Professional Documents
Culture Documents
Akupuntur PDF
Uploaded by
jayanti indrayaniOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Akupuntur PDF
Uploaded by
jayanti indrayaniCopyright:
Available Formats
Observation
Effects of acupuncture on
preeclampsia in Chinese women:
Editors choice
Scan to access more
free content a pilot prospective cohort study
Yingchun Zeng,1 Bing Liu,1 Taizhen Luo,1 Yun Chen,1 Guangen Chen,2
Dunjin Chen1
1
Department of Obstetrics, ABSTRACT function, renal impairment, pulmonary
The Third Affiliated Hospital of Objective To investigate the acceptability and oedema or new-onset cerebral or visual
Guangzhou Medical University,
Guangzhou, China feasibility of acupuncture treatment as an disturbances.1 It remains a leading cause
2
Department of Rehabilitation adjunct to usual care in Chinese women with of maternal and perinatal mortality and
Sciences, The Third Affiliated preeclampsia. morbidity, and complicates 28% of all
Hospital of Guangzhou Medical
University, Guangzhou, China
Methods This was a pilot prospective cohort pregnancies.2 3 In China, the prevalence
study. Pregnant women with a diagnosis of of preeclampsia is approximately 5%.4
Correspondence to preeclampsia were offered acupuncture and The global incidence of preeclampsia
Research Associate Professor, allocated into groups based on their choice: the appears to be increasing, most likely due
Yingchun Zeng, Department of
Obstetrics and Gynecology, The acupuncture group (n=11) comprised women to advancing maternal age, the higher
Third Affiliated Hospital of electing to receive treatment (up to 10 sessions prevalence of obesity and medical
Guangzhou Medical University, over 2 weeks). The control group (n=11) was comorbidities, and the use of assisted
No 63 DuoBao Road, Liwan made up of women who declined and was reproductive techniques.4 Women with
District, Guangzhou, Guangdong
Province 510150, China; matched for age, gestation at diagnosis, and preeclampsia are at risk of various
chloezengyc@hotmail.co.uk parity. All women received usual care and complications including eclampsia,
underwent measurement of blood pressure (BP) renal failure, placental abruption, and
Accepted 7 October 2015
Published Online First
at four time points: at baseline, at the end of the preterm birth in the peripartum period.5
29 October 2015 intervention, immediately before delivery, and Furthermore, following the pregnancy,
postpartum (within 24 h). they have an increased risk of cardiovas-
Results Patients in the acupuncture group had cular disease throughout their lives.6
significantly lower BP at time of delivery, and Approximately one-half of patients with
postpartum, than patients in the control group high blood pressure (BP) outside of preg-
( p<0.05). The individual change in BP between nancy are non-compliant with drug
baseline and the end of treatment was therapy for various reasons, including
significantly greater in the acupuncture group adverse effects and complications.7
versus the control group for both systolic BP During pregnancy, in particular, several
(median (IQR) 8 (3 to 14) vs +1 (7 to +9) antihypertensive agents can have signifi-
mm Hg, p=0.007) and diastolic BP (3 (1 to cant side effects. For example, the use of
3) vs +2 (2 to +7) mm Hg, p=0.013). There -blockers is associated with fetal growth
were no significant differences between the restriction, and ACE inhibitors such as
groups in perinatal outcomes and no adverse captopril can cause fetal renal impairment
effects of treatment. and reduce placental perfusion.8 For this
Conclusions Acupuncture plus usual care was reason, there has been a growing interest
associated with a greater reduction in BP than in alternative therapies such as acupunc-
usual care alone. Further studies are needed to ture for the treatment of preeclampsia.
clarify the role of acupuncture in the treatment In China, acupuncture has been used to
of preeclampsia. treat disease for more than 2500 years.9
There is an increasing body of evidence
INTRODUCTION supporting the effectiveness of acupunc-
Preeclampsia is a specific disorder of ture in the treatment of hypertension in
pregnancy, which is characterised by general.7 1012 However, to date there
To cite: Zeng Y, Liu B, Luo T, gestational hypertension together with have been only two observational studies
et al. Acupunct Med proteinuria or other stigmata, such as of acupuncture for treatment of hyper-
2016;34:144148. thrombocytopenia, impaired liver tension during pregnancy, both of which
144 Zeng Y, et al. Acupunct Med 2016;34:144148. doi:10.1136/acupmed-2015-010893
Observation
suggested that acupuncture was safe and effective but Acupuncture treatment
were conducted in women with pregnancy-induced The acupuncture group received manual acupuncture,
hypertension (PIH) without associated proteinuria or which was provided by a single acupuncturist trained
systemic features of preeclampsia.8 13 Moreover, both in Traditional Chinese Medicine. Sterile, disposable,
studies lacked a control group with which to draw any stainless steel needles (length 4 cm, diameter
comparisons. Accordingly, the aim of the present 0.25 mm, HuanQiu, China) were inserted at a com-
study was to investigate the acceptability and feasibil- bination of the following seven acupuncture points:
ity of acupuncture treatment in women with a formal GB20 (Fengchi), LR3 (Taichong), LI11 (Quchi), ST36
diagnosis of preeclampsia, and to examine its effects (Zusanli), LI4 (Hegu), SP6 (Sanyinjiao) and GV20
on the condition relative to a contemporaneous (Baihui), unilaterally or bilaterally, depending on each
control group of women not receiving acupuncture. womans traditional diagnosis (constitution) as deter-
mined by the acupuncturist. The total number of
points needled was 12 in all participants, the duration
METHODS of needling was 20 min, the frequency of treatment
Ethical approval and study procedure
was five times per week, and the total number of
This was a pilot prospective cohort study, undertaken treatments was intended to be 10 per patient. The
at the Third Affiliated Hospital of Guangzhou depth of needling varied between 25 and 40 mm
Medical University. The study was conducted in depending upon the individual point.
