Professional Documents
Culture Documents
Full Issue
Uploaded by
RioHasibuanCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Full Issue
Uploaded by
RioHasibuanCopyright:
Available Formats
Unless otherwise noted, the publisher, which is the American Speech-Language-
Hearing Association (ASHA), holds the copyright on all materials published in
Perspectives on Neurophysiology and Neurogenic Speech and Language
Disorders, both as a compilation and as individual articles. Please see Rights
and Permissions for terms and conditions of use of Perspectives content:
http://journals.asha.org/perspectives/terms.dtl
Vol. 24, No. 3, pp. 74117
June 2014
In This Issue
Guest Editors Column by Candace Vickers..........................................................................7677
Tutorial for Verb Network Strengthening Treatment (VNeST): Detailed Description of the
Treatment Protocol with Corresponding Theoretical Rationale by Lisa A. Edmonds...............7888
Facilitating Life Participation in Severe Aphasia With Limited Treatment Time
by Jacqueline Hinckley.........................................................................................................8999
Maximizing Outcomes in Group Treatment of Aphasia: Lessons Learned From a
Community-Based Center by Darlene Williamson.............................................................100105
Communication Recovery Groups for Persons with Aphasia: A Replicable Program
for Medical and University Settings by Candace Vickers and Darla Hagge.........................106113
Alternative Service Delivery Model: A Group Communication Training Series for
Partners of Persons with Aphasia by Darla Hagge.............................................................114117
74
Downloaded From: http://sig2perspectives.pubs.asha.org/pdfaccess.ashx?url=/data/journals/ashannsld/930947/ on 09/19/2017
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
Perspectives on Neurophysiology and Neurogenic Speech and Language Disorders is a member publication
for affiliates of American Speech-Language-Hearing Association Special Interest Group 2, Neurophysiology
and Neurogenic Speech and Language Disorders. Planned publication months are January, April, June, and
October. Affiliates of any of ASHAs 18 SIGs have access to read all SIG Perspectives. To learn more about
joining a SIG, visit http://www.asha.org/SIG/join/. Contact Perspectives at sigs@asha.org.
Disclaimer of warranty: The views expressed and products mentioned in this publication may not reflect
the position or views of the American Speech-Language-Hearing Association or its staff. As publisher, the
American Speech-Language-Hearing Association does not warrant or guarantee the accuracy, completeness,
availability, merchantability, fitness for a particular purpose, or noninfringement of the content and
disclaims responsibility for any damages arising out of its use. Advertising: Acceptance of advertising does
not imply ASHAs endorsement of any product, nor does ASHA accept responsibility for the accuracy of
statements by advertisers. ASHA reserves the right to reject any advertisement and will not publish
advertisements that are inconsistent with its professional standards.
Vol. 24, No. 3, June 2014
SIG 2 Editor: Michael de Riesthal
SIG 2 2014 Editorial Review Board Members:
Angela Ciccia Tepanta Fossett Gina Griffiths Amy Krantz Shannon Mauszycki Peter Meulenbroek
Katie Ross Julie Wambaugh
SIG 2 CE Content Manager: Amanda Hereford
SIG 2 2014 Coordinating Committee: Carole Roth, SIG Coordinator Mary H. Purdy, Associate Coordinator
Michael de Riesthal, Perspectives Editor Gloriajean Wallace Sarah Wallace Monica Sampson, ASHA SIG 2
Ex Officio
ASHA Board of Directors Board Liaisons: Donna Fisher Smiley, Vice President for Audiology Practice
Gail J. Richard, Vice President for Speech-Language Pathology Practice
ASHA Production Editor: Victoria Davis
ASHA Advertising Sales: Pamela J. Leppin
ASHA Board of Directors: Elizabeth S. McCrea, President Judith L. Page, President-Elect Patricia A.
Prelock, Immediate Past President Donna Fisher Smiley, Vice President for Audiology Practice Perry F.
Flynn, Speech-Language Pathology Advisory Council Chair Wayne A. Foster, Audiology Advisory Council
Chair Howard Goldstein, Vice President for Science and Research Carlin F. Hageman, National Student
Speech Language Hearing Association (NSSLHA) National Advisor Carolyn W. Higdon, Vice President for
Finance Barbara J. Moore, Vice President for Planning Robert E. Novak, Vice President for Standards
and Ethics in Audiology Gail J. Richard, Vice President for Speech-Language Pathology Practice Shari B.
