Professional Documents
Culture Documents
03 - Nutritional Screening and Assessment PDF
Uploaded by
bocah_britpopOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
03 - Nutritional Screening and Assessment PDF
Uploaded by
bocah_britpopCopyright:
Available Formats
Nutritional Assessment and Techniques
Topic 3
Module 3.1
Nutritional Assessment Yitshal Berner
Rmy Meier
Lubos Sobotka
Nachum Vaisman
Learning Objectives
To understand nutritional screening and assessment;
To assess a patient for general nutritional status;
To realize the signs and the symptoms of nutritional problems;
To be familiar with nutritional screening;
To understand different methods used for the nutritional assessment;
To know limitations of different methods for nutritional assessment;
To know the benefits and limits of laboratory and balance-studies for nutritional assessments.
Contents
1. Nutritional screening and assessment
1.1 TScreening
1.2 Assessment
2. Techniques used in nutritional assessment
2.1 History
2.2 Physical examination
2.3 Functional tests
2.4 Laboratory parameters
Serum proteins, total lymphocyte counts, vitamins and minerals
Creatinine height index (CHI)
Nitrogen balance studies
2.5 Assessment of food intake
Key Messages
To understand how important to get the history taking and physical examination on the
definition of nutritional problems;
Nutritional screening and assessment are important part of patient care to identify patients
requiring nutritional support;
Nutrition screening is an important tool for rapid and simple evaluation of an individual
nutritional status;
Nutrition assessment is important for detailed diagnosis of acute and chronic malnutrition
(over- and undernutrition);
Nutrition screening and assessment are important in clinical medicine because acute and
chronic malnutrition (over- and undernutrition) are prevalent.
Copyright 2006 by ESPEN
1. Nutritional screening and assessment
Nutrition screening is an important Nutritional status
tool for rapid and simple evaluation
of an individual nutritional status.
Undernutrition screening and assessment
Nutrition assessment is Diagnosis of malnutrition (undernutrition)
important for detailed
diagnosis of acute and chronic
malnutrition (over- and Screening Assessment
undernutrition).
Nutrition screening and Screening is a simple and Assessment is a
assessment are important in rapid process, to select diagnostic process which
clinical medicine because subjects who are characterizes degree of
acute and chronic malnutrition malnourished or at risk of malnutrition and risk of
(over- and undernutrition) are malnutrition. It should be complications related to
prevalent (1, 2, 3). sensitive enough to detect malnutrition. The process of
all or nearly all the patients nutritional assessment is
at nutritional risk. much more complex than
1.1 Screening screening
Screening is a simple and rapid Fig. 1
process, to select subject who are
malnourished or at risk of
malnutrition. It can be carried out
by busy admitting nursing and BMI (kg/m2) Weight loss in 3-6 months Acute disease effect
medical staff. It should be sensitive 0 : >20.0 0 : <5 % Add a score of 2 if there
enough to detect all or nearly all 1 : = 18.5-20.0 1 : = 5-10 % is likely to be no
nutritional intake for > 5
the patients at nutritional risk. 2< 18.5 2 : > 10 % days
Most screening tools address four
basic questions (4):
recent weight loss OVERALL RISK OF UNDERNUTRITION
recent food intake 2 or more
0 (LOW) (HIGH)
current body mass index 1 (MEDIUM)
TREAT
ROUTINE OBSERVE
disease severity CLINICAL CARE
ESPEN published guidelines for
Hospital - refer to
nutrition screening in the Hospital - document dietitian or implement
community, in the hospital and Repeat screening dietary and fluid intake local policies. Generally
Hospital - every week for 3 days
among elderly in institutions. food first followed by
Care Homes - every Care Homes (as for
Screening tools recommended by month hospital) food fortification and
ESPEN for: Community - every Community - Repeat supplements Care
year for screening, e.g. from <1 Homes (as for hospital)
Community: Malnutrition
special groups, e.g. mo to >6 mo (with dietary Community (as for
Screening tool (MUST) (5); those >75 y advice if necessary) hospital)
Hospital: Nutritional Risk
Screening.
Fig. 2 Malnutrition Universal Screening Tool (MUST) for adults
Copyright 2006 by ESPEN
Table 1 Nutritional Risk Screening (NRS 2002)
Initial screening I
1 Is BMI < 20.5 Yes No
2 Has the patient lost weight within the last 3 months?
3 Has the patient had a reduced dietary intake in the last
week?
4 Is the patient severely ill ? (e.g. in intensive therapy)
Yes: If the answer is Yes to any question, the final screening is performed.