accordance with the Declaration of Helsinki code of Both groups received usual care, which included
ethics. Ethical approval was obtained from the ethics oral antihypertensives for BP control, diazepam for
review committee of the Third Affiliated Hospital sedation, and magnesium sulfate to reduce the risk of
of Guangzhou Medical University (reference no. seizures. When necessary, glyceryl trinitrate (nitrogly-
2014#028). All patients participated on a voluntary cerine) was used to keep BP below 160/100 mm Hg
basis and gave their written informed consent before to minimise the risk of intraventricular haemorrhage.
data collection. A research nurse was responsible for
recruiting subjects and for providing a full explanation
Outcome measures
of the study, while a dedicated acupuncturist per-
The primary outcomes were the changes in systolic BP
formed the interventions. A second nurse collected
(SBP) and diastolic BP (DBP), averaged over a 24 h
the outcome data and was deliberately kept blind as to
period, between baseline (T0) and completion of the
whether or not patients had been treated.
course of acupuncture treatment (T1). Secondary out-
comes included BP at the time of delivery (T2) and
Inclusion and exclusion criteria within 24 h of delivery (T3), gestational age at delivery,
Pregnant women with a diagnosis of preeclampsia birth weight, incidence of low birth weight (<2.5 kg),
(defined as new-onset hypertension after 20 weeks rate of admission to the neonatal intensive care unit
gestation with evidence of maternal liver, renal, (NICU), and rates of maternal or neonatal complica-
neurological or haematological abnormalitiespro- tions (to assess safety). In addition, all patients in the
teinuria)1 were invited to participate. Exclusion cri- intervention group were asked to rate their satisfaction
teria included multiple pregnancy, pre-existing with the acupuncture treatment by selecting one of the
hypertension and/or secondary causes of hypertension following options in response to the statement that acu-
(such as underlying renal disease) and PIH (defined as puncture was helpful for them: extremely agree,
new-onset hypertension without any additional fea- agree, disagree or extremely disagree.
tures of preeclampsia, as listed above). Between
January and mid-May 2015, a total of 47 women Data collection and analysis
with preeclampsia met the above inclusion criteria: 43 All data are presented as meanSD unless otherwise
were willing to participate and four declined. Women stated. SPSS V.20.0 was used for statistical analysis
who accepted the offer of acupuncture treatment (SPSS, IBM Corp, Armonk, New York, USA).
formed the intervention group (n=11). The contem- Categorical data were compared by the 2 test.
poraneous control group was selected from the 32 Continuous data were checked for normality of distri-
women who declined acupuncture (usually based on bution and analysed using the independent samples t
personal opinion or the advice of friends and/or test (to compare between study groups) and repeated
family) but otherwise met inclusion criteria and were measures analysis of variance followed by post-hoc
willing to contribute outcome data to the study. Bonferonni test (to compare BP between different
According to the pre-agreed study protocol, in order time points). All statistical tests were two-tailed, and
to achieve a 1:1 ratio in the intervention and com- p<0.05 was taken to indicate statistical significance.
