Professional Documents
Culture Documents
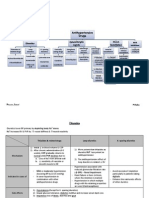
Antihypertensive Drugs
Uploaded by
Aiman TymerCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Antihypertensive Drugs
Uploaded by
Aiman TymerCopyright:
Available Formats
Anti-hypertensive drugs
Diuretics:
Thiazides: Hydrochlorothiazides, Chlorothalidone
High ceiling: Furosemide
K+ sparing: Spironolactone, Triamterene & Amiloride
MOA: Acts on kidneys to excretion of Na & H2O in blood volume blood pressure
Adverse effect
Hypokalaemia muscle pain & fatigue
Hyperglycemia : inhibition of insulin release due to K+ depletion (proinsulin to insulin) precipitation of diabetes
Hyperlipidemia : rise in total LDL level risk of stroke
Hyperurecaemia : inhibition of urate excretion
Sudden cardiac death tosades depointes (hypokalaemia)
All the above metabolic side effects ~ higher doses (50-100mg per day); but, its observed that these adverse effects are minimal with low doses
(12.5 25mg). Average fall in blood pressure is 10mm Hg
Angiontensin-converting Enzyme (ACE) inhibitors:
Captopril, Lisinopril, Enalapril, Ramipril & Fosinopril
MOA: Inhibits synthesis of Angiotensin II - in peripheral resistance & blood volume
Angiontensin I (AT-I) inhibitors:
Lasortan, Candesartan, Valsartan & Telmisartan
MOA: Blocks binding of AT-II to its receptors
Centrally acting:
Clonidine, Methyldopa
MOA: Act on central a 2A receptors to sympathetic outflow fall in blood pressure
Alpha-Methyldopa (prodrug) ~ precursor of Dopamine & NA
MOA: Converted to (alpha) methyl noradrenaline which acts on -2 receptors in brain & causes inhibiton of adrenergic discharge in
medulla fall in PVR (peripheral vessel resistance) & fall in blood pressure
Adverse effect
Cognitive impairment, postural hypotension, +ve Coombs test, etc (not used therapeutically now except in hypertesion in pregnancy)
Clonidine: Imidazoline derivative, partial agonist of central -2 receptors (not frequently used now because of tolerance &
withdrawal hypertension)
-adrenergic blockers:
Aiman Tymer 2012
Non-selective: Propanolol [others: Hadolol, Timolol, Pindolol, Labetolol]
Cardioselective: Metoprollol [others: Atenolol, Esmolol, Betaxolol]
MOA: Bind to -adrenergic receptors & blocks the activity
K+ channel activators:
Diazoxide, Minoxidil & Nicorandil
MOA: Leaking of K+ due to opening hyperpolarization of smooth muscle cells relaxation of smooth muscle cells
Vasodilators:
o Arteriolar: Hydralazine (also Calcium Channel Blockers & K+ channel activators)
o Arterio-venular: Sodium Nitroprusside
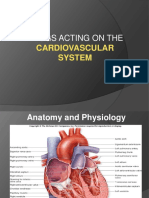
Calcium Channel Blockers ~ blocks influx of Ca2+ in smooth muscle cells relaxation of smooth muscle cells - blood pressure
MOA: 3 types Ca2+ channels in smooth muscles voltage sensitive, receptor operated & leak channel
1. Voltage sensitive 3 types (L-typer, T-typer, N-type)
Normally, L-typer of channels admit Ca2+ & causes depolarization excitation-contraction coupling through phosphorylation of myosin light chain
contraction of vascular smooth muscle elevation of blood pressure
Calcium Channel Blocker L-type:
Smooth muscle relaxation
-ve chronotropic, ionotropic, chronotropic effects in heart
DHPs have highest smooth muscle relaxation & vasodilator action followed by Verapamil & Diltiazem; Other action: DHPs have diuretic
action
Advantage
Unlike diuretics, no adverse metabolic effetcs but mild adverse effect like ~ dizziness, fatigue, etc
Do not compromise haemodynamics= no impairment of work capacity
No sedation / CNS effect
Can be given to asthma, angina & PVD patients
No renal & male sexual function impairment
No adverse fetal effects & can be given in pregnancy
Minimal effect on quality of life
Contraindication
Unstable angina
Heart failure
Hypotension
Aiman Tymer 2012
Post infarct cases
Severe aortic stenosis
Vasodilators:
o Arteriolar: Hydralazine (also Calcium Channel Blockers & K+ channel activators)
o Arterio-venular: Sodium Nitroprusside
Directly acting vasodilators:
MOA: Hydralazine molecules combine with receptor in endothelium of arterioles NO release relaxation of vascular smoth muscle fall
in BP
Subsequently fall in blood pressure stimulation of adrenergic sys leading to cardiac stimulation producing palpitation & cardiac output
even in IHD & patients anginal attack; Tachycardia; renin secretion Na+ retention (these effects are encoutered by administration of
blockers & diuretics, however many do not agree to this theory)
Uses
I. Moderate hypertension when 1st line fails with -blocker & diuretics
II. Hypertension in pregnancy
Treatment of hypertension General Principles
1) Stage 1
Start with a single most appropriate drug with a low dose, preferably start with Thiazides, others like -blockers, Calcium
Channel Blockers (CCB), ARBs & Angiotensin-converting Enzyme (ACE) inhibitors may also be considered. CCB in case of elderly
& stroke prevention. If required dose moderately.
