Professional Documents
Culture Documents
J 1365-2842 2006 01542 X
Uploaded by
dwinugrohojuandaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
J 1365-2842 2006 01542 X
Uploaded by
dwinugrohojuandaCopyright:
Available Formats
Journal of Oral Rehabilitation 2006 33; 152159
Review Article
Dental implants in patients with bruxing habits
F. LOBBEZOO*, J. E. I. G. BROUWERS*, M.S. CUNE & M. NAEIJE* *Department of Oral
Function, Academic Centre for Dentistry Amsterdam (ACTA), Amsterdam and Department of Oral and Maxillofacial Surgery, Prosthodontics
and Special Dental Care, University Medical Center, Utrecht, The Netherlands
SUMMARY Bruxism (teeth grinding and clenching) is careful approach is recommended. There are a few
generally considered a contraindication for dental practical guidelines as to minimize the chance of
implants, although the evidence for this is usually implant failure. Besides the recommendation to
based on clinical experience only. So far, studies to reduce or eliminate bruxism itself, these guidelines
the possible cause-and-effect relationship between concern the number and dimensions of the implants,
bruxism and implant failure do not yield consistent the design of the occlusion and articulation patterns,
and specific outcomes. This is partly because of and the protection of the final result with a hard
the large variation in the literature in terms of both occlusal stabilization splint (night guard).
the technical aspects and the biological aspects of KEYWORDS: bruxism, dental implants, overload, fail-
the study material. Although there is still no proof ure, causality
for the suggestion that bruxism causes an overload
of dental implants and of their suprastructures, a Accepted for publication 3 May 2005
sion criterion for the selection of their participants in
Introduction
clinical studies concerning treatment modalities with
Bruxism is a movement disorder of the masticatory dental implants (e.g. 1416). These authors argue that
system that is characterized, among others, by teeth the overloading influence of bruxism on implants and
grinding and clenching, during sleep as well as during their suprastructures yields a higher risk of biological and
wakefulness (1, 2). Several recent review articles biomechanical complications than would be the case
describe the definitions, epidemiology, (differential) during physiological masticatory activities. However,
diagnosis, aetiology, and treatment of this disorder (3 sound scientific proof for such an argument is never
5). Bruxism is frequently considered an aetiological mentioned. In this review article, aspects of load and
factor for temporomandibular disorders (TMD), tooth overload of dental implants are described and the
wear (e.g. attrition), loss of periodontal support, and available evidence for a possible cause-and-effect rela-
failure of dental restorations, although conflicting tionship between bruxism and implant failure is being
evidence for many of these purported aetiological discussed. Finally, a set of practical guidelines is given for
relationships can be found in the literature (611). clinicians who have indicated a treatment with dental
Bruxism has also been suggested to cause excessive implants in a patient with bruxism.
(occlusal) load of dental implants and their suprastruc-
tures, ultimately resulting in bone loss around the
implants or even in implant failure. Not surprisingly,
(Over) load
bruxism is, therefore, often considered a cause of concern Forces on dental implants are characterized by their
or even a contraindication for implant treatment, as magnitude and direction. An in vivo study by Richter
stated in many textbooks and conference proceedings on (17) has demonstrated maximum vertical forces (load
oral implantology and prosthetic dentistry (e.g. 12, 13). levels) on implants in the premolar region during
In addition, many researchers use bruxism as an exclu- habitual mastication to vary from about 60 N for brittle
2006 Blackwell Publishing Ltd 152
DENTAL IMPLANTS IN BRUXERS 153
foods (crackers) up to 120 N for tough foods (jelly complications. Biological complications can, in turn, be
babies). In the same study, it was shown that maximal divided into early failures and late failures (22). In case
clenching in the intercuspal position, during which not of early failures, osseointegration was insufficient: the
only the implant but the entire dental arch is loaded, implant is lost before the first prosthetic loading. Early
yields maximum vertical forces of about 50 N on the failures, however, may also occur in case of early
implant, while maximal clenching on an occlusal foil, loading (68 weeks after surgery) or immediate loading
inserted at the level of the implant, doubles the (within 2 weeks following surgery) of dental implants.
maximum load levels on the implant. In another In such cases, the implant fails at an early stage, with a
in vivo study, Richter (18) demonstrated that the hori- suprastructure in situ.
zontal components of forces, applied to suprastructures, Contrary to early failures, late biological failures are
result in bending moments of about 90 Nmm for forces characterized by pathological bone loss after full osseo-
in the linguo-buccal direction and of about 170 Nmm integration was obtained at an earlier stage. Such bone
for bucco-lingual forces. These latter forces also yield loss is usually localized around the cervix of the
the highest stress values in the alveolar bone, viz. up to implant, and is considered excessive when the loss is
maximum values of more than 6 MPa at the residual more than 02 mm year)1, after the implant has been
ridge crest on the buccal side. For comparison reasons, functional for 1 year (23). Late biological implant
mesio-distal forces cause a maximum cervical stress of failures are, among others, associated with overload.