parator groups, women were chosen based on age
(within 1 year), gestational age at diagnosis (within RESULTS
2 weeks), and parity in order to form the matched Table 1 shows the baseline data in the acupuncture
control group (n=11). and control groups (n=11 each). After selecting
Zeng Y, et al. Acupunct Med 2016;34:144148. doi:10.1136/acupmed-2015-010893 145
Observation
suggested that acupuncture was safe and effective but Acupuncture treatment
were conducted in women with pregnancy-induced The acupuncture group received manual acupuncture,
hypertension (PIH) without associated proteinuria or which was provided by a single acupuncturist trained
systemic features of preeclampsia.8 13 Moreover, both in Traditional Chinese Medicine. Sterile, disposable,
studies lacked a control group with which to draw any stainless steel needles (length 4 cm, diameter
comparisons. Accordingly, the aim of the present 0.25 mm, HuanQiu, China) were inserted at a com-
study was to investigate the acceptability and feasibil- bination of the following seven acupuncture points:
ity of acupuncture treatment in women with a formal GB20 (Fengchi), LR3 (Taichong), LI11 (Quchi), ST36
diagnosis of preeclampsia, and to examine its effects (Zusanli), LI4 (Hegu), SP6 (Sanyinjiao) and GV20
on the condition relative to a contemporaneous (Baihui), unilaterally or bilaterally, depending on each
control group of women not receiving acupuncture. womans traditional diagnosis (constitution) as deter-
mined by the acupuncturist. The total number of
points needled was 12 in all participants, the duration
METHODS of needling was 20 min, the frequency of treatment
Ethical approval and study procedure
was five times per week, and the total number of
This was a pilot prospective cohort study, undertaken treatments was intended to be 10 per patient. The
at the Third Affiliated Hospital of Guangzhou depth of needling varied between 25 and 40 mm
Medical University. The study was conducted in depending upon the individual point.
accordance with the Declaration of Helsinki code of Both groups received usual care, which included
ethics. Ethical approval was obtained from the ethics oral antihypertensives for BP control, diazepam for
review committee of the Third Affiliated Hospital sedation, and magnesium sulfate to reduce the risk of
of Guangzhou Medical University (reference no. seizures. When necessary, glyceryl trinitrate (nitrogly-
2014#028). All patients participated on a voluntary cerine) was used to keep BP below 160/100 mm Hg
basis and gave their written informed consent before to minimise the risk of intraventricular haemorrhage.
data collection. A research nurse was responsible for
recruiting subjects and for providing a full explanation
Outcome measures
of the study, while a dedicated acupuncturist per-
The primary outcomes were the changes in systolic BP
formed the interventions. A second nurse collected
(SBP) and diastolic BP (DBP), averaged over a 24 h
the outcome data and was deliberately kept blind as to
period, between baseline (T0) and completion of the
whether or not patients had been treated.
course of acupuncture treatment (T1). Secondary out-
comes included BP at the time of delivery (T2) and
Inclusion and exclusion criteria within 24 h of delivery (T3), gestational age at delivery,
Pregnant women with a diagnosis of preeclampsia birth weight, incidence of low birth weight (<2.5 kg),
(defined as new-onset hypertension after 20 weeks rate of admission to the neonatal intensive care unit
gestation with evidence of maternal liver, renal, (NICU), and rates of maternal or neonatal complica-
neurological or haematological abnormalitiespro- tions (to assess safety). In addition, all patients in the
teinuria)1 were invited to participate. Exclusion cri- intervention group were asked to rate their satisfaction
teria included multiple pregnancy, pre-existing with the acupuncture treatment by selecting one of the
hypertension and/or secondary causes of hypertension following options in response to the statement that acu-
(such as underlying renal disease) and PIH (defined as puncture was helpful for them: extremely agree,
new-onset hypertension without any additional fea- agree, disagree or extremely disagree.
tures of preeclampsia, as listed above). Between
January and mid-May 2015, a total of 47 women Data collection and analysis
with preeclampsia met the above inclusion criteria: 43 All data are presented as meanSD unless otherwise
were willing to participate and four declined. Women stated. SPSS V.20.0 was used for statistical analysis
who accepted the offer of acupuncture treatment (SPSS, IBM Corp, Armonk, New York, USA).
formed the intervention group (n=11). The contem- Categorical data were compared by the 2 test.
poraneous control group was selected from the 32 Continuous data were checked for normality of distri-
women who declined acupuncture (usually based on bution and analysed using the independent samples t
personal opinion or the advice of friends and/or test (to compare between study groups) and repeated
family) but otherwise met inclusion criteria and were measures analysis of variance followed by post-hoc
willing to contribute outcome data to the study. Bonferonni test (to compare BP between different
According to the pre-agreed study protocol, in order time points). All statistical tests were two-tailed, and
to achieve a 1:1 ratio in the intervention and com- p<0.05 was taken to indicate statistical significance.
