Professional Documents
Culture Documents
Head and Neck Assignment
Uploaded by
api-334402872Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Head and Neck Assignment
Uploaded by
api-334402872Copyright:
Available Formats
Seth Cox
DOS 531
2/26/2017
Head and Neck Assignment
Professor Vann
Group 5:Hypopharynx
Patient presented with malignant neoplasm of overlapping
sites of hypopharynx (T3N2bMO) squamous cell carcinoma
arising from the right hypopharynx.
After identifying a specific case answer the following questions:
1. How was this patient positioned? What positioning
devices/accessories were used, how and why? (5 points)
Patient was placed on the table in a head in supine position on a
neutral headrest. An aquaplast face and shoulder mask was made
to aide in patient immobilization and treatment reproducibility.
Patients arms were folded and resting on abdomen, red knee
sponge was placed under patients legs.
2. What specific avoidance structures were contoured? What
is their tolerance dose? (20 points)
Avoidance structures that were contoured included (Quantec and
RTOG protocol requirements):
Left and right brachial plexus 66 Gy max dose
Brain V12 Gy < 5-10 cc
Brain Stem 54 Gy max dose
Esophagus Mean dose less than 45 Gy
Left and right eyes Max dose less than 50 Gy
Glottic Larynx Mean dose less than 45 Gy
Larynx Mean < 44 Gy Max 63-66 Gy when risk of tumor is limited
Left and right lens Max dose 7 Gy
Lips Mean < 20 Gy for non-oral cavity
Mandible 70 Gy, if not possible then no more than 1 CC to exceed
75 Gy
Optic Chiasm 50 Gy max dose
Left and right Optic Nerve 50 Gy max dose
Oral Cavity Mean dose less than 40 Gy
Left and right Parotid Mean dose of < 26 Gy in at least one gland
or at least 20 CC of combined volume of both will receive < 20 Gy
or at least 50% of one gland will receive < 30 Gy
Spinal Cord 45 Gy max dose
3. What are the anatomical boundaries of the tumor
volume? You should use Radiotherap-e
(http://www.radiotherap-e.com) and other anatomy
references to help you describe this. You can use a
diagram and screen shots of your CT data to point out the
boundaries. (20 points)
With nodal involvement, patient will need to have level II-V and
retropharyngeal nodes treated. The superior border is the skull
base and the inferior border is 1cm below the inferior extent of
the disease. 1
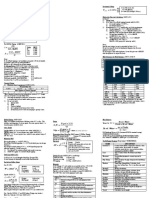
With the shape of the disease and treatment area, a 0.5cm
margin was put around the GTV (the red on the above picture)
giving us a PTV in green.
When including the nodes in the treatment field, the margin
changes:
The dark blue is our treatment area for the nodes within the
neck, as identified within RadioTherap-e while levels two and
three are the only nodal involvements found, we must treat to
level five nodes. 1
4. Are lymph nodes included in the treatment area? If so can
you identify the level nodes use a diagram and screen
shots to help you label the nodal regions treated. (20
points)
Yes, patient had nodal involved in right level II (upper jugular) and
level III (midjugular) nodes. Involvement was great, as the normal
fat plane between level II nodal group and sternocleidomastoid
muscle group was lost.2
5. What radiation technique is used to treat this patient?
Describe in detail the technique (35 points)
There are two high quality of arc based therapies, tomotherapy
and volumetric modulated arc therapy.3 99% of our treatments
for IMRT are done on our tomotherapy machine as it allows for
image guided radiation therapy, because it is best for with
surrounding normal tissue tolerance is lower than that of the
prescribed radiation dose for the tumor volume.4
Yet, it does not do a good job of allowing for an explanation of
beams, angles and collimators, so we created a plan on our
trilogy linac in order to create a greater understanding of the
needs and the techniques to properly treat this patient.
First, we utilized four 6x-IMRT beams, with four arcs, Two arcs
went in a clockwise motion, two arcs went in the counter-
clockwise rotation.
There were no couch rotations, but, there were gantry rotations
and collimator rotations we needed to use in order to get the
coverage needed and avoid the areas within the hypopharynx
and stay within our tolerance of organs to avoid. Going from 181
to 179 then 179 to 181 kept the beam going into the
hypopharynx region, while sparing the organs at risk. By keeping
the beams only moving from 179 to 181 and back you can
concentrate the treatment area to the front of the neck. By
using collimator rotations you can move your MLC leaves (block)
onto different structures to keep the beam from getting into
different organs.