Partial response / no response add from another group of drug, but remember it should be a low dose combination.
If not controlled change to another low dose combination
In case of side effects lower dose / substitute with other group
2) Stage 2
Start with 2 drug combination one should diuretic
3) In clinical practice a large number of patient require combination therapy the combination should rational & from different patterns of
haemodynamic effects
Sympathetic inhibitors (not -blockers) & vasodilators + diuretics
Diuretics, CCB, ACE inhibitors & vasodilators + -blockers (block renin release)
Hydralazine & CCB + -blockers (tachycardia countered)
ACE inhibitors + diuretics
4) 3 drugs combination: CCB + ACE / ARB + diuretics; CCB + -blockers + diuretic; ACE / ARB + -blockers + diuretic
5) Never combine:
Aiman Tymer 2012
/ - blocker & Clonidine antagonist
Nifedepine & diuretic synergism
Hydralazine with DHP / Prazosin same type of action
Ditiazem & Verapamil with -blocker bradycardia
Methyldopa & Clonidine
6) Hypertension & pregnancy
No drug is safe during pregnancy
Avoid diuretics, Propranolol, ACE inhibitor, Sodium nitroprusside, etc
Safer drugs: Hydralazine, Methyldopa, Cardioselective -blockers & Prazosin
All -blockers similar antihypertensive effetcs irrespective of additional properties]
o Reduction in cardiac output (CO) but no change in blood pressure (BP) initaially but slowly
o Adaptation by residence vessels to chronically reduced CO antihypertensive action
o Other mechanisms - renin release from kidney (-1 mediated)
o Reduced NA release & central sympathetic outflow reduction
o Non-selective ones reduction in g.f.r. but not with selective one
o Drugs with intrinsic sympathomimetic activity may cause less reduction in heart rate (HR) & CO
Drawback (side effects)
o Fatigue, lethargy (low CO) - work capacity
o Loss of libido impotence
o Cognetive defects - forgetfulness
o Difficult to stop suddenly
Therefore cardio-selective drugs are preffered now
Aiman Tymer 2012
& adrenergic blockers: Labetolol & Carbedilol
adrenergic blockers:
Prazosin, terazosin, doxazosin, phenoxybenzamine & phentolamine
MOA: Blocking of adrenergic receptors in smooth muscles vasodilatation
Non-selective blockers are not used in chronic essential hypertension (phenoxybenzamine, phentolamine), only used sometimes as in
phaechromocytoma
Specific -1 blockers like Prazosin, Terazosin & Doxazosine are used
Prazosin is the prototype of -blockers
Redcution in t.p.r. & mean BP also reduction in venomotor tone & pooling of blood reduction in CO
Does not produce tachycardia as presynaptic auto (-2) receptor are not inhibited autoregulation of NA release remains intact
Adverse effect
Prazosin causes postural hypotension start 0.5mg at bed time with dose & up to 10mg daily
Fluid retention in monotherapy
Headache, dry mouth, weakness, blurred vision, rash, drowsiness, failure of ejaculation in males
Aiman Tymer 2012
You might also like
- Atrial Fibrillation A Simple Guide to The Condition, Treatment And Related DiseasesFrom EverandAtrial Fibrillation A Simple Guide to The Condition, Treatment And Related DiseasesRating: 4 out of 5 stars4/5 (1)
- Antihypertensive Drugs: Dr/Azza Baraka Prof of Clinical Pharmacology Faculty of Medicine Alexandria UniversityDocument71 pagesAntihypertensive Drugs: Dr/Azza Baraka Prof of Clinical Pharmacology Faculty of Medicine Alexandria UniversityMoonAIRNo ratings yet
- Antihypertensive AgentsDocument41 pagesAntihypertensive AgentsRwapembe StephenNo ratings yet
