Professional Documents
Culture Documents
Aggressive Combined Modality Therapy For Recurrent Colon CA - Overman2008
Uploaded by
Joy GhoseOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Aggressive Combined Modality Therapy For Recurrent Colon CA - Overman2008
Uploaded by
Joy GhoseCopyright:
Available Formats
Case Report
Aggressive Combined Modality Therapy for
Recurrent Colorectal Cancer Involving the
Duodenum and Pancreas: A Report of 5 Cases
Michael J. Overman,1 David Fogelman,1 Aref Al-Kali,2 Christopher H. Crane,3
Douglas Evans,4 Eddie K. Abdalla,4 Peter Pisters,4 Scott Kopetz,1
Cathy Eng,1 Robert A. Wolff1
Abstract
We report 5 cases in which the recurrence of colorectal cancer (CRC) presented as a mass involving the duodenum
and pancreas. The treatment approach for such recurrences is not standardized, and in particular, the benets of pan-
creaticoduodenectomy for such cases are not known. We describe the successful use of aggressive multimodality
treatment with chemotherapy, radiation, and en bloc surgical resection. Such trimodality therapy can result in durable
palliation of symptoms and long-term survival for patients with recurrent CRC involving the duodenum and pancreas,
even when other metastases are present.
Clinical Colorectal Cancer, Vol. 7, No. 5, 338-342, 2008; DOI: 10.3816/CCC.2008.n.045
Keywords: Adenocarcinoma, Capecitabine, Pancreaticoduodenectomy, Relapse, Resection, Trimodality
Introduction creaticoduodenectomy.5-7 Though much rarer, recurrent CRC involv-
For locally advanced colorectal cancers (CRCs) that invade or ing the duodenum and pancreas can result from a local recurrence of
adhere to adjacent organs or structures, en bloc resection of all a right-sided colon cancer, extension from neighboring lymph nodes,
involved structures is considered the standard of care. For example, in or hematogenous metastasis.8,9 At present, the therapeutic paradigm
cases of locally recurrent rectal cancer, aggressive surgery, often requir- for recurrent colon cancer involving the duodenum and pancreas is
ing pelvic exenteration, is considered the standard of care, particularly not well defined.
when negative resection margins are achievable.1,2 In addition, resec- In this case series, we present 5 cases treated at The University
tion of metastatic deposits in the liver or lung has demonstrated clear of Texas M. D. Anderson Cancer Center (MDACC). Information
improvements in survival, with curative potential.3,4 regarding these 5 cases was obtained under an institutional review
Given the close anatomic relationship between the hepatic flexure, boardapproved protocol and represents a collection of selected
the second portion of the duodenum, and the head of the pancreas, cases evaluated at MDACC from 2001 to 2005. These cases illus-
invasion of these sites by a locally advanced right-side colon cancer is trate the biologic mechanisms of recurrence at the duodenal and
not uncommon. Case series of patients with colonic tumors invading pancreatic interface and demonstrate the potential role of aggressive
the pancreas and duodenum at initial presentation have suggested multimodality intervention.
improved survival with aggressive en bloc resections that include pan-
Case 1
In 1991, a 61-year-old man underwent low anterior resection
1Department of Gastrointestinal Medical Oncology for a T3 N0 M0 rectal adenocarcinoma. Surgery was followed
The University of Texas M. D. Anderson Cancer Center, Houston by adjuvant therapy with 5-fluorouracil (5-FU) and radiation. In
2MedicalOncology/Hematology Fellowship, Oklahoma University, Oklahoma City
3Department of Radiation Oncology 2000, the patient underwent surgical resection of a rectal cancer
4Department of Surgical Oncology
metastasis to the right lung and subsequently received 6 months of
The University of Texas M. D. Anderson Cancer Center, Houston
postoperative 5-FU therapy.
Submitted: Mar 26, 2008; Revised: May 20, 2008; Accepted: Jun 23, 2008 In January 2001, the patient developed gastrointestinal bleeding,
Address for correspondence: Michael J. Overman, MD, M. D. Anderson Cancer and esophagogastroduodenoscopy (EGD) revealed a duodenal ulcer.
Center, Unit 426, 1515 Holcombe Blvd, Houston, TX 77005 Biopsy of this ulcer demonstrated adenocarcinoma. The patient was
Fax: 713-745-1163; e-mail: moverman@mdanderson.org
referred to MDACC, where computed tomography (CT) of the abdo-
Electronic forwarding or copying is a violation of US and International Copyright Laws.
Authorization to photocopy items for internal or personal use, or the internal or personal use of specific clients, is granted by CIG Media Group, LP,
ISSN #1533-0028, provided the appropriate fee is paid directly to Copyright Clearance Center, 222 Rosewood Drive, Danvers, MA 01923 USA 978-750-8400.
