Professional Documents
Culture Documents
Presenting The Patient
Uploaded by
Ali ZeinOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Presenting The Patient
Uploaded by
Ali ZeinCopyright:
Available Formats
PRESENTATION TEMPLATE
Presentation without template: Presentation WITH template:
H&P: H&P: H&P:
Ms. Smith is a 56yoF who has been having shortness (Killer first line:)
Ms. Smith is a _(age)_ yo __(M/F)__ Ms. Smith is a 56yoF with history of CAD with
of breath for a week. She is very anxious and has with history of ___(pertinent PMH/meds)_____ stents now on plavix, CHF with EF of 30% on lasix,
not been sleeping well the past week, as she keeps presenting today with (timeline) of ___(chief and mild asthma, here with 1 week of slowly
waking up suddenly gasping for air. She has a complaint)___ . worsening shortness of breath.
history of asthma and has also been using her
albuterol. She has been having some leg pain as well (OLD CARTS - additional description of chief It is worse when she lies down at night and with
which is worse when she walks. The legs are complaint.) walking. She used to be able to walk 1 block and
swollen, too. She has been taking her lasix and took It ________(briefly describe timeline, quality, now she gets short of breath just walking to the
an extra dose yesterday. She has been having more constant/comes/goes, what makes it better or worse, bathroom. She did take an extra dose of lasix
shortness of breath walking around the house, treatments). which helped a little.
where as she used to be able to walk a block. She
has not had any recent surgery or long distance (Sx for/against Differential #1): (#1- CHF)
travel. No sick contacts. It is associated with ____ (pertinent positives). It is associated with worsening leg swelling
bilaterally, that is slightly painful. It is worse at
ROS are positive for shortness of breath, leg night and sometimes she wakes up gasping, which
swelling, anxiety, and leg pain. is affecting her sleep and causing lots of anxiety.
ROS are negative for headache, fevers, chills, (Sx for/against Differential #2) : (#2- asthma)
diaphoresis, changes in vision, chest pain, cough, She does have ___ (pertinent positives). But does not She does have a history of asthma but in the past
rhinorrhea, wheezing, abdominal pain, nausea, have ____ (pertinent negatives). has been very well controlled and immediately
vomiting, diarrhea, constipation, numbness, resolves with albuterol. She did try albuterol and
weakness, falls, extremity pain. it did not help her shortness of breath. No
wheezing or rhinorrhea / itching.
PMH includes CHF, CAD, stents, and asthma. She
has never blood clots. (Neg ROS that make Differential #3 unlikely): (#3- ACS)
She does not have _______. She is not having any chest pain, diaphoresis, arm
Her medications include albuterol, lasix, and plavix. pain, or nausea.
(Neg ROS that make Differential #4 unlikely): (#4 - PNA)
There is no _______. She is not having any fevers, productive cough or
body aches.
(Neg ROS that make Differential #5 unlikely): (#5 - PE)
There is no _______. Her leg swelling is bilateral, she has no hx of
clots/DVTs, no recent immobility.
Exam: Exam: Exam:
Her temp is 98F, HR is 80, RR is 22, BP of 160/90, Vitals- Interpret! She is afebrile and not tachycardic. Slightly
and her O2 sat is 90% on RA (insert rest of pertinent exam here) hypertensive at 160/90. Increased respiratory
rate of 22, is slightly hypoxic at 90% on RA
Impression: Impression: Impression:
The differential diagnosis includes CHF (Differential #1) (#1- CHF)
exacerbation, asthma exacerbation, acute MI, I am concerned the pt is having __(#1)___. or I I am concerned the patient is having a CHF
pneumonia or pulmonary embolism. think in this patient we need to rule out __(#1)___. exacerbation and is fluid overloaded.
(Differential #2/3) (#2- asthma)
I think we should get: She also might have __(#2/3)___ due to the She does have a history of asthma, but her
- basic labs ___(findings for)___ however she doesnt have shortness of breath today is not associated with
- BNP ___(findings against)___. wheezing on exam, and the leg swelling still makes
- VBG CHF more likely.
- d dimer
- cardiac enzymes (#3- ACS)
- give oxygen She could be having an MI that is exacerbating the
- EKG CHF, although she does not have any chest pain.
