Professional Documents
Culture Documents
tmpDAD TMP
Uploaded by
FrontiersOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
tmpDAD TMP
Uploaded by
FrontiersCopyright:
Available Formats
Clinical Research & Bioethics Khan, J Clin Res Bioeth 2016, 7:1
http://dx.doi.org/10.4172/2155-9627.1000255
Case Report Open access journal
Between a Rock and a Hard Place: When Patient Confidentiality conflicts
with a Physicians Duty to Warn
Nida Khan*
Sindh Secretariat, Planning and Development department, Pakistan
*Corresponding author: Nida Khan, Provincial Coordinator, Sindh Secretariat, Planning and Development Department, Pakistan, Tel: 00922135660371; E-mail:
enn.kay1@gmail.com
Received date: October 28, 2015; Accepted date: January 08, 2016; Published date: January 11, 2016
Copyright: 2015, Khan N. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use,
distribution, and reproduction in any medium, provided the original author and source are credited.
Keywords: Confidentiality; Autonomy Not disclosing this information may limit her ability to do that.
Some may argue that the duty of this physician is only toward his
Case Scenario patient and not toward his wife. Not disclosing this information will
potentially harm the wife and will go against the principle of non-
Patient A is a young gentleman who is married and has recently maleficence. I would approach this matter with a utilitarian thought, to
been found to be HIV positive. The patient confides in his primary maximize good for the maximum number of people and not just worry
care physician and informs him that he has had several sexual partners about one individuals inherent right to privacy. The consequences of
before his marriage. He understands that this disease is life threatening not telling the wife are very grave. If the wife is not aware of her risk,
if treatment is not begun. He claims that he is very happy in his she will not take steps to minimize risk to her unborn child. Such steps
marriage and that he and his wife are now expecting their first child. have been shown to be very effective in reducing the transfer of the
He does not want his HIV status to be disclosed to his wife because it virus. For instance, to deliver by Caesarean section and knowing not to
will jeopardize his married life. He also says that if his wife is informed breastfeed [3]. There is a possibility that the wife may at some stage
without his consent he will stop taking treatment. The physician is able find out about her husbands health status and that will result in her
to persuade A into starting his treatment. After several counseling losing trust in the physician and the entire health care system. The
sessions however, his physician is unable to persuade him into sheer coincidence that she is not my patient and only her husband has
disclosing this to his wife. The physician tells him that his wifes HIV sought care, does not take away my duty of doing no harm that is so
status should be determined so that she also begins treatment. The ingrained in my professional oath. On the flip side, failure to maintain
physician is also concerned about the impending arrival of the baby, privacy and respect the confidentiality of HIV patients has shown to
and the need to administer prophylaxis to the mother in order to drive them away from further testing, counseling and treatment and
prevent HIV transmission to the baby. What does a physician do in undermines the trust they have in their physicians. Losing trust of the
such a situation? patient is the last thing that a physician would want.
According to Beauchamp and Childress, disclosure of information
Conflicting Principles and Moral Duties to third parties is sometimes permissible and at other times, even
obligatory. If there is a high probability of a major harm to an
Confidentiality, privacy, respect for autonomy v/s duty to identifiable or known individual such as in this case the patients wife
inform/warn and duty to treat/care and unborn child, the breach of confidentiality is justified. Guidelines
also propose that physicians inform the patient of the limits on
Respect for autonomy requires that personal information should not
confidentiality in their relationship. According to the American
be disclosed without the patients consent. Central to the therapeutic
Psychiatric Association, if the physician has convincing clinical
relationship of a physician-patient, is trust [1], which is a unique
information that the patient is infected with HIV and also has good
privilege given to the doctors by the patient when they share their
reason to believe that the patients actions will place others at on-going
deepest most intimate matters freely and without fear of disclosure.