about 1 MPa only (18). Some insight into bone physiology is needed for a
The values of the forces and moments, as presented by proper understanding of the mechanisms of excessive
Richter (17, 18), have been established during the bone loss because of overload. Mechanical load causes
performance of conscious oral activities. For unconscious adaptation and remodelling of bone via a process of
oral motor activities like bruxism, such values are not yet resorption and deposition. When similar amounts of
available. Proprioception around dental implants is bone are being resorbed and deposited, equilibrium is
limited because of the absence of a periodontal ligament. present that is characteristic for a physiological loading
Consequently, the proprioceptive feedback mechanisms of bone (24). In case of overload, equilibrium between
to the jaw closing muscles are limited as well. In addition, bone resorption and deposition is being disturbed,
the perception of forces is limited in implant patients thereby causing fatigue-related micro-fractures at, and
(19). It is, therefore, not unlikely that forces that are around, the boneimplant interface (24). These frac-
applied to implants during bruxism are even larger than tures are being repaired by bone resorption and a
those exerted during mastication. Engel et al. (20) claim subsequent ingrowth of connective tissue and epithe-
this to be common knowledge. In other words, chewing lium instead of new bone. This process was derived
is supposed to be a physiological load for dental implants; from animal studies (2527). Likewise, animal studies
bruxism, an overload. also demonstrated that dynamic overload, like teeth
When the term overload is being used, it is impli- grinding, results in excessive angular bone loss (28).
citly suggested that an implant is either in the process of Form the above, the suggestion can be gathered that
ailing or failing, or has already failed (21). According to bruxism is associated with implant failure. Supposedly,
El Askary et al. (21), the warning signs of implant especially the large, laterally directed forces that go
failure are: loosening or fracture of connecting screws with teeth grinding are responsible for this clinical
or abutment (screws), swelling or bleeding of peri- problem.
implant soft tissues, purulent exudate from deep
peri-implant pockets, pain (rare), fracture of supra-
Biomechanical complications
structures, angular bone loss as noted on radiographs,
and chronic infection and soft tissue sloughing during In case of biomechanical complications, one or more
the healing phase following first-stage surgery. components of an implant system fail, e.g. fracture of
an implant itself, loosening or fracture of connecting
screws or abutment screws, loosening or excessive wear
Biological complications
of mesostructural components in overdentures, and
The consequences of overload of dental implants can be excessive wear or fracture of suprastructural porcelain
divided into two groups: biological and biomechanical or acrylic teeth (29, 30).
2006 Blackwell Publishing Ltd, Journal of Oral Rehabilitation 33; 152159
154 F . L O B B E Z O O et al.
Especially, the loosening of screwnut attachments in prospective approach of the study sample is required; it
prosthetic constructions occurs relatively frequent (31). is not possible to establish the order of events retro-
The preload of the screw (i.e. the tensile force estab- spectively. Moreover, it is essential to include multiple
lished in the screw after tightening) and the clamping evaluations over time in the study design. Many studies
force between the surfaces of screw and nut stabilize to the association between bruxism and implant failure,
the attachments. The screw loosens when the occlusal however, have a retrospective design (e.g. 33, 35) or
forces on the prosthetic construction exceed these even have the format of a case report (e.g. 36).
stabilizing forces (32). Obviously, the larger the forces Therefore, these studies are difficult to interpret. For-
on the construction, the sooner loosening will occur. tunately, several studies do have a prospective design.
Fractures of implants and screws happen only seldom Lindquist et al. (37) presented a 15-year prospective
(29). Pre-disposing factors are thin implants and loss of study, during which five evaluations were performed.
bone till a weak part of the implant, which is mostly at They concluded that clenching was not significantly
the level where the abutment screw ends. The fracture correlated with marginal bone loss and did not lead to
of a connecting screw of implant components is usually problems with suprastructures. Given the strong study
preceded by a stage of screw loosening (33). Connecting design, this conclusion is important for the final
screws mostly fracture at the level where the screw judgement of the purported causal relationship that is
thread part ends. being evaluated in the present article. Contrary to the
conclusion of Lindquist et al. (37), several other
prospective studies, although covering shorter study
Causality
periods than in the study by Lindquist et al. do report
To present convincing evidence for the possibility that significant associations between bruxism and problems
bruxism leads to failure of dental implants, a cause-and- with dental implants or their suprastructures. Wannfors
effect relationship needs to be established. The criteria et al. (38) reported a significant relationship between
for a valid causal relationship are summarized in bruxism and implant failure after the implants have
Table 1, following the guidelines proposed by Spilker been functional for 1 year. Likewise, Glauser et al. (39)
(34). found a higher percentage of implant loss in bruxists
The first criterion in Table 1, viz. the absence of bias than in non-bruxists (41% versus 12%, after 1 year).
and confounding factors, is not met in articles that deal Bragger et al. (40) even reported technical problems
with the association between bruxism and failure of with implants in 60% of their bruxists over 5 years, as
dental implants: none of the below-cited articles is compared with about 20% in their non-bruxists.
completely free of bias and confounders. For sake of Interestingly, in contrast with their later findings in
conciseness, no details will be presented, but a convin- 1996 (37), Lindquist et al. conclude in 1988 (41) that
cing example of the vast presence of bias is the fact that clenching does contribute significantly to marginal
a diagnosis of bruxism, being an oral movement bone loss over a 6-year period. Taken all evidence
disorder with two faces (dynamic teeth grinding and together, the prospective studies do not have unequi-
static clenching), is difficult to establish (see below). vocal outcomes. Nevertheless, the available evidence
As a second criterion for a valid cause-and-effect slightly tends to confirm the presence of a causal
relationship, the suggested cause (i.e. bruxism) should relationship between bruxism and implant failure.