- CXR She does have coronary history, though, so I think
- place her on the monitor we need to rule it out.
- give lasix, albuterol neb and ASA
- call the cardiologist (Differential #4 / #5) (#4- PNA; #5- PE)
- monitor urine output I think that this is less consistent with ___(#3)___ or I dont think this is consistent with a pneumonia or
- repeat lung exams I dont think she is having __(#4)__ because of pulmonary embolism.
_____.
(or may be no need to explain why not if you already
mentioned the pertinent negatives in your H&P)
** this is not necessarily an incorrect workup, but the
Treatments:
presentation style does not let your college know I think we should:
Treatments:
what you are thinking - place her on the monitor
I think we should give her ____(oxygen, pain control,
- give oxygen by NC
tylenol, ASA, place on monitor, give fluids)___
- give her a dose of IV lasix for diuresis
- could try an albuterol neb to see if it helps
- giver her an ASA in case she is having an MI
Workup:
Workup: I think we should get:
I think we should get ___(lab)___ to look for / rule out - a BNP to assess for fluid overload/CHF
___(# 1/2/3/4)__ - cardiac enzymes to rule out MI
- a VBG to look for signs of CO2 retention
- a CBC to rule out anemia and infection
- a BMP to look for electrolyte abnormalities and
assess her renal function
- an EKG to rule out MI or arrhythmia
And we should get __(imaging/EKG)__ to look for / rule - a CXR to look for signs of fluid overload and rule
out ___(# 1/2/3/4)__ out pneumonia or effusion
OLD CARTS for HPI: - monitor urine output after the lasix
- I will call her cardiologist to get the most recent
Onset (timing, acute, gradual)
(consider) I am going to call __consult/PMD__ to ask echo report and let him know she is here
Location
Duration (hours, days, intermittent, constant) for __ (consult, records, more hx)__
Initial Disposition:
Characteristics (quality, sharp, aching)
I think we should
Aggravating factors Initial Disposition:
(its ok for this to change!)
- repeat a lung exam / O2 Sat after diuresis
Relieving factors I think we should (examples:)
- consider getting a d-dimer to rule out PE if she
Treatments (previously tried, results) - reassess her after the pain medication
remains hypoxic and the workup is not consistent
Severity (number scale, mild, severe) - do serial abdominal exams
with CHF
- have her follow up with ortho in 1 week
- have her return for wound check in 48 hours
Anna Pickens, MD
Emergency Medicine
EMin5.com
You might also like
- Brunner Step 2 CK Study PlanDocument2 pagesBrunner Step 2 CK Study PlanhellayeahNo ratings yet
- Amazing Esqs With Answers Pediatrics-ShelfDocument31 pagesAmazing Esqs With Answers Pediatrics-ShelfDrSajid BuzdarNo ratings yet
- Ebp HandoutDocument2 pagesEbp Handoutapi-543558169No ratings yet
- CS Final PDFDocument46 pagesCS Final PDFOsteoprosis MyopathyNo ratings yet
- Soap Note Template 01Document1 pageSoap Note Template 01Matthew MarrNo ratings yet
- Mo Intern Handbook - FinalDocument37 pagesMo Intern Handbook - FinalGideon K. MutaiNo ratings yet
- 22 Disritmia 2018Document60 pages22 Disritmia 2018Nur akilaNo ratings yet
- ONDOC Format & Guide To Oral PresentationsDocument10 pagesONDOC Format & Guide To Oral PresentationsZainNo ratings yet
- Survival GuideDocument54 pagesSurvival Guidejoeyblowey88No ratings yet