- NAPLEX Practice Question Workbook: 1,000+ Comprehensive Practice Questions (2023 Edition)From EverandNAPLEX Practice Question Workbook: 1,000+ Comprehensive Practice Questions (2023 Edition)Rating: 4.5 out of 5 stars4.5/5 (3)
- Hypertension TejaDocument64 pagesHypertension TejaAnushka MaheshwariNo ratings yet
- Lec 22 ANTIHYPERTENSIVE - 2Document22 pagesLec 22 ANTIHYPERTENSIVE - 2Abdul MananNo ratings yet
- Cardiovascular Endocrinology and Metabolism: Theory and Practice of Cardiometabolic MedicineFrom EverandCardiovascular Endocrinology and Metabolism: Theory and Practice of Cardiometabolic MedicineAndrew J. KrentzNo ratings yet
- CVS PharmacologyDocument60 pagesCVS PharmacologyGølà Sèèñàà–baale irraaNo ratings yet
- Anti Hypertensive DrugsDocument46 pagesAnti Hypertensive DrugsShabaka KashataNo ratings yet
- Anti Hypertensive 20191211Document35 pagesAnti Hypertensive 20191211helloitsmenadNo ratings yet
- 10 and 11 Treatment of Hypertension and AnginaDocument10 pages10 and 11 Treatment of Hypertension and AnginaBrandon AviciiNo ratings yet
- Anti-hypertensive Drugs GuideDocument16 pagesAnti-hypertensive Drugs GuideALNAKINo ratings yet
- HTN JmiDocument39 pagesHTN Jmink999999No ratings yet
- Cardiology Review: HTN: Julia Akaah M.DDocument40 pagesCardiology Review: HTN: Julia Akaah M.DJose LunaNo ratings yet
- Essential Guidelines for Managing HypertensionDocument23 pagesEssential Guidelines for Managing HypertensionMaulana HasanNo ratings yet
- Antinanginal DrugsDocument43 pagesAntinanginal DrugsHUZAIFA YAMAANNo ratings yet
- ANTIHYPERTENSIVE DRUGS: DIURETICS, BETA-BLOCKERS, ACE INHIBITORSDocument37 pagesANTIHYPERTENSIVE DRUGS: DIURETICS, BETA-BLOCKERS, ACE INHIBITORSIrna Purwanti RahayuNo ratings yet
- Ishac M2 Cardio Antihypertensives 2010Document16 pagesIshac M2 Cardio Antihypertensives 2010Franchesca LugoNo ratings yet
- HypertensionDocument54 pagesHypertensionBadri KarkiNo ratings yet
- Antihypertensive & Antianginal DrugsDocument5 pagesAntihypertensive & Antianginal Drugsdomememe1No ratings yet
- 7,8 - Antihypertensive DrugsDocument10 pages7,8 - Antihypertensive DrugsHusniya MehamedNo ratings yet
- Antihypertensive Drugs.Document35 pagesAntihypertensive Drugs.Abdul WahabNo ratings yet
- Antihypertensive Drugs ٠١١٦٥٨Document10 pagesAntihypertensive Drugs ٠١١٦٥٨mohnad806mNo ratings yet
- Antihypertensive Agents GuideDocument3 pagesAntihypertensive Agents GuideCharles BayogNo ratings yet
- FARMAKOGNOSI - Obat AntihipertensiDocument7 pagesFARMAKOGNOSI - Obat AntihipertensiTrianisa FebyNo ratings yet
- 1 Antihypertensive DrugsDocument14 pages1 Antihypertensive DrugsReda SoNo ratings yet
- Lecture 1 antihypertensionSDSDocument7 pagesLecture 1 antihypertensionSDSSara AbbasNo ratings yet
- Anoosha Roll#21Document19 pagesAnoosha Roll#21Anusha ZubairNo ratings yet
- Hypertension PDFDocument57 pagesHypertension PDFrahul m dNo ratings yet
- Antihypertensive DrugsDocument7 pagesAntihypertensive Drugshamadadodo7No ratings yet
- Cholinergic System: e CarbamatesDocument26 pagesCholinergic System: e CarbamatesAcai BoncaiNo ratings yet
- Anti-Hypertensive Drugs Classification and MechanismsDocument64 pagesAnti-Hypertensive Drugs Classification and MechanismsPSC100% (1)
- Antihypertensive AgentsDocument52 pagesAntihypertensive Agentssameena ramzanNo ratings yet
- Class: Statin (PCKS9 Inhibitors) o High Intensity: Atorvastatin (Lipitor), Rosuvastatin (Crestor)Document15 pagesClass: Statin (PCKS9 Inhibitors) o High Intensity: Atorvastatin (Lipitor), Rosuvastatin (Crestor)LionelWrightNo ratings yet