precede the effect (i.e. implant failure). To that end, a To fulfil the third criterion for a causal relationship,
the association between bruxism and implant failure
needs to be plausible from an epidemiological point of
Table 1 Criteria for establishing causation [after Spilker (34)]
view. About 620% of the general adult population
reports bruxism (for a review, see 7). Given the high
Cause-and-effect criteria
Bias and confounding factors are absent success rates for most dental implant systems, it is
The cause precedes the effect therefore unlikely that all implants fail in the presence
The association makes epidemiological sense of bruxism. On the other hand, it is possible that
A doseresponse gradient is present bruxism is a commonly used contraindication for
The association is specific
implant procedures, so that the presence of bruxism
The association is consistent
in populations of implant patients is lower than that in
2006 Blackwell Publishing Ltd, Journal of Oral Rehabilitation 33; 152159
DENTAL IMPLANTS IN BRUXERS 155
the general population. Unfortunately, there is no very suitable for the quantification of bruxism. In the
research available about this subject. The usually high study sample of Tosun et al. (44), implant failure was
success rates of implant procedures, which sometimes found in 5% of the cases. PSG recordings of this 5%-
reach up to almost 99% (37), indicate that implant subsample revealed the presence of sleep bruxism in
failure is an exception rather than the rule. As a about one-third of the cases. Unfortunately, the uncon-
consequence, studies to factors that contribute to trolled character of this study prevents an unequivocal
implant failure, such as bruxism, need to include large interpretation of this outcome. In the other studies, to
samples as to ascertain large-enough numbers of which this review refers, bruxism was determined
failures. anamnestically and/or clinically, so that no reliable
The literature does indicate that in studies, in which diagnosis of bruxism was established in these studies. In
bruxism was used as an exclusion criterion, success some of the articles, the mode of bruxism determin-
rates of about 95% are found after 1824 months ation is not given at all. From the above, it is clear that
(1416), while for studies that included bruxism the existence of a causal relationship between bruxism
patients in their study sample, lower success rates are and implant failure cannot be proven on the basis of the
reported, i.e. about 80% after 12 years (39, 42). On fourth criterion in Table 1.
the other hand, some studies report high success rates The more specific the association is, the likelier the
despite the inclusion of bruxists in the study popula- causal character of the relationship of interest (Table 1,
tion. For example, the cumulative success rate after criterion 5). In other words, when fewer factors are
6 years varies between 92 and 95% in a study by involved in the failure of dental implants, this criterion
Quirynen et al. (43), while Lidquist et al. (37) reported a is better fulfilled. Most studies, however, indicate that
success rate of almost 99% after 15 years. In other multiple factors play a role in implant failure: bruxism,
words, epidemiological data yield equivocal results with but also (and may be even more importantly) smoking
regard to the purported causal relationship between (37), a bad oral hygiene (37, 41), post-operative
bruxism and implant failure. Hence, the third criterion infections (38), and a poor bone quality (39). Possibly,
in Table 1 is not fulfilled unequivocally. the simultaneous presence of multiple factors leads to
According to the fourth criterion for a valid cause- multiple implant failures at the same time (35). In
and-effect relationship, a doseresponse gradient needs short, the failure of dental implants is not specifically
to be present. Although on the response side, efforts because of bruxism. The fifth criterion is thus not
have been undertaken to collect sufficient evidence (for fulfilled.
example the amount of marginal bone loss is suitable Finally, according to the sixth criterion in Table 1,
for quantifying the response), on the side of the dose the association between bruxism and implant failure
only little has been carried out so far to quantify needs to be consistent. From the above description
bruxism. Engel et al. (20) use the amount of tooth wear about the other criteria for valid cause-and-effect
as a measure of parafunctional activities. These authors relationships, it can be gathered that bruxism some-
found no association between tooth wear and marginal times can, and at other times cannot, be associated with
bone loss. In the discussion of their paper, they the failure of dental implants. Hence, the sixth criterion
elaborate on the disadvantages of their measure for is not fulfilled either.
bruxism, which, among others, can be the result of Taking all evidence together, it must be concluded
teeth grinding, but not of clenching. On top of that, the that so far, the proof for a cause-and-effect relationship
clinical distinction between attrition and other types of between bruxism and implant failure is insufficient:
tooth wear, like erosion, is sometimes difficult. Further, only the second criterion partly contributes to the
the observed tooth wear may have happened in the evidence. Future studies need to be designed as to
past while at the time of the clinical evaluation, specifically address this purported causal relationship.
bruxism is no longer present. Finally, it is difficult, if
not impossible, to determine the amount of tooth wear
Discussion
on restored teeth. In contrast to Engel et al. (20), Tosun
et al. (44) used the current gold-standard technique for From the above paragraphs, it can be gathered that the
the establishment of a diagnosis of sleep bruxism, viz. a various biomechanical, epidemiological, and experi-
sleep recording (polysomnography; PSG) (3). PSG is mental (clinical) studies yield contradictory results in
2006 Blackwell Publishing Ltd, Journal of Oral Rehabilitation 33; 152159
156 F . L O B B E Z O O et al.
relation to the question whether or not bruxism may implant failure and who want to enable a comparison
lead to the failure of dental implant procedures. Apart with other researchers studies to this relationship at
from the fact that the association under study only the same time. At least, authors should describe the
partly fulfils the criteria for a valid causal relationship, factors mentioned in the table, so that the reader can
there is a large variation between studies in both the identify the differences and similarities between studies.