parator groups, women were chosen based on age
(within 1 year), gestational age at diagnosis (within RESULTS
2 weeks), and parity in order to form the matched Table 1 shows the baseline data in the acupuncture
control group (n=11). and control groups (n=11 each). After selecting
Zeng Y, et al. Acupunct Med 2016;34:144148. doi:10.1136/acupmed-2015-010893 145
Observation
Table 1 Baseline data
Acupuncture Control group
Variables group (n=11) (n=11) p Value
Age (years) 31.9 (3.96) 32.7 (4.47) 0.65
Gestational age at 28.2 (3.74) 28.4 (3.69) 0.95
diagnosis (weeks)
(2134)
Gravidity (13) 0.75
1 9 (81.8) 8 (72.7)
2 1 (9.1) 2 (18.2)
3 1 (9.1) 1 (9.1)
Parity (01) 0.55
0 10 (90.9) 9 (81.8)
1 1 (9.1) 2 (18.2)
Systolic blood 152.6 (12.79) 152.5 (13.87) 0.975
pressure (mmHg)
Diastolic blood 99.9 (13.08) 99.7 (8.41) 0.969
pressure (mmHg)
Data are mean (SD) for continuous variables and number (%) for
categorical variables.
controls on the basis of maternal age (range 25
41 years), gestational age at diagnosis (range 21
34 week gestation) and parity, the two groups were
highly similar with respect to these four variables,
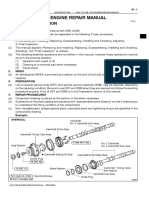
confirming balanced matching. Due to Chinas one Figure 1 Systolic and diastolic blood pressure measurements
child policy, most women were nulliparous. In add- at four time points in 22 women with preeclampsia receiving up
ition, there were no significant differences at baseline to 10 sessions of manual acupuncture plus usual care
(Acupuncture group, n=11) or usual care alone (Control group,
in gravidity or BP. Three of 11 patients did not com-
n=11). T0, baseline; T1, following completion of acupuncture
plete 10 sessions of acupuncture: one patient went treatment; T2, at time of delivery; T3, postpartum (within 24 h
into preterm labour secondary to placental abruption of delivery). *p<0.05.
and two patients were medically induced by their phy-
sicians as they were approaching term (37 weeks patient developed pulmonary oedema and another
gestation). experienced eclampsia, both in the control group.
Figure 1 shows the mean SBP and DBP at the four There were no other maternal complications. In terms
assessment time points by group: baseline (T0), at the of neonatal complications, one neonate was born with
end of the treatment period (T1), before delivery a traumatic injury to the urethra (very unlikely to be
(T2), and day 1 post-delivery (T3). The average 24 h related to acupuncture). The number of neonates
SBP and DBP before delivery and postpartum were admitted to NICU was equivalent between the two
significantly lower in the acupuncture group than in groups and was predominantly due to prematurity.
the control group ( p<0.05). Although mean SBP and No significant adverse effects were reported as a
DBP did not differ between groups immediately fol- result of the acupuncture treatments. Three patients in
lowing treatment, the primary outcome (individual the study group reported minor complaints: needle-
change in BP from baseline, ie, T0 to T1) was greater related bruising, needling pain, and spot bleeding,
in the acupuncture group versus the control group for respectively. One patient in the acupuncture group
both SBP (mean (IQR) 8 (3 to 14) vs +1 (7 to experienced placental abruption during the interven-
+9) mm Hg, p=0.007) and DBP (3 (1 to 3) vs tion period; however, notably, the incidence of placen-
+2 (2 to +7) mm Hg, p=0.013). In both groups, tal abruption in this group (one of 11) was identical
postpartum BP readings were significantly lower com- to that in the control group. With respect to patient
pared to time points T0, T1 and T2 ( p<0.001 satisfaction, six out of 11 patients who received acu-
0.032), reflecting the natural history of preeclampsia puncture reported that it was extremely helpful, four
(which resolves following delivery). reported that it was helpful, and only one reported
In terms of perinatal outcomes in the acupuncture that it did not help.
and control groups (table 2), there were no statistically
significant differences between the two groups for any DISCUSSION
parameter. With respect to maternal complications, This is the first pilot study to investigate the effects of
two women experienced placental abruption (one acupuncture treatment on preeclampsia. The results
each in the acupuncture and control groups). One showed that acupuncture reduced systolic and diastolic
146 Zeng Y, et al. Acupunct Med 2016;34:144148. doi:10.1136/acupmed-2015-010893
Observation
Table 2 Perinatal outcomes study was very small, which may have been com-
Acupuncture Control group
pounded by the fact that some pregnant women and
Variables group (n=11) (n=11) p Value their obstetricians hold conservative attitudes toward
applying acupuncture during pregnancy. Moreover,
Gestational age at 34.2 (2.82) 32.1 (3.83) 0.16
delivery (weeks) many acupuncturists fear the fact that certain acu-
(2638) puncture points (eg, SP6) can trigger uterine contrac-
Mode of delivery 0.59 tions in pregnant women,14 16 although there is no
Vaginal delivery 2 (18.2) 1 (9.1) scientific evidence that stimulating such acupuncture
Caesarean section 9 (81.8) 10 (90.9) points is harmful during pregnancy.16 17 A sham-
Maternal 0.26 controlled trial would be needed to control for the
complications non-specific effects of acupuncture treatment;
Yes 1 (9.1) 3 (27.3) however, this poses an ethical dilemma in view of the
No 10 (90.9) 8 (72.7) serious nature of preeclampsia and need for effective
Birth weight (g) 1517 (986) 1471 (1160) 0.11 treatment. Zaslawski18 argues that a trial comparing
Apgar score 0.59 acupuncture plus conventional care versus conven-
<7 1 (9.1) 2 (18.2) tional care alone is the most ethical option, because
7 10 (90.9) 9 (81.8) there is no attempt to prevent patients from receiving
Neonatal 0.30 conventional treatment. Ultimately, a randomised con-
complications trolled trial will be required to examine whether acu-
Yes 0 (0.0) 1 (9.1) puncture has positive effects on reducing BP in
No 11 (100) 10 (90.9) women with preeclampsia.