Robertson, Vice President for Academic Affairs in Speech-Language Pathology Theresa H. Rodgers, Vice
President for Government Relations and Public Policy Barbara K. Cone, Vice President for Academic Affairs
in Audiology Lissa A. Power-deFur, Vice President for Standards and Ethics in Speech-Language Pathology
Arlene A. Pietranton, Chief Executive Officer (ex officio to the Board of Directors)
75
Downloaded From: http://sig2perspectives.pubs.asha.org/pdfaccess.ashx?url=/data/journals/ashannsld/930947/ on 09/19/2017
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
We conclude with Darla Hagges description of an alternative service delivery model for a
six week communication training series. Partners of persons with aphasia attended the series
learning communication strategies for PWA and experiencing peer support while their family
members with aphasia attended conversation groups which were facilitated by trained volunteers
and graduate students.
All articles in this edition were written with the awareness that SLPs across the United
States are under more constraints than ever while they try to bring about tangible results and
improvement for persons with aphasia across the spectrum of care. We hope clinicians will find
useful ideas that help to expand service to PWA which can be applied in their own settings.
References
Edmonds, L. A., & Babb, M. (2011). Effect of verb network strengthening treatment in moderate-to-severe
aphasia. American Journal of Speech-Language Pathology, 20, 131145.
Leach, E., Cornwell, P., Fleming, J., & Haines, T. (2010). Patient-centered goal setting in a subacute
rehabilitation setting. Disability and Rehabilitation, 32, 159172.
Kagan, A., Black, S., Duchan, J., Simmons-Mackie, N., & Square, P. (2001) Training volunteers as
conversation partners using Supported conversation for adults with aphasia (SCA): A controlled trial.
Journal of Speech, Language and Hearing Research, 44, 624638.
Rowden-Racette, K. (2013, September 01). In the limelight: Guides for the long journey back. The ASHA Leader.
77
Downloaded From: http://sig2perspectives.pubs.asha.org/pdfaccess.ashx?url=/data/journals/ashannsld/930947/ on 09/19/2017
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
The VNeST protocol applies this theory by requiring participants to produce diverse scenarios
related to trained verbs (e.g., a nurse weighs a patient, a cashier weighs produce, a jeweler weighs
gold, a veterinarian weighs a puppy), which potentially promotes spreading activation to untrained
neurological networks, thereby facilitating generalized word retrieval in sentences and discourse.
With increased availability of words, persons with aphasia can potentially communicate their ideas
with more ease and/or specificity. Additionally, a verbs syntactic frame (composed of the verbs
and its arguments) is also activated and potentially strengthened during VNeST, which could aid
in sentence construction. Further, the repeated selection of subject/agents and object/patients
in relation to trained verbs involves mapping thematic role information onto syntactic argument
structure, which can be impaired in persons with aphasia (e.g., Webster, Franklin, & Howard,
2004).
Participants
It is beyond the scope of this article to provide a comprehensive review of VNeST studies.
However, a few pertinent details regarding participant outcomes are provided (see original articles
for more information). Three studies investigated VNeST in 17 people with aphasia (10 male)
(Edmonds & Babb, 2011; Edmonds et al., 2014; Edmonds et al., 2009), and one study provided
a computerized version of VNeST (VNeST-C) via teletherapy to two males (Furnas & Edmonds,
2014). All participants were at the chronic stage of aphasia ( 9 months) and most had moderately
severe aphasia. Two participants had severe aphasia (Edmonds & Babb, 2011). Five participants
were diagnosed with anomic aphasia (all mild), 5 with conduction aphasia (one with substantial
jargon), 4 with transcortical motor aphasia, 2 with Brocas aphasia (both severe), and 1 with
Wernickes aphasia. The participants who received VNeST-C had moderate-severe Brocas aphasia
with mild to moderate apraxia of speech (AOS) and mild anomic aphasia with moderate-severe
AOS.
Overall, there has been replicated improvement and generalization of lexical retrieval
abilities in confrontation naming of nouns and verbs, sentence production and discourse, as well
as clinically significant improvement on the Western Aphasia Battery (WAB; Kertesz, 1982, 2006).
