Professional Documents
Culture Documents
HCP LAN APM Framework One-Pager 2017
Uploaded by
iggybauCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
HCP LAN APM Framework One-Pager 2017
Uploaded by
iggybauCopyright:
Available Formats
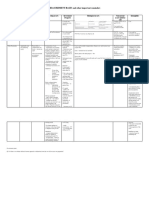
Alternative Payment Models
THE APM FRAMEWORK
This Framework represents payments from public and private payers to provider organizations (including payments between the
payment and delivery arms of highly integrated health systems). It is designed to accommodate payments in multiple categories
that are made by a single payer, as well as single provider organizations that receive payments in different categoriespotentially
from the same payer. Although payments will be classified in discrete categories, the Framework captures a continuum of
clinical and financial risk for provider organizations.
CATEGORY 1 CATEGORY 2 CATEGORY 3 CATEGORY 4
FEE FOR SERVICE FEE FOR SERVICE APMS BUILT ON POPULATION
NO LINK TO LINK TO QUALITY FEE-FOR-SERVICE BASED PAYMENT
QUALITY & VALUE & VALUE ARCHITECTURE
A A A
Foundational Payments APMs with Condition-Specic
for Infrastructure Shared Savings Population-Based
& Operations (e.g., shared savings with Payment
(e.g., care coordination upside risk only) (e.g., per member per month
fees and payments for payments, payments for
HIT investments) B specialty services, such as
oncology or mental health)
APMs with
B Shared Savings
Pay for Reporting and Downside Risk B
(e.g., bonuses for reporting (e.g., episode-based Comprehensive
data or penalties for not payments for procedures Population-Based
reporting data) and comprehensive Payment
payments with upside (e.g., global budgets or
C and downside risk) full/percent of premium
payments)
Pay-for-Performance
(e.g., bonuses for quality C
performance)
Integrated Finance
& Delivery Systems
(e.g., global budgets or
full/percent of premium
payments in integrated
systems)
3N 4N
Risk Based Payments Capitated Payments
NOT Linked to Quality NOT Linked to Quality
hcp-lan.org
You might also like
- Cost Benefit Analysis in A Government ContextDocument26 pagesCost Benefit Analysis in A Government ContextMariel SumisimNo ratings yet
- Annex B - Compliance With Other Regulatory Requirements For CY2022Document16 pagesAnnex B - Compliance With Other Regulatory Requirements For CY2022Cha Gamboa De LeonNo ratings yet
- Format Sec 14 SarfaesiDocument11 pagesFormat Sec 14 SarfaesiHari100% (6)
- Project Background BhopalDocument13 pagesProject Background Bhopalbnkarthik00dbNo ratings yet
- Standardized Approach For Counterparty Credit RiskDocument2 pagesStandardized Approach For Counterparty Credit RiskjalutukNo ratings yet
- Pay Is inDocument2 pagesPay Is inJo YelleNo ratings yet
- Legal - Research FINAL EXAMDocument2 pagesLegal - Research FINAL EXAMBenhar Limpasan Jr.No ratings yet
- Template WFP-Expenditure Form 2024Document22 pagesTemplate WFP-Expenditure Form 2024Joey Simba Jr.No ratings yet
- Elements of Accounting LectureDocument43 pagesElements of Accounting LectureRaissa Mae100% (1)
- Rosalind Krauss, Cultural Logic of The Late Capitalist MuseumDocument16 pagesRosalind Krauss, Cultural Logic of The Late Capitalist MuseumMartha SchwendenerNo ratings yet
- HCP Lan Apm Fact Sheet 2017Document2 pagesHCP Lan Apm Fact Sheet 2017iggybauNo ratings yet
- Jica Basic Concept of AP and Case Study in JapanDocument28 pagesJica Basic Concept of AP and Case Study in JapanhenrikoNo ratings yet
- Control Costs: MehsansaeedDocument15 pagesControl Costs: MehsansaeedShahbaz Khan NiaziNo ratings yet
- MEASUREMENT BASES and Other Important RemindersDocument2 pagesMEASUREMENT BASES and Other Important RemindersShaina Monique RangasanNo ratings yet