- DeVirglio NotesDocument77 pagesDeVirglio NotesAlvand SehatNo ratings yet
- Internal Medicine Topic List 2015Document3 pagesInternal Medicine Topic List 2015Krystal Mae LopezNo ratings yet
- Pediatrics - Neonatal Jaundice PDFDocument2 pagesPediatrics - Neonatal Jaundice PDFJasmine KangNo ratings yet
- 01 Interview FormDocument7 pages01 Interview FormSavage SkylenNo ratings yet
- U.S. Preventive Services Task Force (USPSTF) Recommendations - Stats - Medbullets Step 2 - 3Document5 pagesU.S. Preventive Services Task Force (USPSTF) Recommendations - Stats - Medbullets Step 2 - 3mtataNo ratings yet
- Dr. Ali's Uworld Notes For Step 2 CKDocument30 pagesDr. Ali's Uworld Notes For Step 2 CKuyesNo ratings yet
- Personal Statement - FinalDocument2 pagesPersonal Statement - Finalapi-383932502No ratings yet
- Answer Sheet For Step 2 CK NBME 3Document2 pagesAnswer Sheet For Step 2 CK NBME 3JOSENo ratings yet
- Treatment of Resistant and Refractory HypertensionDocument21 pagesTreatment of Resistant and Refractory HypertensionLuis Rodriguez100% (1)
- OSCE Final 1 PDFDocument204 pagesOSCE Final 1 PDFamalNo ratings yet
- Chief Complaint HPI: Additional Info For PRESENTINGDocument2 pagesChief Complaint HPI: Additional Info For PRESENTINGAnonymous PozjVFR9100% (1)
- History and Physical AssessmentDocument31 pagesHistory and Physical AssessmentShalini RavNo ratings yet
- Oral Case Presentation Benchmarks - : Identifying Information & Chief ConcernDocument9 pagesOral Case Presentation Benchmarks - : Identifying Information & Chief ConcernManisanthosh KumarNo ratings yet
- Cardiology ConsultsDocument2 pagesCardiology ConsultsjuweriyNo ratings yet
- Dr. Ali's Uworld Notes For Step 2 CKDocument40 pagesDr. Ali's Uworld Notes For Step 2 CKmarina shawkyNo ratings yet
- Preventive Care Checklist Form ExplanationsDocument3 pagesPreventive Care Checklist Form ExplanationsKak KfgaNo ratings yet
- UWorld JournalDocument21 pagesUWorld JournalMaria SvarkaNo ratings yet
- Mock Record B-1-2-Well Child VisitsDocument4 pagesMock Record B-1-2-Well Child VisitsaelteeNo ratings yet
- Mnemonics For CsDocument7 pagesMnemonics For CsTony Menias100% (1)
- Usmle Step 2 CsDocument70 pagesUsmle Step 2 CsAlvi MuldaniNo ratings yet
- Trusted Evidence For Confident Clinical Decisions: Resources For Medication, Disease, and ToxicologyDocument10 pagesTrusted Evidence For Confident Clinical Decisions: Resources For Medication, Disease, and ToxicologyCurcubeuAuroraNo ratings yet
- Nbme 7 Block 1 AnswersDocument20 pagesNbme 7 Block 1 AnswersVictoria BlentiranNo ratings yet
- Divine Intervention Step 2CK Podcasts Notes - Read Only File - Docx (Dragged) 4Document3 pagesDivine Intervention Step 2CK Podcasts Notes - Read Only File - Docx (Dragged) 4winston1234No ratings yet
- List of Most Common Usmle DiseasesDocument5 pagesList of Most Common Usmle DiseasesDenise NewsomeNo ratings yet
- Musculoskeletal: Unit 553 September 2018Document34 pagesMusculoskeletal: Unit 553 September 2018dragon66No ratings yet
- Wallenberg Syndrome: Publication DetailsDocument9 pagesWallenberg Syndrome: Publication DetailsHuang Jen Liang100% (1)
- High Yield SurgeryDocument77 pagesHigh Yield SurgeryDr.2020No ratings yet
- Deepak Step 2 CK UwDocument347 pagesDeepak Step 2 CK Uwusmleaddict proNo ratings yet