No: If the answer is No to all questions, the patient is re-screened at weekly intervals.
If the patient e.g. is scheduled for a major operation, a preventive nutritional care plan is
considered to avoid the associated risk status.
Table 2 Final screening II
Impaired nutritional status Severity of disease (increase in requirements)
Absent Normal nutritional Absent Normal nutritional
status requirements
Mild Score 1 Wt loss > 5% in 3 Mild Score 1 Hip fracture* Chronic
mos or Food intake patients, in particular
below 5075% of with acute complications:
normal requirement cirrhosis*, COPD*. Chronic
in preceding week hemodialysis, diabetes,
oncology
Moderate Score 2 Wt loss > 5% in 2 Moderate Score 2 Major abdominal surgery*
mos or BMI 18.5 Stroke* Severe
20.5 + impaired pneumonia, hematologic
general condition or malignancy
Food intake 2560%
of normal
requirement in
preceding week
Severe Score 3 Wt loss > 5% in 1 Severe Score 3 Head injury* Bone
month (> 15% in 3 marrow transplantation*
mos) or BMI o18.5 + Intensive care patients
impaired general (APACHE 10).
condition or Food
intake 0-25% of
normal requirement
in preceding week
in preceding week.
Score: + Score: =Total score:
Age if 70 years: add 1 to total score above = age-adjusted total score:
Score >3: the patient is nutritionally at-risk and a nutritional care plan is initiated
Score <3: weekly rescreening of the patient. If the patient e.g. is scheduled for a major
operation, a preventive nutritional care plan is considered to avoid the associated risk status.
Copyright 2006 by ESPEN
Table 3 Elderly: Mini Nutritional Assessment (MNA) (6)
Initial Screening in Mini Nutritional Assessment (MNAr) for the Elderly
A Has food intake declined over the past 3 months due to loss of appetite
digestive problems, chewing or swallowing difficulties?
0 = severe loss of appetite
1 = moderate loss of appetite
2 = no loss of appetite
B Weight loss during last months?
0 = weight loss greater than 3 kg
1 = does not know
2 = weight loss between 1 and 3 kg
3 = no weight loss
C Mobility?
0 = bed or chair bound
1 = able to get out of bed/chair but does not go out
2 = goes out
D Has suffered physical stress or acute disease in the past 3 months?
0 = yes
2 = no
E Neuropsychological problems?
0 = severe dementia or depression
1 = mild dementia
2 = no psychological problems
F Body Mass Index (BMI) |weight in kg|/|height in m|2
0 = BMI less than 19
1 = BMI 19 to less than 21
2 = BMI 21 to less than 23
3 = BMI 23 or greater
Screening score (total max. 14 points)
12 points or grater Normal not at risk no need to complement assessment
11 points or below Possible malnutrition continue assessment
1.2 Assessment
Assessment is a diagnostic process which characterizes degree of malnutrition and risk of
complications related to malnutrition. The process of nutritional assessment is much more complex
than screening and it should include the following principles:
history and examination;
factors leading to malnutrition;
natural history of the patients condition;
weight loss;
appetite;
gastrointestinal symptoms;
fever;
medical and drug history;
diet history:
disease status,
temperature,
pulse rate,
blood pressure,
laboratory tests of inflammation,
Copyright 2006 by ESPEN
nutrient losses from wounds, fistulae etc.;
functional assessment;
energy expenditure;
mental and physical dysfunction;
muscle strength;
mental scoring system;
mood status;
laboratory tests;
quantifying inflammation and disease severity;
plasma protein levels (transthyretin, transferrin etc.);
plasma changes in minerals (e.g. K, Ca, Mg, P, Zn, Fe);
plasma levels of vitamins;
fluid balance.
There are many methods and indexes which are based on above mentioned assessment methods,
however their interpretation and correlation is still difficult see Nutr. Rev. 2000.
2. Techniques used in nutritional assessment
2.1 History
The history is the starting point for any nutritional assessment. Specific features of note include a
recent weight changes; dietary habits and alteration in dietary intake; allergies and food
intolerance; medications that may effect appetite, gastrointestinal functions and symptoms;
current functional capacity, including recent limitations; and previous medical conditions (any
chronic or acute disease state).
2.2 Physical examination
Physical examination is the next step in nutritional assessment. This assessment predominantly
relies on subjective and descriptive information. Although not quantitative, a physical examination
is may still influence the nutritional management of a patient.