338 Clinical Colorectal Cancer September 2008
men and pelvis revealed the presence of nonspecific duodenal wall In November 2000, the patient developed epigastric discom-
thickening without other evidence of metastatic disease. Subsequent fort and persistent nausea. Endoscopic duodenal biopsies revealed
positron emission tomography demonstrated a hypermetabolic focus adenocarcinoma, but no definitive mass was observed on CT scans.
at the duodenum with no other sites of abnormal uptake detected. Systemic chemotherapy with 5-FU was initiated, and repeat imaging
After multidisciplinary treatment planning, he received concurrent in June 2001 revealed a 4-cm mass lateral to the second portion of
5-FU and external-beam radiation therapy (EBRT) followed by a the duodenum and anterior to the midportion of the right kidney.
pancreaticoduodenectomy. Pathology showed that the adenocarci- Combination therapy with capecitabine and radiation was given,
noma was moderately differentiated and had invaded through the followed by therapy with capecitabine alone. In April 2002, the
muscularis propria into the underlying pancreas. No cancer was patient developed locally progressive disease with partial gastric outlet
found in 5 resected lymph nodes. Immunohistochemical (IHC) obstruction from duodenal narrowing. Despite the presence of low-
analysis revealed a cytokeratin (CK) 20positive and CK7-negative volume lung metastases, he underwent a pancreaticoduodenectomy
immunophenotype and had similar morphology in comparison with with en bloc resection of the distal ileum, proximal transverse colon,
the patients previous rectal cancer. and right kidney. Pathologic evaluation revealed a 4-cm moderately
In August 2002, an isolated lung metastasis was discovered and differentiated adenocarcinoma involving the duodenum, head of
resected. A second lung metastasis was resected in March 2003, but the pancreas, and serosa of the ileocolic anastomosis. Additionally, 2
by July 2003, two and a half years after the diagnosis of his duode- of 16 lymph nodes examined were involved. Comparison with the
nal recurrence, the patient was noted to have multifocal metastatic patients previous tumor revealed a similar morphology and an identi-
disease. He subsequently received irinotecan- and oxaliplatin-based cal CK20-positive, CK7-negative IHC phenotype.
systemic chemotherapy regimens. The patient died of metastatic dis- Pulmonary metastases slowly progressed, and he received sev-
ease in November 2006, approximately 70 months after the initial eral investigational treatments, none of which led to an objective
diagnosis of metastatic disease to the duodenum. response. In January 2004, he started treatment with irinotecan and
oxaliplatin for progressive lung and retroperitoneal disease. He died
Case 2 in January 2005, approximately 50 months after treatment for the
In 1995, a 67-year-old man underwent a right hemicolectomy recurrence involving the pancreas and duodenum.
and 1 year of adjuvant 5-FU therapy for a T3 N2 M0 well-dif-
ferentiated adenocarcinoma of the cecum. In February 2004, he Case 4
presented with partial gastric outlet obstruction. Computed tomog- In October 2003, a 59-year-old man underwent a right hemicolec-
raphy imaging revealed an 8-cm mesenteric mass involving the site tomy and anterior duodenal wall resection for a T4 N1 M0 adenocar-
of his previous right hemicolectomy with adjacent invasion of the cinoma of the hepatic flexure. Pathology revealed a moderately differ-
head of the pancreas and proximal duodenum. Endoscopic biopsy entiated colonic adenocarcinoma with invasion through the colonic
confirmed adenocarcinoma. He underwent a gastrojejunostomy for wall and into the periduodenal fibroadipose tissue. Additionally, 1 of
relief of his duodenal obstruction and shortly thereafter underwent 16 lymph nodes examined was positive. The surgical margin status
combined-modality therapy with capecitabine and EBRT. In June could not be definitively determined because of specimen fragmenta-
2004, the patient underwent a pancreaticoduodenectomy with en tion. The patient received 9 months of adjuvant therapy with 5-FU.
bloc resection of the transverse colon and distal small bowel, as In August 2004, the patient developed right-side abdominal pain,
well as extended retroperitoneal and mesenteric lymphadenectomy. nausea, and vomiting. Computed tomography showed a mass in the
Pathologic evaluation revealed foci of well-differentiated adenocar- second portion of the duodenum that had invaded the pancreas and
cinoma involving the ileocolic anastomosis, duodenum, pancreas, was obstructing the biliary and pancreatic ducts. Esophagogastrodu
and surrounding fibroadipose tissue that was morphologically con- odenoscopy revealed a large, partially obstructing ulcerative mass in
sistent with a colonic adenocarcinoma. Additionally, 6 of 14 lymph the duodenum with an endoscopic biopsy, demonstrating moderately
nodes were positive. Because of the patients previous long disease- differentiated adenocarcinoma. Analysis of the original tumor speci-
free interval (DFI), he was followed expectantly. In May 2007, the men and recurrent tumor specimen revealed microsatellite instability
patient developed a solitary pulmonary metastasis with a biopsy with loss of human mutL homolog 1 expression and a focal CK7-
demonstrating caudal-related homeobox 2positive, CK20-posi- positive and CK20-negative staining pattern.
tive, and CK7-negative adenocarcinoma consistent with a colonic The patient underwent a biliary bypass and palliative gastroje-
primary. He received 3 cycles of oxaliplatin-based therapy followed junostomy, followed by combination therapy with capecitabine
by lung resection. At last follow-up (48 months after the initial and radiation. After a stable response to this therapy, the patient
recurrence), the patient is alive and without evidence of disease. was presented at a multidisciplinary conference, and because of
poor nutritional status, surgical resection was not recommended.