- Weekly Clinical Prep Packet 12 REVISEDDocument12 pagesWeekly Clinical Prep Packet 12 REVISEDMei SarteNo ratings yet
- Cardiology Arteritis ChartDocument3 pagesCardiology Arteritis ChartM PatelNo ratings yet
- Pass 2010 ScheduleDocument1 pagePass 2010 SchedulewldcrdNo ratings yet
- General Principles of Disorders of Water Balance (Hyponatremia and Hypernatremia) and Sodium Balance (Hypovolemia and Edema)Document31 pagesGeneral Principles of Disorders of Water Balance (Hyponatremia and Hypernatremia) and Sodium Balance (Hypovolemia and Edema)Juan InsignaresNo ratings yet
- Jane Elizabeth Doe: 639 Street ST - Town, CT 00000Document2 pagesJane Elizabeth Doe: 639 Street ST - Town, CT 00000Kasagga BrianNo ratings yet
- Neurology Clerkship Orientation 2018-19Document32 pagesNeurology Clerkship Orientation 2018-19Elyzza G. AguasNo ratings yet
- MZ/MR A. I. First I'll Ask You Ii. Then I'll Do A Quick Iii. Then I'll Give You MyDocument6 pagesMZ/MR A. I. First I'll Ask You Ii. Then I'll Do A Quick Iii. Then I'll Give You Mykabal321No ratings yet
- Neurologic Emergencies Stroke & Tia: Devin R. Harris, MD MHSC CCFP (Em)Document10 pagesNeurologic Emergencies Stroke & Tia: Devin R. Harris, MD MHSC CCFP (Em)Samantha Lui100% (2)
- USMLE Step 2 CK Lecture Notes Obstetrics, GynecologyDocument282 pagesUSMLE Step 2 CK Lecture Notes Obstetrics, GynecologyNaeem JanwariNo ratings yet
- Kathynotes PDFDocument103 pagesKathynotes PDFvarrakeshNo ratings yet
- USMLE Step 2 (3) - Thyroid DiseaseDocument4 pagesUSMLE Step 2 (3) - Thyroid DiseaseMavra zNo ratings yet
- H&P and Dictation Template - Right Handed (6!4!15)Document1 pageH&P and Dictation Template - Right Handed (6!4!15)Solomon Seth SallforsNo ratings yet
- Brainstorm Step 2 CKDocument6 pagesBrainstorm Step 2 CKEduardo HernandezNo ratings yet
- SyncopeDocument3 pagesSyncopeanishdNo ratings yet
- Post-Cardiac Arrest Therapeutic Hypothermia Targeted Temperature Manangement (TTM) Quick SheetDocument3 pagesPost-Cardiac Arrest Therapeutic Hypothermia Targeted Temperature Manangement (TTM) Quick SheetkimberlyNo ratings yet
- Pediatrics - Lower AirwayDocument3 pagesPediatrics - Lower AirwayJasmine KangNo ratings yet
- Arteriolar Dilator Decreases After Load Ejection FractionDocument1 pageArteriolar Dilator Decreases After Load Ejection FractionJack GuccioneNo ratings yet
- Objectives IMDocument104 pagesObjectives IMlaraNo ratings yet
- CMS - Ob - Gyn 1-Answers PDFDocument13 pagesCMS - Ob - Gyn 1-Answers PDFSelena GajićNo ratings yet
- Spectroscopy ProblemDocument1 pageSpectroscopy ProblemAli ZeinNo ratings yet
- Cancers: Human Papillomavirus in Head and Neck CancerDocument22 pagesCancers: Human Papillomavirus in Head and Neck CancerAli ZeinNo ratings yet
- New Text DocumentDocument1 pageNew Text DocumentAli ZeinNo ratings yet
- MARKETING STUDY EditedDocument48 pagesMARKETING STUDY EditedRichard Rhamil Carganillo Garcia Jr.No ratings yet
- University Grading System - VTUDocument3 pagesUniversity Grading System - VTUmithilesh8144No ratings yet
- Lesson Tasks: Lesson Plan: Addition and Subtraction To 20Document2 pagesLesson Tasks: Lesson Plan: Addition and Subtraction To 20Марина СтанојевићNo ratings yet
- Hamza Akbar: 0308-8616996 House No#531A-5 O/S Dehli Gate MultanDocument3 pagesHamza Akbar: 0308-8616996 House No#531A-5 O/S Dehli Gate MultanTalalNo ratings yet