risk of exposure, then it is ethically permissible for the physician to
Maintaining privacy enhances the development of trust between the
notify an identifiable person who the physician believes is in danger of
two parties. However, the key word is mutual trust - trust in the
contracting the virus [4]. As an example of circumstances in which
doctors expertise and knowledge and trust that the patient is
disclosure is considered obligatory, public health professionals have a
consulting the doctor, for his/her/their own health, wellbeing and
duty to report sexually transmitted diseases. Not only that, they are
welfare, without agenda or bias [2]. The patient has indicated that he
duty bound to report the identity and location of all the possible sexual
will quit treatment in case his wife is informed which will result in
contacts of the infected individual. This is a standard procedure, called
relapse and even death. He may also risk future sexual partners and
contact tracing. The primary justification is that health professionals
contribute to the spread of this yet incurable disease. So the question
are obligated to reduce risk of death [4]. There is an overarching moral
arises, is confidentiality absolute? At best, it is contextual. The rights-
duty of beneficence that is compelling enough in order to protect
based autonomy, privacy and fidelity-based arguments fail to support
others from harm.
the absoluteness of confidentiality. In this case autonomy of another
person is also an issue. The wife also has a right to making fully A possible way out of this dilemma is to designate the duty to
informed decisions about her health and lifestyle. What about her inform, to public health authorities. They may inform the wife that she
autonomy? If she doesnt even know her HIV status, how will she be may have been exposed to HIV and recommend testing. Public health
able to make decisions about her health? authorities will not inform her of the source of the infection, which she
may deduce eventually in this case. In this manner, at least some
J Clin Res Bioeth Volume 7 Issue 1 1000255
ISSN:2155-9627 JCRB, an open access journal
Citation: Khan N (2016) Between a Rock and a Hard Place: When Patient Confidentiality conflicts with a Physicians Duty to Warn. J Clin Res
Bioeth 7: 255. doi:10.4172/2155-9627.1000255
Page 2 of 2
measures would be taken in order to protect the patients instance, the Confidentiality of HIV-Related Information Act, under
confidentiality [5] while simultaneously fulfilling the duty to inform which a physician may disclose confidential HIV-related information
and the duty to prevent harm. to a known contact of the patient. Contact is defined as a "sex sharing
or needle sharing partner of the subject [9]." Potential harm can be
There was a similar case reported in India [6] where a young man
an incurable disease like HIV and the spouse is the identifiable third
who became HIV positive failed to inform his wife who later became
party directly at risk. It is imperative that potential harms of non-
pregnant. Even though she sensed his ill health and recommended
disclosure of HIV status to the spouse be weighed against the harms
waiting until his recovery to start a family, he attributed his symptoms
caused by breach of confidentiality. If the patient refuses to inform the
to tuberculosis alone. She discovered his HIV positive status when she
spouse and cannot be persuaded to do so, then such violation of
was eight months pregnant.
privacy and breach of confidentiality would not only be justified but
Multiple authors contributed to this discussion and this case raised obligatory upon the physician in order to avert preventable loss of life.
new questions regarding the duties and responsibilities of not just the
medical professionals but also the family members and the state. There References
is no general definitive guideline for hospitals and health care
professionals concerning the extent of their duty to warn at risk third 1. http://www.ethics-network.org.uk/case-studies/confidentiality-and-ivf-
parties of a patients HIV status. If we are to contain this incurable treatment.
disease, certain policies are to be formulated in order to clearly 2. Myers J (2014) Medical Ethics: Context Is the Key Word. International
Journal of Clinical Medicine 5: 1030-1045.
describe the limits of confidentiality. According to Kaplan, in cases
where another individuals life or safety is at stake, the duty of a 3. http://www.ethics-network.org.uk/case-studies/confidentiality-and-ivf-
treatment.
physician to protect life and warn possible contacts overweighs his
duty to entrusted confidentiality. In such cases, the physician should 4. Beauchamp TL, Childress J (2001) Principles of Biomedical Ethics
(5thEd) Oxford University press, New York.
transfer the information, even if the patient did not waive his right for
5. http://www.sunnybrook.ca/content/index.asp?page=articles.
secrecy [7]. The legal precedence of this concept was set in the case of
Tarasoffv Regents of the University of California (1976). McWhinney, 6. Disclosure of HIV status and human rights: the duties and responsibilities
of couples, medical professionals, family members and the state (2000).
