Professional Documents
Culture Documents
Cardio Pulmonary Resuscitation: Internal and Critical Care Medicine Study Notes
Uploaded by
eryxspOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cardio Pulmonary Resuscitation: Internal and Critical Care Medicine Study Notes
Uploaded by
eryxspCopyright:
Available Formats
Cardio Pulmonary Resuscitation
Internal and critical care medicine study notes
Dr. Ali Ragab
Critical Care Medicine
Damanhur Medical National Institute
Facebook (ali_ragab_ali@yahoo.com)
Cardio Pulmonary Resuscitation
Internal and critical care medicine study notes
Dr. Ali Ragab
Critical Care Medicine
Damanhur Medical National Institute
Facebook (ali_ragab_ali@yahoo.com)
Dr. Ali Ragab 2
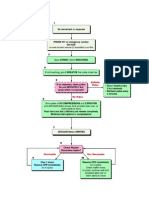
Basic Life Support (BLS)
Commencement of cardiopulmonary resuscitation
The current BLS guidelines recommend that CPR be commenced if the victim is
unresponsive and not breathing normally
An appropriately trained ALS provider can check for a central pulse (e.g.
carotid) for up to 10 seconds during this period of assessment, but this should
not delay CPR
It is now recommended that CPR should start with compressions
External cardiac compression
Site of compression
The desired compression point for CPR in adults remains over the lower half
of the sternum
Compressions that are provided higher than this become less effective, and
compressions lower than this are also less effective and have an increased risk
of damage to intra abdominal organs
Rate of compression
It is recommended that chest compressions should be performed at a rate of
approximately 100 compressions/min
Lower rates (<80/min) were associated with worse outcomes
Higher rates (>120/min) were associated with more fatigue, and shallower
compressions
Depth of compression
The recommended compression depth for adults is now at least 5 cm; the chest
should be compressed approximately one-third of its depth
Dr. Ali Ragab 3
Minimise interruptions to compressions
Interruptions in chest compressions (hands-off time) are common, often
prolonged, and are associated with a decrease in coronary perfusion pressure
and a deceased likelihood of defibrillation success
These adverse effects commence within 10 seconds of stopping CPR, but appear
to be at least partially reversible with the recommencement of chest
compressions
It is recommended that chest compressions be commenced as soon as the
victim is confirmed to be unresponsive and not breathing normally
The frequency and duration of interruptions in compressions for rhythm
recognition or specific interventions (such as ventilations, charging the
defibrillator, defibrillation, or intubation) should be kept to a minimum
Compression/Ventilation ratio
A single compression/ventilation ratio of 30/2 remains recommended for adult
BLS before the airway is secured
The tidal breath should be delivered within 1 second
The desired tidal volume to be delivered is one that results in a visible chest rise
Monitoring the quality of CPR
Simple monitoring techniques include
Observing of the rate, depth and positioning of chest compressions
Observing the rate and depth of ventilation
Palpating central pulses
Waveform capnography should be considered for all arrests
Additional monitoring techniques that can be used include
Mechanical devices (e.g. For monitoring the depth of compressions)
Monitor/defibrillators (e.g. for monitoring the depth and rate of compressions
and ventilation)
Dr. Ali Ragab 4
Utility of end-tidal carbon dioxide monitoring during cardiac arrest
Cardiovascular (absolute value of ETCO2)
Falls immediately at the onset of cardiac arrest
Increases immediately with chest compressions
Provides a linear correlation with cardiac index
Allows early detection of ROSC (sudden increase)
Respiratory (ETCO2 waveform)
Allows assessment of endotracheal tube placement
Allows assessment of expiratory flow limitation
Prognosis (absolute value of ETCO2)
Predicts successful resuscitation
Compression-only CPR
Despite the limited data to support compression-only CPR, it is recommended
that if rescuers are unable, not trained, or unwilling to perform mouth-to-
mouth ventilation (rescue breathing) then they should perform compression
only CPR, as any attempt at resuscitation is better than no attempt
Defibrillation
Defibrillation remains the definitive treatment for shockable rhythms such as
pulseless ventricular tachycardia or ventricular fibrillation
Successful defibrillation requires an appropriate combination of defibrillator
waveform and energy level
Dr. Ali Ragab 5
Early defibrillation Vs CPR before defibrillation
The traditional approach to the treatment of a shockable rhythm during cardiac
arrest has been to perform defibrillation as soon as possible
In the scenario of recent-onset VF, and the best outcomes are associated with
defibrillation within 3 minutes (e.g. in electrophysiology labs or coronary care
units)
In situations where the VF has persisted for more than a few minutes, an initial
period of CPR could be considered before defibrillation
Waveform for defibrillation
No specific defibrillator waveform (either monophasic or biphasic) is
consistently associated with a greater incidence of return of spontaneous
circulation (ROSC) or increased hospital discharge rates from cardiac arrest due
to ventricular fibrillation
Defibrillation with biphasic waveforms using equal or lower energy levels,
appears at least as effective as monophasic waveforms for termination of VF
Energy levels
Recommendations for energy levels to be used for defibrillation vary according
to the type of defibrillator that the rescuers are using
The recommended energy level for defibrillation in adults where monophasic
defibrillators are used is 360 J for all shocks
When using biphasic waveforms, the energy level should be set at 200 J for all
shocks unless there exist relevant clinical data for the specific defibrillator
suggesting that an alternative energy level provides adequate shock success
There is no consistent evidence (e.g. survival benefit) to suggest that an
escalation of energy levels is required for subsequent shocks
Dr. Ali Ragab 6
Manual defibrillation or automated external defibrillator
Automated external defibrillators provide an opportunity for untrained
bystanders and BLS providers to defibrillate a shockable rhythm
In the hands of skilled healthcare providors, manual defibrillation should be
used whenever possible as the delays inherent in the use of an AED may be
detrimental
Single-shock technique
The use of a single-shock strategy for defibrillation is recommended (i.e.
