Professional Documents
Culture Documents
CAP Flow Sheet PDF 62015 PDF
Uploaded by
roshmaeOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
CAP Flow Sheet PDF 62015 PDF
Uploaded by
roshmaeCopyright:
Available Formats
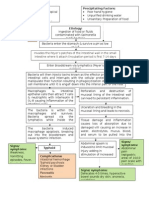
PEDIATRIC COMMUNITY-ACQUIRED PNEUMONIA CLINICAL GUIDELINE
Guideline Eligibility Criteria: Assessment: Respiratory status (rate for age,
Age 3 months to 17 years WOB, crackles, decreased or abnormal breath
Previously healthy children with no underlying conditions sounds), AMS, apnea, pulse ox < 90% on room
Clinical findings of CAP air, Immunization Status (DTaP, Pneumoccocal,
influenza, HiB), Exposure to TB
Guideline Exclusion:
Aspiration Intervention: oxygen to keep sats >92%, IVF if
Immunocompromised children clinically indicated.
Recent hospitalization (<7days before the onset of
illness)
Underlying lung disease or other chronic condition *Tachypnea*
Meets inpatient criteria: Age 0-2mo: >60
Age 2-12mo: >50
Outpatient Management O2 sats < 90% Age 1-5 yrs: >40
Influenza: oseltamivir (or NO Not tolerating PO Age >5 yrs: >20
zanamivir for children 7) Age 3 to 6 mo
Presumed bacterial: Respiratory distress WHO Criteria for severe illness
Not able to drink
Preferred: amoxicillin
persistent vomiting
(Alternative: augmentin) YES convulsions
PCN allergic: CTX, cefotaxime, lethargic or unconscious
or clindamycin Severely ill? stridor in a calm child
Presumed atypical: Azithromycin
NO YES
>5years old: Consider empiric
Inpatient Management:
addition of azithromycin
Severe or concern for Complicated CAP
Repeat CXR in 4-6 wks if concern Inpatient Management: CXR at admission
for lung collapse to r/o mass, Uncomplicated CAP Labs to consider: Flu/RSV if <3yrs, Flu if >3
anatomic anomaly CXR at admission yrs, (RVP only if Flu/RSV negative), Blood culture
No labs required x1, CRP/ESR (only to trend improvement)
Start therapy CBC is not helpful in trending disease or
determining viral vs bacterial cause
Start therapy
ANTI-MICROBIAL THERAPY
Continued Considerations Immunized
D/c antibiotics if RVP positive Ampicillin or penicillin G
D/c IVF when tolerating PO Alternatives (PCN allergic): ceftriaxone, cefotaxime, clindamycin
Change to oral antibiotics upon Not Fully Immunized for H. flu and S. pneumo
clinical improvement Ceftriaxone or cefotaxime
Repeat CXR if no clinical Resistant organism
improvement in 48 to 72 hrs
Ceftriaxone 100 mg/kg/day divided q12-24h
Discharge Criteria **Add macrolide only if M. pneumonia or C. pneumonia are
Tolerating PO significant considerations
No supplemental O2 for 12-24h
Respiratory rate normal for age **Start oseltamivir if influenza + or if high suspicion for influenza
even if test negative
If severely Ill consider:
Empiric influenza treatment
Created 6/2015. Based on IDSA CAP guidelines 2011.
CA-MRSA, add vancomycin or clindamycin
Temp>39? WBC >15,00Suspician for CA-MRSA?
You might also like
- Coagulation Cascade: Difference Between Intrinsic and Extrinsic PathwayDocument10 pagesCoagulation Cascade: Difference Between Intrinsic and Extrinsic Pathwayroshmae100% (1)
- Cap PDFDocument1 pageCap PDFroshmaeNo ratings yet
- CAP Flow Sheet PDF 62015 PDFDocument1 pageCAP Flow Sheet PDF 62015 PDFroshmaeNo ratings yet
- IM - Focal Seizure ReportDocument2 pagesIM - Focal Seizure ReportroshmaeNo ratings yet
- Topic:: Obejctives Content TA T-L Activitie S Materials Resources Evaluatio NDocument2 pagesTopic:: Obejctives Content TA T-L Activitie S Materials Resources Evaluatio NroshmaeNo ratings yet
- CPG Pcap 2012 PDFDocument54 pagesCPG Pcap 2012 PDFroshmae67% (3)
- Surgery - PAODDocument4 pagesSurgery - PAODroshmaeNo ratings yet
- PD Surgery - Incarcerated Hernia - Dr. RanaDocument2 pagesPD Surgery - Incarcerated Hernia - Dr. RanaroshmaeNo ratings yet
- IM - Focal Seizure ReportDocument8 pagesIM - Focal Seizure ReportroshmaeNo ratings yet
- FCM IiiDocument2 pagesFCM IiiroshmaeNo ratings yet
- BP: HR: RR: Temp:: CBC Count Pulse Oximetry (Oxygen Saturation) CreatinineDocument2 pagesBP: HR: RR: Temp:: CBC Count Pulse Oximetry (Oxygen Saturation) CreatinineroshmaeNo ratings yet
- Sentinel Lymph Node DissectionDocument9 pagesSentinel Lymph Node DissectionroshmaeNo ratings yet
- ACS WorksheetDocument6 pagesACS WorksheetroshmaeNo ratings yet
- Gyne - Congenital HypothyroidismDocument3 pagesGyne - Congenital HypothyroidismroshmaeNo ratings yet
- POT - NutritionDocument18 pagesPOT - NutritionroshmaeNo ratings yet
- After Bea's PPT Psych Reports. 4.5 - 4.6Document51 pagesAfter Bea's PPT Psych Reports. 4.5 - 4.6roshmaeNo ratings yet