technical aspects (i.e. related to the implants and their The many possible combinations in Table 2 also dem-
suprastructures) as well as the biological aspects (i.e. onstrate that the subject of this review still offers a lot of
related to the patients) of the material under examina- challenges.
tion: there are hardly any studies whose materials are
fully comparable. This further complicates the inter-
Practical guidelines
pretation of the literature about this subject. Moreover,
there is also a lot of variation in the mode, duration, Although so far, there is no convincing evidence that
and frequency of the evaluations as well as in the study bruxism causes an overload of dental implants and their
design. For example, a large part of the current suprastructures, practitioners better proceed carefully
knowledge about loading of dental implants is derived when planning implant procedures in bruxists, given
from studies using finite element models (e.g. 45). the seriousness of the possible complications. Below,
However, because of the assumptions that are part of some practical guidelines are given as to reduce the risk
such mathematical models, one cannot easily extrapo- of complications and, ultimately, implant failure. It
late the findings to the clinical situation (46). Unfortu- should be stressed that, because of the lack of a solid
nately, a clinical verification of the outcomes of finite scientific foundation, the guidelines are not evidence
element analyses is not easy to perform for ethical and based, but rather experience based: they are mainly
practical reasons. extracted from expert papers on this subject. All
Table 2 gives an impression of the many factors that guidelines aim to minimize the forces that are applied
should be taken into account by researchers, who want to the implants.
to study the causal relationship between bruxism and A frequent advice is related to the number of
implants. In the presence of bruxism, most authors
Table 2 Overview of factors that can differ among studies to the recommend to place more implants than would have
possible causal relationship between bruxism and implant failure been necessary in the absence of this movement
disorder. More specifically, as to avoid free-ending
Implant-related factors situations, one implant should be placed for each
Environment: edentulous, partially dentate
missing element (21, 32). This recommendation is
Position: upper, lower, anterior, posterior
supported by the findings of in vivo studies that
Number: ranging from 2 per jaw up to 1 per element
Implant: shape, material, length, diameter indicate a reduction of the forces that are being
Suprastructure: fixed, removable exerted on an individual implant when the number
Attachment: bar (extensions yes/no), ball of implants increases (47). Of course, given the costs
Loading: immediate, early, late and the irreversible nature of placing more implants,
Occlusion: area contact, point contact
careful clinical decision-making should be built into
Articulation: balanced, cuspid guidance
Prevention of failure: stabilization splint yes/no the treatment plan. In addition, mechanically con-
Patient-related factors necting the implants leads to a better distribution of
Age the forces and a reduction of the stresses in the bone
Gender around the implants (48). Interestingly, the type of
General health: complication yes/no
mesostructure (bar with or without extension; ball),
Oral health: complications yes/no
from which the overdenture obtains its retention, is
Bruxism: present yes/no
Evaluation-related factors not a factor that needs to be taken into account in
Frequency edentulous bruxists (49). A final recommendation
Duration: short-term, long-term regarding the implants themselves is related to their
Design: retrospective, prospective length and diameter: longer implants with a larger
Implant failure: criteria yes/no
diameter help to keep the stresses in the bone as low
Bruxism: oral history, inspection, polysomnography
as possible (21, 50).
2006 Blackwell Publishing Ltd, Journal of Oral Rehabilitation 33; 152159
DENTAL IMPLANTS IN BRUXERS 157
According to Esposito et al. (51), the literature does References
not yet indicate how predicable early loading or
1. Thorpy MJ. Parasomnias. In: Thorpy MJ, ed. International
immediate loading of dental implants is. Caution is, Classification of Sleep Disorders: Diagnostic and Coding
therefore, recommended when using either of these Manual. Rochester, MN: Allen Press; 1990:142185.
techniques, especially in bruxists. Most authors agree 2. Okeson JP. Orofacial Pain. Guidelines for assessment, diag-
that in occlusion, the prosthetic rehabilitation should nosis, and management. Chicago, IL: Quintessence Publishing
have single point contacts as close to the centre of the Co., Inc.; 1996.
3. Lavigne GJ, Manzini C. Sleep bruxism and concomitant motor
implant as possible. Articulation should be character-
activity. In: Kryger M, Roth T, Dement WC, eds. Principles
ized by flat incline planes of the cusps as to protect the and practice of sleep medicine. Philadelphia, PA: WB Saun-
implant system against the lateral components of the ders Co.; 2000:773785.
forces that are being exerted during, for example, teeth 4. Lobbezoo F, Naeije M. Bruxism is mainly regulated centrally,
grinding (5254). Research using finite element models not peripherally. J Oral Rehabil. 2001a;28:10851091.