The main objective of a physical examination is to establish signs and symptoms of nutrient
deficiencies or toxicities, and tolerance of current nutritional support. A systems approach should
be applied using the examination techniques of inspection, palpation, percussion, and auscultation.
The physical examination should include (7):
Assessment of muscle mass and subcutaneous fat stores;
Inspection and palpation for edema and ascites. These two conditions are important physical
indicators of diminished visceral protein levels and hepatic dysfunction;
Inspection and evaluation for sings and symptoms of vitamin and mineral deficits, such as
dermatitis, glossitis, cheilosis, neuromuscular irritability, and coarse, easily pluckable hair;
The patients prescribed medication should be examined for potential drug-nutrient interactions,
increased macro-or micronutrient requirements, and nutritionally related side effects such as
constipation, diarrhea, nausea, vomiting.
The simplest validated nutritional assessment is the SGA, whish is based on patients history and
physical examination. Clinicians prefer SGA because of its simplicity, feasibility and sensitivity
that is almost equivalent to objective tests.
Nutritional assessment of patients is not an easy procedure. Although, lots of the clinical and
laboratory measurements are available for nutritional assessment, all of them have lots of
deficiencies. Nutritional assessment is an art more than science. At the current state of the art, in
addition to the physical examination and clinical history, many experienced clinicians solve this
problem by using a few laboratory tests.
2.3 Functional tests
Hand dynamometry;
Direct muscle stimulation;
Peak flow and FEV;
Immune function;
Copyright 2006 by ESPEN
Skin responses to intradermal antigens;
Lymphocyte count;
Proportion and number of T-lymphocytes.
Immune function can be tested by lymphocyte counts and by cutaneous applied skin tests. In most
hospitalized patients, delayed hypersensitivity reactivity and total lymphocyte counts are not very
useful components of a nutrition assessment profile
2.4 Laboratory parameters
The serum albumin;
The shorter half time proteins;
Transthyretin (formerly prealbumin) - 2 days;
Transferrin - 7 days;
Creatinine height index (CHI);
Nitrogen balance.
A complete nutritional assessment consists of a combination of subjective and objective
parameters, but up to now, no single parameter has been shown to be useful in all patients. Most
nutritional parameters lack sensitivity and specificity; therefore, methods of identifying
malnourished patients are not entirely satisfactory.
Laboratory testing is useful for assessment of the nutritional status and monitoring of nutritional
interventions.
Serum proteins, total lymphocyte counts, vitamins and minerals
Several laboratory parameters (serum proteins, total lymphocyte counts, vitamins and minerals) are
used. Serum proteins have different half-life times. Serum albumin is a good predictor for outcome
and reflects disease severity. On the other hand, it is a bad marker to assess nutritional status.
Serum albumin can be used for long term control.
To assess short term changes, prealbumin or transferrin is more useful. Serum proteins have many
limitations. The serum concentrations of visceral proteins decline with overhydration and increase
with dehydration independent of nutritional status. Low serum albumin levels exacerbate ascites,
lower extremity edema, and gut edema because of depressed colloid oncotic pressure. Serum
transferrin is the less affected protein by other factors.
Creatinine height index (CHI)
The somatic protein compartment Norm-
Norm-values for urinary-
urinary-creatinine
can be evaluated by the creatinine
Urinary creatinine (mg/24h)
height index (CHI).
Creatinine excretion correlates
with lean body mass and body
weight. The CHI is depended on
urine creatinine excretion.
Renal insufficiency, meat Norm/men Norm/women
consumption, physical activity,
fever, infections and trauma
influence urine creatinine
excretion
Height (cm)
Fig. 3
Copyright 2006 by ESPEN
Role and Limitations of Nitrogen Balance Nitrogen balance studies
Nitrogen balance = N input N output Nitrogen balance studies are often
Neg. N-balance used to assess protein catabolism.
In non-stressed conditions, urea
The rate of protein catabolism exceeds
composes 30-90% of total urea
the role of protein anabolism
nitrogen. For usual clinical
Pos. N-balance purposes, nitrogen balance
calculation done with urinary urea
Indicative of nitrogen retention nitrogen instead of total urinary
nitrogen is adequate.
Research tool It has to be considered that
nitrogen excretion calculated from
In clinical conditions urinary urea nitrogen is affected by
intake is often overestimated increased stress, which can alter
losses in urine, faeces, skin, wounds is urea production and/or increase of
Fig. 4 often underestimated non-urea nitrogen by-products.
The validity of nitrogen balance is
affected by severe nitrogen
retention disorders, accuracy of
the 24-hour-urine collection and
Nitrogen-balance completeness of protein or amino-
acid intake data.