delivers a single shock and then immediately commences CPR)
This strategy minimises the interruptions to chest compressions that occur
during defibrillation attempts
The Australian Resuscitation Council recommends the consideration of a
stacked shock strategy (up to three shocks as necessary) in specific
circumstances: patients with a perfusing rhythm who develop a shockable
rhythm, in a witnessed and monitored setting, where a manual defibrillator is
immediately available (e.g. first shock able to be delivered within 20 seconds)
and the time required for rhythm recognition and charging of the defibrillator
is short (e.g. <10 seconds). All subsequent shocks should be given using a
single-shock strategy
Pads or paddles
Self-adhesive defibrillation pads are safe and effective for defibrillation, can
facilitate pacing and allow charging during compressions
If there are concerns about contact or success of defibrillation, then paddles can
be used, but they require the use of conductive gel pads and the application of
sufficient firm pressure to maximise electrical contact
Dr. Ali Ragab 7
Advanced life support
Precordial thump
A precordial thump may be considered in a pulseless ventricular tachycardia if a
defibrillator is not immediately available
The technique should not delay defibrillation.
A precordial thump is no longer recommended for ventricular fibrillation
Chest compressions
Interruptions to chest compressions for definitive procedures or interventions
should be kept as brief as possible
Chest compressions should be continued up until defibrillation, including
during charging of the defibrillator
CPR should also be commenced again immediately following defibrillation
(without checking the rhythm), and continued for at least 2 minutes unless
signs of life return (the victim becomes responsive or starts breathing)
Even if defibrillation has successfully reverted the rhythm into one that could
generate a pulse, in the vast majority of cases this is not initially associated with
an output. Immediate compressions in these situations avoid the detrimental
effects of prolonged interruptions in compressions and maintain the coronary
perfusion
After each 2 minutes of CPR (or if signs of life return), the underlying rhythm
should be checked, and if a rhythm compatible with a return of spontaneous
circulation is observed at that time then a central pulse should also be checked
Dr. Ali Ragab 8
Airway management during CPR
Endotracheal intubation remains the gold standard for airway maintenance
and airway protection during CPR
The endotracheal tube provides optimal isolation and patency of the airway,
allows suctioning of the airway and also provides access for the delivery of some
drugs (e.g. epinephrine (adrenaline), lidocaine and atropine)
Attempts at endotracheal intubation should not interrupt cardiac compressions
for more than 20 seconds
A large number of supraglottic airway devices have been trialled as
alternatives to the endotracheal tube
Ventilation during CPR
Before the airway is secured; a compression/ventilation ratio of 30/2 is
recommended
After the airway is secured; a ventilation rate of 810/minute is
recommended; one way to provide this, and to minimise interruptions to
compressions is to use a compression/ventilation ratio of 15/1 once the airway is
secured
Avoid hyperventilation
Hyperventilation during cardiac arrest is associated with increased
intrathoracic pressure, decreased coronary and cerebral perfusion
If there is a concern about potential gas trapping, a period of disconnection
from the ventilation circuit may be beneficial
The tidal volume recommended is one that results in a visible chest rise
Dr. Ali Ragab 9
Identification of reversible causes
Consider and correct
1. Hypoxia
2. Hypovolaemia
3. Hyper/hypokalaemia/metabolic disorders
4. Hypothermia/hyperthermia
5. Tension pneumothorax
6. Tamponade
7. Toxins
8. Thrombosis (pulmonary/coronary)
Diagnosis
A number of techniques are available to assist in the diagnosis and exclusion of
these conditions. These include a good history, a careful clinical examination,