Case 3 He subsequently developed progressive metastatic disease and died
In May 1997, a 51-year-old man underwent a right hemicolec- 14 months after recurrence.
tomy for a poorly differentiated T3 N2 M0 adenocarcinoma of
the cecum, followed by 1 year of adjuvant therapy with 5-FU. In Case 5
February 2000, he underwent bilateral pulmonary wedge resections In 1999, a 66-year-old man was diagnosed with a T3 N1 M0
for metastases, followed by 4 months of adjuvant therapy with colonic adenocarcinoma of the hepatic flexure. Adjuvant therapy with
5-FU and irinotecan. 5-FU was given for 6 months.
Clinical Colorectal Cancer September 2008 339
Treatment for Recurrent Colorectal Cancer Involving the Duodenum and Pancreas
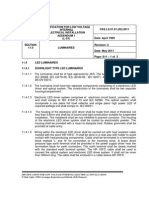
Table 1 Summary of Five Cases of Recurrent Colorectal Cancer Involving the Duodenum and Pancreas
Overall
Age Primary Initial Time to
Case Pathology Mode of Other Sites Survival
(Years) Location Stage Recurrence Symptoms Treatment
Recurrence of Disease* Status
(Months)
(Months)
Moderately None
Neoadjuvant 5-FU/Xrt and Hematogenous (previous lung
1 61 Rectal T3 N0 115 Bleeding differentiated 70 (Dead)
pancreaticoduodenectomy adenocarcinoma metastasis metastasis)
Nausea, Neoadjuvant capecitabine/Xrt Well-differentiated Local None
2 67 Cecum T3 N2 103 48 (Alive)
vomiting and pancreaticoduodenectomy adenocarcinoma recurrence
Poorly None
Pain, nausea, Neoadjuvant capecitabine/Xrt Local
3 51 Cecum T3 N2 42 differentiated (previous lung 50 (Dead)
vomiting and pancreaticoduodenectomy recurrence
adenocarcinoma metastases)
Moderately
Pain, nausea, Local
4 59 Right colon T4 N1 10 Capecitabine/Xrt differentiated None 14 (Dead)
vomiting adenocarcinoma recurrence
Poorly
Lymphatic Liver and
5 66 Right colon T3 N1 46 Pain Capecitabine/oxaliplatin differentiated 6 (Dead)
adenocarcinoma metastasis lung
*Attime of duodenal recurrence.
From duodenal recurrence.
Abbreviations: 5-FU = 5-fluorouracil; Xrt = radiation therapy
In May 2003, the patient reported weight loss and vague abdominal only 1 case. The surgical margins from the initial CRC resection were
pain. Computed tomography revealed a 6-cm peripancreatic mass negative in each case except case 4, in which the margin status could
with invasion into the pancreas and duodenum. The patient also had not be determined.
retroperitoneal and mesenteric lymphadenopathy, liver metastases, The mechanism of recurrence was thought to be by direct exten-
and lung metastases. Esophagogastroduodenoscopy revealed a duode- sion in 3 patients, hematogenous spread in 1 patient, and lymphatic
nal mass, which pathology confirmed was adenocarcinoma. Review of spread in 1 patient (Table 1). Three patients underwent aggressive
his duodenal pathology specimen at MDACC showed that the tumor trimodality treatment, with a resulting mean survival of 56 months.
was a poorly differentiated CK20-positive and CK7-negative adeno- Of these 3 cases, patient 2 remains alive without evidence of disease
carcinoma. The patient was presented to a multidisciplinary confer- recurrence at last follow-up (48 months after recurrence), while
ence, and considering his cytokeratin staining pattern and extensive patients 1 and 3 died of disease at 70 and 50 months, respectively,
ileocolic mesenteric adenopathy, the patient was determined to have after their duodenal recurrence. These impressive survival results
recurrent colon cancer, with the peripancreatic mass representing a were observed despite both patients having a history of previous
large nodal mass. pulmonary metastases. All 3 patients who underwent pancreati-
Despite treatment with capecitabine and oxaliplatin, the patient coduodenectomy experienced durable relief from their presenting
died in December 2003, 7 months after the recurrence. symptoms of bleeding, as in patient 1, or duodenal obstruction,
as in patients 2 and 3. The 2 patients who did not have surgical
Results resection of their duodenal recurrence survived for 6 months and
The time from initial diagnosis of colon or rectal cancer to recurrence 14 months, respectively, after the diagnosis of recurrence.