Admission to NICU 1.00 In conclusion, this pilot study shows that acupunc-
Yes 9 (81.8) 9 (81.8) ture appears effective at reducing BP in women with
No 2 (18.2) 2 (18.2) preeclampsia when used as an adjunct to standard
Data are mean (SD) for continuous variables and number (%) for care; however, this needs to be verified by further
categorical variables. research including a larger sample size and randomisa-
NICU, neonatal intensive care unit. tion. Future studies need to be sufficiently powered to
determine whether acupuncture, in addition to poten-
BP over the study period. After matching for subjects tially reducing BP, can improve perinatal outcomes for
baseline BP, age, gestational age at diagnosis and parity, women with preeclampsia and their babies, in order
there were no significant baseline differences between to guide clinical practice in the future.
the acupuncture and control groups, so imbalance of
any of these variables is unlikely to account for the Contributors YZ, BL and TL designed the study. YC collected
observed positive effects of acupuncture on BP in the data. GC provided the acupuncture. DC diagnosed
participants and supervised the reseach project. YZ drafted the
women with preeclampsia. However, the lack of any manuscript. All authors approved the final version of the
randomisation means that the possibility of residual manuscript.
confounding cannot be completely ruled out. Funding This research was supported by Guangzhou Municipal
In the present study, there were no statistically signifi- Bureau of Traditional Chinese Medicine (20152A011020), and
cant effects of acupuncture on perinatal outcomes, Traditional Chinese Medicine Bureau of Guangdong Province
(20141179).
which is likely to reflect the small number of patients
Competing interests None declared.
included. Previous retrospective clinical observations
Patient consent Obtained.
have also indicated that acupuncture can help treat
PIH, thereby improving perinatal outcomes.8 13 Ethics approval The Third Affiliated Hospital of Guangzhou
Medical University.
Although it has been reported anecdotally that acu-
Provenance and peer review Not commissioned; externally
puncture treatments can be dangerous during preg- peer reviewed.
nancy,14 this study did not find any significant adverse
effects during the entire study period. In this pilot
study, there were only minor adverse effects, including REFERENCES
needle pain and spot bleeding. This study finding was 1 American Congress of Obstetricians and Gynecologists. New
congruent with previous observations that acupuncture guidelines in preeclampsia diagnosis and care include revised
imposes no significant risks for pregnant women.15 16 definition of preeclampsia. http://www.acog.org/ (accessed 15
Jan 2015).
This pilot study has two main limitations. Firstly,
2 Steegers EAP, von Dadelszen P, Duvekot JJ, et al. Pre-eclampsia.
there was no sham acupuncture procedure provided in
Lancet 2010;376:63144.
the control group, so we are unable to exclude 3 Duley L. The global impact of pre-eclampsia and eclampsia.
placebo effects. As group assignment was based on Semin Perinatol 2009;33:1307.
patient cooperation, patients in the acupuncture group 4 Qiao C, Yang X, Lin Q. Advanced research in epidemiology of
may have received more attention, which may have preeclampsia. Chin J Fam Plann Gynecol Obstet 2013;5:58.
had a psychological effect. The sample size of this [in Chinese].