and some specific investigations and interventions
Echocardiography can potentially diagnose (or help exclude) a number of
cardiac and non-cardiac reversible causes
Potentially useful diagnoses detectable by echocardiography
Hypovolaemia
Tamponade (pericardial)
Tension pneumothorax
Thrombosis (pulmonary)
Thrombosis (coronary) (regional or global wall motion abnormalities, including
lack of cardiac motion)
Pacemaker capture
Unexpected VF
Acute valvular insufficiency (e.g. papillary muscle rupture)
Ventricular rupture
Aortic dissection
Massive pleural effusion
Dr. Ali Ragab 10
Medications during CPR
Route of administration
The intraosseous route should be considered for administration of medications
if venous access is not immediately available
Vasopressors
The beneficial effect of vasopressors during cardiac arrest is to increase the
perfusion pressure to the heart and brain
Epinephrine remains the vasopressor of choice during the management of
cardiac arrest
The initial adult dose is 1 mg and this should be repeated approximately every
4 minutes
Anti-arrhythmics
Administration of amiodarone (300 mg or 5 mg/kg) for shock refractory
ventricular fibrillation
Either amiodarone or lidocaine (but not both) should be considered in those
patients still in ventricular fibrillation after repeated attempts at defibrillation
have failed (i.e. immediately after the third shock)
Dr. Ali Ragab 11
Cardiac arrest medications in specific circumstances
Medication Potential indications
Atropine Cholinergic/cardiac glycoside toxicity
Anti-venom Snake, funnel-web spider, box jellyfish venom
Benzodiazepines Sympathomimetic toxicity
Calcium Hypocalcaemia, hypermagnesaemia,
hyperkalaemia, beta-blocker/calcium channel
blocker toxicity
Digoxin-specific antibodies Cardiac glycoside toxicity
Flumazenil Benzodiazepine toxicity
Epinephrine Beta-blocker/calcium channel blocker toxicity
Glucagon Beta-blocker/calcium channel blocker toxicity
High-dose insulin/dextrose Beta-blocker/calcium channel blocker toxicity
Lipid emulsion Local anaesthetic agents
Magnesium Hypomagnesaemia, hypokalaemia,
hypercalcaemia, tricyclic antidepressant/cardiac
glycoside toxicity, torsade de pointes
Naloxone Opioid toxicity
Potassium Hypokalaemia
Pyridoxine Isoniazid toxicity
Sodium bicarbonate Hyperkalaemia, tricyclic antidepressant/sodium-
channel-blocker toxicity
Adjuncts to CPR
Active-compression decompression (ACD) CPR is the most widely evaluated
technique
Mechanical devices (such as LUCAS or the load distributing band) may be
useful alternatives to manual CPR in situations where traditional CPR is
difficult or hazardous (e.g. during transport, or during interventions)
Dr. Ali Ragab 12
Management of the resuscitated post cardiac arrest patient
Pathophysiology
Post cardiac arrest brain injury
Accounts for a large portion of morbidity and mortality in resuscitated cardiac
arrest patients
The brain has limited tolerance to ischemia and has a unique response to
reperfusion
Much of the neurologic dysfunction that occurs after ROSC can be attributed to
cerebral edema, post ischemic neurodegeneration, and impaired
cerebrovascular autoregulation
Post cardiac arrest myocardial dysfunction
Patients can be hemodynamically unstable after ROSC because of a period of
global hypokinesis (myocardial stunning) that occurs or directly from the
precipitating pathology (e.g. myocardial infarction)
Myocardial stunning is usually reversible but can last up to 72 hours
Systemic ischemia/reperfusion response
After ROSC, a sepsis-like state has been described, in which there is a
significant systemic inflammatory response syndrome (SIRS) response,
impaired vasoregulation, increased coagulation, and adrenal suppression
Persistent precipitating pathology
The underlying cause of the arrest commonly contributes to and complicates
the pathophysiologic state of the patient, such as acute coronary syndrome,
pulmonary embolism, respiratory failure, electrolyte abnormalities, metabolic
abnormalities, environmental insults, toxic exposures, trauma, sepsis, and