Further, significant improvement on reports of functional communication from family members
(on the Communicative Effectiveness Index [CETI; Lomas et al., 1989]) has been reported in 11
of 11 participants for whom we have those data. While every participant did not improve on all
outcome measures, all exhibited improvement and generalization to a number of outcome measures.
Thus, it is reasonable to suggest that VNeST may be appropriate for participants who generally
fit within the parameters of these participants. However, keep in mind the following: (a) We have
only tested one person with Wernickes aphasia (who also had a severe verb impairment). Her
improvement was encouraging, with improvements on the WAB, verb and noun naming, informative
and complete utterances in discourse, and the CETI (per her husbands ratings; Edmonds et al.,
2014); (b) We have excluded people with greater than mild to moderate AOS except in the
computerized VNeST study, where typing was included as part of the treatment. Even though
VNesST-C participants improved in spoken and written modalities, we cannot make generalized
clinical recommendations at this time; and (c) Diagnosis of global aphasia has also been an
exclusionary variable, because VNeST requires better comprehension than is often seen in persons
with global aphasia.
Dosage
In all VNeST studies, we have provided treatment 2 times/week for 1.52 hours per session
(though VNeST-C was delivered 3 times/week for 2 hours each session). In our most recent study,
we controlled dosage to 10 weeks of treatment with 10 verbs for approximately 3.5 hours of
treatment per week (35 hours total). The group of 11 participants exhibited improvement across
outcome measures (Edmonds et al., 2014) and examination of the slopes of improvement on
sentence probes administered throughout treatment revealed that participants did not plateau
79
Downloaded From: http://sig2perspectives.pubs.asha.org/pdfaccess.ashx?url=/data/journals/ashannsld/930947/ on 09/19/2017
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
Tutorial for Verb Network Strengthening Treatment (VNeST):
Detailed Description of the Treatment Protocol with
Corresponding Theoretical Rationale
Lisa A. Edmonds
Department of Communication Sciences and Disorders, Teachers College, Columbia University
New York, NY
Financial Disclosure: Lisa A. Edmonds is an Associate Professor at Columbia University.
Nonfinancial Disclosure: Lisa A. Edmonds has previously published in the subject area.
Abstract
Verb Network Strengthening Treatment (VNeST) is a theoretically motivated aphasia
treatment that has resulted in promising generalization to untrained sentences and
discourse in persons with aphasia. As with all speech and language therapies, it is critical
that clinicians understand the theoretical motivation behind VNeSTs protocol in order to
make informed decisions during provision of the treatment. This article provides a detailed
VNeST tutorial, including characteristics of participants who might be suitable, dosage
information, and detailed instructions for each treatment step, including rationale, cueing
guidelines, and frequently asked questions. Further guidance is provided regarding verb
selection, and a score sheet is included for easy recording of responses and cueing levels.
Aphasia is an acquired language disorder, primarily caused by stroke, which affects
language production and comprehension. Anomia, or difficulty retrieving words, is a pervasive
symptom of aphasia that can negatively impact basic communication functions such as interacting
with family and co-workers, talking on the phone, and expressing needs, wants, and emotions.
A fundamental challenge in aphasia treatment is to achieve improved lexical retrieval in sentences
and discourse, particularly for untrained words in untrained language contexts (i.e., generalization).
Verb Network Strengthening Treatment (VNeST) is a theoretically motivated aphasia treatment
that has resulted in promising generalization to sentences and discourse in persons with aphasia
(Edmonds & Babb, 2011; Edmonds, Nadeau, & Kiran, 2009; Edmonds, Mammino & Ojeda, 2014;
Furnas & Edmonds, 2014). There are a number of treatment steps in VNeST, and each has a
specific purpose with regard to the treatments theoretical foundation. Therefore, the purpose of
this article is to provide clinicians and researchers with a tutorial that details the logistics and
rationale of each treatment step. Suggestions regarding selection and development of treatment
and testing materials are also provided.