5. Kato T, Thie NMR, Huynh N, Miyawaki S, Lavigne GJ. Topical
has indicated that especially non-axial, horizontal
review: sleep bruxism and the role of peripheral sensory
forces result in high tensions around the cervix of an influences. J Orofacial Pain. 2003;17:191213.
implant (45). 6. Lavigne GJ, Rompre PH, Montplaisir JY, Lobbezoo F. Motor
A hard stabilization splint for nightly use (night activity in sleep bruxism with concomitant jaw muscle pain: a
guard) contributes to optimally distributing, and ver- retrospective pilot study. Eur J Oral Sci. 1997;105:9295.
tically redirecting, the forces that go with nocturnal 7. Lobbezoo F, Lavigne GJ. Do bruxism and temporomandibular
disorders have a cause-and-effect relationship? J Orofacial
teeth grinding and clenching (21, 32, 50, 5355).
Pain. 1997;11:1523.
Finally, most authors recommend to at least try to 8. John MT, Frank H, Lobbezoo F, Drangsholt M, Dette KE. No
minimize or, even better, eliminate bruxism behaviour association between incisal tooth wear and temporomandib-
in implant patients. However, such efforts require ular disorders. J Prosthet Dent. 2002;87:197203.
difficult, and often multidisciplinary, treatments with 9. Lavigne GJ, Kato T, Kolta A, Sessle BJ. Neurobiological
mechanisms involved in sleep bruxism. Crit Rev Oral Biol
unpredictable outcomes (3, 56).
Med. 2003;14:3046.
10. Hirsch C, John MT, Lobbezoo F, Setz JM, Schaller HG. Incisal
tooth wear and self-reported temporomandibular disorder
Conclusion
pain in children and adolescents. Int J Prosthodont.
Bruxism is generally considered a contraindication for 2004;17:151156.
dental implants, although the evidence for this is 11. Lobbezoo F, van der Zaag J, Visscher CM, Naeije M. Oral
kinesiology. A new postgraduate programme in The Nether-
usually based on clinical experience only. So far,
lands. J Oral Rehabil. 2004;31:192198.
studies to the possible cause-and-effect relationship 12. Lundgren D, Laurell L. Occlusal aspects if fixed bridgework
between bruxism and implant failure do not yield supported by endosseous implants. In: Lang NP, Karring T,
consistent and specific outcomes. This is partly because eds. Proceedings of the 1st European workshop in periodon-
of the large variation in the literature in terms of both tology. London: Quintessence Books; 1994:326327.
13. Palmer RM, Smith BJ, Howe LC, Palmer PJ. Complications
the technical aspects and the biological aspects of the
and maintenance: single tooth and fixed bridge. In: Palmer
study material. Nevertheless, given the seriousness of RM, Smith BJ, Howe LC, Palmer PJ, eds. Implants in clinical
possible biological and biomechanical complications, dentistry. London: Martin Dunitz Ltd; 2002:241.
careful pre-surgical planning and (post-) prosthetic 14. Becker W, Becker BE. Replacement of maxillary and man-
preventive measures should be given consideration in dibular molars with single endosseous implant restorations: a
bruxists. retrospective study. J Prosthet Dent. 1995;74:5155.
15. Colomina LE. Immediate loading of implant-fixed mandibular
prosthesis: a prospective 18-month follow-up clinical study
Acknowledgments preliminary report. Implant Dent. 2001;10:2329.
16. Vanden Bogaerde L, Pedretti G, Dellacasa P, Mozzati M,
This paper is an adapted and translated version of the Rangert B. Early function of splinted implants in maxillas and
Dutch article Lobbezoo F, Brouwers JEIG, Cune MS, posterior mandibles using Branemark system machined-sur-
face implants: an 18-month prospective clinical multicenter
Naeije M. Tandheelkundige implantaten bij bruxisten.
study. Clin Implant Dent Relat Res. 2003;5:2127.
Ned Tijdschr Tandheelkd 2004;111:85-90, with per- 17. Richter EJ. In vivo vertical forces on implants. Int J Oral
mission from The Nederlands Tijdschrift voor Tandhe- Maxillofac Implants. 1995;10:99108.
elkunde B.V., Nieuwegein, The Netherlands.
2006 Blackwell Publishing Ltd, Journal of Oral Rehabilitation 33; 152159
158 F . L O B B E Z O O et al.
18. Richter EJ. In vivo horizontal bending moments on implants. 37. Lindquist LW, Carlsson GE, Jemt T. A prospective 15-year
Int J Oral Maxillofac Implants. 1998;13:232244. follow-up study of mandibular fixed prostheses supported by
19. Hammerle CH, Wagner D, Bragger U, Lussi A, Karayiannis A, osseointegrated implants. Clin Oral Implant Res. 1996;7:329
Joss A, Lang NP. Threshold of tactile sensitivity perceived with 336.
dental endosseous implants and natural teeth. Clin Oral 38. Wannfors K, Johansson B, Hallman M, Strandkvist T. A
Implants Res. 1995;6:8390. prospective randomized study of 1- and 2-stage sinus inlay
20. Engel E, Gomez-Roman G, Axmann-Krcmar D. Effect of bone grafts: 1-year follow-up. Int J Oral Maxillofac Implants.
occlusal wear on bone loss and Periotest value of dental 2000;15:625632.
implants. Int J Prosthodont. 2001;14:144150. 39. Glauser R, Ree A, Lundgren AK, Gottlow J, Hammerle CHF,
21. El Askary AS, Meffert RM, Griffin T. Why do dental implants Scharer P. Immediate occlusal loading of Branemark
fail? Part I. Implant Dent. 1999;8:173185. implants applied in various jawbone regions: a prospective,
22. Tonetti MS, Schmid J. Pathogenesis of implant failures. 1-year clinical study. Clin Implant Dent Relat Res. 2001;
Periodontology 2000. 1994;4:127138. 3:204213.
