Professional Documents
Culture Documents
Medical Imaging Reading, Essential Clinical Anatomy
Uploaded by
BoCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Medical Imaging Reading, Essential Clinical Anatomy
Uploaded by
BoCopyright:
Available Formats
INTRODUCTION TO CLINICAL ANATOMY 39
sympathetic system in its distribution. The parasympathetic sys- information about the condition of the bodys internal envi-
tem distributes only to the head, visceral cavities of the trunk, ronment. This information is integrated in the CNS, often
and erectile tissues of the external genitalia. With the exception triggering visceral or somatic reflexes or both. Visceral reflexes
of the latter, it does not reach the body wall or limbs, and except regulate blood pressure and chemistry by altering such func-
for initial parts of the anterior rami of spinal nerves S2S4, its tions as heart and respiratory rates and vascular resistance.
fibers are not components of spinal nerves or their branches. Visceral sensation that reaches a conscious level is generally
Four discrete pairs of parasympathetic ganglia occur in the categorized as pain that is usually poorly localized and may
head (see Chapters 7 and 9). Elsewhere, presynaptic parasym- be perceived as hunger or nausea. However, adequate stim-
pathetic fibers synapse with postsynaptic cell bodies, which ulation, such as the following, may elicit true pain: sudden
occur singly in or on the wall of the target organ (intrinsic or distention, spasms or strong contractions, chemical irritants,
enteric ganglia). Most presynaptic parasympathetic fibers are mechanical stimulation (especially when the organ is active),
long, extending from the CNS to the effector organ, whereas and pathological conditions (especially ischemiainadequate
the postsynaptic fibers are short, running from a ganglion lo- blood supply) that lower the normal thresholds of stimulation.
cated near or embedded in the effector organ. Normal activity usually produces no sensation but may do so
when there is ischemia. Most visceral reflex (unconscious)
sensation and some pain travel in visceral afferent fibers that
Visceral Afferent Sensation accompany the parasympathetic fibers retrograde. Most vis-
Visceral afferent fibers have important relationships to the ceral pain impulses (from the heart and most organs of the
ANS, both anatomically and functionally. We are usually un- peritoneal cavity) travel centrally along visceral afferent fibers
aware of the sensory input of these fibers, which provides accompanying sympathetic fibers.
Medical Imaging
Body Systems Arch of aorta
Clavicle Rib Trachea Pulmonary
Familiarity with imaging techniques commonly used in clinical artery
settings enables one to recognize abnormalities such as congeni-
tal anomalies, tumors, and fractures. The introduction of contrast
media allows the study of various luminal or vascular organs and
potential or actual spaces, such as the digestive or alimentary sys-
tem, blood vessels, kidneys, synovial cavities, and subarachnoid
space. This section consists of short descriptions of the principles
of some of the commonly used diagnostic imaging techniques:
Conventional radiography (ordinary X-ray images)
Computerized tomography (CT) Heart
Ultrasonography (US)
Magnetic resonance imaging (MRI)
Positron emission tomography (PET)
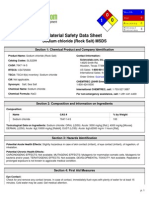
CONVENTIONAL RADIOGRAPHY
The essence of a radiological examination is that a highly penetrat- Right dome
of diaphragm Apex of heart
ing beam of X-rays transilluminates the patient, showing tissues of
differing densities of mass within the body as images of differing Postero-anterior (PA) projection
densities of light and dark on the X-ray film (Fig. I.32). A tissue
FIGURE I.32. Radiograph of thorax (chest).
or organ that is relatively dense in mass, such as compact bone in
a rib, absorbs more X-rays than does a less dense tissue, such as
spongy (cancellous) bone (Table I.5). Consequently, a dense tissue area when the film is processed. A very dense substance is radi-
or organ produces a relatively transparent area on the X-ray film opaque, whereas a substance of less density is radiolucent.
because relatively fewer X-rays reach the emulsion in the film. Many of the same principles that apply to making a shadow
Therefore, relatively fewer grains of silver are developed at this apply to conventional radiography. Radiographs are made with the
Moore_Ch00_Intro.indd 39 1/9/14 9:41 PM
40 INTRODUCTION TO CLINICAL ANATOMY
TABLE I.5 BASIC PRINCIPLES OF X-RAY IMAGE X-ray tube
FORMATION
Most radiolucent Air Least radiodense
Fat
Water and most tissues
Spongy bone
Least radiolucent Compact bone Most radiodense
Detectors
part of the patients body being studied close to the X-ray film or
detector to maximize the clarity of the image and minimize mag-
nification artifacts. In basic radiological nomenclature, postero- (A)
anterior (PA) projection refers to a radiograph in which the X-rays
traversed the patient from posterior (P) to anterior (A); the X-ray
tube was posterior to the patient and the X-ray film or detector Right Left
was anterior. A radiograph using anteroposterior (AP) projection
radiography is the opposite. Both PA and AP projection radio- Rib
graphs are viewed as if you and the patient were facing each other
(the patients right side is opposite your left); this is referred to as Pancreas
an anteroposterior view. Thus, the standard chest X-ray, taken to
examine the heart and lungs, is an AP view of a PA projection. For Liver Aorta
lateral radiographs, radiopaque letters (R or L) are used to indicate
Vertebra
the side placed closest to the film or detector, and the image is
viewed from the same direction that the beam was projected. Left
The introduction of contrast media (radiopaque fluids such as kidney
iodine compounds or barium) allows the study of various luminal
or vascular organs and potential or actual spacessuch as the (B) Transverse CT image of upper abdomen
digestive tract, blood vessels, kidneys, synovial cavities, and the
subarachnoid spacethat are not visible in plain films. Most
radiological examinations are performed in at least two projections
at right angles to each other. Because each radiograph presents
a two-dimensional (2-D) representation of a three-dimensional
(3-D) structure, structures sequentially penetrated by the X-ray
beam overlap each other. Thus, more than one view is usually
necessary to detect and localize an abnormality accurately.
