Professional Documents
Culture Documents
Pulmonary Tuberculosis in Infants: Radiographic and CT Findings
Uploaded by
Rahma Puji LestariOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pulmonary Tuberculosis in Infants: Radiographic and CT Findings
Uploaded by
Rahma Puji LestariCopyright:
Available Formats
Kim et al.
Pe d i a t r i c I m a g i n g C l i n i c a l O b s e r v a t i o n s
Radiography
and CT of
Pulmonary
Tuberculosis
in Infants
Downloaded from www.ajronline.org by 36.79.19.147 on 04/29/15 from IP address 36.79.19.147. Copyright ARRS. For personal use only; all rights reserved
A C E N T U
R Y O F
Pulmonary Tuberculosis in Infants:
MEDICAL IMAGING
Radiographic and CT Findings
Woo Sun Kim1 OBJECTIVE. As complications of tuberculosis are frequent in infancy, correct diagnosis
Joon-Il Choi1,2 of tuberculosis in infants is important. The purposes of this study are to summarize radio-
Jung-Eun Cheon1 graphic and CT findings of pulmonary tuberculosis in infants and to determine the radiologic
In-One Kim1 features frequently seen in infants with this disease.
Kyung Mo Yeon1 CONCLUSION. Frequent radiologic findings of pulmonary tuberculosis in infants are
mediastinal or hilar lymphadenopathy with central necrosis and air-space consolidations, es-
Hoan Jong Lee3
pecially masslike consolidations with low-attenuation areas or cavities within the consolida-
Kim WS, Choi J-I, Cheon J-E, Kim I-O, Yeon tion. Disseminated pulmonary nodules and airway complications are also frequently detected
KM, Lee HJ in this age group. CT is a useful diagnostic technique in infants with tuberculosis because it can
show parenchymal lesions and tuberculous lymphadenopathy better than chest radiography.
CT scans can also be helpful when chest radiographs are inconclusive or complications of tu-
berculosis are suspected.
uberculosis remains an important disease in patients whose chest radiographs
T cause of morbidity and mortality
worldwide. Mainly as a result of
the worsening HIV epidemic,
are normal or equivocal. CT scans can re-
veal lymphadenopathy; calcifications; bron-
chogenic nodules; and complications such
homelessness, drug abuse, and immigration as airway narrowing, emphysema, and pleu-
from developing countries, the problem of ral effusion [1217]. High-resolution CT
pulmonary tuberculosis in Western countries may depict miliary nodules or bronchogenic
has markedly increased [14]. Children rep- nodules in the lung parenchyma, especially
resent one of the high-risk groups in the resur- in patients with no evidence of nodules on
gence of this disease [57]. Among children, the chest radiograph [17, 18]. Although a
Keywords: chest, CT, infant/neonate, primary tuberculosis, those younger than 5 years are at the highest few studies have reported chest radio-
chest radiography, tuberculosis risk for pulmonary tuberculosis [2]. graphic findings of infant tuberculosis
Pulmonary tuberculosis in infants has some [79], CT findings of the disease have been
DOI:10.2214/AJR.04.0751
differences from that seen in older children; it is reported only sporadically [16, 19]. The
Received May 11, 2004; accepted after revision more symptomatic, and the risk of severe and purposes of this study are to summarize ra-
June 7, 2005. life-threatening complications such as tubercu- diographic and CT findings of pulmonary
lous meningitis or miliary tuberculosis is higher tuberculosis in infants and identify the fre-
1Department of Radiology, Seoul National University [79]. Therefore, early diagnosis and prompt quent radiologic findings of pulmonary tu-
College of Medicine Institute of Radiation Medicine,
treatment are very important for infants with tu- berculosis in infants.
SNUMRC (Seoul National University Medical Research
Center), Seoul, Korea. berculosis. Bacteriologic confirmation of the
disease in children is difficult [5, 10, 11], and in Materials and Methods
2Present address: Department of Radiology, National younger infants (< 3 months), the tuberculin We retrospectively reviewed chest radiographs
Cancer Center, 809 Madu-I-dong, Islan dong-gu, skin test is frequently negative [811]. There- (n = 25) and chest CT scans (n = 17) of 25 consec-
Goyang-si, Gryeonggi-do, Korea. Address correspondence
to J.-I. Choi (dumkycji@hanmail.net).
fore, chest radiographs and a history of direct utive infants who were diagnosed with pulmonary
contact with patients who have contagious tu- tuberculosis in our institution from 1991 to 2003.
3Department of Pediatrics, Seoul National University berculosis play essential roles in diagnosing tu- The diagnosis of tuberculosis was established by
College of Medicine, Seoul, Korea. berculosis in infants. The importance of the role positive culture or staining of gastric aspirates for
AJR 2006; 187:10241033
of radiologists cannot be overemphasized. acid-fast bacilli in four patients, positive results of
CT scans have advantages over conven- polymerase chain reaction for Mycobacterium
0361803X/06/18741024
tional radiographs in diagnosing tuberculo- tuberculosis in five patients, positive culture of
American Roentgen Ray Society sis in pediatric patients and can detect the ascites for M. tuberculosis in one, and surgical
1024 AJR:187, October 2006
Radiography and CT of Pulmonary Tuberculosis in Infants
Fig. 14-month-old girl with pulmonary tuberculosis (patient 15). Masslike
consolidation and bronchial obstruction caused by hilar lymphadenopathy.
A, Chest radiograph shows consolidation in right lower lung zone (asterisk) and
widening of right upper mediastinum (arrows).
B, Enhanced CT scan shows well-defined, well-enhancing, masslike consolidation in
right lower lobe (asterisk). Note low-attenuation lymphadenopathy (arrow)
obstructing bronchus intermedius.
C, CT scan in lower level of image seen in B shows large consolidation in right middle
Downloaded from www.ajronline.org by 36.79.19.147 on 04/29/15 from IP address 36.79.19.147. Copyright ARRS. For personal use only; all rights reserved
lobe and right lower lobe. Consolidation is slightly volume expanding. There are
multiple low-attenuation areas (arrows) in consolidation area.
A C
biopsy in one. In the remaining 14 patients, more promised, and none were HIV positive. Twenty-one lows: brain (n = 4), liver (n = 2), spleen (n = 3), and
than two of the following three criteria were met patients were vaccinated with BCG (bacille Cal- kidney (n = 1). The median duration of symptoms
[20]: tuberculin skin test (Mantoux test) with five mette-Gurin) at the age of 4 weeks. Physical ex- before the diagnosis of tuberculosis and start of an-
tuberculin units of purified protein derivative that amination of the BCG site and the regional lymph tituberculous medication was 50 days (range, 190
resulted in an area of induration of 10 mm or nodes revealed no abnormalities. The Mantoux test days). In four infants (16%), the duration of symp-
greater; ruling out other causes of disease and was performed in all patients and showed positive toms was less than 1 week.
finding that subsequent clinical course of the dis- results in 11 (44%). Seven patients (28%) were ex- Initial chest radiographs were available in all pa-
ease was consistent with tuberculosis (clinical or posed to household members with active pulmo- tients. Follow-up chest radiographs were available
radiologic improvement from antituberculous nary tuberculosis. Symptoms of the patients were in 23 patients. The radiographic follow-up was not
medications); and discovery of at least one family fever (84%), cough (76%), sputum (48%), rhinor- uniform in all patients, and the mean follow-up du-
member with contagious tuberculosis. rhea (36%), and tachypnea (32%). In two patients, ration was 2 years (range, 4 months to 3.5 years).
