Professional Documents
Culture Documents
Cerebral Perfusion
Uploaded by
Patrick DycocoOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cerebral Perfusion
Uploaded by
Patrick DycocoCopyright:
Available Formats
NURSING CARE PLAN
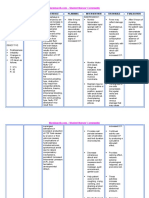
ASSESSMENT NURSING DIAGNOSIS RATIONALE OBJECTIVES NURSING INTERVENTIONS RATIONALE EVALUATION
Gen. Objective: Independent:
Objective Cues: 3. Risk for ineffective cerebral Edema & hematoma Promote or maintain 1. Assess neurologic status & A change in level of consciousness
craniectomy was perfusion related to edema formation causes effective cerebral vital signs frequently & compare is the first sign of an
performed for formation or bleeding after compression of nerves & perfusion. with baseline values. increasing intracranial pressure.
decompression craniectomy or due to blood vessels resulting to 2. Elevated head of bed to 30 Elevation facilitates venous
and evacuation hematoma formation. altered blood flow; these Specific Objectives: degrees. drainage and reduces edema.
of comminuted occupies normal tissue After the nursing 3. Maintain head & neck in This facilitates venous
fracture spaces leading to interventions have been neutral alignment. drainage and reduces edema.
a comminuted compression. employed, 4. Change position slowly. Rapid changes in position
fracture on the Compression alters blood flow the patient will: increase cerebral blood flow and
frontal area resulting to ischemia, and 1. Have an ICP of less pressure.
A drain has been necrosis may occur than 15 mmHg 5. Avoid a Valsalva maneuver. Straining during coughing,
held in place destroying major 2. Neurologic movement in bed, or moving
to promote blood functions. assessment and vital bowel increases ICP.
drainage and signs are at baseline 6. Monitor intake & output Excess fluids can promote edema
prevent possible values or improved. frequently. dehydration can decrease
hematoma 3. No manifestations of cerebral arterial flow.
formation increased ICP. 7. Suction airway as needed. Routine suctioning not
4. Body temperature advised because it stimulates
less than 38.5C. cough and increases ICP;
however, sputum plugs cause
retention of carbon dioxide and
need to be removed
because carbon dioxide
increase cerebral blood flow and
pressure.
8. Administer steroids as ordered. This reduces cerebral edema.
9. Administer anti - epileptic Seizures are a common
drug as ordered. sequelae of brain surgery.
10 Observe for signs of Hematoma formation causes
hematoma formation. compression to brain tissues
(dangerous complication of brain leading to ischemia and
surgery secondary to VA.) necrosis.
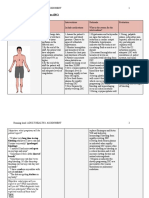
3. Patient will be able to 1. Assess the over all nutritional
But could be given by body requirements realted to very essential since we can't demonstrate progress- status of the client by checking her previous data.
cotton water. inability to ingest/ digest food or survive without the two. ive weight gain toward daily weights, tissue integrity
absorb nutrients; N & V, NPO Gradual decrease of food goal with normalization & presence of adequate body fat
O: Patient is weak, status & nasogastric suctioning & intake would lead to body of laboratory values; and muscle mass.
restless, pallor, loss of appetite as evidenced by failure. Demonstrate behaviors, 2. Encourage client to choose To stimulate appetite.
showing expressions reported inadequate food intake lifestyle changes to foods that are appealing.
of difficulty with her less than RDA, lack of interest in regain and or maintain 3. Avoid foods that causes So as not to cause intestinal
situation. food "waray gana pagkaon,"/ appropriate weight. intolerances/ gastric motility problems.
aversion to eating & perceived (gas - forming foods, hot & spicy)
inability to digest food. 4. Limit fiber/ bulk. Since they can lead to early
satiety.
5. Promote pleasant, relaxing To stimulate proper appetite/
environment. enhance intake.
6. Limiting fluids hours prior to So as not to cause early
meal satiety.
7. Weigh weekly & prn. To monitor effectiveness of
care.
DISCHARGE PLANNING:
1. Emphasize importance of well
balance, nutritious intake.
2. Provide info regarding
individual needs & ways to meet
these needs within financial
constraints.