in our series ranged from 6 months to 10 years. All patients initially
had localized disease treated with surgery and adjuvant chemotherapy Discussion
with or without radiation therapy. The most common presenting Adenocarcinoma involving the duodenum and pancreas can result
symptoms of recurrence at the duodenal-pancreatic interface were pain, from primary duodenal adenocarcinoma, primary pancreatic adeno-
nausea, and vomiting. In all cases, pathologic evaluation conducted carcinoma, metastatic disease, or local invasion by adenocarcinoma
at MDACC determined that the recurrence was an adenocarcinoma originating in neighboring organs. Differentiating between these
consistent with a colorectal primary tumor. Comparison with the various situations requires thorough pathologic analysis and high-qual-
patients primary tumor was performed in 3 cases (cases 1, 3, and 4). ity radiologic imaging. In particular, making a distinction between
No coexisting adenoma or dysplasia was present to suggest a duodenal adenocarcinomas of the small bowel and colon is often difficult. A
primary tumor in any case. study examining the use of CK7 and CK20 to distinguish small
In these 5 cases, evaluation with EGD or CT (and usually both) bowel adenocarcinoma from colorectal adenocarcinoma found that, of
demonstrated the presence of recurrent disease. Pathologic diagnosis of 24 small-intestine adenocarcinomas, CK7 and CK20 were expressed
recurrence was made by endoscopic duodenal biopsy in all patients. All in 100% and 67%, respectively.10 Of the 23 CRC cases in the study,
cases presented with involvement of the pancreas and second portion of CK7 was expressed in 4%, and CK20 was expressed in 95%. However,
the duodenum. Lymph node involvement at the initial CRC diagnosis a recent study examining 486 carcinomas of the digestive system found
was present in 4 cases, whereas direct duodenal invasion was present in far fewer discernable differences in CK7 and CK20 expression levels.11
340 Clinical Colorectal Cancer September 2008
Michael J. Overman et al
Table 2 Reported Cases of Relapsed Colorectal Cancer Involving the Duodenum and Pancreas
Primary Time to Recurrence Other Sites Overall Survival
Study Year Treatment Survival Status
Location (Months) of Disease* (Months)
Kamal et al6 2003 Rectum 48 None Duodenal resection 10 Alive
Right colon 48 None Pancreaticoduodenectomy 31 Alive
Sperti et al28 2003 Colon Synchronous Colon Pancreaticoduodenectomy 28 Alive
Right colon 10 None Pancreaticoduodenectomy 17 Dead
Ascending colon 42 None Pancreaticoduodenectomy 20 Alive
Wagle et al29 2001
Hepatic flexure 18 None Pancreaticoduodenectomy 4 Alive
Le Borgne et al30 2000 Colon 6 None Pancreaticoduodenectomy 12 Dead
Yoshimi et al31 1999 Ascending colon 36 None Pancreaticoduodenectomy 24 Dead
Right colon 15 NR Pancreaticoduodenectomy 41 Dead
Harrison et al27 1997
Right colon 15 NR Pancreaticoduodenectomy 21 Dead
Colon 34 None Pancreaticoduodenectomy 43 Alive
Nakeeb et al32 1995
Colon 14 None Pancreaticoduodenectomy 24 Dead
Alfonso et al5 1979 Hepatic flexure 17 None Pancreaticoduodenectomy 12 Alive
*Attime of duodenal recurrence.
From duodenal recurrence.
Attime of publication.
Abbreviation: NR = not reported
Of the 23 small intestine adenocarcinomas and 68 colorectal adeno- carcinomatosis and direct extension were excluded, the rate of CRC
carcinomas, CK7 was expressed in 34% and 10%, respectively, while involvement of the small intestine was 2%-3%.21 Hematogenous
CK20 was expressed in 47% and 76%, respectively. Case 4, which spread was the modality of recurrence for the patient in case 1, who
demonstrated a CK20-negative and focal CK7-positive expression initially presented with a primary tumor in the rectum.
pattern, reflects the CK pattern frequently observed in patients with The use of pancreaticoduodenectomy for patients with colon
microsatellite-unstable colon adenocarcinomas.12 cancer who initially present with pancreatic and duodenal involve-
Involvement of the duodenum and pancreas by locally recurrent ment has been described in case series from MDACC and
CRC is most commonly associated with a right-sided colon cancer, Memorial Sloan-Kettering Cancer Center (MSKCC).22,23 In the
as seen in cases 2, 3, and 4. This is because the hepatic flexure of the MDACC series, 7 patients with duodenum or pancreatic head
colon is tightly affixed to the infra-ampullary portion of the descend- invasion by colon cancer underwent a pancreaticoduodenectomy.
ing duodenum by the transverse mesocolon.13 In addition, invasion The median overall survival (OS) was 32 months, with no opera-
from the periduodenal and peripancreatic lymph nodes can result in tive or postoperative deaths. In the series from MSKCC, 8 patients
involvement of the duodenum and pancreas, as seen in case 5. The with right-sided colon cancer involving the duodenum or pancreas
lymphatic drainage from the cecum and ascending colon follows the underwent pancreaticoduodenectomy or duodenectomy. No post-
ileocolic vessels toward the root of the superior mesenteric artery and operative deaths occurred, and 6 patients were alive without disease
vein, adjacent to the duodenum and pancreas. A previous study has recurrence at a median follow-up time of 26 months.
reported 8 cases in which pancreatic involvement from right-side colon Numerous small case series also describe the use of pancre-
cancer were localized to the pancreatic head.14 This involvement was aticoduodenectomy for the treatment of patients with metastatic
believed to result from local peripancreatic nodal invasion in 3 cases, disease involving the pancreas. However, the vast majority of these
from invasion by a paraduodenal mass in 1 case, and from metastatic studies report outcomes for patients with multiple primary tumor
disease in 4 cases. types, with the predominant tumor being renal cell carcinoma.24,25
Metastases to the duodenum and pancreas are rare, with autop- The Fox Chase Cancer Center has reported the outcomes for
sy series reporting small-intestinal metastases in approximately 18 patients, 8 with colon cancer, who had locally recurrent upper
2%-4% of all cancer cases and pancreatic metastases in approximately abdominal cancers that involved the pancreas.26 All patients under-
4%-15%.8,9,15-17 Involvement of the pancreas by primary CRCs has went a pancreatic resection, with all 8 patients with colon cancer
been reported in 2%-7% of cases described in autopsy series.16,17 In requiring a pancreaticoduodenectomy. The median OS for all
general, these metastases are components of widespread metastatic dis- 18 patients was 46 months. In addition, investigators from MSKCC
ease, and the frequency of solitary metastases to these sites is unknown. reported a series of 18 patients who underwent pancreaticoduode-
Tumors that most commonly metastasize to the pancreas are those nectomy for isolated metastatic or locally advanced nonperiampullary
of the lung, stomach, and kidney. For small-intestinal metastases, the cancers.27 The median OS was 40 months. There was no significant
most common primary tumors are melanoma, lung cancers, and breast difference in survival between the subgroup of patients with direct
cancers.8,18-20 In 2 autopsy series in which involvement by peritoneal invasion (8 cases) and the subgroup of patients with metastatic or
Clinical Colorectal Cancer September 2008 341
Treatment for Recurrent Colorectal Cancer Involving the Duodenum and Pancreas
locally recurrent disease (10 cases). The primary tumor types in these resection of colorectal liver metastases: FFCD ACHBTH AURC 9002
18 patients comprised 7 colon cancers, 4 gastric cancers, 3 renal cell trial. J Clin Oncol 2006; 24:4976-82.