The study group included 15 boys and 10 girls seizure was an initial manifestation with no signif- Chest CT scans were performed 110 days
ranging in age from 2 to 12 months (mean age, 5.9 icant respiratory symptoms. Systemic dissemina- (mean, 4 days) after initial chest radiography for
months). None of the children were immunocom- tion was discovered in eight patients (32%) as fol- one or more of the following reasons: to evaluate
AJR:187, October 2006 1025
Kim et al.
CT
On chest CT scans (n = 17), air-space con-
solidation was seen in all 17 patients. Masslike
consolidation was seen in 10 of 17 patients
(59%) (Figs. 1B, 1C, and 3C). The multifocal
low-attenuation areas within the consolidation
Downloaded from www.ajronline.org by 36.79.19.147 on 04/29/15 from IP address 36.79.19.147. Copyright ARRS. For personal use only; all rights reserved
were seen in seven patients (41%) (Figs. 1C
and 3C). Cavities within the consolidation
were observed in five patients (29%). In one
patient with a necrotic cavity within the con-
solidation, the necrotic cavity progressed to ex-
tensive bilateral bullous lesions; he was the
only patient who did not survive. Disseminated
pulmonary nodules were revealed in five pa-
tients (29%) (Figs. 3B, 4B, and 5B). In three of
them, disseminated nodules were larger (> 2
mm in diameter) than the usual miliary nodules
of adult tuberculosis and coalesced with each
other (Figs. 3B and 4B). In one patient, cavities
were seen within disseminated nodules
(Fig. 4B). Bronchogenic nodules were found
Fig. 26-month-old boy with pulmonary tuberculosis (patient 10). Large cavity within consolidation. in seven patients (41%). In all three patients
Chest radiograph shows large cavity within consolidation in right upper lobe (arrow). Multiple nodules are seen
who had high-resolution CT, centrilobular
in left upper lung field (arrowheads).
nodules or branching linear structures suggest-
ing bronchogenic spread of tuberculosis were
seen (Fig. 6B). Excluding patients with dis-
unusual findings on radiographs such as masslike were observed carefully. When we found a con- seminated nodules in both lungs, pulmonary
lesions or widespread nodules; to find or confirm solidation during the reviewing process, which parenchymal lesions were bilateral in six pa-
lymphadenopathy; and to detect or evaluate com- was enhancing well after contrast agent adminis- tients (50%) and involved the right upper lobe
plications such as airway narrowing with or with- tration, was volume preserving or expanding, and (n = 10), left upper lobe (n = 9), left lower lobe
out atelectasis or emphysema, or pleural or peri- had no air-bronchogram within it, we defined it as (n = 7), right lower lobe (n = 7), and right mid-
cardial tuberculosis. a masslike consolidation. dle lobe (n = 5).
CT scans were obtained with third-generation Mediastinal and hilar lymphadenopathies
CT scannersCT/T 9800 scanner or a HiSpeed Results were observed in all 17 patients. On enhanced
Advantage System (both manufactured by GE Chest Radiography CT, involved lymph nodes showed central low
Healthcare)at 40100 mA, 120 kVp, and 12 On chest radiography (n = 25), air-space attenuation and peripheral enhancement in all
seconds of scanning time. CT scans were obtained consolidation was the most common paren- patients (Figs. 1B and 6C). The right paratra-
after IV bolus injection of contrast media, with con- chymal lesion, occurring in 20 patients (80%) cheal and subcarinal nodes were the most fre-
tiguous 510-mm-thick sections from the lung apex (Fig. 1A). Nodular lesions were found in quently involved (for both, n = 13, 76%). Lym-
to the diaphragm. In three patients, supplementary seven patients (28%), and, among them, ipsi- phadenopathies of right hilar nodes were seen
high-resolution CT scans with 1.5-mm-thick sec- lateral or contralateral air-space consolidation in 10 of 17 patients (59%), left paratracheal
tions were obtained at 510-mm intervals with an was seen in five patients (Fig. 2). Dissemi- nodes were found in nine patients (53%), and
edge-enhancing algorithm. nated nodules were found in six patients left hilar nodes were found in seven (41%). In
Three radiologists analyzed the chest radio- (24%) (Figs. 3A, 4A, and 5A), and all of them two patients (12%), calcifications were seen
graphs and CT scans by consensus. In the chest were 4 months old or younger. Cavitations within the enlarged nodes.
radiographs, particular attention was given to the within parenchymal lesions were noted in two Airway complications were also frequent
pattern of pulmonary parenchymal lesions (con- patients (Figs. 2 and 4A). findings on CT scans. Bronchial narrowing
solidation, nodules, and disseminated disease), Mediastinal bulging, suggesting mediasti- was seen in 11 patients (65%) who had adja-
cavities within parenchymal lesions, mediastinal nal or hilar lymphadenopathy, was seen in 18 cent peribronchial lymphadenopathy (Figs. 6C
bulging suggesting lymphadenopathy, and airway patients (72%) (Fig. 1A), but discerning the and 6D). Hyperinflation of the lung with medi-
or pleural complications. On the CT scans, pat- difference between a pulmonary parenchymal astinal lymphadenopathy was seen in eight pa-
terns of pulmonary parenchymal lesions (air- lesion near the hilum and lymphadenopathy tients (47%) (Fig. 6B). Bronchiectasis was
space consolidation, bronchogenic nodules, and was difficult on chest radiographs in many found in one patient.
disseminated nodules); cavities within parenchy- cases. Hyperinflation of the lung (n = 8, 32%) Pleural effusions associated with air-space
mal lesions; mediastinal and hilar lymphadenop- (Fig. 6A), bronchial narrowing (n = 4, 16%) consolidation were seen in five patients (29%),
athy with or without central necrosis; airway (Fig. 6A), and atelectasis (n = 4, 16%) were and it was bilateral in one of them. Pleural effu-
complications; pleural, pericardial, and chest also frequent findings. We found pleural effu- sion was loculated in one patient. Pericardial
wall lesions; and involvement of other organs sion in one patient. thickening was detected in two patients.