Haskins-Herkenham and Hare (1992) note that the Supreme Court Reprod Health Matters 8: 148-163.
imposed an affirmative duty on therapists to warn a potential victim
7. Kaplan O (2004) Waiver of medical confidentiality. Harefuah 143:
of intended harm by the client, stating that the right to confidentiality 295-299, 317,316.
ends when the public peril begins [8]. This was a relationship between 8. http://www.ncrel.org/sdrs/areas/issues/envrnmnt/css/cs3lk1.htm.
a psychologist and his client, where informing the police was not
9. Lenihan LP (1999) Physician duty to warn third parties. Physicians News
enough to prevent the harm. Digest.
Can we truly extrapolate the judgment on this case to physicians in
medical practice? It has certainly led to legislations in US, for in
J Clin Res Bioeth Volume 7 Issue 1 1000255
ISSN:2155-9627 JCRB, an open access journal
You might also like
- Truth Telling in PatientsDocument6 pagesTruth Telling in PatientsHv EstokNo ratings yet
- This House Believes That When Doctors Discover A Patient Has STD'S, They Should Reveal That Information To The Patient's PartnerDocument4 pagesThis House Believes That When Doctors Discover A Patient Has STD'S, They Should Reveal That Information To The Patient's PartnerlilaNo ratings yet
- Ethics Paper FinalDocument7 pagesEthics Paper Finalapi-268670617No ratings yet
- Transformative Health Strategies: Integrative Medicine and the COVID-19 PandemicFrom EverandTransformative Health Strategies: Integrative Medicine and the COVID-19 PandemicNo ratings yet
- Order 506876 1 Need RevisionDocument9 pagesOrder 506876 1 Need RevisionMoffat HarounNo ratings yet
- Case Report Analysis: Angeles University Foundation College of Nursing Medical Surgical Nursing Laboratory (NCM 0112 RLE)Document15 pagesCase Report Analysis: Angeles University Foundation College of Nursing Medical Surgical Nursing Laboratory (NCM 0112 RLE)Katreena SalvadorNo ratings yet
- Chronic: The Hidden Cause of the Autoimmune Pandemic and How to Get Healthy AgainFrom EverandChronic: The Hidden Cause of the Autoimmune Pandemic and How to Get Healthy AgainNo ratings yet
- TruthDocument7 pagesTruthRosse Del Mundo100% (1)
- Cullen and Klein Respect For TruthDocument8 pagesCullen and Klein Respect For TruthMohammed AltekreetiNo ratings yet
- 7-Step Moral Decision-Making Process - Hannah SarioDocument5 pages7-Step Moral Decision-Making Process - Hannah SarioJeceille BorjaNo ratings yet
- Honesty in MedicineDocument7 pagesHonesty in MedicineannisanangNo ratings yet
- Scott Rae's Model Case AnalysisDocument4 pagesScott Rae's Model Case AnalysisPhilip James LopezNo ratings yet
- Truth PatientDocument3 pagesTruth PatientDaniel PancuNo ratings yet
- Truth Telling To Terminally Ill Patients To Tell or Not To Tell 2155 9627 4 159 PDFDocument2 pagesTruth Telling To Terminally Ill Patients To Tell or Not To Tell 2155 9627 4 159 PDFJeffrey ViernesNo ratings yet
- Ethics of Breaking Sad News To Patient by Health C PDFDocument3 pagesEthics of Breaking Sad News To Patient by Health C PDFvidiyahNo ratings yet
- Mold and Mycotoxins: Current Evaluation and Treatment 2022From EverandMold and Mycotoxins: Current Evaluation and Treatment 2022Rating: 5 out of 5 stars5/5 (2)