5. Alfonso A, Morehouse H, Dallemand S, et al. Local duodenal metastasis
cancers, 2 lung cancers, 1 bladder cancer, and 1 melanoma. from colonic carcinoma. J Clin Gastroenterol 1979; 1:149-52.
From the literature, individual patient data are available for 6. Kamal HS, Farah RE, Hamzi HA, et al. Unusual presentation of rectal
13 patients who underwent surgical resection of recurrent or metastat- adenocarcinoma. Rom J Gastroenterol 2003; 12:47-50.
7. Sebastian JJ, Zaragozano R, Vicente J, et al. Duodenal obstruction
ic CRC involving the pancreas and duodenum (Table 2).5,6,27-32 The secondary to a metastasis from an adenocarcinoma of the cecum: a case
majority of these recurrences were from adenocarcinomas of the right report. Am J Gastroenterol 1997; 92:1051-2.
colon (12 of 13). The mean OS for these 12 cases was 24 months. 8. Willis RA. The Spread of Tumours in the Human Body. London:
Butterworth & Co; 1973.
In our series, the mean OS for all 5 patients was 38 months. For 9. Telerman A, Gerard B, Van den Heule B, et al. Gastrointestinal metas-
the 3 patients who underwent aggressive multimodality treatment tases from extra-abdominal tumors. Endoscopy 1985; 17:99-101.
with resection, chemotherapy, and radiation therapy, the OS was 10. Chen ZM, Wang HL. Alteration of cytokeratin 7 and cytokeratin 20
expression profile is uniquely associated with tumorigenesis of primary
48 months, 50 months, and 70 months, respectively. These 3 patients adenocarcinoma of the small intestine. Am J Surg Pathol 2004; 28:1352-9.
represent a highly selected group, with 2 patients demonstrating pro- 11. Lee MJ, Lee HS, Kim WH, et al. Expression of mucins and cytokera-
longed DFIs from initial diagnosis of > 8 years. tins in primary carcinomas of the digestive system. Mod Pathol 2003;
16:403-10.
At MDACC, we often favor the delivery of chemoradiation before 12. McGregor DK, Wu TT, Rashid A, et al. Reduced expression of cyto-
surgical resection in patients with localized recurrences. This approach keratin 20 in colorectal carcinomas with high levels of microsatellite
allows for a reduction in the tumor burden before a planned surgi- instability. Am J Surg Pathol 2004; 28:712-8.
13. Treitel H, Meyers MA, Maza V. Changes in the duodenal loop second-
cal intervention. In addition, preoperative radiation therapy, which ary to carcinoma of the hepatic flexure of the colon. Br J Radiol 1970;
is delivered when blood flow and oxygenation are unimpaired by 43:209-13.
postsurgical changes, might have an improved benefit-to-risk ratio 14. Charnsangavej C, Whitley NO. Metastases to the pancreas and peri-
pancreatic lymph nodes from carcinoma of the right side of the colon:
compared with postoperative radiation therapy. An important benefit CT findings in 12 patients. AJR Am J Roentgenol 1993; 160:49-52.
of this approach is improved patient selection for an aggressive surgical 15. Abrams HL, Spiro R, Goldstein N. Metastases in carcinoma; analysis of
intervention. If, during neoadjuvant therapy, local tumor progression 1000 autopsied cases. Cancer 1950; 3:74-85.
16. Adsay NV, Andea A, Basturk O, et al. Secondary tumors of the pan-
or new metastatic disease develops, inappropriate surgical intervention creas: an analysis of a surgical and autopsy database and review of the
might then be avoided, as in case 4. In the 3 patients who ultimately literature. Virchows Arch 2004; 444:527-35.
underwent pancreaticoduodenectomy, the intervals between initial 17. Nakamura E, Shimizu M, Itoh T, et al. Secondary tumors of the
pancreas: clinicopathologic study of 103 autopsy cases of Japanese
diagnosis of duodenal relapse and surgical resection were 4, 5, and 7 patients. Pathol Int 2001; 51:686-90.
months, respectively. 18. Richie RE, Reynolds VH, Sawyers JL. Tumor metastases to the small
There are limitations to the interpretation of our findings. As a ret- bowel from extra-abdominal sites. South Med J 1973; 66:1383-7.