The calculation of nitrogen balance
is shown on Fig. 5.
N-balance=
balance= Protein-
Protein-intake - UUN** + fecal losses + obligatory losses
g/d 6.25* A simple assessment to assess
2-4 g/d catabolic states is also the urea
production rate and the
urea/creatinine quotient.
*specialized enteral or parenteral formulations have often a different Nutritional monitoring and reasons
conversion coefficient of response can be measured in
vivo (by weight gain, N-balance,
(** urinary urea nitrogen)
nitrogen) complication rates) and in vitro
UUN x (1.25) = TUN
measurements by plasma-serum
concentration of proteins. The
Fig. 5 calculation of urea-production rate
is shown on Fig. 6.
For identifying patients with pre-
existing malnutrition or those at
most risk, a combination with a
Urea-production rate comprehensive nutritionally focus
physical exam together with
carefully selected objective
parameters provide the best
UPR (g/24 h) = information.
UUN (g/24 h)+(d
h)+(d-serum-
serum-crea (mg/dl)x0.0099xBWxfactor*)
*? 0.55
*? 0.6
Interpretation: UPR > 30 g/24 = catabolie
Fig. 6
Copyright 2006 by ESPEN
2.5 Assessment of food intake
Quantifications of food intakes and their comparison with energy expenditures can not only describe
current status but also predict whether the patients nutritional status is likely to improve or
deteriorate.
Nutrient balance = intake (e.g. food intake charts) expenditure
Food intake assessment estimates food intakes and is among the main tools for assessing nutritional
status. Food intake measurements are used not only for the determination of patients nutritional
status, but also characterization of the nutritional status of a population for monitoring and
surveillance.
Assessment of dietary intake has considerable challenge and prone to significant error and bias.
Food balance sheets and household budget surveys are indirect methods of food consumption
studies. Food records and dietary recalls measure food intake on specified periods, usually 1-7 days.
Because of day to day variability, several days of records may be required to estimate usual food
intake. Food frequency questionnaires are developed to describe standardized data on usual long-
term diet.
The determination of the consumption of nutrients can be achieved either by analyzing the foods
consumed directly or by using food composition tables. Most food composition tables are organized
according to the classification of foods into food groups. Dietary reference intakes (DRI) provide
standards to serve as a goal for good nutrition.
Questionnaires are in common use in the medical practice and in nutrition assessment as well as in
decisions making process. Every questionnaire has to pass validation to certain Gold Standard,
and reliability tests.
The data in questionnaire may be of different types:
Dietary data, either before analysis or specific components after dietary analysis;
Anthropometrics data like height, weight, BMI, or body composition;
Laboratory results and special tests done;
Eating habits like timing of meals and where they are taken;
General health questions;
Medical data like diagnoses, surgical treatments and drugs;
Demographic and socio-economic data.
It is very important to evaluate the objective of the questionnaires. Many questionnaires are
designed as epidemiological surveys, and others as clinical tools for specific purposes, some are
designed for every person and some for specific populations, some are for the detection of
malnutrition while other concentrate on risk evaluation due to metabolic diseases as diabetes,
hyperlipidemia and obesity.
Energy expenditure can be measured (indirect calorimetry) or estimated from different formulas
see module energy metabolism.
Energy intake is measured using either 37 day food diaries kept by the patient or food intake charts
kept by nursing staff and used by the dietician to calculate energy and protein intake.