others
Dr. Ali Ragab 13
Diagnosis
ECG should be performed as soon as possible post-ROSC to determine if an ST-
elevation myocardial infarction (STEMI) was the cause of the arrest
Chest x-ray should be performed to detect reversible causes of cardiac arrest
(i.e. pneumothorax) and to confirm position of supporting tubes and lines
A head CT should be performed when there is a suspicion that an intra cranial
event precipitated the cardiac arrest. Otherwise head CT is not mandatory and
should not delay further care
CT angiography of the chest if pulmonary embolism or aortic dissection is
suspected
Laboratory studies appropriate for critically ill patients should be obtained
including complete blood cell count, comprehensive metabolic panel, liver
function tests, cardiac enzymes, lactic acid, arterial blood gas, and toxin screen
Key factors to consider after resuscitation from cardiac arrest
Immediate tasks
Re-evaluate ABCDE
12-lead ECG
Treat precipitating causes
Re-evaluate oxygenation and ventilation
Temperature control (cool)
Early goals
Continue respiratory support
Maintain cerebral perfusion
Treat and prevent cardiac arrhythmias
Determine and treat the cause of the arrest
Dr. Ali Ragab 14
Specific tasks
Maintain MAP 65-100 mmHg
Maintain adequate oxygenation (SaO2 9496%)
Maintain normal pH and normocarbia (e.g. PaCO2 4045 mmHg)
Moderate glycemic control (144-200 mg/dL)
Consider therapeutic hypothermia (unless contraindicated)
Maintain appropriate sedation
Treat seizures
Continue search to identify underlying cause(s) and trauma related to
resuscitation
Consider specific treatment for underlying cause (e.g. percutaneous coronary
intervention, thrombolytics)
Consider prophylactic antiarrhythmics
Consider transfer to resuscitation centre
Therapeutic Hypothermia (TH)
Phases of TH
Induction(obtain target temperature <6 h of ROSC)
Obtain target temperature of 32C to 34C as soon as possible with cold saline
infusion followed by surface cooling systems or invasive cooling catheters
Shivering _ common during TH. Control with analgesics, sedatives, and
possibly neuromuscular blockade as shivering increases 02 consumption and
significantly decreases cooling rates
Maintenance (12-24 h)
Usually the most stable phase of TH
Avoid major temperature fluctuations
Dr. Ali Ragab 15
Rewarming (0.25C/h to 0.5C/h)
Rewarm slowly at a rate of 0.25C/h to 0.5C/h to avoid rebound hyperrhermia,
which can lead to unstable hemodynamics and further neurologic damage
Monitor electrolyte as rewarming precipitates hypoglycemia and hyperkalemia
Normothermia
Maintain normothermia after TH, as hyperthermia post-ROSC has been shown
to be associated with worse outcomes
Relative contraindications
Relative contraindications for TH include traumatic arrest, sepsis as the
etiology of arrest, coma for other reasons, uncontrolled bleeding, prolonged
duration of resuscitation (>60 minutes), or severe intracranial hemorrhage
Oxygenation
Initially during resuscitation, it is common to use 100% oxygen to avoid hypoxia
Wean FIO2 as low as possible for goal SaO2 of 94%-96%
Ventilation
Goal PaCO2 of high normal (40-45 mmHg) should be targeted
Avoid hyperventilation with hypocapnia to prevent cerebral vasoconstriction
and auto-PEEP
Target a tidal volume of 6-8 mL/kg of ideal body weight to prevent lung damage
from alveolar over distension
Hemodynamics
Hypotension is common secondary to relative volume depletion, vasodilation
from the severe SIRS response, and cardiac depression from myocardial
stunning or infarct
Dr. Ali Ragab 16
Early goal-directed therapy
Initial volume resuscitation to optimize preload
If still hypotensive, add vasopressors for a goal MAP between 65-100 mmHg
Echocardiography or invasive hemodynamic monitoring may guide use of
inotropes (e.g. dobutamine or milrinone) for hypotension secondary to
myocardial depression
Consider mechanical support devices like intra aortic balloon pump, ventricular
assist devices, or extracorporeal membrane oxygenation (ECMO) for
persistently hemodynamically unstable patients