- Study Guide For Final Pharmacology HypertensionDocument39 pagesStudy Guide For Final Pharmacology HypertensionAlejandro Daniel Landa MoralesNo ratings yet
- Anti-Anginal Drugs ExplainedDocument19 pagesAnti-Anginal Drugs ExplainedAnusha ZubairNo ratings yet
- Antihypertensive Drugs: Loretta Walker, PH.DDocument11 pagesAntihypertensive Drugs: Loretta Walker, PH.DAdrian Jake LiuNo ratings yet
- Antihypertensive Drugs: HypertensionDocument8 pagesAntihypertensive Drugs: Hypertensionalmastar officeNo ratings yet
- Sympatholytic DrugsDocument20 pagesSympatholytic DrugsAudrey Beatrice Reyes100% (1)
- 11A Drugs Acting On The Cardiovascular SystemDocument85 pages11A Drugs Acting On The Cardiovascular SystemJaps De la CruzNo ratings yet
- AntiHypertensives (Autosaved)Document64 pagesAntiHypertensives (Autosaved)UsamaNo ratings yet
- CHF Drugs Guide: Key Medications for Treating Congestive Heart FailureDocument21 pagesCHF Drugs Guide: Key Medications for Treating Congestive Heart Failuremohsen mirdamadiNo ratings yet
- Anti Hypertensives Overvi-35247Document40 pagesAnti Hypertensives Overvi-35247Alben SigamaniNo ratings yet
- Anti Hypertensive DrugsDocument9 pagesAnti Hypertensive DrugsBaqir BroNo ratings yet
- Drugs For Congestive Heart FailureDocument46 pagesDrugs For Congestive Heart Failuresultan khabeeb100% (1)
- Hypertension An OverviewDocument214 pagesHypertension An OverviewdkhandkeNo ratings yet
- Cvs DrugsDocument106 pagesCvs DrugsIkoona ivanNo ratings yet
- CVD and HTNDocument60 pagesCVD and HTNZsazsa100% (1)
- Lecture 24-25 - Antihypertensive AgentsDocument30 pagesLecture 24-25 - Antihypertensive AgentsJedoNo ratings yet
- M. Gabriel Khan - Cardiac Drug Therapy, Calcium Channel BlockersDocument21 pagesM. Gabriel Khan - Cardiac Drug Therapy, Calcium Channel BlockersluongcongthucNo ratings yet
- Congestive Heart Failure: CardiacDocument36 pagesCongestive Heart Failure: CardiacHUZAIFA YAMAANNo ratings yet
- Adrenergic Antagonists: An Introduction to Alpha and Beta BlockersDocument64 pagesAdrenergic Antagonists: An Introduction to Alpha and Beta BlockersAneeza AhmadNo ratings yet
- Pharmacology - Use of Beta-Blockers & Arbs in Cardiovascular Disease Treating HypertensionDocument5 pagesPharmacology - Use of Beta-Blockers & Arbs in Cardiovascular Disease Treating HypertensionDana20SNo ratings yet
- Antihypertensive DrugsDocument37 pagesAntihypertensive Drugsleiann_jessicaNo ratings yet
- Dr Bahram Soltan - Hypertension Mechanisms and TreatmentDocument64 pagesDr Bahram Soltan - Hypertension Mechanisms and TreatmentParsa EbrahimpourNo ratings yet
- CVPR Prototype Drugs TableDocument27 pagesCVPR Prototype Drugs TablethommyvaNo ratings yet
- Vasodilators by Hiren PatelDocument28 pagesVasodilators by Hiren PatelHiren_Patel_2427No ratings yet
- 3.07 AntiHypertensive Drugs, COMJ, 2022Document35 pages3.07 AntiHypertensive Drugs, COMJ, 2022JedoNo ratings yet
- LeprosyDocument27 pagesLeprosyAiman TymerNo ratings yet
- MycosesDocument28 pagesMycosesAiman TymerNo ratings yet
- PYODERMADocument45 pagesPYODERMAAiman Tymer80% (5)
- Pyoderma (Derma Presentation)Document11 pagesPyoderma (Derma Presentation)Aiman Tymer100% (1)
- Lupus ErythematosusDocument7 pagesLupus ErythematosusAiman TymerNo ratings yet
- Psy Exam 5th Year PDFDocument47 pagesPsy Exam 5th Year PDFAiman TymerNo ratings yet
- Neuro DermatitisDocument19 pagesNeuro DermatitisAiman Tymer100% (1)
- EczemaDocument19 pagesEczemaAiman TymerNo ratings yet