References
1. David E. et al. Current concepts in nutritional assessment Archives of Surgery 2002; 137: 42
2. Basics in Clinical Nutrition Sobotka L.(edit), 3rd edition 2004, Galen
3. Weekes et al. The development, validation and reliability of a nutrition screening tool based on
the recommendations of BAPEN. Clin Nutr 2004; 23: 1104
4. Kondrup J, et al . ESPEN guidelines for nutrtion screening 2002. Clin Nutr 2003; 22: 415
5. Guigoz Y, et al, Assessing the nutritional status of the elderly: the mini nutritional assessment
as part of the geriatric assessment. Nutr Rev 1996;54:S59
6. Ignatavicius et al. Medical-Surgical-Nursing, 2nd ed. WB Saunders, Philadelphia, 1995
7. Detsky et. al. What is subjective global assessment of nutritional status. JPEN 1987; 11:8
Copyright 2006 by ESPEN
You might also like
- Assessment of Digestive and Gastrointestinal FunctionDocument19 pagesAssessment of Digestive and Gastrointestinal FunctionMarichelle Vicente- Delos SantosNo ratings yet
- Nutrition Essentials for Growing PreschoolersDocument6 pagesNutrition Essentials for Growing PreschoolersKeerthana VNo ratings yet
- MCH 161118045354Document38 pagesMCH 161118045354SrideviRaviNo ratings yet
- APGAR Score: Shakuntala Chauhan Payal Maurya Mahesh Chand Meena Pushpam Saroj Shweta KumariDocument15 pagesAPGAR Score: Shakuntala Chauhan Payal Maurya Mahesh Chand Meena Pushpam Saroj Shweta KumariNarendra Singh MeenaNo ratings yet
- Postpartum Nursing PowerpointDocument3 pagesPostpartum Nursing PowerpointAntonella VitaleNo ratings yet
- Dietary Guidelines For A Healthy Postnatal DietDocument4 pagesDietary Guidelines For A Healthy Postnatal DietAkhila Basu100% (1)
- National Immunization ScheduleDocument4 pagesNational Immunization ScheduleKenneth Ralph UrbanNo ratings yet
- Fundal Height ScreeningDocument10 pagesFundal Height ScreeningDr_Soranus100% (1)
- Icds & MMRDocument42 pagesIcds & MMRsanjeev guptaNo ratings yet
- Folic Acid Presentation PDFDocument13 pagesFolic Acid Presentation PDFAngela IlustrisimoNo ratings yet
- Step To Follow Intrapartal CareDocument3 pagesStep To Follow Intrapartal CareyabaeveNo ratings yet
- Preterm Babies: Causes, Clinical Features and ManagementDocument103 pagesPreterm Babies: Causes, Clinical Features and ManagementLyka BernalNo ratings yet
- AdolescentDocument35 pagesAdolescentmalyn1218100% (1)
- The Important Measurements of A NewbornDocument3 pagesThe Important Measurements of A NewbornGraciaNo ratings yet
- Hirschsprung's Disease - AthigamanDocument128 pagesHirschsprung's Disease - Athigamanprived100% (4)
- Session Plan Nutrition AssessmentDocument10 pagesSession Plan Nutrition AssessmentPrabir Kumar ChatterjeeNo ratings yet
- K44 - Nutrition During LactationDocument26 pagesK44 - Nutrition During Lactationbilli lisanuddinNo ratings yet
- Perineal CareDocument4 pagesPerineal CareJny SherpaNo ratings yet
- Icds-Integrated Child Development ServiceDocument12 pagesIcds-Integrated Child Development ServiceAngel AngelNo ratings yet
- Forceps Delivery Treatment & Management - Preoperative Details, Intraoperative Details, Postoperative DetailsDocument10 pagesForceps Delivery Treatment & Management - Preoperative Details, Intraoperative Details, Postoperative DetailsAnonymous wYz8FtLLONo ratings yet
- The Changing Nutritional Needs Across The Life CycleDocument24 pagesThe Changing Nutritional Needs Across The Life CycleFrance Dave CantorNo ratings yet
- Personal Hygiene: Mary Grace L. Araullo RN MSCPDDocument23 pagesPersonal Hygiene: Mary Grace L. Araullo RN MSCPDgraceNo ratings yet
- FAMILY PLANNING PROGRAM HandoutsDocument2 pagesFAMILY PLANNING PROGRAM HandoutsWilma Nierva BeraldeNo ratings yet
- Pregnancy Induced Hypertension PihDocument17 pagesPregnancy Induced Hypertension PihRose DeymNo ratings yet
- ContractedDocument15 pagesContractedswapnil3250No ratings yet