Beam A had a gantry
rotation of 181 to
179, clockwise, with
a collimator rotation
of 20 degrees.
Beam B went counter
clockwise from 179-181
with a rotation of the
collimator to 340
degrees.
Beam C was another clockwise
gantry rotation from 181 to 179,
this time with a collimator rotation of
90 degrees.
The final beam was another
counter clockwise beam
from 179 to 181, also with a
90 degree collimator
rotation.
References:
1. Hansen EK, Roach M HANDBOOK OF EVIDENCE-BASED RADIATION
ONCOLOGY Springer 2007, http://www.radiotherap-e.com/#5004642,
Accessed 2/25/2017
2. Vann, Ann Marie. Hypopharynx [Softchalk]. La Crosse, WI: UW-LAX
medical Dosimerty Program; 2016
3. Teoh M, Clark CH, Wood K, Whitaker S, Nisbet A. Volumetric
modulated arc therapy: a review of current literature and clinical use in
practice. The British Journal of Radiology. 2011;84(1007):967-996.
doi:10.1259/bjr/22373346.
4. Gupta T, Narayan CA. Image-guided radiation therapy: Physicians
perspectives. Journal of Medical Physics / Association of Medical
Physicists of India. 2012;37(4):174-182. doi:10.4103/0971-
6203.103602.
You might also like
- Seth D Cox ResumDocument2 pagesSeth D Cox Resumapi-334402872No ratings yet
- Evals Fall CompleteDocument9 pagesEvals Fall Completeapi-334402872No ratings yet
- Clinic 1Document2 pagesClinic 1api-334402872No ratings yet
- Final DraftDocument18 pagesFinal Draftapi-334402872No ratings yet
- Final DraftDocument18 pagesFinal Draftapi-334402872No ratings yet
- H N ReportDocument24 pagesH N Reportapi-334402872No ratings yet
- Csi ReportDocument20 pagesCsi Reportapi-334402872No ratings yet
- Draft 2Document16 pagesDraft 2api-334402872No ratings yet
- 1st Semester EvalsDocument6 pages1st Semester Evalsapi-334402872No ratings yet
- Final DraftDocument15 pagesFinal Draftapi-334402872No ratings yet
- Draft 3Document18 pagesDraft 3api-334402872No ratings yet
- Clinic 1Document2 pagesClinic 1api-334402872No ratings yet
- Pelvis Lab Final 4-9Document10 pagesPelvis Lab Final 4-9api-334402872No ratings yet
- Draft 1Document15 pagesDraft 1api-334402872No ratings yet
- Lung Lab FinalDocument6 pagesLung Lab Finalapi-334402872No ratings yet
- Final Case StudyDocument13 pagesFinal Case Studyapi-334402872No ratings yet
- Photon 3d CompsDocument3 pagesPhoton 3d Compsapi-334402872No ratings yet
- Extra Credit QuestionsDocument6 pagesExtra Credit Questionsapi-334402872No ratings yet
- Head PPDocument9 pagesHead PPapi-299189797No ratings yet
- Heterogeneity FinalDocument9 pagesHeterogeneity Finalapi-334402872No ratings yet
- Radonc Compare ContrastDocument7 pagesRadonc Compare Contrastapi-334402872No ratings yet
- Head PPDocument9 pagesHead PPapi-299189797No ratings yet
- Ama Challenge 2015Document3 pagesAma Challenge 2015api-295549343No ratings yet
- Lung Lab FinalDocument6 pagesLung Lab Finalapi-334402872No ratings yet
- Statistics Activity 2012 1Document5 pagesStatistics Activity 2012 1api-203178352No ratings yet
- Head PPDocument9 pagesHead PPapi-299189797No ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- 200 300 Series Installation Guide USDocument48 pages200 300 Series Installation Guide USLhexter Mhervin CoNo ratings yet
- The Supply Chain For Electric Vehicle BatteriesDocument21 pagesThe Supply Chain For Electric Vehicle BatteriesProbonogoya Erawan Sastroredjo100% (2)