- Echzema DermatitisDocument7 pagesEchzema DermatitisAiman TymerNo ratings yet
- SclerodermaDocument36 pagesSclerodermaAiman TymerNo ratings yet
- SclerodermaDocument9 pagesSclerodermaAiman TymerNo ratings yet
- Dermatology Lupus Erythematosus: Name: Muhammad Nooraiman Ahmad Noordin Group: 30 ADocument14 pagesDermatology Lupus Erythematosus: Name: Muhammad Nooraiman Ahmad Noordin Group: 30 AAiman TymerNo ratings yet
- Genital Herpes: Aarthi (2012)Document36 pagesGenital Herpes: Aarthi (2012)Aiman TymerNo ratings yet
- Viral Hepatitis: by Shalini Hazael, Group 40aDocument24 pagesViral Hepatitis: by Shalini Hazael, Group 40aAiman TymerNo ratings yet
- Chlamydia: Harsheni Chandran 40 ADocument13 pagesChlamydia: Harsheni Chandran 40 AAiman TymerNo ratings yet
- Genital Herpes: Aarthi (2012)Document36 pagesGenital Herpes: Aarthi (2012)Aiman TymerNo ratings yet
- Donovanosis (Granuloma Inguinale) .PpsDocument14 pagesDonovanosis (Granuloma Inguinale) .PpsAiman TymerNo ratings yet
- Diagnostics of SyphilisDocument18 pagesDiagnostics of SyphilisAiman TymerNo ratings yet
- Donovanosis (Granuloma Inguinale) .PpsDocument14 pagesDonovanosis (Granuloma Inguinale) .PpsAiman TymerNo ratings yet
- Yaw (Tropical Syphilis)Document16 pagesYaw (Tropical Syphilis)Aiman Tymer100% (1)
- Blood Normal TableDocument1 pageBlood Normal TableAiman TymerNo ratings yet
- Pinta (Tropical Syphilis)Document17 pagesPinta (Tropical Syphilis)Aiman Tymer100% (1)
- Test Surgery Exam (Eng)Document36 pagesTest Surgery Exam (Eng)Aiman TymerNo ratings yet
- Micro Sample Patan ExamDocument15 pagesMicro Sample Patan ExamAiman TymerNo ratings yet
- Surgery Examination - 3-4 (Question Cases) (Eng)Document45 pagesSurgery Examination - 3-4 (Question Cases) (Eng)Aiman TymerNo ratings yet
- Dermatology Scleroderma: Click To Edit Master Subtitle StyleDocument36 pagesDermatology Scleroderma: Click To Edit Master Subtitle StyleAiman Tymer100% (1)
- Macro Sample Pathan ExamDocument17 pagesMacro Sample Pathan ExamAiman TymerNo ratings yet
- LeprosyDocument27 pagesLeprosyAiman TymerNo ratings yet
- Dermatology Eczema: Click To Edit Master Subtitle StyleDocument19 pagesDermatology Eczema: Click To Edit Master Subtitle StyleAiman Tymer100% (1)
- BBL™ Mueller Hinton Broth: - Rev. 02 - June 2012Document2 pagesBBL™ Mueller Hinton Broth: - Rev. 02 - June 2012Manam SiddiquiNo ratings yet
- A 55-Year-Old Woman With Shock and Labile Blood PressureDocument11 pagesA 55-Year-Old Woman With Shock and Labile Blood PressureMr. LNo ratings yet
- Congenital SyphilisDocument28 pagesCongenital SyphilisMeena Koushal100% (4)
- 2018 Overview Digestive System HandoutDocument11 pages2018 Overview Digestive System HandoutdraganNo ratings yet
- Nursing Care Plan Neonatal PneumoniaDocument2 pagesNursing Care Plan Neonatal Pneumoniaderic93% (41)
- WORKSHEET 3 Lymphocyte ActivationDocument5 pagesWORKSHEET 3 Lymphocyte ActivationNeha ChoudharyNo ratings yet
- New Drugs 2014-2018Document31 pagesNew Drugs 2014-2018Prem Goel0% (1)
- Nursing Diagnosis For AsthmaDocument6 pagesNursing Diagnosis For AsthmaTINAIDA33% (3)
- 03 Biosecurity Jit PPT FinalDocument20 pages03 Biosecurity Jit PPT FinalReza WratsongkoNo ratings yet
- Pneumonia: Causes, Signs, Symptoms and Nursing CareDocument16 pagesPneumonia: Causes, Signs, Symptoms and Nursing CareMelissa David100% (1)
- Salivation PDFDocument5 pagesSalivation PDFmehdi mafakheri100% (1)
- Superannuation Benefits SessionDocument49 pagesSuperannuation Benefits SessionfunshareNo ratings yet