1026 AJR:187, October 2006
Radiography and CT of Pulmonary Tuberculosis in Infants
Chest radiography and CT findings are (n = 4), confirmation of lymphadenopathy (n = 3). In four patients (24%), a diagnosis
summarized in Table 1. (n = 13), depiction of central necrosis of tuberculosis was suggested only after a
(n = 17) or calcification (n = 2) within the CT scan revealed enlarged lymph nodes with
Additional Information at CT enlarged lymph nodes, detection of bron- central necrosis (Table 1). Extrathoracic in-
In all 17 patients who had a CT scan, we chial stenosis distal to the lobar bronchus volvement (liver [n = 2], spleen [n = 3], and
acquired additional information that could (n = 7), revelation of pleural involvement kidney [n = 1]) of tuberculosis was revealed
Downloaded from www.ajronline.org by 36.79.19.147 on 04/29/15 from IP address 36.79.19.147. Copyright ARRS. For personal use only; all rights reserved
not be obtained at chest radiography: revela- (n = 4) and pericardial thickening (n = 2), in the chest CT scan in three patients with
tion of mediastinal lymphadenopathy and detection of extrathoracic lesions disseminated pulmonary nodules (Fig. 3D).
A B
C D
Fig. 34-month-old girl with systemic disseminated tuberculosis (patient 12).
A, Chest radiograph shows multiple disseminated nodules in both lungs and consolidation in left lower lung zone (asterisk).
B, Chest CT scan shows disseminated nodules of variable size. Most nodules are larger than 2 mm in diameter.
C, Enhanced CT scan shows consolidation with low-attenuation area (arrows) within it in superior segment of left lower lobe.
D, Numerous low-attenuation nodules are noted in spleen on enhanced CT scan.
AJR:187, October 2006 1027
Kim et al.
Fig. 44-month-old boy with acute disseminated tuberculosis (patient 14). Cavitary
changes in nodules are seen.
A, Chest radiograph shows numerous nodules in both lungs. Thin-walled cavity
(arrows) is seen in left lower lobe.
B, On chest CT, multiple variable-sized nodules are detected. Cavity formation in
some nodules is noted (arrows).
C, Follow-up chest radiograph obtained 1 year after A and B shows no parenchymal
nodule in either lung.
Downloaded from www.ajronline.org by 36.79.19.147 on 04/29/15 from IP address 36.79.19.147. Copyright ARRS. For personal use only; all rights reserved
A C
Follow-Up Chest Radiography at initial radiography, was improved in all of phatic vessels (appearing as a linear intersti-
On follow-up chest radiographs (n = 23), these patients at follow-up radiography. The tial pattern on chest radiographs) and results
mediastinal lymphadenopathy and paren- resolution of each radiographic finding after in regional lymphadenopathy. Together, the
chymal lesions had decreased in size in 74% antituberculous medication is summarized primary focus and the enlarged lymph nodes
(17/23) at 1 month after starting the pa- in Table 2. that drain it are called the Ranke complex
tients medication (Table 1). Improvement [2124]. In most cases, the mild parenchymal
of the air-space consolidation preceded re- Discussion lesions and lymphadenopathy resolve sponta-
gression of enlarged nodes, and complete Most pulmonary tuberculosis cases seen in neously. In some cases, however, especially in
resolution of the consolidation occurred infants are primary tuberculosis. The primary young infants, the involved lymph nodes con-
within 6 months (Fig. 4C) in all but the one infection begins with deposition of infected tinue to enlarge [11]. Caseation ne crosis of
patient who developed bullous parenchymal droplets in the lung alveoli, followed by pa- the regional lymph nodes progresses, and
lesions and died due to respiratory failure. renchymal inflammation [11, 21]. The initial the enlarged nodes may compress the regional
In two patients, residual lymphadenopathy inflammation produces localized alveolar bronchi and cause bronchial narrowing, ob-
was identified beyond 1 year (Table 2). New consolidation, which is the primary focus. struction, and emphysema [21, 22]. As dis-
calcifications and decreased lung volume This may, although rarely, progress to involve ease progresses, inflamed nodes can perforate
with focal fibrosis were noted in four pa- a segment or an entire lobe and usually is not neighboring bronchus and discharge caseous
tients and in three patients, respectively, visible on chest radiographs [21, 22]. Infec- material into the bronchial tree, causing bron-
among 18 patients, at 6 months (Fig. 5C). tion then spreads to the central lymph nodes chogenic tuberculosis and focal or lobar
Bronchial narrowing, seen in four patients from the primary focus via draining lym- pneumonia [25, 26].
1028 AJR:187, October 2006
Radiography and CT of Pulmonary Tuberculosis in Infants
Fig. 53-month-old boy (patient 1) with acute disseminated tuberculosis.
A, Chest radiograph shows multiple disseminated nodules with random distribution
in both lungs.
B, Chest CT scan shows multiple small nodules in both lungs.
C, On follow-up chest radiograph obtained after antituberculosis medication for 1
year, nodules are healed, leaving multiple calcifications. Note multiple calcifications
in spleen (arrows).
Downloaded from www.ajronline.org by 36.79.19.147 on 04/29/15 from IP address 36.79.19.147. Copyright ARRS. For personal use only; all rights reserved
B C
Mediastinal lymphadenopathy with or monary tuberculosis was a feature of early one patient revealed tuberculous meningitis
without parenchymal abnormality is a radio- childhood, occurring in 49% of cases; only with disseminated tuberculomas (patient 3).
logic hallmark of primary tuberculosis in 9% of patients in later childhood or adoles- In agreement with other studies [16, 17, 24],
childhood [2024]. In our study, chest radiog- cence showed such findings. However, in our disseminated tuberculosis seemed to be more
raphy showed mediastinal lymphadenopathy study, most patients revealed parenchymal common in infants than older children.
and parenchymal abnormality in 72% and changes in conjunction with lymphadenopa- It is well established that CT scans detect
96% of patients, respectively, and the most thy, and isolated mediastinal lymphadenopa- or confirm lymphadenopathy [1215, 27].
frequent radiographic finding of pulmonary thy without parenchymal abnormality was Delacourt et al. [14], in their series of 15
parenchymal lesions was consolidation rarely seen. In this study, chest radiography children with tuberculous infection and neg-
(80%). Leung et al. [20], in their series of 191 showed disseminated pulmonary tuberculosis ative chest radiography, found enlarged
children, reported age-related differences in in six patients (24%). All of them were 4 lymph nodes in 60% of patients on chest CT.
the prevalence of parenchymal abnormalities. months of age or younger. Disseminated nod- On enhanced CT scans, tuberculous lym-
Children 03 years old had a higher preva- ules were seen in the spleen (n = 2) or liver phadenopathy is seen as enlarged nodes
lence of lymphadenopathy (100%) and a (n = 1) in CT scans of two patients with dis- with low-attenuation centers because of
lower prevalence of parenchymal abnormali- seminated pulmonary tuberculosis (patients 3 caseation necrosis and peripheral rim en-
ties (51%) compared with those 415 years and 12). Diffuse enlargement of the liver, hancement representing inflammatory hy-
old. In their series, lymphadenopathy as the spleen, and kidney was noted in one patient pervascularity [13, 27, 28]. In our study, CT
only radiologic manifestation of primary pul- (patient 1) at CT scan. An MRI of the brain in scans delineated lymphadenopathy in four
AJR:187, October 2006 1029
Kim et al.
Downloaded from www.ajronline.org by 36.79.19.147 on 04/29/15 from IP address 36.79.19.147. Copyright ARRS. For personal use only; all rights reserved
A B
C D
Fig. 65-month-old girl (patient 2) with bronchogenic spread of tuberculosis and bronchial stenosis.