Zeng Y, et al. Acupunct Med 2016;34:144148. doi:10.1136/acupmed-2015-010893 147
You might also like
- Effects of Acupuncture On Preeclampsia in Chinese Women: A Pilot Prospective Cohort StudyDocument5 pagesEffects of Acupuncture On Preeclampsia in Chinese Women: A Pilot Prospective Cohort StudyJayanti IndrayaniNo ratings yet
- Preliminary Clinical Evaluation of Acupuncture Therapy in Patients With Postpartum SciaticaDocument7 pagesPreliminary Clinical Evaluation of Acupuncture Therapy in Patients With Postpartum SciaticasemnasNo ratings yet
- Influence of Acupuncture Stimulation On Pregnancy Rates For Women Undergoing Embryo TransferDocument7 pagesInfluence of Acupuncture Stimulation On Pregnancy Rates For Women Undergoing Embryo TransferFerry DimyatiNo ratings yet
- Jurnal Berpikir KritisDocument9 pagesJurnal Berpikir KritisNindita IllahiNo ratings yet
- Jurnal Berpikir KritisDocument9 pagesJurnal Berpikir KritisNindita IllahiNo ratings yet
- A case series of acupuncture treatment for female infertility with some cases 2014Document5 pagesA case series of acupuncture treatment for female infertility with some cases 2014juba0015No ratings yet
- Liu 2020Document6 pagesLiu 2020Vanessa CarinoNo ratings yet
- Chi Kun GunyaDocument1 pageChi Kun GunyayodhaarspinoNo ratings yet
- A 23-Year, Single-Center, Retrospective Analysis of 36 Cases of AcuteDocument4 pagesA 23-Year, Single-Center, Retrospective Analysis of 36 Cases of AcuteAleGrNo ratings yet
- Effect of Acupressure at P6 On Nausea and Vomiting - Ijerph-19-10886Document10 pagesEffect of Acupressure at P6 On Nausea and Vomiting - Ijerph-19-10886Widya Ingriani P WNo ratings yet
- Aborsi MengancamDocument11 pagesAborsi MengancamIntan PermataNo ratings yet
- Tran 2020Document8 pagesTran 2020whyme becauseNo ratings yet
- Wang 2009Document8 pagesWang 2009Graziele GuimarãesNo ratings yet
- Pathophysiology and Medical Management of Systemic Hypertension in PregnancyDocument11 pagesPathophysiology and Medical Management of Systemic Hypertension in Pregnancydr faathirNo ratings yet
- Paguidian, Griffin John D. Bsn4ADocument10 pagesPaguidian, Griffin John D. Bsn4AGj PaguidianNo ratings yet
- Post Partum Maternal Morbidities and TheDocument102 pagesPost Partum Maternal Morbidities and TheBagusHibridaNo ratings yet
- Apu Cunt UraDocument22 pagesApu Cunt UraAlekhine Cubas MarinaNo ratings yet
- Aderoba 2016Document8 pagesAderoba 2016DONNYNo ratings yet
- Deng 2012Document4 pagesDeng 2012Rachmad RasidinNo ratings yet
- A Cohort Study of The Impact of Epidural Analgesia On Maternal and Neonatal OutcomesDocument7 pagesA Cohort Study of The Impact of Epidural Analgesia On Maternal and Neonatal OutcomesHadad Setiawan FachrulNo ratings yet
- 10 1016@j Ejogrb 2015 09 020Document5 pages10 1016@j Ejogrb 2015 09 020samuel tapia pardoNo ratings yet
- Original Research Articles: Acute Pain SectionDocument8 pagesOriginal Research Articles: Acute Pain SectionFfNo ratings yet
- AkupunturDocument29 pagesAkupunturNoraNo ratings yet
- Pregnancy and Glomerular Disease: A Systematic Review of The Literature With Management GuidelinesDocument11 pagesPregnancy and Glomerular Disease: A Systematic Review of The Literature With Management GuidelinesmeliabudiNo ratings yet
- Embarazo EctópicoDocument7 pagesEmbarazo EctópicomariNo ratings yet
- International Journal of Cardiology: Stefano Raffaele Giannubilo, Stefano Cecchi, Elisa Tidu, Andrea CiavattiniDocument3 pagesInternational Journal of Cardiology: Stefano Raffaele Giannubilo, Stefano Cecchi, Elisa Tidu, Andrea CiavattiniFelipe Cortés VegaNo ratings yet
- Abdominal and Auricular Acupuncture For Blood PressureDocument7 pagesAbdominal and Auricular Acupuncture For Blood PressureitensorNo ratings yet
- 4891 GlobalWarmingImpactsDocument14 pages4891 GlobalWarmingImpactsEdilenaNo ratings yet
- Effectiveness of Acupuncture in The Treatment of Hyperemesis Gravidarum - A Systematic Review and Meta-AnalysisDocument14 pagesEffectiveness of Acupuncture in The Treatment of Hyperemesis Gravidarum - A Systematic Review and Meta-Analysiswiwit vitaniaNo ratings yet