VNeST is based on theories of event memory that conceive of neurological networks of verbs
and related nouns (i.e., verb networks) that wire together through use and world knowledge (e.g.,
Ferretti, McRae, & Hatherell, 2001). The nouns related to the verbs in these proposed networks
are called thematic roles, because they relate to the verb with regards to who is performing the
action (agent), the receiver of the action (patient), the location of the action, and the instrument of
the action (e.g., The plumber [agent] is fixing [verb] the sink [patient] in the bathroom [location] with
a wrench [instrument]). Research has indicated that verbs and their related thematic roles are
neurally co-activated such that agents and patients prime/facilitate activation of related verbs
(Edmonds & Mizrahi, 2011; McRae, Hare, & Ferretti, 2005) and vice versa (Edmonds & Mizrahi,
2011; Ferretti, McRae, & Hatherell, 2001). There is also bidirectional neural co-activation between
verbs (e.g., slicing) and their instruments (e.g., knife) (Ferretti, McRae, & Hatherell, 2001; McRae
et al., 2005) and priming from locations (e.g., restaurant) to related verbs (e.g., eating; Ferretti
et al., 2001).
78
Downloaded From: http://sig2perspectives.pubs.asha.org/pdfaccess.ashx?url=/data/journals/ashannsld/930947/ on 09/19/2017
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
read the words, or read the words for them, as needed. Fade out reading assistance as they
improve. Once they choose the correct word, they can put it under the who or what card (see
Figure 1).
If the participant chooses a foil, (e.g., dentist) say, Lets think about what it means to drive.
Now lets think about a dentist. Is it a dentists job to drive? Typically, people will acknowledge the
problem. If the participant does not understand, then explain that driving involves going from one
place to another in a car or other vehicle. Then ask if that is what a dentist does for his/her job.
We do not discuss what the foil (dentist) does, as this involves training another verb and can cause
some confusion, especially if the participant is already having difficulty.
You can alternate between maximal and minimal cues. For example, a maximal cue might
be required for the first response for a verb, and that might generate ideas so that the participant
may only need minimal cues for the other pairs (or have independent responses). The goal is to
encourage independent responses but to provide sufficient support when needed. However, all cues
should require that the participant choose a correct response rather than being given a response.
Once an agent is chosen, request a corresponding patient (e.g., If they said soldier, the
patient might be tank). Participants are encouraged to provide at least one personal pair (e.g.,
dad/boat for drive), and responses can change from week to week. (Early VNeST studies requested
a list of agents or patients and then the corresponding noun, but it is more natural to generate one
scenario at a time). Elicitation of the corresponding noun is relatively easy for participants, since
the possibilities are constrained. Once it is established that, for example, the driver is a farmer,
then a patient like tractor, or pickup truck comes much easier. If the participant cannot retrieve a
patient independently, provide cues as described above. Once you have one pair, you will repeat
Step 1 until 3 to 4 pairs of words are generated.
To Keep in Mind During Step 1.
1. A verbs meaning is somewhat loose (relative to nouns) (Black and Chiat, 2003), and
the variability in meaning often reflects different thematic role combinations. Thus, it is
important to encourage participants to generate multiple pairs of agents and patients
(e.g., carpenter-lumber, chef-sugar, seamstress-fabric for measure) to comprehensively
activate a verbs multi-dimensional meaning (i.e., semantic representation). It may be
necessary to explicitly elicit variety in responses. For example, if the participant only
discusses family members, say something like You have mentioned a lot of family members,
which is great, but lets think of some other people who might drive, bake, etc. Then cue
as needed.
2. Make sure participants produce at least one personally relevant scenario to activate
their own memories and knowledge of a verb/event. For example, one participant said
that her husband (and she) could chop a banjo. This is a banjo-playing technique
that was relevant to her and would not have been clinician-generated, and it meant a
lot to her and her husband that she was able to express this idea independently.
Frequently Asked Questions about Step 1. Do I always have to start with the agent
(who)? No. In some cases asking for the patient first can be advantageous because some verbs
lend themselves to more patients, or the patients are easier to retrieve. For example, it is easily
understood that cars are driven. Once that is established as a patient, it is easy to prompt a
familiar agent by asking, Who in your family drives? or more specifically Who drove you here
today? Such adaptations are sometimes needed when participants are first learning the protocol
or for participants who have more challenging linguistic or cognitive limitations. Typically,
participants begin to understand the objective and will generate more diverse responses with less
cueing over time.