A, Chest radiograph shows left hilar bulging (white arrow) and hyperinflation of left lung. Note narrowing of left main bronchus (black arrows).
B, High-resolution CT scan reveals peribronchial infiltrations and peripheral small nodules (arrows) suggesting bronchogenic spread of tuberculosis in left upper lobe.
Hyperinflation of left lung is also noted.
C, CT scan shows narrowing of left main bronchus (black arrows) by enlarged subcarinal lymph nodes (white arrow).
D, Segmental bronchi (white arrow) of left upper lobe are also stenosed by hilar lymph nodes (asterisk). Note enlarged subcarinal lymph node with central low attenuation
(black arrows).
patients who were not suspected to have In our study, air-space consolidation was the frequently found masslike consolidation, which
lymphadenopathy on chest radiographs. most common of parenchymal lesions seen on was well enhancing, volume preserving or ex-
Therefore, CT scans can be helpful in diag- CT scans (100%), which was more common panding, and had no air bronchogram within it.
nosing tuberculosis when findings of chest than that reported in the literature for childhood As mentioned previously, enlarged hilar lymph
radiographs are inconclusive. cases (19% [12] and 49% [13]). In this study, we nodes can compress neighboring regional bron-
1030 AJR:187, October 2006
Radiography and CT of Pulmonary Tuberculosis in Infants
TABLE 1: Radiographic and CT Findings of Pulmonary Tuberculosis in 25 Infants
Patients Radiography CT
Parenchymal Lesion Follow-up
Age Mediastinal
No. (mo)/Sex Cons N DN Bulging Others 1 mo 6 mo Cons/Mass Low/Cv N-br DN LNE Others Extrathoracic
1 3/B + + + Ca++ +/ /+ + + Br L, Sp, Kd
Ca++
Downloaded from www.ajronline.org by 36.79.19.147 on 04/29/15 from IP address 36.79.19.147. Copyright ARRS. For personal use only; all rights reserved
2 5/G + + H, Br +/ + + H, Pl
3 2/G + + + N/A N/A +/ +/ + + L, Sp
4 5/B + H, A NC N/A +/+ + + (*) H, Br
5 6/B + + + H V +/ +/+ + + H, Br
6 3/B + + N/A +/+ + (Ca++) H, Br
7 7/B + + H, Br NC Ca++ +/+ +
8 6/B + + Br NC V +/+ + +
9 4/B + + + H, Br, A NL +/+ + + H
10 6/B + (Cv) + Deceased +/ +/+ + + Br, Pl, Pc, Be
11 3/B + + H NL +/+ /+ + + (*) H, Br, Pl
12 4/G + + + H NL +/+ +/ + + H, Br, Pc Sp
13 5/G + + NL +/+ +/ + (Ca++) H, Br
14 4/B + (Cv) + (Cv) NL +/ +/+ + (Cv) + (*) Br, Pl
15 4/G + + V +/+ +/ + Br, Pl
16 4/G + NL +/ + + (*)
17 12/G + + Ca++ +/+ + Br
18 12/B + + NL N/A
19 11/G + + + NC N/A N/A
20 4/B + + A N/A N/A N/A
21 8/G + + A NL N/A
22 11/B + + NL N/A
23 3/G + NC NL N/A
24 10/B + N/A N/A
25 5/B + NL N/A
NoteCons = consolidation of air space, N = nodules, DN = disseminated nodules, Mass = masslike consolidation, Low = low attenuation within the consolidation,
Cv = cavity, N-br = bronchogenically spread nodules, LNE = lymph node enlargement with central low attenuation and peripheral enhancement,
Extrathoracic = extrathoracic involvement detected on chest CT scans, B = boy, = improved pulmonary lesions, Ca++ = calcification, Br = bronchial narrowing, L = liver
involvement, Sp = spleen involvement, Kd = kidney involvement, G = girl, H = hyperinflation of the lung, Pl = pleural effusion or thickening, N/A = not available,
A = atelectasis, NC = no change, V = decreased lung volume with focal fibrosis, NL = normal, = aggravated pulmonary lesions, Pc = pericardial effusion or thickening,
Be = bronchiectasis, (*) = lymph node detected only at CT.
chus and cause diffuse inflammation of the Low-attenuation areas within the consoli- [30, 31]. In our study, one patient developed
bronchus [2123]. The common sequence is hi- dation, representing caseating necrosis, were an extensive bullous lesion.
lar lymphadenopathy, followed by atelectasis also more common in our study, at 41%, than It is well established that CT scans have ad-
and consolidation [11]. The resulting radiographic in that of Kim et al. [13], at 25%. Cavitations vantages over chest radiographs for detecting
findings have been called collapse-consolida- within consolidations were found in 29% of the brochogenic spread of tuberculosis [32]
tion, segmental lesions, and epituberculo- patients in our series. Cavitation, indicating and miliary tuberculosis [1618]. Although
sis [11, 22]. We believe the same disease high infectivity and high bacillary burden, is bronchogenic nodules were seen in only 29%
process described as collapse-consolidation can the hallmark radiographic findings in postpri- of patients with childhood tuberculosis [13],
explain masslike consolidation on CT mary tuberculosis [21, 29], and it is rare in they were found in 41% of patients in our
scans in our study. Collapse-consolidation is children with primary tuberculosis [11, study. Jamieson and Cremin [17] reviewed
more common in infants than older children and 1921]. Cavitation was frequently associated high-resolution CT findings of pulmonary tu-
tends to occur within months of the initial infec- with low-attenuation areas within consolida- berculosis in six young children with multiple
tion [11]. Although masslike consolidation was tions (3/5, 60%) in our study. Bullous or cys- disseminated nodules on chest radiographs. In
found in 59% of the patients with consolidation tic lesions in the lung can develop as a rare their study, disseminated nodules varied in size
on CT scans in our series, it was found in only complication. Necrosis and liquefaction in ar- and were even or irregular in distribution. They
15% of patients in the study by Kim et al. [13] eas of pneumonic consolidation are thought suggested using the term acute disseminated
of childhood tuberculosis. to be the cause of extensive bullous lesions tuberculosis rather than miliary tuberculo-
AJR:187, October 2006 1031
Kim et al.
TABLE 2: Resolution of Radiographic Findings After Antituberculous Medication it is rare in infants [8, 20]. In pleural tuberculo-
in Patients with Infantile Tuberculosis sis, CT scans are also helpful for determining
Follow-Up Times whether the thickening seen on chest radio-
Initial 1 month 3 months 6 months 1 year graphs represents pleural thickening; chronic
Radiographic Findings (n = 25) (n = 23) (n = 23) (n = 18) (n = 9) loculated effusion, which usually needs decorti-
Consolidation 20 13 7 0 0 cation; or empyema [35]. Table 3 summarizes
Downloaded from www.ajronline.org by 36.79.19.147 on 04/29/15 from IP address 36.79.19.147. Copyright ARRS. For personal use only; all rights reserved
the previously reported radiographic and CT
Disseminated nodules 6 4 3 1 0
findings of infant and childhood primary pul-
Mediastinal bulging 18 16 14 5 2
monary tuberculosis compared with our results.