4. RISK for infection related to Body weakness would 4. Achieve timely 1. Demonstrate lifestyle changes For personal growth of the
inadequately primary defenses further lead to infections. healing. Be free of signs to promote safe environment. person.
(weak body), altered peristalsis, of infection 2. Cleanse insertion sites daily & To prevent sepsis.
change in pH secretions, Be afebrile. prn with solution.
nutritional deficiencies & stasis of 3. Encourage early ambulation, For mobilization of gastric
body fluids; chronic diseases, deep breathing, coughing, secretions.
position changes.
DISCHARGE PLANNING:
1. Explain the importance of proper
hygiene especially hand washing.
5. Ineffective breathing pattern Normal range of value for 5. The client will maintain 1. Maintain calm attitude, while To as to maintain and improve
O: RR 30 bpm. related to abdominal pain/ RR is 15 - 20 bpm. an effective breathing dealing with client to limit anxiety. rapport.
Patient having deep,tenderness as evidenced by RR 30 pattern as evidenced by 2. Assist client in use of relaxation So as to relax the client from
shallow, irregular bpm, anxiety/ decreased energy, RR within normal limits, techniques. the tension and anxiety she is
breathing. fatigue. relaxed respiratory effort suffering.
Demonstrate approp.
coping behaviors.
S: Patient uttered, 6. Anxiety related to change in Anxiety is a vague feeling 6. The client will express 1. Assess the client's level of To determine what interventions
"Tangala na ini na health status, change in of apprehension as to what and demonstrate anxiety by listening and observing. are suitable for the client.
adi tak may irong." environment, fear of pain returning will happen next. It is a normal decreasing 2. Reassure the client and To let the client feel secured,
& irritation brought about by the defense mechanism of the manifestations of acknowledge that the unknown is that she is not alone.
O: Fatigue, touchi NGT tube attached. body. anxiety as evidenced of frightening.
the NGT tube which displaying behavior 3. Allow significant others to
she wants to be associated with remain with the client.
removed. relaxation.
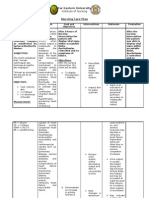
NAME: ROOM & BED #:
AGE/SEX: WARD:
CHIEF COMPLAINT: ATTENDING PHYSICIAN:
Prepared by: Submitted to:
DONN ED MARTIN A. ABRIL MR. ROBERT PONTIAN AGNER, R.N.
RTRMF - CN Student Nurse Clinical Instructor
EVRMC
15-Nov-05
You might also like
- Pendulum DowsingDocument29 pagesPendulum Dowsingraykct100% (5)
- Tutorial Wedge Shoe Cake by Sugar & Spice CakesDocument51 pagesTutorial Wedge Shoe Cake by Sugar & Spice Cakesacdnadmin75% (4)
- Brain Edema & It's ManagementDocument26 pagesBrain Edema & It's ManagementMohammed FareedNo ratings yet
- Blood Supply of Head and NeckDocument44 pagesBlood Supply of Head and NeckPatrick DycocoNo ratings yet
- Review of SystemsDocument2 pagesReview of SystemsPatrick DycocoNo ratings yet
- Cebu City Ordinance No. 2486 Cebu City Market OrdinanceDocument33 pagesCebu City Ordinance No. 2486 Cebu City Market OrdinanceHCD100% (2)
- Nursing Care Plan For HypertensionDocument5 pagesNursing Care Plan For Hypertensionmariejo89% (84)
- Nursing Care PlanDocument7 pagesNursing Care PlanGem Ma100% (7)
- NCP Ineffective Cerebral Tissue Perfusion STROKEDocument3 pagesNCP Ineffective Cerebral Tissue Perfusion STROKEMa. Elaine Carla TatingNo ratings yet
- Nursing Care Plan For HypertensionDocument5 pagesNursing Care Plan For HypertensionJessy MalloNo ratings yet