Goal to achieve Scv02 >70% and lactate clearance
Glucose control
TH can cause insulin resistance and hyperglycemia
Moderate glycemic control (144-200 mg/dL) should be employed
Coronary revascularization
Electrocardiogram _ Obtain immediately post-ROSC to determine if ST
elevations are present, which should prompt immediate consideration for
reperfusion, ideally primary PCI
lschemia without STEMI may also precipitate cardiac arrest, so that even in the
absence of STEMI, it may be reasonable to consider angiography
Coronary angiography should not delay TH
Treatment of seizures
Obtain early and ideally continuous EEG monitoring, as it is common to have
non convulsive status epilepticus in this setting, in particular, for patients who
are paralyzed
It is reasonable to institute prompt and aggressive treatment of seizures
Dr. Ali Ragab 17
Antiarrhythmic drug
It may be reasonable to continue an infusion of an antiarrhythmic drug that
successfully restored a stable rhythm during resuscitation (e.g. lidocaine 24
mg/min or amiodarone 0.6 mg/kg/h for 1224 hours)
Neuroprognostication
Neuroprognostication is extremely difficult in the post arrest period
There are no post arrest physical exam findings or diagnostic tests that can
accurately predict poor outcome during the first 24 hours
At 72 hours, incomplete recovery of brainstem reflexes, myoclonus, extension
posturing or absent motor response to pain, and bilaterally absent
somatosensory cortical evoked potentials (N20) were associated with a 0% false
positive rate for poor outcome. These observations were made in patients who
did not undergo TH
TH and the accompanying use of sedative, analgesic, and paralytic medication
can delay neurologic recovery. In the setting of TH, traditional prognostic
features should be interpreted with caution so as to avoid premature
documentation of poor prognosis leading to inappropriate withdrawal of care in
patients
Until further investigations are conducted, we recommend attempts to provide
neuroprognostication be held at least until 72 hours after patients have been
rewarmed
Dr. Ali Ragab 18
You might also like
- Adult Advanced Life Support: Resuscitation Council (UK)Document23 pagesAdult Advanced Life Support: Resuscitation Council (UK)Masuma SarkerNo ratings yet
- Guidelines Adult Advanced Life SupportDocument35 pagesGuidelines Adult Advanced Life SupportindahNo ratings yet
- 2009 UCSD Medical Center Advanced Resuscitation Training ManualDocument19 pages2009 UCSD Medical Center Advanced Resuscitation Training Manualernest_lohNo ratings yet
- Acls Course HandoutsDocument8 pagesAcls Course HandoutsRoxas CedrickNo ratings yet
- Guidelines Adult Advanced Life SupportDocument34 pagesGuidelines Adult Advanced Life SupportParvathy R NairNo ratings yet
- Advanced Cardiovascular Life Support (ACLS)Document27 pagesAdvanced Cardiovascular Life Support (ACLS)Sara Ali100% (3)
- Mona Adel, MD, Macc A.Professor of Cardiology Cardiology Consultant Elite Medical CenterDocument34 pagesMona Adel, MD, Macc A.Professor of Cardiology Cardiology Consultant Elite Medical CenterOnon EssayedNo ratings yet
- Cardiopulmonar Y ResuscitationDocument34 pagesCardiopulmonar Y ResuscitationRatuSitiKhadijahSarahNo ratings yet
- CPR: Essentials of Cardiopulmonary ResuscitationDocument7 pagesCPR: Essentials of Cardiopulmonary Resuscitationdaniphilip777No ratings yet
- Basic Cardiac Life Support 2011Document6 pagesBasic Cardiac Life Support 2011Tashfeen Bin NazeerNo ratings yet
- Cardiopulmonary Resuscitation 2015Document31 pagesCardiopulmonary Resuscitation 2015Clarissa Maya TjahjosarwonoNo ratings yet
- ANZCOR Guideline 11.2 - Protocols For Adult Advanced Life SupportDocument8 pagesANZCOR Guideline 11.2 - Protocols For Adult Advanced Life SupportMario Colville SolarNo ratings yet
- Cardiopulmonary ResuscitationDocument3 pagesCardiopulmonary ResuscitationLee Liang Lee LiangNo ratings yet
- Guidelines - In-Hospital ResuscitationDocument18 pagesGuidelines - In-Hospital ResuscitationparuNo ratings yet