- Robo AdvisorsDocument2 pagesRobo AdvisorsAn NguyễnNo ratings yet
- Fund Type Overview - McGillDocument13 pagesFund Type Overview - McGillSaiyan IslamNo ratings yet
- الجيالى تكاليف Ch 15 DrDocument5 pagesالجيالى تكاليف Ch 15 DrAhmed TarekNo ratings yet
- Fiscal Monitor: Database of Country Fiscal Measures in Response To The COVID-19 PandemicDocument20 pagesFiscal Monitor: Database of Country Fiscal Measures in Response To The COVID-19 PandemicCytheria JiangNo ratings yet
- All PMP ChartsDocument1 pageAll PMP Chartsgummies6011No ratings yet
- White Paper Consumption Based ABCMDocument8 pagesWhite Paper Consumption Based ABCMMaribet RodríguezNo ratings yet
- Chapter 2Document8 pagesChapter 2karen perrerasNo ratings yet
- ROI IT StartupDocument49 pagesROI IT Startupabdullahsaleem91No ratings yet
- Uts Akling (Gri 2) - Gresita Mahar K 252Document10 pagesUts Akling (Gri 2) - Gresita Mahar K 252aisyahnabillapp02No ratings yet
- Value For Money AnalysisDocument15 pagesValue For Money AnalysisMahamoudou TouréNo ratings yet
- Payment Vs Bid CostDocument12 pagesPayment Vs Bid Costkaren dejoNo ratings yet
- A300396730 - 18770 - 29 - 2021 - CA1 FINM551 2151 2152 2153 2155 Term21221Document13 pagesA300396730 - 18770 - 29 - 2021 - CA1 FINM551 2151 2152 2153 2155 Term21221Ankit pattnaikNo ratings yet
- KDD 2020 阿里妈妈 - DCAF - A Dynamic Computation Allocation Framework for Online Serving SystemDocument8 pagesKDD 2020 阿里妈妈 - DCAF - A Dynamic Computation Allocation Framework for Online Serving SystemMYNo ratings yet
- The Value of Big Data in TelcoDocument3 pagesThe Value of Big Data in Telcosamana residenceNo ratings yet
- Annex III-Price ScheduleDocument2 pagesAnnex III-Price ScheduleManoj MaharjanNo ratings yet
- Cost Accounting & ControlDocument4 pagesCost Accounting & ControlQueeny CuraNo ratings yet
- Part 1A DHS BPMN 2.0 Conventions Standards v2.0 (Names Redacted) (Final SB) PDFDocument15 pagesPart 1A DHS BPMN 2.0 Conventions Standards v2.0 (Names Redacted) (Final SB) PDFRahul AryanNo ratings yet
- UntitledDocument13 pagesUntitledBaldwin AuxNo ratings yet
- Lecture 2 Databases2Document2 pagesLecture 2 Databases2Jad ZoghaibNo ratings yet
- CIA CIA3 BookOnline SU14 OutlineDocument26 pagesCIA CIA3 BookOnline SU14 OutlineSalmanNo ratings yet
- Session 3: Computer Assisted Audit: Tools and Techniques (Caatts)Document15 pagesSession 3: Computer Assisted Audit: Tools and Techniques (Caatts)DENo ratings yet
- MBP InsuranceDocument22 pagesMBP InsuranceMurtuza SadikotNo ratings yet
- Celaws Midterm ModulesDocument30 pagesCelaws Midterm ModulesAnnika MalonzoNo ratings yet
- Performance ManagementDocument10 pagesPerformance ManagementsuryapdlNo ratings yet
- Concepts and Data Model - SAP DocumentationDocument2 pagesConcepts and Data Model - SAP Documentationatanu mohantyNo ratings yet
- BOARD in Ray Way: Case StudyDocument3 pagesBOARD in Ray Way: Case StudyNina_C_ALNo ratings yet
- 2019 - Marriott Budget Guidlines 2019-09-23Document5 pages2019 - Marriott Budget Guidlines 2019-09-23Karim NaitdouchNo ratings yet
- Marketing Strategy 0212Document1 pageMarketing Strategy 0212ditta.ocNo ratings yet
- Key Issues - WarroomDocument4 pagesKey Issues - WarroomXolaniHlatshwayoNo ratings yet
- MEASUREMENT BASES and Other Important RemindersDocument2 pagesMEASUREMENT BASES and Other Important RemindersShaina Monique RangasanNo ratings yet
- Corporate Accounts Checklist 2017 - 05042017Document1 pageCorporate Accounts Checklist 2017 - 05042017franchesca marie t. uyNo ratings yet
- FAR210 MFRS116 PPE - Oct23Document28 pagesFAR210 MFRS116 PPE - Oct23Nur Alya DamiaNo ratings yet
- Section - 1 - AnalyzeDocument10 pagesSection - 1 - AnalyzemoorthyNo ratings yet