- NCP #1 Ineffective Cerebral Tissue PerfusionDocument4 pagesNCP #1 Ineffective Cerebral Tissue PerfusionsteffiNo ratings yet
- NCP For HypertensionDocument6 pagesNCP For HypertensionJaic Ealston D. Tampus0% (2)
- Nursing Care Plan For HypertensionDocument3 pagesNursing Care Plan For HypertensionFranco Razon100% (2)
- Case Study For Review Sitxfsa002Document7 pagesCase Study For Review Sitxfsa002Spencer VelascoNo ratings yet
- NURSING CARE PLAN - HydrocephalusDocument3 pagesNURSING CARE PLAN - Hydrocephalusderic98% (41)
- Heavy Metal Intoxication and Chelators MCQ Answer SheetDocument4 pagesHeavy Metal Intoxication and Chelators MCQ Answer SheetPatrick Dycoco75% (4)
- SITHCCC007 - Prepare Stock Sauces and SoupsDocument57 pagesSITHCCC007 - Prepare Stock Sauces and SoupsAlexander Lopera0% (1)
- Plant Design For The Production of Sodium CarbonateDocument29 pagesPlant Design For The Production of Sodium CarbonateMuhammad Adeel KhalidNo ratings yet
- Myocardial Infarction, NursingDocument17 pagesMyocardial Infarction, NursingApril Mae Magos LabradorNo ratings yet
- Nanda NCP BasedDocument14 pagesNanda NCP Baseddeliejoyce100% (1)
- Nursing Care Plan HydrocephalusDocument3 pagesNursing Care Plan Hydrocephalusstar7707100% (1)
- Urogenital Imaging: A Problem-Oriented ApproachFrom EverandUrogenital Imaging: A Problem-Oriented ApproachS. MorcosRating: 3 out of 5 stars3/5 (1)
- Cardiovascular Disease NCPDocument5 pagesCardiovascular Disease NCPShyla ManguiatNo ratings yet
- Special Topics in Financial Management Business Plan: Ms. Arlene B. MaramotDocument13 pagesSpecial Topics in Financial Management Business Plan: Ms. Arlene B. MaramotShalizza18No ratings yet
- Hydrocephalus, (Fluid in Brain) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHydrocephalus, (Fluid in Brain) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Brain Edema: From Molecular Mechanisms to Clinical PracticeFrom EverandBrain Edema: From Molecular Mechanisms to Clinical PracticeJerome BadautNo ratings yet
- Stroke NCPDocument5 pagesStroke NCPChantal Caragan100% (1)
- IntussusceptionDocument10 pagesIntussusceptionPatrick DycocoNo ratings yet
- Nursing Care Plan: Group 4-Open Wound Head Injury After Debris FallDocument3 pagesNursing Care Plan: Group 4-Open Wound Head Injury After Debris FallNicole Villanueva, BSN - Level 3ANo ratings yet
- Assessment Explanation Planning Interventions Rationale Evaluation Subjective: Objective: STG: STGDocument11 pagesAssessment Explanation Planning Interventions Rationale Evaluation Subjective: Objective: STG: STGGrape JuiceNo ratings yet
- Assessment Diagnosis Outcome Intervention Rationale EvaluationDocument7 pagesAssessment Diagnosis Outcome Intervention Rationale EvaluationArmie Joy Embat CariazoNo ratings yet
- Cardiovascular AccidentDocument7 pagesCardiovascular AccidentSHEILA MAE SACLOTNo ratings yet
- Stroke: Audrey LeeDocument25 pagesStroke: Audrey LeeLurbieleeNo ratings yet
- Decreasing Cerebral Edema Reducing CSF and Intracranial Blood Controlling FeverDocument9 pagesDecreasing Cerebral Edema Reducing CSF and Intracranial Blood Controlling FeverTweenie DalumpinesNo ratings yet
- Increased Intracranial Pressure Is A Rise in TheDocument3 pagesIncreased Intracranial Pressure Is A Rise in TheMark Anthony Dela CruzNo ratings yet
- Neurological Disorders For BSCDocument276 pagesNeurological Disorders For BSCAdmasu BelayNo ratings yet
- HypertensionDocument2 pagesHypertensionRodel Yacas0% (1)
- Nursing Care Plan Assessment Diagnosis Inference Planning Intervention Rationale EvaluationDocument3 pagesNursing Care Plan Assessment Diagnosis Inference Planning Intervention Rationale EvaluationRoselyn Velasco100% (1)