23. Albrektsson T, Zarb G, Eriksson AR. The long-term efficacy of 40. Bragger U, Aeschlimann S, Burgin W, Hammerle CHF, Lang
currently used dental implants: a review and proposed criteria NP. Biological and technical complications and failures with
of success. Int J Oral Maxillofac Implants. 1986;1:1125. fixed partial dentures (FPD) on implants and teeth after
24. Brunsky JB. In vivo bone response to biomechical loading at the four to five years of function. Clin Oral Implant Res. 2001;
bone-dental implant interface. Adv Dent Res. 1999;13:88119. 12:2634.
25. Hoshaw SJ, Brunski JB, Cochran GVB. Mechanical overload- 41. Lindquist LW, Rockler B, Carlsson GE. Bone resorption
ing of Branemark implants affects interfacial bone modeling around fixtures in edentulous patients treated with mandib-
and remodelling. J Oral Surg. 1994;9:345360. ular fixed tissue-integrated prostheses. J Prosthet Dent.
26. Isidor F. Loss of osseointegration caused by occlusal load of 1988;59:5966.
oral implants. A clinical and radiographic study in monkeys. 42. Eckert SE, Meraw SJ, Weaver AL, Loshe CM. Early experience
Clin Oral Implants Res. 1996;7:143152. with wide-platform Mk II implants. Part I: implant survival.
27. Isidor F. Histological evaluation of peri-implant bone at Part II: evaluation of risk factors involving implant survival.
implants subjected to occlusal overload or plaque accumula- Int J Oral Maxillofac Implants. 2001;16:208216.
tion. Clin Oral Implants Res. 1997;8:19. 43. Quirynen M, Naert I, van Steenberghe D, Nys L. A study of
28. Duyck J, Ronold HJ, Van Oosterwyck H, Naert I, Vander 589 consecutive implants supporting complete fixed pros-
Sloten J, Ellingsen JE. The influence of static and dynamic theses. Part I: periodontal aspects. J Prosthet Dent.
loading on marginal bone reactions around osseointegrated 1992;68:655663.
implants: an animal experimental study. Clin Oral Implants 44. Tosun T, Karabuda C, Cuhadaroglu C. Evaluation of sleep
Res. 2001;12:207218. bruxism by polysomnographic analysis in patients with
29. Berglundh T, Persson L, Klinge B. A systematic review of the dental implants. Int J Oral Maxillofac Implants. 2003;
incidence of biological and technical complications in implant 18:286292.
dentistry reported in prospective longitudinal studies of at 45. OMahony A, Bowles Q, Woolsey G, Robinson SJ, Spencer P.
least 5 years. J Clin Periodontol. 2002;29:197212. Stress distribution in the single-unit osseointegrated dental
30. Gothberg C, Bergendal T, Magnusson T. Complications after implant: finite element analyses of axial and off-axial loading.
treatment with implant-supported fixed prostheses: a retro- Implant Dent. 2000;9:207218.
spective study. Int J Prosthodont. 2003;16:201217. 46. Geng JP, Tan KBC, Liu GR. Application of finite element
31. Hemmings KW, Schmitt A, Zarb GA. Complications and analysis in implant dentistry: a review of the literature.
maintenance requirements for fixed prostheses and overden- J Prosthet Dent. 2001;85:585598.
tures in the edentulous mandible: a 5 year report. Int J Oral 47. Duyck J, Van Oosterwyck H, Vander Sloten J, De Cooman M,
Maxillofac Implants. 1994;9:191196. Puers R, Naert I. Magnitude and distribution of occlusal forces
32. Hurson S. Practical clinical guidelines to prevent screw on oral implants supporting fixed prostheses: an in vivo study.
loosening. Int J Dent Symp. 1995;3:2225. Clin Oral Implants Res. 2000;11:465475.
33. Rangert B, Krogh PHJ, Langer B, Van Roekel N. Bending 48. Guichet DL, Yoshinobu D, Caputo AA. Effect of splinting and
overload and implant fracture: a retrospective clinical analysis. interproximal contact tightness on load transfer by implant
Int J Oral Maxillofac Implants. 1995;10:326334. restorations. J Prosthet Dent. 2002;87:528535.
34. Spilker B. Guide to clinical trials. New York: Raven Press; 1991. 49. Duyck J, Van Oosterwyck H, Vander Sloten J, De Cooman M,
35. Ekfeldt A, Christansson U, Eriksson T, Linden U, Lundqvist S, Puers R, Naert I. In vivo forces on oral implants supporting a
Rundcrantz T, Johansson LA , Nilner K, Billstrom C. A mandibular overdenture: the influence of attachment system.
retrospective analysis of factors associated with multiple Clin Oral Invest. 1999;3:201207.
implant failures in maxillae. Clin Oral Implant Res. 50. Misch CE. The effect of bruxism on treatment planning for
2001;12:462467. dental implants. Dentistry Today. 2002;21:7681.