Newly appeared calcification 4 3 Early diagnosis and prompt treatment, con-
Fibrosis and decreased lung volume 3 3 sidering their duration of symptoms (< 1
NoteData are numbers of patients. week), was possible in only four patients in our
study: three patients who showed definite me-
diastinal bulging on initial chest radiographs
sis for pediatric patients because miliary nod- childhood tuberculosis (bronchial narrow- and had a positive Mantoux test, and one pa-
ules are defined as tiny nodules less than 2 mm ing in 37% [13] and 29% [27]). CT scans de- tient who showed miliary dissemination of tu-
in diameter, uniform in size, and widespread in tect airway complications better than chest berculosis at chest radiography and had a his-
distribution [33]. On CT scans in our study, radiographs [34]. In seven of 11 patients tory of recent contact with active tuberculosis.
disseminated nodules were seen in 29% of the with bronchial narrowing, we observed Radiographic regression of primary pulmo-
patients. Nodules were larger (> 2 mm) than bronchial narrowing distal to the lobar bron- nary tuberculosis is a slow process. In our
usual miliary nodules and coalesced with each chus on CT scans that was not seen on the study, complete resolution of the consolidation
other in three of five patients. chest radiographs. occurred after a maximum of 6 months of treat-
Infant airways are smaller and more eas- Pleural effusion in primary tuberculosis re- ment, and improvement of the air-space consol-
ily compressed by enlarged hilar lymph sults from pleural infection via direct exten- idation preceded regression of enlarged nodes.
nodes [8, 11, 34]. In our study, bronchial sionrupture of a subpleural lesion into the Follow-up radiography after antituberculous
narrowing was seen in 65% and hyperinfla- pleural space or spread from caseous lymphad- medication may be performed to be sure that no
tion of lung parenchyma was seen in 47% of enopathy or an adjacent spinal lesion [35]. Pleu- progression or complications have occurred. It
patients on CT scans. These airway compli- ral effusion is not a common feature of primary is not always necessary to achieve normal chest
cations were more common than those of pulmonary tuberculosis in young children, and radiography to discontinue treatment [20, 36].
TABLE 3: Comparison of Radiographic and CT Features of Pulmonary Tuberculosis in Infancy and Childhood:
Literature Review
Schaaf et al. Andronikou et al. Delacourt Leung et al. Bosch-Marcet et al. Uzum et al.
Our Study [8] [27] et al. [14] [20] [15] Kim et al. [13] [12]
Radiologic Studies (n = 25) (n = 29) (n = 100) (n = 15) (n = 191) (n = 32) (n = 41) (n = 48)
Mean age 5.9 mo 65 d 21.5 mo 2y 5.9 y 6y 6y 7.9 y
Radiography
Mediastinal LN 72 89 0 92 63
Consolidation 80 71 0 70
Disseminated nodules 24 26 0
Airway compression 16 41 0
CT
Mediastinal LN 100 92 60 84a 83 73
Ring enhancement 100 67 85
Consolidation 100 49 19b
Masslike consolidation 59 15
Low attenuation 41 25
Cavities 29
Bronchogenic nodules 41 29
Disseminated nodules 29 17
Bronchial narrowing 65 29 37
NoteNumbers in rows under Radiography and CT are all percentages. Cells left blank indicate incidence for this item was not mentioned in the study. LN = lymph node.
a Mediastinal lymph node detected on sonography.
b Parenchymal lesion including consolidation and atelectasis.
1032 AJR:187, October 2006
Radiography and CT of Pulmonary Tuberculosis in Infants
In summary, frequent radiologic findings of 10. Shingadia D, Novelli V. Diagnosis and treatment of manifestations of pulmonary tuberculosis. Radiol
pulmonary tuberculosis of infants are mediastinal tuberculosis in children. Lancet Infect Dis 2003; Clin North Am 1995; 33:655678
or hilar lymphadenopathy with central necrosis 3:624632 23. Marais BJ, Gie RP, Schaaf HS, et al. A proposed ra-
and air-space consolidations, especially masslike 11. Agrons GA, WMarkowitz RI, Kramer SS. Pulmo- diological classification of childhood intra-thoracic
consolidations with low-attenuation areas or cav- nary tuberculosis in children. Semin Roentgenol tuberculosis. Pediatr Radiol 2004; 34:886894
ities within consolidations. Disseminated pulmo- 1993; 28:158172 24. Lamont AC, Cremin BJ, Pelteret RM. Radiological
Downloaded from www.ajronline.org by 36.79.19.147 on 04/29/15 from IP address 36.79.19.147. Copyright ARRS. For personal use only; all rights reserved
nary nodules and airway complications are also 12. Uzum K, Karahan OI, Dogan S, Coskun A, Topcu F. patterns of pulmonary tuberculosis in the paedia-
frequently detected in this age group. CT can be Chest radiography and thoracic computed tomog- tiric age group. Pediatr Radiol 1986; 16:27
a useful diagnostic technique for infant tubercu- raphy findings in children who have family mem- 25. Lorriman G, Bentley FJ. The incidence of segmen-
losis, as it can show parenchymal lesions and tu- bers with active pulmonary tuberculosis. Eur J Ra- tal lesions in primary tuberculosis in childhood. Am
berculous lymphadenopathy better than chest ra- diol 2003; 48:258262 Rev Tuberc 1959; 79:756763
diography. CT scans can also be helpful when 13. Kim WS, Moon WK, Kim IO, et al. Pulmonary tu- 26. Morrison JB. Natural history of segmental lesions
chest radiographs are inconclusive or complica- berculosis in children: evaluation with CT. AJR in primary pulmonary tuberculosis. Arch Dis Child
tions of tuberculosis are suspected. 1997; 168:10051009 1973; 48:9098
14. Delacourt C, Mani TM, Bonnerot V, et al. Com- 27. Andronikou S, Joseph E, Lucas S, et al. CT scanning
puted tomography with normal chest radiograph for the detection of tuberculous mediastinal and hi-
References in tuberculous infection. Arch Dis Child 1993; lar lymphadenopathy in children. Pediatr Radiol
1. Schneider E, Castro KG. Tuberculosis trends in the 69:430432 2004; 34:232236