- Input 3 Assessment of Nutritional StatusDocument81 pagesInput 3 Assessment of Nutritional StatusRauell Rhaj SantosNo ratings yet
- Urine Collection: - Clinical Instructor (Sign Over Printed Name)Document2 pagesUrine Collection: - Clinical Instructor (Sign Over Printed Name)hey aadarshaNo ratings yet
- Congenital AbnormalitiesDocument45 pagesCongenital AbnormalitiesSaad AbdullahNo ratings yet
- Anorectal Malformations: Presented by Khushveer KaurDocument91 pagesAnorectal Malformations: Presented by Khushveer KaurKataria DavinNo ratings yet
- Psychological Changes of PregnancyDocument8 pagesPsychological Changes of PregnancyMaria Ivy Rochelle TanNo ratings yet
- Growth comparison of breast vs formula fed neonatesDocument7 pagesGrowth comparison of breast vs formula fed neonatesOman SantosoNo ratings yet
- Unit 5 Normal Puerperium and Nursing Management: 5.0 ObjectivesDocument14 pagesUnit 5 Normal Puerperium and Nursing Management: 5.0 ObjectivesJissa Daison100% (1)
- Growth and Development of Newborn To InfancyDocument54 pagesGrowth and Development of Newborn To Infancymerin sunilNo ratings yet
- Protein-Energy Malnutrition Diagnosis and TreatmentDocument30 pagesProtein-Energy Malnutrition Diagnosis and TreatmentChinchu MohanNo ratings yet
- Development and Maintenance of Standards Andaccreditation in Nursing EducationprogramsDocument6 pagesDevelopment and Maintenance of Standards Andaccreditation in Nursing EducationprogramsshintofilcyNo ratings yet
- 22nd - ROLES AND FUNCTIONS OF NURSESDocument4 pages22nd - ROLES AND FUNCTIONS OF NURSESMercy Anne Ecat100% (1)
- Breastfeeding Assessment Tool: Neonatal: © Unicef UK Baby Friendly Initiative, Adapted From NHS Greater Glasgow & ClydeDocument2 pagesBreastfeeding Assessment Tool: Neonatal: © Unicef UK Baby Friendly Initiative, Adapted From NHS Greater Glasgow & ClydedeboraNo ratings yet
- NCM 105 Lecture Covers Nutrition Through Life StagesDocument17 pagesNCM 105 Lecture Covers Nutrition Through Life StagesSyed FlyntNo ratings yet
- Faye Abdellah Theory MSC I Year 2 NewDocument88 pagesFaye Abdellah Theory MSC I Year 2 NewASIR DHAYANI100% (1)
- Assessment of The Fetal Well-BeingDocument85 pagesAssessment of The Fetal Well-BeingAlphine DalgoNo ratings yet
- Fetal Growth and DevelopmentDocument35 pagesFetal Growth and DevelopmentDjamnur AgnessiaNo ratings yet
- Basal Metabolic Rate and Factors that Affect Energy ExpenditureDocument14 pagesBasal Metabolic Rate and Factors that Affect Energy ExpenditureAnahgen RomeoNo ratings yet
- Henderson's 14 Basic Human Needs TheoryDocument25 pagesHenderson's 14 Basic Human Needs TheoryChandrashekar Gajula100% (2)
- Assessing High Risk NewbornsDocument42 pagesAssessing High Risk NewbornsKiran KumarNo ratings yet
- ICDS Scheme ExplainedDocument59 pagesICDS Scheme ExplainedRamniwasMahoreNo ratings yet
- Maternal and Child Health CareDocument12 pagesMaternal and Child Health CarePraachii SharmaNo ratings yet
- Fertilization, Implantation & Embryo Development ExplainedDocument54 pagesFertilization, Implantation & Embryo Development ExplainedMarvelousNo ratings yet
- Dietary Standard RDADocument24 pagesDietary Standard RDANurul Afifah50% (2)
- CPMS College Nursing Assignment on Colonic IrrigationDocument3 pagesCPMS College Nursing Assignment on Colonic IrrigationAmy Lalringhluani ChhakchhuakNo ratings yet
- AnthopometryDocument44 pagesAnthopometryghifari2007No ratings yet
- Policy For Patients Under Restraints: Nursing Excellence UnitDocument22 pagesPolicy For Patients Under Restraints: Nursing Excellence UnitjinoNo ratings yet
- Nutritional Problems: Presenter Priyanka Gehlot M. Sc. (Prev.)Document38 pagesNutritional Problems: Presenter Priyanka Gehlot M. Sc. (Prev.)vikas takNo ratings yet
- Nursing Care for Clients with InfertilityDocument23 pagesNursing Care for Clients with Infertilityastraeax pandaNo ratings yet