- Continuous Compared With Cyclic Oral Contraceptives For The Treatment of Primary DysmenorrheaDocument9 pagesContinuous Compared With Cyclic Oral Contraceptives For The Treatment of Primary Dysmenorrheadokter wawanNo ratings yet
- Session 10 - Obstetrics: Hypertension Reference: A2346PG: Hypertensive Disorders in PregnancyDocument1 pageSession 10 - Obstetrics: Hypertension Reference: A2346PG: Hypertensive Disorders in PregnancyAAPRNo ratings yet
- Acupuncture Arivoum UmDocument2 pagesAcupuncture Arivoum UmYoga NaayakNo ratings yet
- Article 233230Document11 pagesArticle 233230arreyemilieneNo ratings yet
- Management of HypertensionDocument6 pagesManagement of HypertensionRioNo ratings yet
- DIABETES MELLITUS PregnancyDocument23 pagesDIABETES MELLITUS PregnancyAdinarayana KashyapNo ratings yet
- Contoh Skenario - TelaahDocument18 pagesContoh Skenario - TelaahnafiraNo ratings yet
- Women's Health Case: Methotrexate vs Laparoscopic SalpingostomyDocument9 pagesWomen's Health Case: Methotrexate vs Laparoscopic SalpingostomyWong Chui YeeNo ratings yet
- Acupuncture Review in Obstetrics and GynecologyDocument6 pagesAcupuncture Review in Obstetrics and GynecologyKeeranmayeeishraNo ratings yet
- Tugas Dokter Yulia Kelompok 2 EditDocument10 pagesTugas Dokter Yulia Kelompok 2 Editfk unpadNo ratings yet
- Safety of Acupuncture During Pregnancy: A Retrospective Cohort Study in KoreaDocument8 pagesSafety of Acupuncture During Pregnancy: A Retrospective Cohort Study in Koreaindra coolNo ratings yet
- Cancer de Endometrio Preserv Fer 2021Document15 pagesCancer de Endometrio Preserv Fer 2021Claudia Mugruza BedoyaNo ratings yet
- Acupuncture For Constipation in Patients With Stroke: Protocol of A Systematic Review and Meta-AnalysisDocument10 pagesAcupuncture For Constipation in Patients With Stroke: Protocol of A Systematic Review and Meta-AnalysisYUTRILIANo ratings yet
- Effectiveness of Per Rectal Misoprostol Versus Intramuscular Oxytocin For Prevention of Primary Postpartum HaemorrhageDocument5 pagesEffectiveness of Per Rectal Misoprostol Versus Intramuscular Oxytocin For Prevention of Primary Postpartum HaemorrhageFuad HasanNo ratings yet
- Walsh 2016Document8 pagesWalsh 2016Ambulatório Dieta Cetogênica HUBNo ratings yet
- Tofacitinib As Induction and Maintenance Therapy For Ulcerative ColitisDocument14 pagesTofacitinib As Induction and Maintenance Therapy For Ulcerative Colitismichal ben meronNo ratings yet
- ACUPUNTURA OBESIDAD TTODocument5 pagesACUPUNTURA OBESIDAD TTOCamiloNo ratings yet
- Pain Relief: Determining The Safety of Ibuprofen With Postpartum PreeclampsiaDocument2 pagesPain Relief: Determining The Safety of Ibuprofen With Postpartum PreeclampsiaAnonymous P5efHbeNo ratings yet
- PIH Renal Doppler Pregnancy - CutDocument4 pagesPIH Renal Doppler Pregnancy - CutAnonymous 9QxPDpNo ratings yet
- Supported By: None.: AbstractsDocument1 pageSupported By: None.: AbstractsFerry DimyatiNo ratings yet
- Acupuncture For Constipation in Patients With Stroke: Protocol of A Systematic Review and Meta-AnalysisDocument5 pagesAcupuncture For Constipation in Patients With Stroke: Protocol of A Systematic Review and Meta-AnalysisYUTRILIANo ratings yet
- Tui Na Pediatrico y DiarreaDocument33 pagesTui Na Pediatrico y DiarreaCristian Dionisio Barros OsorioNo ratings yet
- Imafuku 2019Document5 pagesImafuku 2019Rizki FebriyaniNo ratings yet
- Bai 2017Document4 pagesBai 2017kurnia fitriNo ratings yet
- Acute Pyelonephritis in PregnancyDocument7 pagesAcute Pyelonephritis in PregnancyKvmLlyNo ratings yet
- Podocyturia As A DiagnosticMarker For Preeclampsia 2012Document6 pagesPodocyturia As A DiagnosticMarker For Preeclampsia 2012Diapositivas08No ratings yet
- Suen Traditional Auriculotherapy HypertensionDocument6 pagesSuen Traditional Auriculotherapy Hypertensionruivanov70No ratings yet
- J of Clinical Hypertension - 2021 - Huai - Preventive Effect of Aspirin On Preeclampsia in High Risk Pregnant Women WithDocument8 pagesJ of Clinical Hypertension - 2021 - Huai - Preventive Effect of Aspirin On Preeclampsia in High Risk Pregnant Women WithkrisnawatiNo ratings yet