United States, 19922001. Tuberculosis (Edinb) 15. Bosch-Marcet J, Serres-Creixams X, Zuasnabar- 28. Im JG, Song KS, Kang HS, et al. Mediastinal tuber-
2003; 83:2129 Cotro A, Codina-Puig X, Catala-Puigbo M, Simon- culous lymphadenitis: CT manifestations. Radiol-
2. Buckner CB, Leithiser RE, Walker CW, Allison Riazuelo JL. Comparison of ultrasound with plain ogy 1987; 164:115119
JW. The changing epidemiology of tuberculosis radiography and CT for the detection of mediastinal 29. Shewchuk JR, Reed MH. Pediatric postprimary
and other mycobacterial infections in the United lymphadenopathy in children with tuberculosis. Pe- pulmonary tuberculosis. Pediatr Radiol 2002;
States: implications for the radiologists. AJR diatr Radiol 2004; 34:895900 32:648651
1991; 156:255264 16. Kim KI, Lee JW, Park JH, et al. Pulmonary tuber- 30. Matsaniotis N, Kattamis C, Economou-Mavrou C,
3. FitzGerald JM, Grzybowski S, Allen EA. The im- culosis in five young infants with nursery exposure: Kyriazakou M. Bullous emphysema in childhood
pact of human immunodeficiency virus infection clinical, radiographic and CT findings. Pediatr Ra- tuberculosis. J Pediatr 1967; 71:703707
on tuberculosis and its control. Chest 1991; diol 1998; 28:836840 31. Harris VJ, Schauf V, Duda F, White H. Fatal tu-
100:191200 17. Jamieson DH, Cremin BJ. High resolution CT of the berculosis in young children. Pediatrics 1979;
4. Cremin BJ. Tuberculosis: the resurgence of our lungs in acute disseminated tuberculosis and a pe- 63:912914
most lethal infectious diseasea review. Pediatr diatric radiology perspective of the term miliary. 32. Im JG, Itoh H, Shim YS, et al. Pulmonary tubercu-
Radiol 1995; 25:620626 Pediatr Radiol 1993; 23:380383 losis: CT findingsearly active disease and se-
5. Burroughs M, Beitel A, Kawamura A, et al. Clinical 18. Oh YW, Kim YH, Lee NJ, et al. High-resolution CT quential changes with antituberculous therapy. Ra-
presentation of tuberculosis in culture-positive chil- appearance of miliary tuberculosis. J Comput Assist diology 1993; 186:653660
dren. Pediatr Infect Dis J 1999; 18:440446 Tomogr 1994; 18:862886 33. Tuddenham WJ. Glossary of terms of thoracic ra-
6. Stark JR, Jacobs RF, Jereb J. Resurgence of tuber- 19. Van Hest R, De Vries G, Morbano G, Pijnenburg M, diology: recommendations of the Nomenclature
culosis in children. J Pediatr 1992; 120:839855 Hartwig N, Baars H. Cavitating tuberculosis in an Committee of the Fleischner Society. AJR 1984;
7. Amodio J, Abramson S, Berdon W. Primary pul- infant: case report and literature review. Pediatr In- 143:509517
monary tuberculosis in infancy: a resurgent disease fect Dis J 2004; 23:667670 34. Choe KO, Jeong HJ, Sohn HY. Tuberculous bron-
in the urban United States. Pediatr Radiol 1986; 20. Leung AN, Mller NL, Pineda PR, FitzGerald JM. chial stenosis: CT findings in 28 cases. AJR 1990;
16:185189 Primary tuberculosis in childhood: radiographic 155:971976
8. Schaaf HS, Gie RP, Beyers N, Smuts N, Donald PR. manifestations. Radiology 1992; 182:8791 35. Hulnick DH, Naidich DP, McCauley DI. Pleural tu-
Tuberculosis in infants less than 3 months of age. 21. Effmann EL. Pulmonary infection. In: Kuhn JP, berculosis evaluated by computed tomography. Ra-
Arch Dis Child 1993; 69:371374 Slovis TL, Haller JO, eds. Caffeys pediatric diag- diology 1983; 149:759765
9. Vallejo JG, Ong LT, Starke JR. Clinical features, di- nostic imaging, 10th ed. Philadelphia, PA: Mosby, 36. Correa AG. Unique aspects of tuberculosis in the
agnosis, and treatment of tuberculosis in infants. Pe- 2004:9821039 pediatric population. Clin Chest Med 1997;
diatrics 1994; 94:17 22. McAdams HP, Erasmus J, Winter JA. Radiologic 18:8998
AJR:187, October 2006 1033
You might also like
- Respiratory Diseases of NewbornDocument93 pagesRespiratory Diseases of NewbornTheva Thy100% (1)
- Pulmonary Embolism in Children: Paul G. Thacker Edward Y. LeeDocument11 pagesPulmonary Embolism in Children: Paul G. Thacker Edward Y. LeeYuriansyah Dwi Rahma PutraNo ratings yet
- CT Scan PDFDocument12 pagesCT Scan PDFBunga alaraafNo ratings yet
- Intracranial Tuberculoma 5Document1 pageIntracranial Tuberculoma 5Arief RahmatullahNo ratings yet
- Role of CT in diagnosing neonatal pneumoniaDocument1 pageRole of CT in diagnosing neonatal pneumoniaCatalin PelinNo ratings yet
- CHEST RADIOGRAPHIC FINDINGS IN PULMONARY TUBERCULOSIS AND PNEUMONIA"The title is less than 40 characters long and starts with "TITLEDocument42 pagesCHEST RADIOGRAPHIC FINDINGS IN PULMONARY TUBERCULOSIS AND PNEUMONIA"The title is less than 40 characters long and starts with "TITLEnurza yeyeniNo ratings yet
- Journal Reading: TuberculosisDocument44 pagesJournal Reading: Tuberculosisnurza yeyeniNo ratings yet
- Jurnal Radio Inggris TalDocument17 pagesJurnal Radio Inggris TalimamattamamiNo ratings yet
- Pneumoniain Normaland Immunocompromised Children:Anoverview AndupdateDocument26 pagesPneumoniain Normaland Immunocompromised Children:Anoverview AndupdateEka KurniatiNo ratings yet
- Neonatal Lung Disorders: Pattern Recognition Approach To DiagnosisDocument12 pagesNeonatal Lung Disorders: Pattern Recognition Approach To DiagnosisMeiriyani LembangNo ratings yet
- TBC en NiñosDocument3 pagesTBC en NiñosDionela SotoNo ratings yet
- Interstitiallungdiseases Inchildren, Adolescents, AndyoungadultsDocument16 pagesInterstitiallungdiseases Inchildren, Adolescents, Andyoungadultsgustavo adolfo rodriguez alzateNo ratings yet
- Large Pulmonary Solitary Mass Caused by Mycobacterium Tuberculosis Mimicking A Malignant Tumor in A ChildDocument4 pagesLarge Pulmonary Solitary Mass Caused by Mycobacterium Tuberculosis Mimicking A Malignant Tumor in A Childadipspain981No ratings yet
- Pediatric Chest Disorders Practical Imaging Approach To DiagnosisDocument19 pagesPediatric Chest Disorders Practical Imaging Approach To DiagnosisANTOLINO GENARO ROSALES PIJONo ratings yet