- Rights: Know YourDocument4 pagesRights: Know YourAli HusseinNo ratings yet
- Telling A Patient That He Is To Die A Moral DilemmaDocument1 pageTelling A Patient That He Is To Die A Moral DilemmaKerisia WayneNo ratings yet
- Public HealthDocument7 pagesPublic HealthRobert BwamikiNo ratings yet
- PD PaperDocument4 pagesPD PaperMafie BarreiroNo ratings yet
- Truth Telling in Palliative Care Nursing The Dilemmas of CollusionDocument8 pagesTruth Telling in Palliative Care Nursing The Dilemmas of CollusionCaninet CriseniNo ratings yet
- SHeS Bioethics Reading Material 2Document5 pagesSHeS Bioethics Reading Material 2Lorie Yvonne Quibin AgullanaNo ratings yet
- Your Health in Your Hands: How to be healthy in spite of "medical science"From EverandYour Health in Your Hands: How to be healthy in spite of "medical science"No ratings yet
- Riddiford Ethics Paper Nov17Document6 pagesRiddiford Ethics Paper Nov17api-354529854No ratings yet
- Week 9-Medical FutilityDocument13 pagesWeek 9-Medical FutilityVidya Bala100% (1)
- Dr-Patient Relationship v5Document6 pagesDr-Patient Relationship v5IsmaelJoséGonzálezGuzmánNo ratings yet
- The Slim Book of Health Pearls: The Complete Medical ExaminationFrom EverandThe Slim Book of Health Pearls: The Complete Medical ExaminationNo ratings yet
- Sample CaseDocument3 pagesSample CaseJohn Dhee E. CabreraNo ratings yet
- The Healing Touch: Keeping the Doctor-Patient Relationship Alive Under Managed CareFrom EverandThe Healing Touch: Keeping the Doctor-Patient Relationship Alive Under Managed CareRating: 5 out of 5 stars5/5 (1)
- Fiel Angelo G. Mallari, RNDocument68 pagesFiel Angelo G. Mallari, RNfiel mallariNo ratings yet
- The Daily Dose Secrets To COVID19, A COVID19 Travel Nurse Specialist ExperienceFrom EverandThe Daily Dose Secrets To COVID19, A COVID19 Travel Nurse Specialist ExperienceRating: 5 out of 5 stars5/5 (5)
- Physician Integrity: Why It Is InviolableDocument3 pagesPhysician Integrity: Why It Is InviolableAndrea Villagran100% (1)
- Don't Let Your Doctor Kill You: How to Beat Physician Arrogance, Corporate Greed and a Broken SystemFrom EverandDon't Let Your Doctor Kill You: How to Beat Physician Arrogance, Corporate Greed and a Broken SystemNo ratings yet
- Tasting YOUR OWN Medicine: How to Advocate for Yourself in Healthcare SettingsFrom EverandTasting YOUR OWN Medicine: How to Advocate for Yourself in Healthcare SettingsNo ratings yet
- Everett2011 4Document6 pagesEverett2011 4ceifheiogajNo ratings yet
- Autonomy & VeracityDocument3 pagesAutonomy & VeracityLovie Japhet LopezNo ratings yet
- Invasion of PrivacyDocument2 pagesInvasion of PrivacyJan Jamison ZuluetaNo ratings yet
- Braley Ethics Paper Final March24Document7 pagesBraley Ethics Paper Final March24api-381438480No ratings yet
- "Don't Necessarily" Trust Me, I'm a Doctor: A Roadmap to finding a trustworthy health care provider and avoiding the dangers of not doing soFrom Everand"Don't Necessarily" Trust Me, I'm a Doctor: A Roadmap to finding a trustworthy health care provider and avoiding the dangers of not doing soNo ratings yet