- Basic Life Support and Advanced Cardiovascular Life SupportDocument90 pagesBasic Life Support and Advanced Cardiovascular Life SupportRakhshanda khan100% (1)
- Advanced Life Support-RESSU CouncilDocument30 pagesAdvanced Life Support-RESSU CouncilGigel DumitruNo ratings yet
- What Is BLS?: Respiratory ArrestDocument2 pagesWhat Is BLS?: Respiratory ArrestStephanie Joy EscalaNo ratings yet
- Cardio Pulmonary R Ry Resuscitation 2010Document26 pagesCardio Pulmonary R Ry Resuscitation 2010Fatahillah NazarNo ratings yet
- Resuscitation Council (UK) In-Hospital Cardiac Arrest GuidelinesDocument10 pagesResuscitation Council (UK) In-Hospital Cardiac Arrest GuidelinesCzarian Estillore HigoyNo ratings yet
- Adult Advanced Life SupportDocument23 pagesAdult Advanced Life SupportbigpriapNo ratings yet
- CPR First? or Defibrillation First?: Re-AffirmedDocument4 pagesCPR First? or Defibrillation First?: Re-AffirmedangelNo ratings yet
- Cardio Pulmonary Resuscitation 2010: Djayanti SariDocument26 pagesCardio Pulmonary Resuscitation 2010: Djayanti SariAlessandro AlfieriNo ratings yet
- Cardiopulmonary ResuscitationDocument10 pagesCardiopulmonary ResuscitationLilay MakulayNo ratings yet
- ACLSDocument61 pagesACLSmgthida935100% (1)
- Advanced Life Support Algorithm: Learning OutcomesDocument12 pagesAdvanced Life Support Algorithm: Learning OutcomesAljeirou AlcachupasNo ratings yet
- AHA Defibrilation: Ventricular FibrilationDocument4 pagesAHA Defibrilation: Ventricular FibrilationStacia StefaniNo ratings yet
- CPR & Electrical TherapiesDocument67 pagesCPR & Electrical TherapiesRizaldy Yoga67% (3)
- Cardiac ArrestDocument79 pagesCardiac Arrestnaveena reddyNo ratings yet
- Cardiopulmonary Resuscitation: Australian Training InstituteDocument11 pagesCardiopulmonary Resuscitation: Australian Training InstituteAustralian Training InstituteNo ratings yet
- Lectii ScoalaDocument43 pagesLectii ScoalaGaudiMateiNo ratings yet
- CPR - Cardiopulmonary ResuscitationDocument31 pagesCPR - Cardiopulmonary ResuscitationPanji HerlambangNo ratings yet
- Basic Life SupportDocument6 pagesBasic Life SupportRyan Mathew ScottNo ratings yet
- Advanced Cardiac Life Support: Valentina, MD, FIHADocument34 pagesAdvanced Cardiac Life Support: Valentina, MD, FIHAfaradibaNo ratings yet
- Basic Life Support Study Guide: Critical Care Training CenterDocument12 pagesBasic Life Support Study Guide: Critical Care Training CenterTODNo ratings yet
- ACLS: Advanced Cardiac Life SupportDocument62 pagesACLS: Advanced Cardiac Life SupportAlemayehu beharuNo ratings yet
- Acls Seminar MeDocument62 pagesAcls Seminar MeAbnet Wondimu100% (1)
- ACLS and MegacodeDocument33 pagesACLS and MegacodeMark Joseph100% (1)
- CPR LectureDocument10 pagesCPR LecturejacnpoyNo ratings yet
- 2021.06.26 L6. Resuscitation Management in Operating Theatre - Ms. Carmen LUIDocument71 pages2021.06.26 L6. Resuscitation Management in Operating Theatre - Ms. Carmen LUIElaine LeeNo ratings yet
- Basic Life Support: Submitted By: Kennedy V. Velasco Bscrim 1-AlphaDocument7 pagesBasic Life Support: Submitted By: Kennedy V. Velasco Bscrim 1-AlphaProsperJuan BelieversNo ratings yet
- IntroductionDocument4 pagesIntroductiondyah ayuNo ratings yet
- Civic Welfare Training ServiceDocument13 pagesCivic Welfare Training ServiceVanessa Rose RofloNo ratings yet
- ACLS Provider Manual 2015 NotesDocument5 pagesACLS Provider Manual 2015 Notescrystalshe93% (14)
- 1 Adult BLS 2021Document29 pages1 Adult BLS 2021pioneergloria51No ratings yet
- BLS Basic Life Support CPR AED SkillsDocument15 pagesBLS Basic Life Support CPR AED SkillsMizzy Wat EvaNo ratings yet
- Cardiac Arrest Management: BLS, ACLS ApproachDocument33 pagesCardiac Arrest Management: BLS, ACLS ApproachTemesgen GeletaNo ratings yet
- Emergency Medicine (1st Year) IFNMUDocument188 pagesEmergency Medicine (1st Year) IFNMUEducation Hub Since 2019No ratings yet
- Cardiorespiratory ArrestDocument51 pagesCardiorespiratory ArrestIrham KhairiNo ratings yet
- DEFIBrilatorDocument43 pagesDEFIBrilatoranon_632568468No ratings yet
- Anzcor Guideline 13 6 Apr 2021Document6 pagesAnzcor Guideline 13 6 Apr 2021Essam HassanNo ratings yet