- Delayed Isolation of Active Pulmonary Tuberculosis in Hospitalized Patients: A Pivotal Role of Radiologic EvaluationDocument12 pagesDelayed Isolation of Active Pulmonary Tuberculosis in Hospitalized Patients: A Pivotal Role of Radiologic EvaluationRidhya SilmiNo ratings yet
- The Role of High-Resolution Chest CT in The Diagnosis of Neuroendocrine Cell Hyperplasia of Infancy - A Rare Form of Pediatric Interstitial Lung DiseaseDocument3 pagesThe Role of High-Resolution Chest CT in The Diagnosis of Neuroendocrine Cell Hyperplasia of Infancy - A Rare Form of Pediatric Interstitial Lung DiseaseWalid AissaNo ratings yet
- Guideline Chronic Rhinosinusitis in Children 2019Document7 pagesGuideline Chronic Rhinosinusitis in Children 2019sjhfksglakdjalfsfNo ratings yet
- KJR 11 612Document6 pagesKJR 11 612gitaqNo ratings yet
- Jurnal Radio 1Document11 pagesJurnal Radio 1NadanNadhifahNo ratings yet
- HIstoria NaturalDocument4 pagesHIstoria NaturalEli PeñafielNo ratings yet
- Imaging Features of Extrapulmonary Tuberculosis in ChildrenDocument9 pagesImaging Features of Extrapulmonary Tuberculosis in Childrengiant nitaNo ratings yet
- Coexisting Lung Cysts in Neonate Pose Management ChallengeDocument4 pagesCoexisting Lung Cysts in Neonate Pose Management Challengenesrine ninaNo ratings yet
- Colletti 2013Document7 pagesColletti 2013Dara Dasawulansari SyamsuriNo ratings yet
- Abjas TUR 1Document9 pagesAbjas TUR 1Jojo LastNo ratings yet
- Section II - Chest Radiology: Figure 1ADocument35 pagesSection II - Chest Radiology: Figure 1AHaluk Alibazoglu100% (1)
- Primaey Neolplasm of The LungDocument8 pagesPrimaey Neolplasm of The Lungsamuel kefyalewNo ratings yet
- Journal ReadingDocument17 pagesJournal ReadingintanrhamaNo ratings yet
- ORENSTEIN 2002_Cystic fibrosis- A 2002 updateDocument9 pagesORENSTEIN 2002_Cystic fibrosis- A 2002 updateRafael JustinoNo ratings yet
- Ajr 17 18384Document10 pagesAjr 17 18384storyofmylife600No ratings yet
- Paediatric Respiratory Reviews: Tanyia Pillay, Savvas Andronikou, Heather J. ZarDocument8 pagesPaediatric Respiratory Reviews: Tanyia Pillay, Savvas Andronikou, Heather J. ZarSatria Bayu PratamaNo ratings yet
- Extrapulmonary Involvement in Pediatric TuberculosisDocument11 pagesExtrapulmonary Involvement in Pediatric TuberculosisFlavia Angelina SatopohNo ratings yet
- Jaffe 2008Document7 pagesJaffe 2008Diego AndradeNo ratings yet
- Ijri 25 213Document13 pagesIjri 25 213rodtobingNo ratings yet
- ajr.153.4.727Document4 pagesajr.153.4.727Andi WarlyNo ratings yet
- 247 2017 Article 3868 PDFDocument12 pages247 2017 Article 3868 PDFAndreas NatanNo ratings yet
- Pneumoperitoneum or Chilaiditi's SignDocument3 pagesPneumoperitoneum or Chilaiditi's SignMusdalifah ThahirNo ratings yet
- Pneumonia 6Document7 pagesPneumonia 6Anis BonitaNo ratings yet
- Linical Eat Res Pri Ar L NG Cancer Presenting As P L Nar Cnsliatin Iicingpne NiaDocument5 pagesLinical Eat Res Pri Ar L NG Cancer Presenting As P L Nar Cnsliatin Iicingpne NiaYusi RizkyNo ratings yet
- Histopathologic Analysis of Ct-Guided Core Needle Biopsy in Radiologically Detected Suspicious Mediastinal and Lung Mass: Two Years' Study in Tertiary HospitalDocument4 pagesHistopathologic Analysis of Ct-Guided Core Needle Biopsy in Radiologically Detected Suspicious Mediastinal and Lung Mass: Two Years' Study in Tertiary HospitalDesiree MejicaNo ratings yet
- Tonsil TumorDocument4 pagesTonsil TumorafrisiammyNo ratings yet
- Inadvertent Chest Tube Insertion in Congential Cystic Adenomatoid Malformation and Congential Lobar Emphysema Highlighting An Important ProblemDocument0 pagesInadvertent Chest Tube Insertion in Congential Cystic Adenomatoid Malformation and Congential Lobar Emphysema Highlighting An Important ProblemWenny EudensiaNo ratings yet
- Basic Concepts On Communityacquired Bacterial Pneumonia in PediatricsDocument6 pagesBasic Concepts On Communityacquired Bacterial Pneumonia in PediatricsJesselle LasernaNo ratings yet
- Diagnostic Rule for Tuberculous MeningitisDocument4 pagesDiagnostic Rule for Tuberculous MeningitisAri WirantariNo ratings yet
- Organising PneumoniaDocument12 pagesOrganising PneumoniaA. RaufNo ratings yet
- Accepted Manuscript: 10.1016/j.cpem.2018.02.009Document41 pagesAccepted Manuscript: 10.1016/j.cpem.2018.02.009Richo WijayaNo ratings yet
- Jurnal BedahDocument3 pagesJurnal BedahAb Hakim MuslimNo ratings yet
- Recurrent Pneumonia Caused by Rare Granular Cell TumorDocument7 pagesRecurrent Pneumonia Caused by Rare Granular Cell TumorJoshua MendozaNo ratings yet
- 5 FullDocument2 pages5 FullrahelNo ratings yet
- Respiratory Distress in Term Babies, Can We Predict The Outcome?Document5 pagesRespiratory Distress in Term Babies, Can We Predict The Outcome?Dr. Nimesha GamhewageNo ratings yet
- Imaging Pulmonary Infection: Classic Signs and PatternsDocument15 pagesImaging Pulmonary Infection: Classic Signs and PatternsChrist'na De RedArmyNo ratings yet
- Multiple Cavitary Lung Lesions in An Adolescent - Case Report of A Rare Presentation of Nodular Lymphocyte Predominant Hodgkin LymphomaDocument4 pagesMultiple Cavitary Lung Lesions in An Adolescent - Case Report of A Rare Presentation of Nodular Lymphocyte Predominant Hodgkin LymphomaManisha UppalNo ratings yet
- Pulmonary Interstitial Emphysema Presenting As A Congenital Cystic Adenomatous Malformation On CTDocument3 pagesPulmonary Interstitial Emphysema Presenting As A Congenital Cystic Adenomatous Malformation On CTRonald SanchezNo ratings yet
- Imaging Pulmonary Infection: Classic Signs and PatternsDocument14 pagesImaging Pulmonary Infection: Classic Signs and PatternsSanti ParambangNo ratings yet
- Simplified Cell Culture Method For The Diagnosis ofDocument5 pagesSimplified Cell Culture Method For The Diagnosis ofMarcellaNo ratings yet