- NS3 Ncp-FdarDocument5 pagesNS3 Ncp-FdarArdiene Shallouvette GamosoNo ratings yet
- 7MB, Ac, 1PCSDocument1 page7MB, Ac, 1PCSRicko CiadyNo ratings yet
- College of Nursing and Allied Medical Sciences: WesleyanDocument3 pagesCollege of Nursing and Allied Medical Sciences: WesleyanMay Anne ManuzonNo ratings yet
- Laporan Pendahuluan Dan Asuhan Keperawatan Stroke Hemoragik: Disusun OlehDocument8 pagesLaporan Pendahuluan Dan Asuhan Keperawatan Stroke Hemoragik: Disusun OlehJero KateluNo ratings yet
- I. Nursing Care Plan Assessment Diagnosis Planning Interventions Rationale EvaluationDocument2 pagesI. Nursing Care Plan Assessment Diagnosis Planning Interventions Rationale EvaluationBryan Andrew GonzalesNo ratings yet
- Neuro Across - HandoutDocument10 pagesNeuro Across - HandoutLouie MartinezNo ratings yet
- Surgery For Cerebral Contusions: Rationale and Practice: Review ArticleDocument4 pagesSurgery For Cerebral Contusions: Rationale and Practice: Review ArticleIshan SharmaNo ratings yet
- Rationale EvaluationDocument1 pageRationale EvaluationAshraf DalumaNo ratings yet
- Iloilo Doctors' College College of Nursing West Avenue, Molo, Iloilo City Study Guide QuestionsDocument4 pagesIloilo Doctors' College College of Nursing West Avenue, Molo, Iloilo City Study Guide Questionseloisa lyn pizNo ratings yet
- NCP Tissue PerfusionDocument2 pagesNCP Tissue PerfusionPanJan BalNo ratings yet
- WEEK 10 & 11 Midterm 316Document9 pagesWEEK 10 & 11 Midterm 316Baylon AngelicaNo ratings yet
- AneurysmDocument3 pagesAneurysmMa. Aira Jean PedroNo ratings yet
- DIC Case StudyDocument3 pagesDIC Case StudyJuliaNo ratings yet
- Block 2 Assignment Edited Catherine Ruguru SamsonDocument12 pagesBlock 2 Assignment Edited Catherine Ruguru Samsonmoses karituNo ratings yet
- Case Study of Atherosclerosis 1. Risk Factors of AtherosclerosisDocument5 pagesCase Study of Atherosclerosis 1. Risk Factors of AtherosclerosisCarly Beth Caparida LangerasNo ratings yet
- Revision Notes in Anaesthesia and ICUDocument69 pagesRevision Notes in Anaesthesia and ICUlim sjNo ratings yet
- Nursing Care Plan: Artery Blockage May BeDocument5 pagesNursing Care Plan: Artery Blockage May BeDienizs Labini TadenaNo ratings yet
- Institute of Nursing: Far Eastern UniversityDocument3 pagesInstitute of Nursing: Far Eastern UniversityaleccespirituNo ratings yet
- Pathophysiology and Etiology of Edema in AdultsDocument15 pagesPathophysiology and Etiology of Edema in AdultsJovie Anne CabangalNo ratings yet
- B. Left Sided Heart FailureDocument20 pagesB. Left Sided Heart FailureKia GarciaNo ratings yet
- Assessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Short Term: Short TermDocument5 pagesAssessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Short Term: Short TermJA BerzabalNo ratings yet
- Intracraneanal PressureDocument8 pagesIntracraneanal PressurearturoNo ratings yet
- Explain The Physiological Mechanism That Maintain Normal Intracranial PressureDocument25 pagesExplain The Physiological Mechanism That Maintain Normal Intracranial PressureRAFNo ratings yet
- NCP1Document1 pageNCP1Anna Joy AntoneNo ratings yet
- Polycystic NCP1Document4 pagesPolycystic NCP1Mary Reigns BuhatNo ratings yet
- Risk NCP Decreased Cardiac OutputDocument2 pagesRisk NCP Decreased Cardiac OutputMICHELLE FACTONo ratings yet
- Brainedema 160314142234Document39 pagesBrainedema 160314142234Lulu LuwiiNo ratings yet
- 3 Principles of Intracranial PressureDocument21 pages3 Principles of Intracranial Pressureba.ramirez11No ratings yet