- Understanding the Partogram: Monitoring Labor Progress and OutcomesDocument20 pagesUnderstanding the Partogram: Monitoring Labor Progress and OutcomesKasumba ChandaNo ratings yet
- Food Production & AdulterationDocument23 pagesFood Production & Adulterationvinoth100% (1)
- G & D Assessment, Growth ChartDocument12 pagesG & D Assessment, Growth ChartThilaga RamNo ratings yet
- Perineal Care ProcedureDocument12 pagesPerineal Care ProcedureShikarin KitaNo ratings yet
- 17 Enteral and Parenteral NutritionDocument47 pages17 Enteral and Parenteral NutritionKathleen AngNo ratings yet
- Hirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- 09 - Monitoring and Complications of Parenteral NutritionDocument14 pages09 - Monitoring and Complications of Parenteral Nutritionbocah_britpopNo ratings yet
- 17 - Enhanced Recovery PrinciplesDocument7 pages17 - Enhanced Recovery Principlesbocah_britpopNo ratings yet
- 03 - Energy BalanceDocument8 pages03 - Energy Balancebocah_britpopNo ratings yet
- 17 - Enhanced Recovery PrinciplesDocument7 pages17 - Enhanced Recovery Principlesbocah_britpopNo ratings yet
- m84 PDFDocument14 pagesm84 PDFMico Ga Bisa GendutNo ratings yet
- 17 - The Traumatized PatientDocument7 pages17 - The Traumatized Patientbocah_britpopNo ratings yet
- Interaction of Bone and Vascular Disease in CKDDocument7 pagesInteraction of Bone and Vascular Disease in CKDbocah_britpopNo ratings yet
- 17 - The Traumatized PatientDocument7 pages17 - The Traumatized Patientbocah_britpopNo ratings yet
- Materi PerioperatifDocument11 pagesMateri PerioperatifSyahdat NurkholiqNo ratings yet
- 08 - Oral and Sip FeedingDocument11 pages08 - Oral and Sip Feedingbocah_britpopNo ratings yet
- Indications, Contraindications and Monitoring of Enteral NutritionDocument13 pagesIndications, Contraindications and Monitoring of Enteral Nutritionbocah_britpopNo ratings yet
- 08 - Oral and Sip FeedingDocument11 pages08 - Oral and Sip Feedingbocah_britpopNo ratings yet
- 09 - Compounding and Ready-To-use Preparation of PN Pharmaceutical Aspects. Compatibility and Stability Consideration DrugDocument21 pages09 - Compounding and Ready-To-use Preparation of PN Pharmaceutical Aspects. Compatibility and Stability Consideration Drugbocah_britpopNo ratings yet
- 08 - Complications and Monitoring of enDocument7 pages08 - Complications and Monitoring of enbocah_britpopNo ratings yet
- 17 - Enhanced Recovery PrinciplesDocument7 pages17 - Enhanced Recovery Principlesbocah_britpopNo ratings yet
- 09 - Compounding and Ready-To-use Preparation of PN Pharmaceutical Aspects. Compatibility and Stability Consideration DrugDocument21 pages09 - Compounding and Ready-To-use Preparation of PN Pharmaceutical Aspects. Compatibility and Stability Consideration Drugbocah_britpopNo ratings yet
- Presentation 1Document2 pagesPresentation 1bocah_britpopNo ratings yet
- 08 - Techniques of Enteral NutritionDocument16 pages08 - Techniques of Enteral Nutritionbocah_britpopNo ratings yet
- Materi PerioperatifDocument11 pagesMateri PerioperatifSyahdat NurkholiqNo ratings yet
- Interaction of Bone and Vascular Disease in CKDDocument7 pagesInteraction of Bone and Vascular Disease in CKDbocah_britpopNo ratings yet
- ACS SabistonDocument10 pagesACS Sabistonbocah_britpopNo ratings yet
- Weekly ChartDocument7 pagesWeekly Chartbocah_britpopNo ratings yet
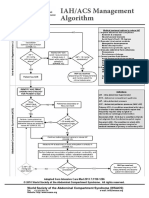
- IAH ACS Medical Management 2014Document1 pageIAH ACS Medical Management 2014bocah_britpopNo ratings yet
- Intraabdominal Pressure MonitoringDocument10 pagesIntraabdominal Pressure Monitoringbocah_britpopNo ratings yet
- University of Colorado NICHE Practice Survey SummaryDocument48 pagesUniversity of Colorado NICHE Practice Survey Summarybocah_britpopNo ratings yet
- Case Disc RadioDocument29 pagesCase Disc Radiobocah_britpopNo ratings yet
- IAH/ACS Management Algorithm Adapted from Intensive Care MedDocument1 pageIAH/ACS Management Algorithm Adapted from Intensive Care Medbocah_britpopNo ratings yet