36. Piattelli A, Piattelli M, Scarano A, Montesani L. Light and 51. Esposito M, Worthington HV, Coulthard P. Interventions for
scanning electron microscopic report on four fractured replacing missing teeth: different times for loading dental
implants. Int J Oral Maxillofac Implants. 1998;13:561564. implants. Cochrane Database Syst Rev. 2003;1:CD003878.
2006 Blackwell Publishing Ltd, Journal of Oral Rehabilitation 33; 152159
DENTAL IMPLANTS IN BRUXERS 159
52. Strazzeri AJ. Applied harmonious occlusion and plaque 56. Lavigne GJ, Goulet JP, Zuconni M, Morisson F, Lobbezoo F.
prevention most important in implant success. Oral Implantol. Sleep disorders and the dental patient: a review of
1975;5:369377. diagnosis, pathophysiology and management. Oral Surg
53. McCoy G. Occlusion and implants. Dentistry Today. Oral Med Oral Pathol Oral Radiol Endod. 1999;88:257
1997;16:108111. 272.
54. McCoy G. Recognizing and managing parafunction in the
reconstruction and maintenance of the oral implant patient. Correspondence: Dr Frank Lobbezoo, Department of Oral Function,
Implant Dent. 2002;11:1927. Academic Centre for Dentistry Amsterdam (ACTA), Louwesweg 1,
55. Perel ML. Parafunctional habits, nightguards, and root form 1066 EA Amsterdam, The Netherlands.
implants. Implant Dent. 1994;3:261263. E-mail: f.lobbezoo@acta.nl
2006 Blackwell Publishing Ltd, Journal of Oral Rehabilitation 33; 152159
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- (14523701 - Serbian Dental Journal) Music As An Alternative Therapy Method in DentistryDocument6 pages(14523701 - Serbian Dental Journal) Music As An Alternative Therapy Method in DentistrydwinugrohojuandaNo ratings yet
- Effects of Adhesive Used As Modeling Liquid On The Stability of The Color and Opacity of CompositesDocument7 pagesEffects of Adhesive Used As Modeling Liquid On The Stability of The Color and Opacity of CompositesdwinugrohojuandaNo ratings yet
- Drg. Lies - Diagnosos & PrognosisDocument95 pagesDrg. Lies - Diagnosos & PrognosisdwinugrohojuandaNo ratings yet
- Tamfelj 2014 International Endodontic JournalDocument2 pagesTamfelj 2014 International Endodontic JournaldwinugrohojuandaNo ratings yet
- The Concept of Radiation-Enhanced Stem Cell Differentiation: Research ArticleDocument8 pagesThe Concept of Radiation-Enhanced Stem Cell Differentiation: Research ArticledwinugrohojuandaNo ratings yet
- Author:Dwi Nugroho Juanda Department: Institution:: Faculty of Dentistry Trisakti UniversityDocument2 pagesAuthor:Dwi Nugroho Juanda Department: Institution:: Faculty of Dentistry Trisakti UniversitydwinugrohojuandaNo ratings yet
- Tips To Minimize Occlusal Corrections: Janos GroszDocument11 pagesTips To Minimize Occlusal Corrections: Janos GroszdwinugrohojuandaNo ratings yet
- Stability of Implant-Abutment Interface With A Hexagon-Mediated Butt Joint: Failure Mode and Bending ResistanceDocument8 pagesStability of Implant-Abutment Interface With A Hexagon-Mediated Butt Joint: Failure Mode and Bending ResistancedwinugrohojuandaNo ratings yet
- Chlorhexidine Preserves Dentin Bond in Vitro: Research ReportsDocument5 pagesChlorhexidine Preserves Dentin Bond in Vitro: Research ReportsdwinugrohojuandaNo ratings yet
- Omi 15 5 Sykara7Document16 pagesOmi 15 5 Sykara7dwinugrohojuandaNo ratings yet
- J 1600-0757 1998 tb00129 PDFDocument6 pagesJ 1600-0757 1998 tb00129 PDFdwinugrohojuandaNo ratings yet
- Biomechanical Effects of Double or Wide Implants For Single Molar Replacement in The Posterior Mandibular RegionDocument4 pagesBiomechanical Effects of Double or Wide Implants For Single Molar Replacement in The Posterior Mandibular RegiondwinugrohojuandaNo ratings yet
- A Clinical Investigation of The Morphological Changes in The Posterior Mandible When Implant-Retained Overdentures Are UsedDocument9 pagesA Clinical Investigation of The Morphological Changes in The Posterior Mandible When Implant-Retained Overdentures Are UseddwinugrohojuandaNo ratings yet
- KjadksjkajdkajsDocument8 pagesKjadksjkajdkajsdwinugrohojuandaNo ratings yet
- MTT Proliferation Assay ProtocolsdaDocument2 pagesMTT Proliferation Assay ProtocolsdadwinugrohojuandaNo ratings yet
- Force Transmission of One-And Two - Piece Morse-Taper Oral Implants: A Nonlinear Finite Element AnalysisDocument9 pagesForce Transmission of One-And Two - Piece Morse-Taper Oral Implants: A Nonlinear Finite Element AnalysisdwinugrohojuandaNo ratings yet