- Cardiopulmonary Resuscitation (CPR)Document21 pagesCardiopulmonary Resuscitation (CPR)Cristy Guzman100% (1)
- Anzcor Guideline 11 10 1 Als Traumatic Arrest 27apr16Document11 pagesAnzcor Guideline 11 10 1 Als Traumatic Arrest 27apr16Mario Colville SolarNo ratings yet
- ACLSDocument39 pagesACLSJason LiandoNo ratings yet
- Unit 5 Cardiac Emergencies: StructureDocument27 pagesUnit 5 Cardiac Emergencies: StructurebtaleraNo ratings yet
- BLS Healthcare ProvidersDocument8 pagesBLS Healthcare ProviderscmurphNo ratings yet
- Advanced Cardiac Life Support Quick Study Guide 2015 Updated GuidelinesFrom EverandAdvanced Cardiac Life Support Quick Study Guide 2015 Updated GuidelinesRating: 4 out of 5 stars4/5 (6)
- Pediatric Advanced Life Support Quick Study Guide 2015 Updated GuidelinesFrom EverandPediatric Advanced Life Support Quick Study Guide 2015 Updated GuidelinesRating: 5 out of 5 stars5/5 (2)
- Basic Life Support (BLS) Provider HandbookFrom EverandBasic Life Support (BLS) Provider HandbookRating: 5 out of 5 stars5/5 (2)
- Cefepime Protocol 2016-02-26Document7 pagesCefepime Protocol 2016-02-26eryxspNo ratings yet
- Surviving Sepsis Campaign International.15Document67 pagesSurviving Sepsis Campaign International.15Tanawat SingboonNo ratings yet
- SSC Statements Sepsis Definitions 3 2016Document2 pagesSSC Statements Sepsis Definitions 3 2016Satbir SinghNo ratings yet
- CACCN Structure of The ICU (Apr 3 2011)Document3 pagesCACCN Structure of The ICU (Apr 3 2011)eryxspNo ratings yet
- 01 Transforaminal Epidural BlockDocument2 pages01 Transforaminal Epidural BlockeryxspNo ratings yet
- Statement On Patient Information and Informed Consent GqkvktuDocument2 pagesStatement On Patient Information and Informed Consent GqkvktueryxspNo ratings yet
- Society of RadiographersDocument6 pagesSociety of RadiographerseryxspNo ratings yet
- 02 Basic Emergency Echocardiography Emed WebDocument20 pages02 Basic Emergency Echocardiography Emed WeberyxspNo ratings yet
- 00 NephrologyDocument98 pages00 Nephrologyeryxsp0% (1)
- Protocols Checklists Sepsis Alert Wesley HealthcareDocument1 pageProtocols Checklists Sepsis Alert Wesley HealthcareeryxspNo ratings yet
- Caccn STND Crit Care 2009Document24 pagesCaccn STND Crit Care 2009eryxspNo ratings yet
- Web Version ASA Anaesthesia RecordDocument2 pagesWeb Version ASA Anaesthesia RecorderyxspNo ratings yet
- BMUS Safety Guidelines 2009 Revision FINAL Nov 2009 PDFDocument18 pagesBMUS Safety Guidelines 2009 Revision FINAL Nov 2009 PDFeryxspNo ratings yet
- My Pain DiaryDocument2 pagesMy Pain DiaryeryxspNo ratings yet
- Applied Epidural Anatomy CEACCP 2005Document3 pagesApplied Epidural Anatomy CEACCP 2005eryxspNo ratings yet
- Ventilator-Associated Event (VAE)Document6 pagesVentilator-Associated Event (VAE)eryxspNo ratings yet
- Airway Master ClassDocument11 pagesAirway Master ClasselbagouryNo ratings yet
- Outcome Measures For Pain After Surgery - Gordon-ZaslanskyDocument5 pagesOutcome Measures For Pain After Surgery - Gordon-ZaslanskyeryxspNo ratings yet
- Airway Masterclass 2 TOTW 043 2007Document11 pagesAirway Masterclass 2 TOTW 043 2007eryxspNo ratings yet
- Airway Masterclass 1 Philosophy TOTW 012 2005Document10 pagesAirway Masterclass 1 Philosophy TOTW 012 2005eryxspNo ratings yet
- Pain Assessment-New WayDocument5 pagesPain Assessment-New WayeryxspNo ratings yet
- Airway AN0514 WMDocument28 pagesAirway AN0514 WMeryxspNo ratings yet
- (Ultra) Sounding Out A New Way To Treat Chronic Pain - NSF - National Science FoundationDocument2 pages(Ultra) Sounding Out A New Way To Treat Chronic Pain - NSF - National Science FoundationeryxspNo ratings yet
- The 2014 Consensus Guidelines For The Management.1Document3 pagesThe 2014 Consensus Guidelines For The Management.1eryxspNo ratings yet
- Sensory PhysiologyDocument57 pagesSensory PhysiologyeryxspNo ratings yet
- Technical Spec. FLOW-i C20Document2 pagesTechnical Spec. FLOW-i C20eryxspNo ratings yet
- Standardisation of Perioperative Outcome Measures.4Document2 pagesStandardisation of Perioperative Outcome Measures.4eryxspNo ratings yet