- TCM For Neck and LBPDocument37 pagesTCM For Neck and LBPpelizNo ratings yet
- Novasure Treatment For One Case of AUB With Active SLEDocument4 pagesNovasure Treatment For One Case of AUB With Active SLEferifhransNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 9: GynecologyFrom EverandComplementary and Alternative Medical Lab Testing Part 9: GynecologyNo ratings yet
- DLL - Science 6 - Q3 - W3Document6 pagesDLL - Science 6 - Q3 - W3AnatasukiNo ratings yet
- The Effects of Cabergoline Compared To Dienogest in Women With Symptomatic EndometriomaDocument6 pagesThe Effects of Cabergoline Compared To Dienogest in Women With Symptomatic EndometriomaAnna ReznorNo ratings yet
- Research Proposal by Efe Onomake Updated.Document18 pagesResearch Proposal by Efe Onomake Updated.efe westNo ratings yet
- Solidworks Inspection Data SheetDocument3 pagesSolidworks Inspection Data SheetTeguh Iman RamadhanNo ratings yet
- Housekeeping NC II ModuleDocument77 pagesHousekeeping NC II ModuleJoanne TolopiaNo ratings yet
- The Five Laws of Light - Suburban ArrowsDocument206 pagesThe Five Laws of Light - Suburban Arrowsjorge_calvo_20No ratings yet
- Organisation Study of KAMCODocument62 pagesOrganisation Study of KAMCORobin Thomas100% (11)
- CP ON PUD (1) ADocument20 pagesCP ON PUD (1) ADeekshitha DanthuluriNo ratings yet
- Cost Allocation Methods & Activity-Based Costing ExplainedDocument53 pagesCost Allocation Methods & Activity-Based Costing ExplainedNitish SharmaNo ratings yet
- Opportunity, Not Threat: Crypto AssetsDocument9 pagesOpportunity, Not Threat: Crypto AssetsTrophy NcNo ratings yet
- Supply Chain AssignmentDocument29 pagesSupply Chain AssignmentHisham JackNo ratings yet
- Tennessee Inmate Search Department of Corrections LookupDocument9 pagesTennessee Inmate Search Department of Corrections Lookupinmatesearchinfo50% (2)
- GCSE Bearings: Measuring Bearings Test Your UnderstandingDocument5 pagesGCSE Bearings: Measuring Bearings Test Your UnderstandingSamuel KalemboNo ratings yet
- Auto TraderDocument49 pagesAuto Tradermaddy_i5100% (1)
- The Wild PartyDocument3 pagesThe Wild PartyMeganMcArthurNo ratings yet
- How To Use This Engine Repair Manual: General InformationDocument3 pagesHow To Use This Engine Repair Manual: General InformationHenry SilvaNo ratings yet
- What Blockchain Could Mean For MarketingDocument2 pagesWhat Blockchain Could Mean For MarketingRitika JhaNo ratings yet
- Mastering ArpeggiosDocument58 pagesMastering Arpeggiospeterd87No ratings yet
- Communicative Competence: Noam ChomskyDocument2 pagesCommunicative Competence: Noam ChomskyKiara Denise SuarezNo ratings yet
- Icici Bank FileDocument7 pagesIcici Bank Fileharman singhNo ratings yet
- Sample Letter of Intent To PurchaseDocument2 pagesSample Letter of Intent To PurchaseChairmanNo ratings yet
- 11th AccountancyDocument13 pages11th AccountancyNarendar KumarNo ratings yet
- 2020 Book WorkshopOnFrontiersInHighEnerg PDFDocument456 pages2020 Book WorkshopOnFrontiersInHighEnerg PDFSouravDeyNo ratings yet
- 12 Preliminary Conference BriefDocument7 pages12 Preliminary Conference Briefkaizen shinichiNo ratings yet
- Science 10-2nd Periodical Test 2018-19Document2 pagesScience 10-2nd Periodical Test 2018-19Emiliano Dela Cruz100% (3)
- Quiz 1 model answers and marketing conceptsDocument10 pagesQuiz 1 model answers and marketing conceptsDavid LuNo ratings yet
- Java Interview Questions: Interfaces, Abstract Classes, Overloading, OverridingDocument2 pagesJava Interview Questions: Interfaces, Abstract Classes, Overloading, OverridingGopal JoshiNo ratings yet
- Ethnic Conflicts and PeacekeepingDocument2 pagesEthnic Conflicts and PeacekeepingAmna KhanNo ratings yet
- Improve Your Social Skills With Soft And Hard TechniquesDocument26 pagesImprove Your Social Skills With Soft And Hard TechniquesEarlkenneth NavarroNo ratings yet
- AFRICAN SYSTEMS OF KINSHIP AND MARRIAGEDocument34 pagesAFRICAN SYSTEMS OF KINSHIP AND MARRIAGEjudassantos100% (2)