COMPUTERIZED TOMOGRAPHY
CT shows images of the body that resemble transverse anatomi-
cal sections (Fig. I.33). A beam of X-rays is passed through the
body as the X-ray tube and detector rotate around the axis of the
body. The amount of radiation absorbed by each different type
of tissue of the chosen body plane varies with the amount of fat,
bone, and water in each element. A computer compiles and gen- (C) Three-dimensional CT reconstruction
erates images as 2-D slices and total 3-D reconstructions. of bones of wrist and hand (palmar view)
FIGURE I.33. Computerized tomography. A. The X-ray tube rotates
ULTRASONOGRAPHY around the person in the CT scanner and sends a fan-shaped beam of
US is a technique that allows visualization of superficial or deep X-rays through the persons body from a variety of angles. X-ray detectors
structures in the body by recording pulses of ultrasonic waves on the opposite side of the persons body measure the amount of radia-
reflecting off the tissues (Fig. I.34). The images can be viewed tion that passes through a transverse section of the person. B and C. A
computer reconstructs the CT images. Transverse scans are oriented so
in real time to demonstrate the motion of structures and flow
they appear the way an examiner would view the section when standing at
within blood vessels (Doppler US) and then recorded as single the foot of the bed and looking toward a supine persons head.
Moore_Ch00_Intro.indd 40 1/9/14 9:41 PM
INTRODUCTION TO CLINICAL ANATOMY 41
images or as a movie. Because US is noninvasive and does not
use radiation, it is the standard method of evaluating the growth
and development of the embryo and fetus.
MAGNETIC RESONANCE IMAGING
MRI shows images of the body similar to those produced by CT,
but they are better for tissue differentiation (Fig. I.35). Using
MRI, the clinician is able to reconstruct the tissues in any plane,
even arbitrary oblique planes. The person is placed in a scanner
Transducer
with a strong magnetic field, and the body is pulsed with radio
Acoustic gel waves. Signals subsequently emitted from the patients tissues
coupling agent
are stored in a computer and may be reconstructed in 2-D or
Body wall 3-D images. The appearance of tissues on the generated images
Ultrasound can be varied by controlling how radiofrequency pulses are sent
waves and received. Scanners can be gated or paced to visualize mov-
Echo ing structures, such as the heart and blood flow, in real time.
Kidney POSITRON EMISSION TOMOGRAPHY
PET scanning uses cyclotron-produced isotopes of extremely
short half-life that emit positrons. PET scanning is used to eval-
(A)
uate the physiological functions of organs such as the brain on a
dynamic basis. Areas of increased brain activity will show selec-
tive uptake of the injected isotope (Fig. I.36).
RK
RK
(B)
LK
LRV
LRA
(C) Transverse Doppler ultrasound
FIGURE I.34. Ultrasonography. A. The image results from the echo of
ultrasound waves from structures of different densities. B. A longitudinal
image of a right kidney (RK) is displayed. C. Doppler US shows blood flow
to and away from the kidney. LK, left kidney; LRA, left renal artery; LRV,
left renal vein.
Moore_Ch00_Intro.indd 41 1/9/14 9:41 PM
42 INTRODUCTION TO CLINICAL ANATOMY
Right atrium Aorta Left atrium
Air-filled Brain Cerebellum Venous sinus
sinus (cerebrum) (fluid-filled)
Fluid-filled Spinal cord Subcutaneous
subarachnoid tissue (fat)
space
Right ventricle Left ventricle
(A) Left lateral views (B)
FIGURE I.35. Magnetic resonance imaging. A. Sagittal MRI study of the head and upper neck. B. Magnetic resonance angiogram of heart and great
vessels.
(B)
FIGURE I.36. Positron emission tomography. A. PET scanner.
B. Transverse scans. Observe the differences in brain activity associated
with the planning and execution of a specific task in contrast to a control
(A) brain.
Go to http://thePoint.lww.com/ for helpful study tools, including USMLE-style questions, case studies, images, and more!