- Analgesic6 WhatsNewDocument2 pagesAnalgesic6 WhatsNeweryxspNo ratings yet
- RSUP Dr. Hasan Sadikin Anesthesia CardDocument4 pagesRSUP Dr. Hasan Sadikin Anesthesia CarderyxspNo ratings yet
- CALCULUS PHYSICS MIDTERMDocument41 pagesCALCULUS PHYSICS MIDTERMMACARIO QTNo ratings yet
- Assignment - Final TestDocument3 pagesAssignment - Final TestbahilashNo ratings yet
- Computer Networks Transmission Media: Dr. Mohammad AdlyDocument14 pagesComputer Networks Transmission Media: Dr. Mohammad AdlyRichthofen Flies Bf109No ratings yet
- 2020 Global Finance Business Management Analyst Program - IIMDocument4 pages2020 Global Finance Business Management Analyst Program - IIMrishabhaaaNo ratings yet
- Laryngeal Diseases: Laryngitis, Vocal Cord Nodules / Polyps, Carcinoma LarynxDocument52 pagesLaryngeal Diseases: Laryngitis, Vocal Cord Nodules / Polyps, Carcinoma LarynxjialeongNo ratings yet
- Developing the cycle of maslahah based performance management system implementationDocument27 pagesDeveloping the cycle of maslahah based performance management system implementationM Audito AlfansyahNo ratings yet
- SEC QPP Coop TrainingDocument62 pagesSEC QPP Coop TrainingAbdalelah BagajateNo ratings yet
- CFO TagsDocument95 pagesCFO Tagssatyagodfather0% (1)
- Kalley Ltdn40k221twam Chassis msd6308 SM PDFDocument49 pagesKalley Ltdn40k221twam Chassis msd6308 SM PDFjulio cesar calveteNo ratings yet
- Strategies For StartupDocument16 pagesStrategies For StartupRoshankumar BalasubramanianNo ratings yet
- Week 15 - Rams vs. VikingsDocument175 pagesWeek 15 - Rams vs. VikingsJMOTTUTNNo ratings yet
- White Box Testing Techniques: Ratna SanyalDocument23 pagesWhite Box Testing Techniques: Ratna SanyalYogesh MundhraNo ratings yet
- Flowmon Ads Enterprise Userguide enDocument82 pagesFlowmon Ads Enterprise Userguide ennagasatoNo ratings yet
- KPUPDocument38 pagesKPUPRoda ES Jimbert50% (2)
- Advantages of Using Mobile ApplicationsDocument30 pagesAdvantages of Using Mobile ApplicationsGian Carlo LajarcaNo ratings yet
- Statistical Decision AnalysisDocument3 pagesStatistical Decision AnalysisTewfic SeidNo ratings yet
- EC GATE 2017 Set I Key SolutionDocument21 pagesEC GATE 2017 Set I Key SolutionJeevan Sai MaddiNo ratings yet
- Steps To Christ AW November 2016 Page Spreaad PDFDocument2 pagesSteps To Christ AW November 2016 Page Spreaad PDFHampson MalekanoNo ratings yet
- Checklist of Requirements For OIC-EW Licensure ExamDocument2 pagesChecklist of Requirements For OIC-EW Licensure Examjonesalvarezcastro60% (5)
- Worksheet 5 Communications and Privacy: Unit 6 CommunicationDocument3 pagesWorksheet 5 Communications and Privacy: Unit 6 Communicationwh45w45hw54No ratings yet
- Master SEODocument8 pagesMaster SEOOkane MochiNo ratings yet
- Corporate Governance, Corporate Profitability Toward Corporate Social Responsibility Disclosure and Corporate Value (Comparative Study in Indonesia, China and India Stock Exchange in 2013-2016) .Document18 pagesCorporate Governance, Corporate Profitability Toward Corporate Social Responsibility Disclosure and Corporate Value (Comparative Study in Indonesia, China and India Stock Exchange in 2013-2016) .Lia asnamNo ratings yet
- Brochure en 2014 Web Canyon Bikes How ToDocument36 pagesBrochure en 2014 Web Canyon Bikes How ToRadivizija PortalNo ratings yet
- Indian Journal of Natural Products and Resources Vol 1 No 4 Phytochemical pharmacological profile Cassia tora overviewDocument8 pagesIndian Journal of Natural Products and Resources Vol 1 No 4 Phytochemical pharmacological profile Cassia tora overviewPRINCIPAL BHILWARANo ratings yet
- Damcos Mas2600 Installation UsermanualDocument26 pagesDamcos Mas2600 Installation Usermanualair1111No ratings yet
- EXPERIMENT 4 FlowchartDocument3 pagesEXPERIMENT 4 FlowchartTRISHA PACLEBNo ratings yet
- What's Wrong With American Taiwan Policy: Andrew J. NathanDocument14 pagesWhat's Wrong With American Taiwan Policy: Andrew J. NathanWu GuifengNo ratings yet
- Hipotension 6Document16 pagesHipotension 6arturo castilloNo ratings yet
- Bad DayDocument3 pagesBad DayLink YouNo ratings yet