- SHEDocument3 pagesSHEroshmaeNo ratings yet
- Causes and Symptoms of HypothyroidismDocument3 pagesCauses and Symptoms of HypothyroidismroshmaeNo ratings yet
- ACS WorksheetDocument6 pagesACS WorksheetroshmaeNo ratings yet
- Recommendations 1Document1 pageRecommendations 1roshmaeNo ratings yet
- PD - Heart Failure ReportDocument28 pagesPD - Heart Failure ReportroshmaeNo ratings yet
- ResearchDocument3 pagesResearchroshmaeNo ratings yet
- PD - CopdDocument3 pagesPD - CopdroshmaeNo ratings yet
- Gyne - Functional Ovarian Cysts Treatment and ManagementDocument1 pageGyne - Functional Ovarian Cysts Treatment and ManagementroshmaeNo ratings yet
- Surgery 1Document2 pagesSurgery 1roshmaeNo ratings yet
- Typhoid Fever PathophysiologyDocument1 pageTyphoid Fever PathophysiologyroshmaeNo ratings yet
- Cervical CancerDocument32 pagesCervical CancervvmgkikiNo ratings yet
- PD - Heart Failure ReportDocument28 pagesPD - Heart Failure ReportroshmaeNo ratings yet
- Case 1 Gyne ID, PEDocument2 pagesCase 1 Gyne ID, PEroshmaeNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5784)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Brest Lump History TakingDocument3 pagesBrest Lump History Takinganon_619577898No ratings yet
- Rashes in Children - Paediatric Dermatology Guideline Jan17 PDFDocument24 pagesRashes in Children - Paediatric Dermatology Guideline Jan17 PDFpatmcgarryNo ratings yet
- DaftaDocument5 pagesDaftaAstika Ulfah IzzatiNo ratings yet
- Buku Ishihara 38 Plates Single CoverDocument53 pagesBuku Ishihara 38 Plates Single CoverPriNceZheBaroxBozkidAvengedsefenvold86% (7)
- Traudel Saurenmann, MD University Children S Hospital Zürich, SwitzerlandDocument40 pagesTraudel Saurenmann, MD University Children S Hospital Zürich, SwitzerlandKhun Leang ChhunNo ratings yet
- Skripsi. Jurnal Untan - Ac.id Miopi PDFDocument20 pagesSkripsi. Jurnal Untan - Ac.id Miopi PDFrifkaraihanaNo ratings yet
- Journal CubDocument33 pagesJournal CubHaritha K MuraleedharanNo ratings yet
- Irish Study Finds High Incidence of Sudden Cardiac Death in YouthDocument8 pagesIrish Study Finds High Incidence of Sudden Cardiac Death in YouthDusan OrescaninNo ratings yet
- EmpagliflozinDocument2 pagesEmpagliflozinAusaf AhmadNo ratings yet
- Daftar Diagnosa Penyakit Berdasarkan Icd-10: Poli Dalam Poli ParuDocument4 pagesDaftar Diagnosa Penyakit Berdasarkan Icd-10: Poli Dalam Poli ParuNannda SuccindaaNo ratings yet
- Sedative-Hypnotic and Antipsychotic Drugs GuideDocument17 pagesSedative-Hypnotic and Antipsychotic Drugs GuideBijay Kumar MahatoNo ratings yet
- Infectious Disease Naplex QuestionsDocument3 pagesInfectious Disease Naplex QuestionsSARANYA0% (1)
- Management of Common Infections With Antimicrobials Guidance Clinical Practice Guidelines (2019) PDFDocument4 pagesManagement of Common Infections With Antimicrobials Guidance Clinical Practice Guidelines (2019) PDFveerrajuNo ratings yet
- Drug Study GuideDocument2 pagesDrug Study GuideAubrey SungaNo ratings yet
- Master DDD 2017Document904 pagesMaster DDD 2017Ainul YuyunNo ratings yet
- Obstetrics History ExampleDocument3 pagesObstetrics History ExampleMohamed Elprince Adel100% (3)
- MRANZCOG Sample Multiple Choice Questions GOBDocument4 pagesMRANZCOG Sample Multiple Choice Questions GOBdreamzbooksNo ratings yet
- Examples of Types of TabletsDocument1 pageExamples of Types of TabletsBianca Therese67% (6)
- Pharma Exam SampleDocument4 pagesPharma Exam SampleteabagmanNo ratings yet
- AppendicitisDocument1 pageAppendicitisvaleriaNo ratings yet
- Rundown SeminarDocument5 pagesRundown SeminarMuhamad AriefNo ratings yet
- Analgesic in Oral SurgeryDocument24 pagesAnalgesic in Oral SurgeryPushpa KumariNo ratings yet
- Drug Study HydralazineDocument10 pagesDrug Study HydralazineLuige AvilaNo ratings yet
- Drug List FinalsDocument2 pagesDrug List FinalsMyzhel InumerableNo ratings yet
- Ada-Montefiore Dka Protcol Version 3.0 5 22 20Document3 pagesAda-Montefiore Dka Protcol Version 3.0 5 22 20ibnuNo ratings yet
- Symptoms of Low PotassiumDocument3 pagesSymptoms of Low PotassiumCharlene Mae Calanoy100% (1)
- Practice Template Red FlagsDocument32 pagesPractice Template Red FlagsAngelaNo ratings yet
- Hiv VaccinationsDocument5 pagesHiv Vaccinationsblueivy66No ratings yet
- Peritonsillar Abscess (Quinsy)Document18 pagesPeritonsillar Abscess (Quinsy)Michael AmandyNo ratings yet
- Major R Cance Er Miles Stones: Overvie EwDocument14 pagesMajor R Cance Er Miles Stones: Overvie Ewtkobosz4877No ratings yet