- Dentures Are A Reservoir For Respiratory PathogensDocument7 pagesDentures Are A Reservoir For Respiratory PathogensdwinugrohojuandaNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Assessment and Re-Assessment of Patients According To The Scope of ServiceDocument9 pagesAssessment and Re-Assessment of Patients According To The Scope of Servicegiya nursingNo ratings yet
- Adverse Eventsd DefinitionsDocument30 pagesAdverse Eventsd Definitionsika sartikaNo ratings yet
- How To Critically Appraise A PaperDocument6 pagesHow To Critically Appraise A PaperAmbar RahmanNo ratings yet
- ORAL REVALIDA (Diabetes Mellitus)Document5 pagesORAL REVALIDA (Diabetes Mellitus)Aubrey Unique EvangelistaNo ratings yet
- Polycythemia Vera: DR - Karthik.S Moderator:Dr - Sumedh ShettyDocument51 pagesPolycythemia Vera: DR - Karthik.S Moderator:Dr - Sumedh ShettyDr. Apoorva KottaryNo ratings yet
- To Hospitals & Hospital PhrmacyDocument27 pagesTo Hospitals & Hospital PhrmacyBvayNo ratings yet
- Elements of Medical NegligenceDocument4 pagesElements of Medical NegligenceGuevarra RemNo ratings yet
- Pharmacology For Nurses: A Pathophysiologic Approach: Fifth EditionDocument31 pagesPharmacology For Nurses: A Pathophysiologic Approach: Fifth Editionadni_wgNo ratings yet
- Monaco Treatment Planning Enhances Departmental EfficienciesDocument9 pagesMonaco Treatment Planning Enhances Departmental Efficienciesricky rdnNo ratings yet
- 2009-SUPPORT Tools For Evidence-Informed Policymaking in Health 18-Planning Monitoring and Evaluation of PoliciesDocument8 pages2009-SUPPORT Tools For Evidence-Informed Policymaking in Health 18-Planning Monitoring and Evaluation of PoliciesJULIO CESAR MATEUS SOLARTENo ratings yet
- Management of Perio Prostho Situations in DentistryDocument18 pagesManagement of Perio Prostho Situations in DentistryHarsha ReddyNo ratings yet
- 2017 MMSR Book Final For ViewDocument168 pages2017 MMSR Book Final For ViewWael Yacoub67% (6)
- Miscarriage or Early Pregnancy Loss-Diagnosis and ManagementDocument22 pagesMiscarriage or Early Pregnancy Loss-Diagnosis and ManagementherryNo ratings yet
- Romano Et Al-2024-Cochrane Database of Systematic ReviewsDocument111 pagesRomano Et Al-2024-Cochrane Database of Systematic Reviewsaraujoaoh07No ratings yet
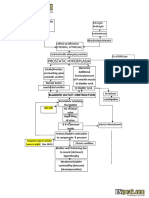
- Benign Prostatic Hyperplasia - BPH - Pathophysiology - Schematic DiagramDocument2 pagesBenign Prostatic Hyperplasia - BPH - Pathophysiology - Schematic DiagramSimran JosanNo ratings yet
- Postpartum Abdominal PainDocument4 pagesPostpartum Abdominal PainPinto ModakNo ratings yet
- VET0811 SeDocument6 pagesVET0811 SeterrywinkleNo ratings yet
- Reflective Essay Samantha JohnsonDocument5 pagesReflective Essay Samantha Johnsonapi-329945753No ratings yet
- Terapi CompressionDocument10 pagesTerapi CompressionErlinda KarimNo ratings yet
- Ontario - Schedule of Benefits 2021Document970 pagesOntario - Schedule of Benefits 2021Raj LoganathanNo ratings yet
- Etiologi Krisis Tiroid Dan Koma MiksedemaDocument4 pagesEtiologi Krisis Tiroid Dan Koma MiksedemaRaafi Puristya Aries DarmawanNo ratings yet
- TheileriaDocument42 pagesTheileriaMEENU MANOHARNo ratings yet
- OP4OT1 - Ocular Pharmacol - Therapeutics 2011-12Document6 pagesOP4OT1 - Ocular Pharmacol - Therapeutics 2011-12Aoy RangsimaNo ratings yet
- HemoglobinopathiesDocument10 pagesHemoglobinopathiespriscillaNo ratings yet
- Chapter 14 - Fluid and Electrolytes - Balance and DisturbanceDocument20 pagesChapter 14 - Fluid and Electrolytes - Balance and DisturbanceEmily Cormier100% (1)
- Practice Nurseled Proactive Care For Chronic Depression in Primary Care A Randomised Controlled TrialDocument7 pagesPractice Nurseled Proactive Care For Chronic Depression in Primary Care A Randomised Controlled TrialIndah SundariNo ratings yet
- SurvivalDocument61 pagesSurvivalsgod34No ratings yet
- PatellofemuralDocument216 pagesPatellofemuralandrei_costea100% (2)
- Publication Price List-1Document2 pagesPublication Price List-1Vinayak AmteNo ratings yet
- Hiatus Hernia - Chinese Herbs, Chinese Medicine, AcupunctureDocument6 pagesHiatus Hernia - Chinese Herbs, Chinese Medicine, AcupunctureCarlCordNo ratings yet