- Small ScienceDocument368 pagesSmall Sciencereach27No ratings yet
- Manual Direct Fired 160h Through 800h PN 54000 07-12-13 - 1Document53 pagesManual Direct Fired 160h Through 800h PN 54000 07-12-13 - 1Fer YamashitaNo ratings yet
- Drag LinesDocument31 pagesDrag LinesJonas GondimNo ratings yet
- Assignment On Computer HardwareDocument9 pagesAssignment On Computer HardwareMuktadirhasan100% (1)
- Shears Cysts of The Oral and Maxillofacial Regions, 5th Edition (Paul Speight)Document382 pagesShears Cysts of The Oral and Maxillofacial Regions, 5th Edition (Paul Speight)Miriam Tovar OgazonNo ratings yet
- Leadership Theory Application and Skill Development 5th Edition Lussier Test Bank 1Document36 pagesLeadership Theory Application and Skill Development 5th Edition Lussier Test Bank 1douglasbrownyipsmrgkob100% (29)
- Report of Mechanics of Machines 1Document12 pagesReport of Mechanics of Machines 1muhammaduzairNo ratings yet
- Business Operations Group AssignmentDocument7 pagesBusiness Operations Group Assignmentankit gangeleNo ratings yet
- English 4 Q2 Weeks 1-4Document36 pagesEnglish 4 Q2 Weeks 1-4Em AdrianoNo ratings yet
- Nissan Skyline RB Engine Oil Control ModsDocument1 pageNissan Skyline RB Engine Oil Control Modsbyrnesvictim100% (1)
- Tzu Chi Medical Journal: Xiao-Jun Lin, I-Mei Lin, Sheng-Yu FanDocument5 pagesTzu Chi Medical Journal: Xiao-Jun Lin, I-Mei Lin, Sheng-Yu Fanperisici4_535458722No ratings yet
- Virgin Mobile Insurance BookletDocument51 pagesVirgin Mobile Insurance BookletdanatheteacherNo ratings yet
- 51-11-15-001-Data Recording of Allowable Damage and Repairs-A320Document6 pages51-11-15-001-Data Recording of Allowable Damage and Repairs-A320FredNo ratings yet
- Adime NoteDocument2 pagesAdime Noteapi-384503305100% (1)
- Operation and Analysis of The Three Phase Fully Controlled Bridge ConverterDocument24 pagesOperation and Analysis of The Three Phase Fully Controlled Bridge Convertermohammed aliNo ratings yet
- Ttrack 514889Document24 pagesTtrack 514889Fernando Shadow100% (1)
- RFP Master PlanDocument9 pagesRFP Master PlanakhilchibberNo ratings yet
- Chapter 14: Understanding Clutches and Their Operating PrinciplesDocument39 pagesChapter 14: Understanding Clutches and Their Operating PrinciplespapipapiiNo ratings yet
- 06072G Chapter Sample PDFDocument11 pages06072G Chapter Sample PDFAnonymous 1hOgJqwZuzNo ratings yet
- Modeling Relationships in Scatter PlotsDocument45 pagesModeling Relationships in Scatter PlotsSiddarth Kalyan100% (1)
- Surge Arrester Function and Working PrinciplesDocument25 pagesSurge Arrester Function and Working PrinciplesMidhun Varghese100% (1)
- Outrider Character SheetDocument6 pagesOutrider Character SheetColin ZachauNo ratings yet
- Quick Reference CardDocument3 pagesQuick Reference Cardaslam.ambNo ratings yet
- Solah (Prayer in Islam)Document22 pagesSolah (Prayer in Islam)Anif Ilham IsmailNo ratings yet
- DMAE Powder Safety Data SheetDocument3 pagesDMAE Powder Safety Data SheetAInhoaNo ratings yet
- 842e In001 - en PDocument4 pages842e In001 - en PNilson Eduardo TorresNo ratings yet
- Pulp Digester FailuredDocument93 pagesPulp Digester FailuredTim Ku100% (1)
- Analytical Positivism of Glanville Williams and Ludwig WittgensteinDocument9 pagesAnalytical Positivism of Glanville Williams and Ludwig WittgensteinPrabhakaran KarthikeyanNo ratings yet