Moore_Ch00_Intro.indd 42 1/9/14 9:41 PM
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Publically Available Patent 3Document90 pagesPublically Available Patent 3BoNo ratings yet
- Publically Available Patent 2Document39 pagesPublically Available Patent 2BoNo ratings yet
- Publically Available Patent 1Document40 pagesPublically Available Patent 1BoNo ratings yet
- 2017 Arkansas Health Manpower ReportDocument95 pages2017 Arkansas Health Manpower ReportBoNo ratings yet
- Organic Chemistry WorksheetDocument10 pagesOrganic Chemistry WorksheetBoNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Flip Chart 06 IUDDocument12 pagesFlip Chart 06 IUDLamyaa Ali HasanNo ratings yet
- Nursing Management HydrocephalusDocument4 pagesNursing Management HydrocephalusPrecious Mae Benologa100% (1)
- Spring Meadows Hospital VsDocument10 pagesSpring Meadows Hospital VsManoj Kumar MNo ratings yet
- Director, Office of Workers' Compensation Programs, United States Department of Labor v. August Mangifest, 826 F.2d 1318, 3rd Cir. (1987)Document27 pagesDirector, Office of Workers' Compensation Programs, United States Department of Labor v. August Mangifest, 826 F.2d 1318, 3rd Cir. (1987)Scribd Government DocsNo ratings yet
- Ebook - Yoga - The Science of BreathDocument2 pagesEbook - Yoga - The Science of BreathGabriel CiocanNo ratings yet
- Maquet Meera BrochureDocument16 pagesMaquet Meera BrochureFeridun MADRANNo ratings yet
- Typhoid Fever at A GlanceDocument2 pagesTyphoid Fever at A GlanceLIZNo ratings yet
- CAPNOGRAPHYDocument10 pagesCAPNOGRAPHYJessica GuzmanNo ratings yet
- Chalcone Synthesis, Structure DiversityDocument13 pagesChalcone Synthesis, Structure DiversityDini Elsi ANo ratings yet
- Sodium Chloride (Rock Salt) MSDS: Section 1: Chemical Product and Company IdentificationDocument6 pagesSodium Chloride (Rock Salt) MSDS: Section 1: Chemical Product and Company IdentificationMohamed MaghawryNo ratings yet
- Current Management of LabourDocument48 pagesCurrent Management of Labourapi-3705046100% (4)
- CyberTherapy & Rehabilitation, Issue 3 (3), Winter 2010.Document52 pagesCyberTherapy & Rehabilitation, Issue 3 (3), Winter 2010.Giuseppe RivaNo ratings yet
- Stages of Labor and DeliveryDocument4 pagesStages of Labor and DeliveryvienreyNo ratings yet
- Pga CetDocument31 pagesPga CetDrHassan Ahmed ShaikhNo ratings yet
- Womens Era May (Second) 2010Document148 pagesWomens Era May (Second) 2010ShaktirajanNo ratings yet
- Social Stratification in The PhilippinesDocument11 pagesSocial Stratification in The PhilippinesMichael VillavertNo ratings yet
- Risk Factors Pathophysiology and Management of HypertensionDocument13 pagesRisk Factors Pathophysiology and Management of HypertensionDominggas RusunwullyNo ratings yet
- Sistem Pelaporan Dan Pembelajaran Keselamatan Pasien RS Arjaty 2022Document13 pagesSistem Pelaporan Dan Pembelajaran Keselamatan Pasien RS Arjaty 2022vera kusunyadewiNo ratings yet
- AlprazolamDocument10 pagesAlprazolamWen SilverNo ratings yet
- Raja Sir CampDocument6 pagesRaja Sir CampNivedan KothekarNo ratings yet
- NCP Peptic Ulcer DsDocument4 pagesNCP Peptic Ulcer Dsplug0650% (10)
- Procalcitonin Testing To Guide Antibiotic Therapy in Acute Upper and Lower Respiratory Tract InfectionsDocument2 pagesProcalcitonin Testing To Guide Antibiotic Therapy in Acute Upper and Lower Respiratory Tract InfectionsMr. LNo ratings yet
- CarcinogenesisDocument40 pagesCarcinogenesisNatasha AmaldaNo ratings yet
- 1005 Hemorrhage ControlDocument88 pages1005 Hemorrhage ControlZainescu Dan100% (2)
- JCIA Handbook 2020Document61 pagesJCIA Handbook 2020WAQASNo ratings yet
- EDIC Guidelines 2017 PDFDocument22 pagesEDIC Guidelines 2017 PDFZia ShaikhNo ratings yet
- DR Irza Wahid - Annemia Approach - 139Document60 pagesDR Irza Wahid - Annemia Approach - 139single_ladyNo ratings yet
- Compare Prokaryotes and Eukaryotes: Gram +ve Gram - Ve Peptidoglycan Layer Teichoic Acid Surface AntigenDocument12 pagesCompare Prokaryotes and Eukaryotes: Gram +ve Gram - Ve Peptidoglycan Layer Teichoic Acid Surface AntigenAamir BugtiNo ratings yet
- Fascio LaDocument20 pagesFascio LaMuhammad NoorNo ratings yet
- 10 Hip Replacement SurgeryDocument13 pages10 Hip Replacement SurgeryDIA PHONG THANGNo ratings yet