- 19m (12-00) Develop The Audit Program - Costs and ExpensesDocument2 pages19m (12-00) Develop The Audit Program - Costs and ExpensesAnh Tuấn TrầnNo ratings yet
- Superannuation Notes General InsuranceDocument5 pagesSuperannuation Notes General InsuranceAvadrozeNo ratings yet
- MI CH 1. The Fundamental of CostingDocument4 pagesMI CH 1. The Fundamental of CostingPonkoj Sarker TutulNo ratings yet
- Finding Budget F Lexibility - or Not:: The Impact of Fixed and Variable CostDocument5 pagesFinding Budget F Lexibility - or Not:: The Impact of Fixed and Variable CostCristian Camilo Garcia BetancurNo ratings yet
- 55910bosintermay20 p3 cp12Document50 pages55910bosintermay20 p3 cp12Anand PandeyNo ratings yet
- Implementing Public Bicycle Share (PBS) Systems in India: - Ashwin Prabhu & Ranjana MenonDocument25 pagesImplementing Public Bicycle Share (PBS) Systems in India: - Ashwin Prabhu & Ranjana MenonAshish AggarwalNo ratings yet
- ManAcc S05 SlidesDocument88 pagesManAcc S05 SlidesNina Selin OZSEKERCINo ratings yet
- HBZ Criteria Matrix-Council Scoring2Document1 pageHBZ Criteria Matrix-Council Scoring2Derek YoungNo ratings yet
- Section CDocument20 pagesSection CSANJAY SOLANKINo ratings yet
- Service CostingDocument60 pagesService Costingpranoti tardeNo ratings yet
- Latest SeviceDocument60 pagesLatest SeviceNaga ChandraNo ratings yet
- 4.service & Operating CostingDocument60 pages4.service & Operating CostingNaga ChandraNo ratings yet
- Factsheet IAS19 Employee BenefitsDocument15 pagesFactsheet IAS19 Employee BenefitsHamza Fath-dinNo ratings yet
- Oracle IFRS 17 BlueprintDocument4 pagesOracle IFRS 17 BlueprintMegan CastilloNo ratings yet
- Management of Project and Consortium: 5.3. Plan For SustainabilityDocument5 pagesManagement of Project and Consortium: 5.3. Plan For SustainabilitySunny PardeshiNo ratings yet
- Transmission Loss Allocation Part I-SingleDocument6 pagesTransmission Loss Allocation Part I-SingleNorway ChadNo ratings yet
- Monitoring Report For Faculty Online Classes Bachelor of Science in AccountancyDocument8 pagesMonitoring Report For Faculty Online Classes Bachelor of Science in AccountancyJay AnnNo ratings yet
- Management Accounting Strategy Study Resource for CIMA Students: CIMA Study ResourcesFrom EverandManagement Accounting Strategy Study Resource for CIMA Students: CIMA Study ResourcesNo ratings yet
- AAFP Letter To Domestic Policy Council 6-10-2020Document3 pagesAAFP Letter To Domestic Policy Council 6-10-2020iggybauNo ratings yet
- Bostock v. Clayton County, Georgia DecisionDocument119 pagesBostock v. Clayton County, Georgia DecisionNational Content DeskNo ratings yet
- Boston Mayor Executive Order 6-12-2020Document3 pagesBoston Mayor Executive Order 6-12-2020iggybauNo ratings yet
- A Bill: in The House of RepresentativesDocument2 pagesA Bill: in The House of RepresentativesiggybauNo ratings yet
- HR 6437 Coronavirus Immigrant Families Protection AcfDocument16 pagesHR 6437 Coronavirus Immigrant Families Protection AcfiggybauNo ratings yet
- S 3609 Coronavirus Immigrant Families Protection ActDocument17 pagesS 3609 Coronavirus Immigrant Families Protection ActiggybauNo ratings yet
- S 3721 COVID-19 Racial and Ethnic Disparities Task ForceDocument11 pagesS 3721 COVID-19 Racial and Ethnic Disparities Task ForceiggybauNo ratings yet
- SF StayHome MultiLang Poster 8.5x11 032620Document1 pageSF StayHome MultiLang Poster 8.5x11 032620iggybauNo ratings yet
- HR 6763 COVID-19 Racial and Ethnic Disparities Task ForceDocument11 pagesHR 6763 COVID-19 Racial and Ethnic Disparities Task ForceiggybauNo ratings yet
- NCAPIP Recommendations For Culturally and Linguistically Appropriate Contact Tracing May 2020Document23 pagesNCAPIP Recommendations For Culturally and Linguistically Appropriate Contact Tracing May 2020iggybauNo ratings yet