- Mod 2 MC - GSM, GPRSDocument61 pagesMod 2 MC - GSM, GPRSIrene JosephNo ratings yet
- Electron LayoutDocument14 pagesElectron LayoutSaswat MohantyNo ratings yet
- MnemonicsDocument1 pageMnemonicsSunil Boyz-uNo ratings yet
- TOPIC 2 - Fans, Blowers and Air CompressorDocument69 pagesTOPIC 2 - Fans, Blowers and Air CompressorCllyan ReyesNo ratings yet
- Open Book Online: Syllabus & Pattern Class - XiDocument1 pageOpen Book Online: Syllabus & Pattern Class - XiaadityaNo ratings yet
- Cooperative LinuxDocument39 pagesCooperative Linuxrajesh_124No ratings yet
- Code of Conduct For Public OfficialDocument17 pagesCode of Conduct For Public OfficialHaNo ratings yet
- MGN815: Business Models: Ajay ChandelDocument38 pagesMGN815: Business Models: Ajay ChandelSam RehmanNo ratings yet
- Statistics and Probability Course Syllabus (2023) - SignedDocument3 pagesStatistics and Probability Course Syllabus (2023) - SignedDarence Fujihoshi De AngelNo ratings yet
- MATLAB For Data VisualizationDocument63 pagesMATLAB For Data Visualizationfahmi fawjiNo ratings yet
- Fortigate System Admin 40 Mr2Document115 pagesFortigate System Admin 40 Mr2KhaleelNo ratings yet
- Adolescence Problems PPT 1Document25 pagesAdolescence Problems PPT 1akhila appukuttanNo ratings yet
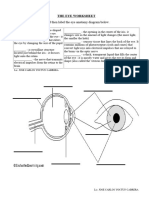
- The Eye WorksheetDocument3 pagesThe Eye WorksheetCally ChewNo ratings yet
- Grade 8 Science Text Book 61fb9947be91fDocument289 pagesGrade 8 Science Text Book 61fb9947be91fNadarajah PragatheeswarNo ratings yet
- ARMY - Chapter Eight Explosive BreachingDocument25 pagesARMY - Chapter Eight Explosive Breachingrsreeth100% (1)
- MVC Training Course Prerequisite: WWW - Focustech.InDocument2 pagesMVC Training Course Prerequisite: WWW - Focustech.InLakshman Samanth ReddyNo ratings yet
- Notes 3 Mineral Dressing Notes by Prof. SBS Tekam PDFDocument3 pagesNotes 3 Mineral Dressing Notes by Prof. SBS Tekam PDFNikhil SinghNo ratings yet
- 1941 Iraq and The IlluminatiDocument4 pages1941 Iraq and The IlluminatiZaneWeltonNo ratings yet
- Vialyn Group ResearchDocument17 pagesVialyn Group ResearchVial LynNo ratings yet
- Interventional Studies 2Document28 pagesInterventional Studies 2Abdul RazzakNo ratings yet
- On The Margins - A Study of The Experiences of Transgender College StudentsDocument14 pagesOn The Margins - A Study of The Experiences of Transgender College StudentsRory J. BlankNo ratings yet
- Exploring Nurses' Knowledge of The Glasgow Coma Scale in Intensive Care and Emergency Departments at A Tertiary Hospital in Riyadh City, Saudi ArabiaDocument9 pagesExploring Nurses' Knowledge of The Glasgow Coma Scale in Intensive Care and Emergency Departments at A Tertiary Hospital in Riyadh City, Saudi Arabianishu thapaNo ratings yet
- Norm ANSI PDFDocument1 pageNorm ANSI PDFAbdul Quddus Mat IsaNo ratings yet
- Claudia Maienborn, Semantics, 381Document34 pagesClaudia Maienborn, Semantics, 381robert guimaraesNo ratings yet
- Grade 8 Least Mastered Competencies Sy 2020-2021: Handicraft Making Dressmaking CarpentryDocument9 pagesGrade 8 Least Mastered Competencies Sy 2020-2021: Handicraft Making Dressmaking CarpentryHJ HJNo ratings yet
- Chapter 5: Current and Resistance: 5.1 The Motion of Electric ChargeDocument11 pagesChapter 5: Current and Resistance: 5.1 The Motion of Electric Chargeayunna ayunniNo ratings yet