- Reason and Impartiality As Minimum Requirement For MoralityDocument6 pagesReason and Impartiality As Minimum Requirement For MoralityKimchi Haru91% (23)
- Ethics and The DoctorDocument3 pagesEthics and The DoctorvinsynthNo ratings yet
- 2.2 Reason and Impartiality As Minimum Requirement For MoralityDocument5 pages2.2 Reason and Impartiality As Minimum Requirement For MoralityMarifer CavintaNo ratings yet
- Journal 1 EntryDocument4 pagesJournal 1 EntryMeet DandiwalNo ratings yet
- Psychological Aspects of Living With HIV Disease: PracticeDocument4 pagesPsychological Aspects of Living With HIV Disease: PracticeAntro BerrinNo ratings yet
- Reclaim Responsibility.: Redefine Your Perspective on Health and WellbeingFrom EverandReclaim Responsibility.: Redefine Your Perspective on Health and WellbeingNo ratings yet
- Study - Session - 2 - The Ethics of Breaking Bad NewsDocument6 pagesStudy - Session - 2 - The Ethics of Breaking Bad NewsSANDHYANo ratings yet
- AutonomyDocument3 pagesAutonomyMae Jane AuzaNo ratings yet
- Appointment with Danger: Medical Care Can Kill You: Medical Care Can Kill YouFrom EverandAppointment with Danger: Medical Care Can Kill You: Medical Care Can Kill YouNo ratings yet
- Ethics 1Document1 pageEthics 1Aya SalahNo ratings yet
- Building A Cooperative Patient/doctor RelationshipDocument4 pagesBuilding A Cooperative Patient/doctor RelationshipskjfdsahjkdfsaNo ratings yet
- Ethical PrinciplesDocument2 pagesEthical PrinciplesDarlyn CadalinNo ratings yet
- Communication With and On Behalf of PatientsDocument133 pagesCommunication With and On Behalf of PatientsDes Anggraeni RuniasiwiNo ratings yet
- tmpF178 TMPDocument15 pagestmpF178 TMPFrontiersNo ratings yet
- Tmp1a96 TMPDocument80 pagesTmp1a96 TMPFrontiersNo ratings yet
- Tmpa077 TMPDocument15 pagesTmpa077 TMPFrontiersNo ratings yet
- tmpE3C0 TMPDocument17 pagestmpE3C0 TMPFrontiersNo ratings yet
- tmp998 TMPDocument9 pagestmp998 TMPFrontiersNo ratings yet
- tmp3656 TMPDocument14 pagestmp3656 TMPFrontiersNo ratings yet
- tmp27C1 TMPDocument5 pagestmp27C1 TMPFrontiersNo ratings yet
- tmpA7D0 TMPDocument9 pagestmpA7D0 TMPFrontiersNo ratings yet
- tmp96F2 TMPDocument4 pagestmp96F2 TMPFrontiersNo ratings yet
- tmp97C8 TMPDocument9 pagestmp97C8 TMPFrontiersNo ratings yet
- Adrenal Gland Disorders: Addison's DiseaseDocument4 pagesAdrenal Gland Disorders: Addison's DiseaseyoussraselimNo ratings yet
- Pharmacology of Drugs For PPHDocument55 pagesPharmacology of Drugs For PPHFaye CagayanNo ratings yet
- Endocrine Physiology - Part 3 Parathyroid GlandDocument30 pagesEndocrine Physiology - Part 3 Parathyroid GlandTerrence Beniasi CharumbiraNo ratings yet
- Movie A Beautiful MindDocument3 pagesMovie A Beautiful Mindhang doNo ratings yet
- Central Council of Indian Medicine New Delhi: Syllabus of Ayurvedacharya (Bams) CourseDocument22 pagesCentral Council of Indian Medicine New Delhi: Syllabus of Ayurvedacharya (Bams) CourseAnanya MenonNo ratings yet
- 2nd Quarter Exam Science 10Document11 pages2nd Quarter Exam Science 10Brille Anthony BunielNo ratings yet