19. Kadakia SC, Parker A, Canales L. Metastatic tumors to the upper
rospective case series, there is the potential for selection and interpreta- gastrointestinal tract: endoscopic experience. Am J Gastroenterol 1992;
tion bias. Because of the aggressive nature of the treatment discussed in 87:1418-23.
this report, patients who underwent multimodality therapy represent 20. Brady LW, ONeill EA, Farber SH. Unusual sites of metastases. Semin
Oncol 1977; 4:59-64.
a heavily selected group. The selection of such patients for aggressive 21. Farmer RG, Hawk WA. Metastatic tumors of the small bowel.
therapy, as represented in our report, should be made by an integrated Gastroenterology 1964; 47:496-504.
multidisciplinary team, and the applicability of our treatment approach 22. Curley SA, Evans DB, Ames FC. Resection for cure of carcinoma of
the colon directly invading the duodenum or pancreatic head. J Am
to other medical settings without multidisciplinary cancer care might Coll Surg 1994; 179:587-92.
not be appropriate. 23. Koea JB, Conlon K, Paty PB, et al. Pancreatic or duodenal resection
or both for advanced carcinoma of the right colon: is it justified? Dis
Colon Rectum 2000; 43:460-5.
Conclusion 24. Eidt S, Jergas M, Schmidt R, et al. Metastasis to the pancreas-an indica-
This case series and literature review suggests that selected patients tion for pancreatic resection? Langenbecks Arch Surg 2007; 392:539-42.
with CRC with relapsed disease involving the duodenum and pan- 25. Hiotis SP, Klimstra DS, Conlon KC, et al. Results after pancreatic
resection for metastatic lesions. Ann Surg Oncol 2002; 9:675-9.
creas can achieve long-term palliation of symptoms and prolonged 26. Pingpank JF Jr, Hoffman JP, Sigurdson ER, et al. Pancreatic resection
survival with a pancreaticoduodenectomy. Our experience suggests for locally advanced primary and metastatic nonpancreatic neoplasms.
that the best outcomes appear to be obtained through a multimodal- Am Surg 2002; 68:337-40; discussion 340-1.
27. Harrison LE, Merchant N, Cohen AM, et al. Pancreaticoduodenectomy
ity therapy approach. for nonperiampullary primary tumors. Am J Surg 1997; 174:393-5.
28. Sperti C, Pasquali C, Liessi G, et al. Pancreatic resection for metastatic
tumors to the pancreas. J Surg Oncol 2003; 83:161-6; discussion 166.
References 29. Wagle PK, Katrak MP, Navadgi SM, et al. Pancreaticoduodenectomy
1. Garcia-Aguilar J, Cromwell JW, Marra C, et al. Treatment of locally for metastatic colonic cancer--report of two cases. Indian J Gastroenterol
recurrent rectal cancer. Dis Colon Rectum 2001; 44:1743-8. 2001; 20:68-9.
2. Tepper JE, OConnell M, Hollis D, et al. Analysis of surgical salvage 30. Le Borgne J, Partensky C, Glemain P, et al. Pancreaticoduodenectomy
after failure of primary therapy in rectal cancer: results from Intergroup for metastatic ampullary and pancreatic tumors. Hepatogastroenterology
Study 0114. J Clin Oncol 2003; 21:3623-8. 2000; 47:540-4.
3. Nordlinger B, Guiguet M, Vaillant JC, et al. Surgical resection of 31. Yoshimi F, Asato Y, Kuroki Y, et al. Pancreatoduodenectomy for locally
colorectal carcinoma metastases to the liver. A prognostic scoring advanced or recurrent colon cancer: report of two cases. Surg Today
system to improve case selection, based on 1568 patients. Association 1999; 29:906-10.
Francaise de Chirurgie. Cancer 1996; 77:1254-62. 32. Nakeeb A, Lillemoe KD, Cameron JL. The role of pancreaticoduode-
4. Portier G, Elias D, Bouche O, et al. Multicenter randomized trial of nectomy for locally recurrent or metastatic carcinoma to the periam-
adjuvant fluorouracil and folinic acid compared with surgery alone after pullary region. J Am Coll Surg 1995; 180:188-92.