- Diagnosis and Management of Cystic Fibrosis: Rosalind L SmythDocument6 pagesDiagnosis and Management of Cystic Fibrosis: Rosalind L SmythMuhammadShahzadNo ratings yet
- A Case of Pulmonary Tuberculosis With Multiple Nodules Mimicking Lung MetastasesDocument4 pagesA Case of Pulmonary Tuberculosis With Multiple Nodules Mimicking Lung MetastasesKusuma IntanNo ratings yet
- Jurnal Olla 2Document2 pagesJurnal Olla 2Ola AzzahraNo ratings yet
- Lung Adenocarcinoma With Solitary MetastDocument88 pagesLung Adenocarcinoma With Solitary MetastMikmik bay BayNo ratings yet
- Pleuropulmonary BlastomaDocument8 pagesPleuropulmonary BlastomaAdriana RuizNo ratings yet
- Indian J Radiol Imaging Word 1Document14 pagesIndian J Radiol Imaging Word 1Adie BrianNo ratings yet
- Thoracic Endoscopy: Advances in Interventional PulmonologyFrom EverandThoracic Endoscopy: Advances in Interventional PulmonologyMichael J. SimoffNo ratings yet
- Imaging in The Jaundiced Child PDFDocument14 pagesImaging in The Jaundiced Child PDFRahma Puji LestariNo ratings yet
- Jurnal DinaDocument11 pagesJurnal DinaRahma Puji LestariNo ratings yet
- Caesarean Section Delivery and The Risk of Allergic Disorders in ChildhoodDocument7 pagesCaesarean Section Delivery and The Risk of Allergic Disorders in ChildhoodRahma Puji LestariNo ratings yet
- Wa0001Document4 pagesWa0001Rahma Puji LestariNo ratings yet
- SGGS SGDO - PutuberbagiDocument1 pageSGGS SGDO - PutuberbagiRahma Puji LestariNo ratings yet
- HGHHLKHLKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKDocument1 pageHGHHLKHLKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKKRahma Puji LestariNo ratings yet
- T TTTTT TTTTT TTTTT TTTTT TTTTTDocument1 pageT TTTTT TTTTT TTTTT TTTTT TTTTTRahma Puji LestariNo ratings yet
- GGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGDocument1 pageGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGRahma Puji LestariNo ratings yet
- CarbohydrateDocument10 pagesCarbohydrateRahma Puji LestariNo ratings yet
- Marginal Zone Lymphomas: Subtypes: MALT (Extranodal), Nodal, SplenicDocument2 pagesMarginal Zone Lymphomas: Subtypes: MALT (Extranodal), Nodal, SplenicwwxxmmNo ratings yet
- AHA Vs ERC GuidelinesDocument39 pagesAHA Vs ERC GuidelinesYoel Harianto100% (2)
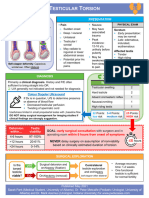
- Testicular Torsion, Peds Cases NotesDocument1 pageTesticular Torsion, Peds Cases NotesdzalhcNo ratings yet
- BAD Cryotherapy Update March 2018 - Lay Review March 2018Document4 pagesBAD Cryotherapy Update March 2018 - Lay Review March 2018Mehret TechaneNo ratings yet
- Horner Syndrome: DescriptionDocument3 pagesHorner Syndrome: DescriptionMeike WinataNo ratings yet
- A Laser Peripheral Iridotomy Would Most Likely Relieve AngleDocument2 pagesA Laser Peripheral Iridotomy Would Most Likely Relieve AngleGlaucoma UnhasNo ratings yet
- Leukemias Nursing ManagementDocument20 pagesLeukemias Nursing ManagementAnusha Verghese100% (5)
- Acute Respiratory Failure For StudentDocument41 pagesAcute Respiratory Failure For Studentapi-379952350% (4)
- Psychiatrics McqsDocument20 pagesPsychiatrics McqsHirwaNo ratings yet
- MECONIUM Aspiration SyndromeDocument37 pagesMECONIUM Aspiration SyndromekamalaNo ratings yet
- Neuroanatomical Changes After Eye Movement Desensitization and Reprocessing (EMDR) Treatment in Posttraumatic Stress DisorderDocument2 pagesNeuroanatomical Changes After Eye Movement Desensitization and Reprocessing (EMDR) Treatment in Posttraumatic Stress DisorderClaudio PeñafielNo ratings yet
- Multiple Organ Failure As A Cause of DeaDocument6 pagesMultiple Organ Failure As A Cause of DeaEliza DiaconescuNo ratings yet
- Acne (Causes and Symptoms)Document4 pagesAcne (Causes and Symptoms)Siddharth ChoudheryNo ratings yet
- Gastroenterology - Lower GI Bleeding - SOAP Note - Maitreyi RamanDocument4 pagesGastroenterology - Lower GI Bleeding - SOAP Note - Maitreyi RamanFrancieudo Sampaio100% (1)
- VAERS Report Details Deaths and Adverse Events Following COVID VaccinesDocument234 pagesVAERS Report Details Deaths and Adverse Events Following COVID VaccinesbeneNo ratings yet
- Emerging Re-Emerging Infectious Disease 2022Document57 pagesEmerging Re-Emerging Infectious Disease 2022marioNo ratings yet
- Actea SpicataDocument4 pagesActea SpicataRaveendra MungaraNo ratings yet
- Lash Lift Waiver and File SheetDocument2 pagesLash Lift Waiver and File SheettiffyoloNo ratings yet
- Factors Influencincing Discharge Against Medical Advice Among Paediatric Patients in Abakaliki, Southeastern NigeriaDocument3 pagesFactors Influencincing Discharge Against Medical Advice Among Paediatric Patients in Abakaliki, Southeastern NigeriaMorayo TimothyNo ratings yet
- HemorrhoidectomyDocument5 pagesHemorrhoidectomydrnareshkumar3281100% (1)
- HAAD Exam For Nurses Questions 2018Document46 pagesHAAD Exam For Nurses Questions 2018Asif Newaz100% (6)
- Pediatric Tuberculosis: Causes, Symptoms and TreatmentDocument112 pagesPediatric Tuberculosis: Causes, Symptoms and TreatmentFenny RahmadaniNo ratings yet
- Journal Club: DR Meera Nandan 3 Year MD ClinicalyogaDocument54 pagesJournal Club: DR Meera Nandan 3 Year MD ClinicalyogaMeera NandanNo ratings yet
- Essay 5Document13 pagesEssay 5api-549025764No ratings yet
- Acute Kidney Injury in Pregnancy and The Use of Non-Steroidal Anti-In Ammatory Drugs PDFDocument9 pagesAcute Kidney Injury in Pregnancy and The Use of Non-Steroidal Anti-In Ammatory Drugs PDFSai Khin Aung TintNo ratings yet
- Soft Tissue InjuryDocument72 pagesSoft Tissue InjuryCucu Ne Eyang Kakung75% (8)
- About This Leaflet: FibroadenomaDocument2 pagesAbout This Leaflet: FibroadenomaEnvhy WinaNo ratings yet
- Sept 4, 2015Document8 pagesSept 4, 2015Deity CelleNo ratings yet
- Celluar and Neural Regulation StudentDocument52 pagesCelluar and Neural Regulation StudentCruz YrNo ratings yet