- Pulmonary Arterial Hypertension: Diagnosis and Evidence-Based TreatmentFrom EverandPulmonary Arterial Hypertension: Diagnosis and Evidence-Based TreatmentRobyn BarstNo ratings yet
- Vascular Innervation and Receptor Mechanisms: New PerspectivesFrom EverandVascular Innervation and Receptor Mechanisms: New PerspectivesRolf UddmanNo ratings yet
- Cerebral Edema, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandCerebral Edema, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Tof Case ReportDocument11 pagesTof Case ReportPatrick DycocoNo ratings yet
- EVRMC 1st EndorsementDocument4 pagesEVRMC 1st EndorsementPatrick DycocoNo ratings yet
- STDDocument69 pagesSTDPatrick DycocoNo ratings yet
- AsthmaDocument72 pagesAsthmaPatrick DycocoNo ratings yet
- Acute PancreatitisDocument7 pagesAcute PancreatitisPatrick DycocoNo ratings yet
- Dengue Pedia MMCDocument26 pagesDengue Pedia MMCPatrick DycocoNo ratings yet
- PCM Epidemiology of Yellow FeverDocument7 pagesPCM Epidemiology of Yellow FeverPatrick DycocoNo ratings yet
- AsthmaDocument1 pageAsthmaPatrick DycocoNo ratings yet
- Superficial MycosesDocument6 pagesSuperficial MycosesPatrick DycocoNo ratings yet
- 1º+ESO+++Document2 pages1º+ESO+++caladelmoral1993834No ratings yet
- Feed MixDocument4 pagesFeed MixTony1248No ratings yet
- Orthodontics Food N DietDocument4 pagesOrthodontics Food N DietnatashaNo ratings yet
- Dishwasher Manual 9000568171Document81 pagesDishwasher Manual 9000568171Matt WinneNo ratings yet
- Tai Lieu Tofle JuniorDocument4 pagesTai Lieu Tofle JuniorTrinh NguyễnNo ratings yet
- Signs and Symptoms Nursing Diagnosis Rationale Objective Nursing Intervention Rationale EvaluationDocument5 pagesSigns and Symptoms Nursing Diagnosis Rationale Objective Nursing Intervention Rationale EvaluationRemuelMagsinoNo ratings yet
- ENT600Document21 pagesENT600ZUREEN NATASYA ZULKIFLINo ratings yet
- Business PlanningDocument51 pagesBusiness PlanningJustine MadambaNo ratings yet
- Chemistry Project CHIRANJIBIDocument18 pagesChemistry Project CHIRANJIBIKrìsHna BäskēyNo ratings yet
- Centro de Idiomas: Final Exam-B02 (4 Edition) )Document3 pagesCentro de Idiomas: Final Exam-B02 (4 Edition) )juanitoNo ratings yet
- 11 - 19, 21-23, 24-25, 27Document8 pages11 - 19, 21-23, 24-25, 27Guile PTNo ratings yet
- Density Work BookDocument23 pagesDensity Work Bookdemetri lanezNo ratings yet
- Radionics AgriDocument4 pagesRadionics AgriNisha JoshiNo ratings yet
- ProverbsDocument11 pagesProverbsKaviraj NairNo ratings yet
- Oats ProcessingDocument25 pagesOats ProcessingGiannini Angelo Eugenius LebelahaNo ratings yet
- Go Go Bird MenuDocument1 pageGo Go Bird MenuFarley ElliottNo ratings yet
- Action Plan Gift GivingDocument5 pagesAction Plan Gift GivingAnnie Lyn De ErioNo ratings yet
- At The Farm 16Document18 pagesAt The Farm 16api-677034951No ratings yet
- Luo Han Guo Uses, Benefits & Dosage - DrugsDocument3 pagesLuo Han Guo Uses, Benefits & Dosage - Drugsdeny irwanNo ratings yet
- Cae ProvisionalDocument6 pagesCae ProvisionalBritannia OurenseNo ratings yet
- Lt2.1 With AnswerDocument2 pagesLt2.1 With AnswerKaren Anne Canasa BeltranNo ratings yet
- Research Paper Factory FarmingDocument5 pagesResearch Paper Factory Farmingc9sj0n70100% (1)
- Repeated Fed-Batch Lactic Acid Production in A Packed Bed-Stirred Fermentor System Using A PH Feedback Feeding MethodDocument7 pagesRepeated Fed-Batch Lactic Acid Production in A Packed Bed-Stirred Fermentor System Using A PH Feedback Feeding MethodBeeviFathimaNo ratings yet