum NCPReyzel PahunaoNo ratings yet
- Price List Last Update 26-06-2023Document565 pagesPrice List Last Update 26-06-2023Sowrya Tej SunkaraNo ratings yet
- NSLHD Policy Procedure Guideline Communique 14 Oct 2019Document3 pagesNSLHD Policy Procedure Guideline Communique 14 Oct 2019Andrew WongNo ratings yet
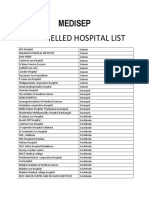
- Empanelled Hospital ListDocument7 pagesEmpanelled Hospital ListExpress WebNo ratings yet
- Entire Infection Control Manual PDFDocument252 pagesEntire Infection Control Manual PDFAbidi HichemNo ratings yet
- Cardiotocography Trace Pattern Evaluation Using MATLAB ProgramDocument6 pagesCardiotocography Trace Pattern Evaluation Using MATLAB ProgramdianaNo ratings yet
- SAP EHS - Occupational Health - EHS-HEA - V1.1 PDFDocument87 pagesSAP EHS - Occupational Health - EHS-HEA - V1.1 PDFMukesh ChauhanNo ratings yet
- The Mechanism of Notifying and Record Keeping Three Forms Are Used For Notifying and Record KeepingDocument6 pagesThe Mechanism of Notifying and Record Keeping Three Forms Are Used For Notifying and Record KeepingRoger FernandezNo ratings yet
- Revised Nursing College Webinar CalenderDocument1 pageRevised Nursing College Webinar CalenderMahida RanjitNo ratings yet
- Record Storage SafekeepingDocument3 pagesRecord Storage Safekeepingilog ndpNo ratings yet
- Reproductive Health Services For Syrian Refugees in Zaatri Refugee Camp and Irbid City, Jordan PDFDocument122 pagesReproductive Health Services For Syrian Refugees in Zaatri Refugee Camp and Irbid City, Jordan PDFmeNo ratings yet
- Form DH2 - Monthly ASHA Performance (For District)Document3 pagesForm DH2 - Monthly ASHA Performance (For District)vinodaksNo ratings yet
- FPA India-Madurai Branch Provides Reproductive Health ServicesDocument12 pagesFPA India-Madurai Branch Provides Reproductive Health ServicesValarmathiNo ratings yet
- Jama Carson 2023 SC 230002 1696973901.0012-1Document11 pagesJama Carson 2023 SC 230002 1696973901.0012-1Luz Elena ValderramaNo ratings yet
- What Your Doctor Won't Disclose - Revisión Del IntentoDocument7 pagesWhat Your Doctor Won't Disclose - Revisión Del IntentoJosé Miguel Cayetano MárquezNo ratings yet
- Lab Requisition SampleDocument1 pageLab Requisition SampleUser SmuggNo ratings yet
- Head Nurse For MinetteDocument1 pageHead Nurse For MinetteMiggy SikatNo ratings yet
- Chapter 6 DiscussionDocument3 pagesChapter 6 DiscussionyughaNo ratings yet
- Engleza Sinonime An 2Document18 pagesEngleza Sinonime An 2Andrei RadulescuNo ratings yet
- Compliance With Thromboprophylaxis After Gynecology SurgeryDocument10 pagesCompliance With Thromboprophylaxis After Gynecology SurgeryShahla AlalafNo ratings yet
- Step by Step Governance Practices Assessment GuideDocument19 pagesStep by Step Governance Practices Assessment Guideadam MajbourNo ratings yet
- Principles of Nursing Services AdministrationDocument69 pagesPrinciples of Nursing Services AdministrationMack Chacha0% (1)
- Context Clues Guided Reading 4.1Document4 pagesContext Clues Guided Reading 4.1Dannah SteeleNo ratings yet
- Your Roadmap To Sibo Imo Recovery GuideDocument26 pagesYour Roadmap To Sibo Imo Recovery Guideps piasNo ratings yet