342 Clinical Colorectal Cancer September 2008
You might also like
- En Bloc Resection For Locally Advanced Colon Ca - Asai PDFDocument6 pagesEn Bloc Resection For Locally Advanced Colon Ca - Asai PDFJoy GhoseNo ratings yet
- En Bloc Resection For Locally Advanced Colon Ca - Asai PDFDocument6 pagesEn Bloc Resection For Locally Advanced Colon Ca - Asai PDFJoy GhoseNo ratings yet
- Should We Operate On The Locally Advanced Colon - SokolovDocument5 pagesShould We Operate On The Locally Advanced Colon - SokolovJoy GhoseNo ratings yet
- Surgical Management of Locally Advanced Colon CA - LandmannDocument8 pagesSurgical Management of Locally Advanced Colon CA - LandmannJoy GhoseNo ratings yet
- Pancreaticoduodenectomy For Locally Advanced Colon CA in HNPCC - ZhuDocument5 pagesPancreaticoduodenectomy For Locally Advanced Colon CA in HNPCC - ZhuJoy GhoseNo ratings yet
- Transverse Colon Cancer Secondarily Involving The Liver Duodenum Pancreas - Suzaki1996Document4 pagesTransverse Colon Cancer Secondarily Involving The Liver Duodenum Pancreas - Suzaki1996Joy GhoseNo ratings yet
- Pancreatoduodenectomy With Colon Cancer - Marsman2016Document8 pagesPancreatoduodenectomy With Colon Cancer - Marsman2016Joy GhoseNo ratings yet
- Right Hemicolectomy Plus Pancreaticoduodenectomy Vs Partial Duodenectomy - Cirocchi2014Document7 pagesRight Hemicolectomy Plus Pancreaticoduodenectomy Vs Partial Duodenectomy - Cirocchi2014Joy GhoseNo ratings yet
- Thirty-Day Outcomes in Patients Treated With en Bloc Colectomy and Pancreatectomy - Paquette2011Document6 pagesThirty-Day Outcomes in Patients Treated With en Bloc Colectomy and Pancreatectomy - Paquette2011Joy GhoseNo ratings yet
- Right Hemicolectomy and Multivisceral Resection 21 Cases - ZhaoDocument4 pagesRight Hemicolectomy and Multivisceral Resection 21 Cases - ZhaoJoy GhoseNo ratings yet
- Sigmoidoduodenal Fistula - Melissas2003Document3 pagesSigmoidoduodenal Fistula - Melissas2003Joy GhoseNo ratings yet
- Surgical Treatment and Prognosis of Cancers of Colon Invading Duodenum - Yang2011Document4 pagesSurgical Treatment and Prognosis of Cancers of Colon Invading Duodenum - Yang2011Joy GhoseNo ratings yet
- Pancreatic Head Resection For Invasive Colon CA - MeyerDocument4 pagesPancreatic Head Resection For Invasive Colon CA - MeyerJoy GhoseNo ratings yet
- Long-Term Survival Case of A Recurrent Colon CA at Hepaticojejunostomy - ZhuDocument6 pagesLong-Term Survival Case of A Recurrent Colon CA at Hepaticojejunostomy - ZhuJoy GhoseNo ratings yet
- T4N0 Colon Cancer Has Oncologic Outcomes Comparable To Stage III - Rottoli2012Document6 pagesT4N0 Colon Cancer Has Oncologic Outcomes Comparable To Stage III - Rottoli2012Joy GhoseNo ratings yet
- En Bloc Pancreaticodudenectomy With Colectomy - BhandariDocument3 pagesEn Bloc Pancreaticodudenectomy With Colectomy - BhandariJoy GhoseNo ratings yet
- Pancreatic or Duodenal Resection - Koea2000Document6 pagesPancreatic or Duodenal Resection - Koea2000Joy GhoseNo ratings yet
- Laparoscopic Partial Sleeve Duodenectomy (PSD) - Stauffer2013Document6 pagesLaparoscopic Partial Sleeve Duodenectomy (PSD) - Stauffer2013Joy GhoseNo ratings yet
- Combined Right Hemicolectomy and Pancreaticoduodenectomy - Sheng2015Document5 pagesCombined Right Hemicolectomy and Pancreaticoduodenectomy - Sheng2015Joy GhoseNo ratings yet
- Pancreatectomy For Non-Pancreatic Malignancies Results in Improved Survival - VarkerDocument6 pagesPancreatectomy For Non-Pancreatic Malignancies Results in Improved Survival - VarkerJoy GhoseNo ratings yet
- Pancreatectomy For Non-Pancreatic Malignancies Results in Improved Survival - VarkerDocument6 pagesPancreatectomy For Non-Pancreatic Malignancies Results in Improved Survival - VarkerJoy GhoseNo ratings yet
- Malignant Duodenocolic Fistulas Case Report ReviewDocument4 pagesMalignant Duodenocolic Fistulas Case Report ReviewJoy GhoseNo ratings yet
- Management of Patients of Right CA Colon Invading Duodenum or Pancreas - Fuks 2008Document5 pagesManagement of Patients of Right CA Colon Invading Duodenum or Pancreas - Fuks 2008Joy GhoseNo ratings yet
- Long Term Survival After Right Hemicolectomy and Pancreatoduodenectomy - Perysinakis2011Document2 pagesLong Term Survival After Right Hemicolectomy and Pancreatoduodenectomy - Perysinakis2011Joy GhoseNo ratings yet
- Limiting The Resectability in Locally Advanced Colon CA - SokolovDocument10 pagesLimiting The Resectability in Locally Advanced Colon CA - SokolovJoy GhoseNo ratings yet
- Ileal Conduit For Reconstruction of The Duodenum After PPPD - OhriDocument3 pagesIleal Conduit For Reconstruction of The Duodenum After PPPD - OhriJoy GhoseNo ratings yet