- Doe v. Trump Denial of All Writs Injunction Against April 2020 Presidential ProclamationDocument9 pagesDoe v. Trump Denial of All Writs Injunction Against April 2020 Presidential ProclamationiggybauNo ratings yet
- HR 6585 Equitable Data Collection COVID-19Document18 pagesHR 6585 Equitable Data Collection COVID-19iggybauNo ratings yet
- Covid-19 Data For Asians Updated 4-21-2020Document2 pagesCovid-19 Data For Asians Updated 4-21-2020iggybauNo ratings yet
- Doe v. Trump Preliminary Injunction Against Proclamation Requiring Private Health InsuranceDocument48 pagesDoe v. Trump Preliminary Injunction Against Proclamation Requiring Private Health InsuranceiggybauNo ratings yet
- Exposing Corporate Profiteering From Immigration Detention and Enforcement September 2018Document16 pagesExposing Corporate Profiteering From Immigration Detention and Enforcement September 2018iggybauNo ratings yet
- CDC Covid-19 Report FormDocument2 pagesCDC Covid-19 Report FormiggybauNo ratings yet
- MACRA Quality Payment Program Year 2 Final RuleDocument662 pagesMACRA Quality Payment Program Year 2 Final RuleiggybauNo ratings yet
- 01 NIC Annual Report 64-65Document84 pages01 NIC Annual Report 64-65Ronit KcNo ratings yet
- Exchange Rate Regimes: Classification and ConsequencesDocument22 pagesExchange Rate Regimes: Classification and ConsequencesMuhammad Arslan UsmanNo ratings yet
- Venture Capital - V SemDocument65 pagesVenture Capital - V SemPratik RambhiaNo ratings yet
- Bachelor ThesisDocument41 pagesBachelor ThesisRoberto MachadoNo ratings yet
- Afm - ADocument2 pagesAfm - Asunru24No ratings yet
- Contemporary Issues in Banking Sector in BangladeshDocument8 pagesContemporary Issues in Banking Sector in Bangladeshangel100% (5)
- Pricing of ServicesDocument30 pagesPricing of ServicesAnand VANo ratings yet
- Industrial Training Report Citigroup Transaction Services (M) SDN BHDDocument27 pagesIndustrial Training Report Citigroup Transaction Services (M) SDN BHDhisyamstarkNo ratings yet
- Amity School of Business: BBA, Semester 3 Financial Management 1Document44 pagesAmity School of Business: BBA, Semester 3 Financial Management 1Orange NoidaNo ratings yet
- Description: Tags: 0809CODTechRefVol2Sec4EditsDocument35 pagesDescription: Tags: 0809CODTechRefVol2Sec4Editsanon-670649No ratings yet
- Financial Analysis of Ogdcl and SSGCLDocument24 pagesFinancial Analysis of Ogdcl and SSGCLShahid MehmoodNo ratings yet
- Atlas Development and Support Services - Listing Statement PDFDocument134 pagesAtlas Development and Support Services - Listing Statement PDFKen AlwalaNo ratings yet
- Amended Salary Loan GuidelinesDocument43 pagesAmended Salary Loan GuidelinesKrizia Iris De MesaNo ratings yet
- MMFSL Published PDFDocument290 pagesMMFSL Published PDFDominic SavioNo ratings yet
- L&T Long Term Infrastructure Bond Tranche 1 Application FormDocument8 pagesL&T Long Term Infrastructure Bond Tranche 1 Application FormPrajna CapitalNo ratings yet
- Bad DebtDocument5 pagesBad DebtlamorlaNo ratings yet
- BMR Case StudyDocument92 pagesBMR Case StudychamatkaribabaNo ratings yet
- Prepayments LiabilitesDocument1 pagePrepayments LiabilitesKrishele G. GotejerNo ratings yet
- Recto Law and Maceda LawDocument3 pagesRecto Law and Maceda LawdhadhagladysNo ratings yet
- Viking RaidDocument31 pagesViking RaidAnonymous 61kSe1MNo ratings yet
- East Asian Miracle PDFDocument11 pagesEast Asian Miracle PDFDinesh KumarNo ratings yet
- INVESTMENT AND COMPETITION LAW - Unit 2Document62 pagesINVESTMENT AND COMPETITION LAW - Unit 2saif aliNo ratings yet
- 02 Heirs of Fe Tan Uy vs. International Exchange BankDocument15 pages02 Heirs of Fe Tan Uy vs. International Exchange BankD Del SalNo ratings yet