- Upper Abdominal Pain Case ReportDocument2 pagesUpper Abdominal Pain Case Reportbocah_britpopNo ratings yet
- HydrocephalusDocument51 pagesHydrocephalusbocah_britpopNo ratings yet
- SOW Fabrikasi C-335-01 - 19.116.1Document1 pageSOW Fabrikasi C-335-01 - 19.116.1AlfanNo ratings yet
- SC - R Oil Free Compressor: Installation, Operation, & Maintenance Manual V2.13Document41 pagesSC - R Oil Free Compressor: Installation, Operation, & Maintenance Manual V2.13Luis JaimesNo ratings yet
- The Mental Training of A Tennis Player Using Biofeedback - Preliminary Case StudyDocument1 pageThe Mental Training of A Tennis Player Using Biofeedback - Preliminary Case StudyStefan LucianNo ratings yet
- The Best Way For A Client To Brief An AgencyDocument24 pagesThe Best Way For A Client To Brief An AgencyThien ThanhNo ratings yet
- Food Biotechnology LectureDocument36 pagesFood Biotechnology Lecturezekariyas kuneNo ratings yet
- Resume References - Brittany DrakeDocument3 pagesResume References - Brittany Drakeapi-661857782No ratings yet
- Operation of Portable Generators - IET Wiring GuideDocument7 pagesOperation of Portable Generators - IET Wiring GuideRyan Scott100% (1)
- Animal ProjectDocument1 pageAnimal Projectapi-377110324No ratings yet
- KVS Recruitment for Principal, PGT, TGT and PRT PostsDocument19 pagesKVS Recruitment for Principal, PGT, TGT and PRT PostsATI039 POOVAIMANAGAR GHSSNo ratings yet
- Adhi Wardana 405120042: Blok PenginderaanDocument51 pagesAdhi Wardana 405120042: Blok PenginderaanErwin DiprajaNo ratings yet
- SB66JRT English Hoogwerker Aerial Lift SnorkelDocument2 pagesSB66JRT English Hoogwerker Aerial Lift Snorkelhoogwerker0% (1)
- Data Flow Diagrams - Set 2Document72 pagesData Flow Diagrams - Set 2Blessing MotaungNo ratings yet
- English Learning Kit: Senior High SchoolDocument19 pagesEnglish Learning Kit: Senior High SchoolKare CaspeNo ratings yet
- Entrepreneur Vs ManagerDocument12 pagesEntrepreneur Vs ManagerHimadhar Sadu100% (1)
- Red Wing Style #3561Document1 pageRed Wing Style #3561Richard cruz 0845No ratings yet
- SQL COMMANDS FOR HIGH SCHOOL DATABASEDocument47 pagesSQL COMMANDS FOR HIGH SCHOOL DATABASESooraj Rajmohan75% (28)
- Algebra Geometry Statistics AllDocument26 pagesAlgebra Geometry Statistics AllDwin donever PacuriNo ratings yet
- Airbus A321-100 Lufthansa: Recolored by Cibula Papercraft 2019Document7 pagesAirbus A321-100 Lufthansa: Recolored by Cibula Papercraft 2019Siva Adithya100% (2)
- ENG 122 Introduction To LinguisticsDocument51 pagesENG 122 Introduction To Linguisticsalexbernard247No ratings yet
- RFBT-13 (Banking Laws)Document10 pagesRFBT-13 (Banking Laws)Alliah Mae ArbastoNo ratings yet
- Project RubricDocument6 pagesProject RubricShiela Aringo0% (1)
- Cekungan Tomori Dan SalawatiDocument17 pagesCekungan Tomori Dan SalawatiDimas WijayaNo ratings yet
- 1.super Value Titanium CardDocument3 pages1.super Value Titanium CardFasih AhmadNo ratings yet
- Chris Griswold's ResumeDocument2 pagesChris Griswold's ResumechrisgriswoldNo ratings yet
- Diagnostic X-Ray Generators: Fluoroscopy Radiography Tomography Digital RadiographyDocument6 pagesDiagnostic X-Ray Generators: Fluoroscopy Radiography Tomography Digital RadiographyWaheed MidoNo ratings yet
- Benny Lim Kian Heng ResumeDocument3 pagesBenny Lim Kian Heng ResumeMichael MyintNo ratings yet
- HexagonDocument15 pagesHexagonKiran Kumar YadaNo ratings yet
- Method of Preparation and Systematic Examination of A Direct Fecal SmearDocument3 pagesMethod of Preparation and Systematic Examination of A Direct Fecal SmearCelne CentinoNo ratings yet
- Taylor & Francis, Ltd. Public Performance & Management ReviewDocument26 pagesTaylor & Francis, Ltd. Public Performance & Management ReviewRamadona SimbolonNo ratings yet
- Bio (DWCL Main) - NoapplicDocument16 pagesBio (DWCL Main) - NoapplicPRC Board100% (1)