- Scientific Breakthroughs in Autophagy MechanismsDocument7 pagesScientific Breakthroughs in Autophagy MechanismshananNo ratings yet
- Food For The BrainDocument34 pagesFood For The BrainKristine Mae AbrasaldoNo ratings yet
- Acute and Chronic PyelonephritisDocument7 pagesAcute and Chronic PyelonephritisMatthew Ryan100% (1)
- Indian Herbs Cooking GuideDocument37 pagesIndian Herbs Cooking Guidehitesh mendirattaNo ratings yet
- Science Magazine, Issue 6657 (August 4, 2023)Document175 pagesScience Magazine, Issue 6657 (August 4, 2023)Kim LevrelNo ratings yet
- Biochem SGD 3Document4 pagesBiochem SGD 3Hemanth KokaNo ratings yet
- CDC's HIV Infection Through Oral Sex, Fact SheetDocument2 pagesCDC's HIV Infection Through Oral Sex, Fact SheetCésar E. ConcepciónNo ratings yet
- Letter WritingDocument17 pagesLetter WritingEmtiaj RahmanNo ratings yet
- WHATs New in CPCRDocument4 pagesWHATs New in CPCRJessicaHernandezNo ratings yet
- GugulipidDocument7 pagesGugulipidManish WadhwaniNo ratings yet
- Bipolar Depression Diagnosis and Treatment OptionsDocument21 pagesBipolar Depression Diagnosis and Treatment OptionsThuvija DarshiniNo ratings yet
- Sermon On Spirituality & Mental Illness by Rev Laura MancusoDocument12 pagesSermon On Spirituality & Mental Illness by Rev Laura MancusoRev. Laura L. MancusoNo ratings yet
- Introduction of PHCDocument39 pagesIntroduction of PHCIdiris Mohamed100% (1)
- 2023 Summit Program Draft 5 Apr18Document43 pages2023 Summit Program Draft 5 Apr18Raheem KassamNo ratings yet
- ABG AnalysisDocument15 pagesABG AnalysisPabhat Kumar100% (2)
- Section 5 - Students WorksheetDocument4 pagesSection 5 - Students WorksheetEsraa AhmedNo ratings yet
- Physical Paper +1ANNUALDocument5 pagesPhysical Paper +1ANNUALprabhnoorprimeNo ratings yet
- The Circulatory System - Lecture STEMDocument50 pagesThe Circulatory System - Lecture STEMMargeory Calatan100% (1)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (402)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 3.5 out of 5 stars3.5/5 (2)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (78)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (13)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- Techniques Exercises And Tricks For Memory ImprovementFrom EverandTechniques Exercises And Tricks For Memory ImprovementRating: 4.5 out of 5 stars4.5/5 (40)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 5 out of 5 stars5/5 (4)
- The Ultimate Guide To Memory Improvement TechniquesFrom EverandThe Ultimate Guide To Memory Improvement TechniquesRating: 5 out of 5 stars5/5 (34)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 5 out of 5 stars5/5 (4)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisFrom EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisRating: 5 out of 5 stars5/5 (8)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 3.5 out of 5 stars3.5/5 (33)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Summary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisFrom EverandSummary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisRating: 5 out of 5 stars5/5 (3)
- The Happiness Trap: How to Stop Struggling and Start LivingFrom EverandThe Happiness Trap: How to Stop Struggling and Start LivingRating: 4 out of 5 stars4/5 (1)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsFrom EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsNo ratings yet
- The Tennis Partner: A Doctor's Story of Friendship and LossFrom EverandThe Tennis Partner: A Doctor's Story of Friendship and LossRating: 4.5 out of 5 stars4.5/5 (4)