- Long-Term Survival in Patients With en Bloc Pancreaticoduodenectomy - Saiura2008Document4 pagesLong-Term Survival in Patients With en Bloc Pancreaticoduodenectomy - Saiura2008Joy GhoseNo ratings yet
- En Bloc Right Hemicolectomy and Pancreaticoduodenectomy With SMV Resection - Noda2010Document3 pagesEn Bloc Right Hemicolectomy and Pancreaticoduodenectomy With SMV Resection - Noda2010Joy GhoseNo ratings yet
- Laparoscopic en Bloc Resection of T4 Colon Cancer - Chen2016Document2 pagesLaparoscopic en Bloc Resection of T4 Colon Cancer - Chen2016Joy GhoseNo ratings yet
- En Bloc Resection of Right-Sided Colonic Adenoca - Kapoor2005Document4 pagesEn Bloc Resection of Right-Sided Colonic Adenoca - Kapoor2005Joy GhoseNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Nelson Sanchez GE Module October 2020Document92 pagesNelson Sanchez GE Module October 2020Nneg Gray0% (1)
- Pump IntakeDocument6 pagesPump IntakeAnonymous CMS3dL1T100% (1)
- Book 2 - Test 1Document2 pagesBook 2 - Test 1Đức LongNo ratings yet
- Types of Ego?Document2 pagesTypes of Ego?S.UdhayakumarNo ratings yet
- (Nima Naghibi) Rethinking Global Sisterhood Weste PDFDocument220 pages(Nima Naghibi) Rethinking Global Sisterhood Weste PDFEdson Neves Jr.100% (1)
- JKR Specs L-S1 Addendum No 1 LED Luminaires - May 2011Document3 pagesJKR Specs L-S1 Addendum No 1 LED Luminaires - May 2011Leong KmNo ratings yet
- Automated Crime Reporting SystemDocument101 pagesAutomated Crime Reporting SystemDeepak Kumar60% (10)
- Inclusive E-Service or Risk of Digital Divide The Case of National ICT Policy 2018 of BangladeshDocument11 pagesInclusive E-Service or Risk of Digital Divide The Case of National ICT Policy 2018 of BangladeshInternational Journal of Innovative Science and Research Technology100% (1)
- Solution Manual For Illustrated Guide To The National Electrical Code 7th Edition Charles R MillerDocument24 pagesSolution Manual For Illustrated Guide To The National Electrical Code 7th Edition Charles R MillerHenryJohnsonaswek97% (39)
- Asian Games African Games: Beach VolleyballDocument5 pagesAsian Games African Games: Beach VolleyballJessan Ybañez JoreNo ratings yet
- We Generally View Objects As Either Moving or Not MovingDocument11 pagesWe Generally View Objects As Either Moving or Not MovingMarietoni D. QueseaNo ratings yet
- All Types of Switch CommandsDocument11 pagesAll Types of Switch CommandsKunal SahooNo ratings yet
- MAN 2 Model Medan Introduction to School Environment ReportDocument45 pagesMAN 2 Model Medan Introduction to School Environment ReportdindaNo ratings yet
- CPS Layoffs BreakdownDocument21 pagesCPS Layoffs BreakdownjroneillNo ratings yet
- STR File Varun 3Document61 pagesSTR File Varun 3Varun mendirattaNo ratings yet
- 42U System Cabinet GuideDocument68 pages42U System Cabinet GuideGerman AndersNo ratings yet
- TR-Pharmacy Services NC IIIDocument135 pagesTR-Pharmacy Services NC IIIAljon Fortaleza Balanag100% (2)
- Linear Programming Models: Graphical and Computer MethodsDocument91 pagesLinear Programming Models: Graphical and Computer MethodsFaith Reyna TanNo ratings yet
- Ra 11223 PDFDocument34 pagesRa 11223 PDFNica SalazarNo ratings yet
- LP IV Lab Zdvzmanual Sem II fbsccAY 2019-20z 20-ConvxvzzertedDocument96 pagesLP IV Lab Zdvzmanual Sem II fbsccAY 2019-20z 20-ConvxvzzertedVikas GuptaNo ratings yet
- SpringDocument4 pagesSpringarun123123No ratings yet
- Impact of Endurance Exercise Training in the Fasted State on Muscle Metabolism and Insulin SensitivityDocument14 pagesImpact of Endurance Exercise Training in the Fasted State on Muscle Metabolism and Insulin SensitivityYo Vivo Fit Pablo y KarlaNo ratings yet
- ECE 4400 Performance Analysis Local Computer Networks HomeworkDocument2 pagesECE 4400 Performance Analysis Local Computer Networks HomeworkNguyen Phi HungNo ratings yet
- CELTA Pre-Interview Grammar, Vocabulary and Pronunciation ExercisesDocument4 pagesCELTA Pre-Interview Grammar, Vocabulary and Pronunciation ExercisesMichelJorge100% (2)
- Philippine Politics and Constitution SyllabusDocument7 pagesPhilippine Politics and Constitution SyllabusIvy Karen C. Prado100% (1)
- Linear Piston Actuators: by Sekhar Samy, CCI, and Dave Stemler, CCIDocument18 pagesLinear Piston Actuators: by Sekhar Samy, CCI, and Dave Stemler, CCIapi-3854910No ratings yet
- Komposit UHMWPE Sebagai Alternatif Bantalan Rel Kereta Api: Abel Evan, Alia Kristika, Farid Mulia LatiefDocument11 pagesKomposit UHMWPE Sebagai Alternatif Bantalan Rel Kereta Api: Abel Evan, Alia Kristika, Farid Mulia LatiefAlia KristikaNo ratings yet
- Homer BiographyDocument3 pagesHomer BiographyKennethPosadasNo ratings yet
- 2018 Diesel TOYOTA Jun11Document90 pages2018 Diesel TOYOTA Jun11eko sulistyo75% (4)
- GEd 105 Midterm ReviewerDocument17 pagesGEd 105 Midterm ReviewerAndryl MedallionNo ratings yet