- Radiation Protection in Medical Radiography 1Document17 pagesRadiation Protection in Medical Radiography 1nonoadwan12No ratings yet
- Workshop On Early Warning Score System - Ali HaedarDocument76 pagesWorkshop On Early Warning Score System - Ali HaedarVicky ShuarNo ratings yet
- PEMF Therapy Controls Physical Effects of StressDocument2 pagesPEMF Therapy Controls Physical Effects of StressAndreas LooseNo ratings yet
- D'OXYVA Information Summary For Healthcare Professionals - Proofreadv3 W.O CommentsDocument12 pagesD'OXYVA Information Summary For Healthcare Professionals - Proofreadv3 W.O CommentsCircularity HealthcareNo ratings yet
- Comprehensive Review of Chest Tube Management A ReviewDocument6 pagesComprehensive Review of Chest Tube Management A ReviewCesar LinaresNo ratings yet
- Monobind Assay Technical GuideDocument16 pagesMonobind Assay Technical GuideDaNny XaVierNo ratings yet
- Code of Practice On: Workplace Safety and Health (WSH) Risk ManagementDocument51 pagesCode of Practice On: Workplace Safety and Health (WSH) Risk Managementaminul islamNo ratings yet
- Evolution of Aortic Arches in VertebratesDocument2 pagesEvolution of Aortic Arches in Vertebratesarbazkhan825lNo ratings yet
- 6 Minute Walk TestDocument7 pages6 Minute Walk Testriccardo6grassiNo ratings yet
- Pharmaceutical and Clinical Study of Kumkumadi Cream Prepared Using Kwath As Water Phase and Oil As Modern Phase On The Disease Vyanga'Document8 pagesPharmaceutical and Clinical Study of Kumkumadi Cream Prepared Using Kwath As Water Phase and Oil As Modern Phase On The Disease Vyanga'freemoronsNo ratings yet
- Mandibular NerveDocument3 pagesMandibular Nervervinluan.dentNo ratings yet
- ASYNCHRONOUS ACTIVITY#2 PassssssesesesesesDocument18 pagesASYNCHRONOUS ACTIVITY#2 PassssssesesesesesNur SanaaniNo ratings yet
- 174 Anatomy Teeth and GumsDocument20 pages174 Anatomy Teeth and GumsRhona AngelaNo ratings yet
- Jurnal MigrainDocument6 pagesJurnal MigrainReksyNo ratings yet
- 1) Correction of Single Gene Defect Diseases Recessive Inborn Errors ofDocument6 pages1) Correction of Single Gene Defect Diseases Recessive Inborn Errors ofesam889No ratings yet
- Case Note 6: Patient DetailsDocument3 pagesCase Note 6: Patient DetailsBINCYNo ratings yet
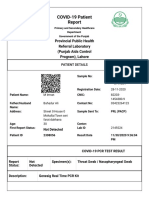
- Https Covid-19.Pshealthpunjab - Gov.pk PublicSampleResults PatientPublicSampleResultDocument2 pagesHttps Covid-19.Pshealthpunjab - Gov.pk PublicSampleResults PatientPublicSampleResultmuhammad imranNo ratings yet
- MRCPCH q15Document30 pagesMRCPCH q15Galaleldin AliNo ratings yet
- Neuromuscular BlockersDocument25 pagesNeuromuscular BlockersAbdelrahman GalalNo ratings yet
- Range of Motion ExerciseDocument8 pagesRange of Motion ExerciseAmit Martin83% (6)
- Maintenance Fluid Therapy in ChildrenDocument4 pagesMaintenance Fluid Therapy in ChildrenNicole_0No ratings yet
- Legal Aid Society Complaint Re Homeless YouthDocument65 pagesLegal Aid Society Complaint Re Homeless YouthPaul SchindlerNo ratings yet
- DESSERTATIONDocument9 pagesDESSERTATIONKinjal VasavaNo ratings yet
- Review Article Yoda THD DM (Manuskrip)Document4 pagesReview Article Yoda THD DM (Manuskrip)shafiyyah putri maulanaNo ratings yet