What if a participant has difficulty with maximal cueing? Maximal cueing can be adapted
by reducing the number of choices from four to two (one foil and one correct response). Further,
82
Downloaded From: http://sig2perspectives.pubs.asha.org/pdfaccess.ashx?url=/data/journals/ashannsld/930947/ on 09/19/2017
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
before 10 weeks. Thus, while there is potential variability regarding length of treatment, most
participants should show a reasonable amount of recovery by 10 weeks (see Edmonds and Babb,
2011 with severe participants).
Materials
Treatment Materials
VNeST was designed to be low tech, so that it could be administered in any setting. At
minimum, all that is needed is a pen and paper. However, materials can be prepared ahead of time
on cardstock (we cut index cards into thirds) for repeated use or use a clipboard-sized erasable
white board to write responses. The cards provide the benefit of being manipulable, but a whiteboard
or sheets of paper should work just as well.
There are a variety of verbs that can be used in treatment. One basic requirement is that
the verb is a two-place verb (takes 2 arguments; e.g., a subject and object; The waiter folds the
napkin.). Thus, one-place verbs, which only require one argument (e.g., The boy swims.) are not
recommended. However, our research has shown that training two-place verbs often results in
improvement to one-place verbs, so one-place verbs and/or sentence production can be evaluated
as a generalization measure. See Appendix A for suggestions on verb selection.
Outcome Measures
The outcome measures chosen to evaluate improvement should reflect a participants
treatment goals. Lexical retrieval abilities across a range of tasks, including confrontation naming
for nouns and verbs, sentence production, and discourse should be examined. You can also
evaluate aphasia severity (e.g., WAB-R), sentence comprehension, and functional communication.
The sentence probe pictures used in VNeST studies are not currently available. However, we have
also used the Northwestern Assessment of Verbs and Sentences (NAVS; Thompson, 2011) to
evaluate sentence production and comprehension as well as verb naming. The NAVS can be found
online (Flintbox, 2010). For noun naming, the Philadelphia Naming Test (PNT) is downloadable
free-of-charge online (Moss Rehabilitation Research Institute, 2013), complete with answer sheets
and scoring information. There are many ways to analyze discourse. One option is the stimuli
and analysis methods from Nicholas and Brookshire (1993), which can be found on the ASHA
website. In addition to the outcome variables described in Nicholas and Brookshire, we have
examined complete utterances, which consider both the completeness (contains a subject, verb,
and object [when required]) and relevance (relevant to the topic) of utterances (see Edmonds et al.,
2009; Edmonds et al., 2014). Evaluating the relative improvement of relevance and completeness
is also informative.
Treatment Protocol
See Appendix B for an example of a VNeST answer sheet.
Step 1. Generation of Multiple Scenarios Around the Trained Verb
Detailed Instructions. Set down the cards with the words who and what written on
them (see Figure 1). Point to each card and tell the participant that these cards say who and
what. Then place the card with the verb written on it between the who and what cards and
ask Who can/might (verb) something/someone? In this example, we will use the verb drive. If
the participant does not understand the word who, then you can say, Can you think of a person
who drives something? If the participant is able to independently produce a plausible response
(e.g., chauffeur, my wife, taxi drive), write the word on a blank card and set it under the who card
(see Figure 1).
80
Downloaded From: http://sig2perspectives.pubs.asha.org/pdfaccess.ashx?url=/data/journals/ashannsld/930947/ on 09/19/2017
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
Move on to the Next Verb
After completion of all steps for one verb, move to another verb. We train 10 verbs. Once we
train all 10 verbs, we cycle through them again. It is ideal to get through all 10 verbs in one week,
if possible.
Treatment Settings
VNeST has only been evaluated in outpatient sessions with trained clinicians. We have not
trained family members or volunteers to conduct VNeST; therefore, we do not have information
on how participants respond in these cases. Provision of VNeST requires an understanding of the
treatments principles, including feedback. Thus, if family members are trained to do VNeST, they
should be highly involved in treatment sessions with the clinicians first. The information in this
article may be helpful for home use/practice and training of volunteers or family members as well.
References
Black, M., & Chiat, S. (2003). Nounverb dissociations: A multi-faceted phenomenon. Journal of
Neurolinguistics, 16, 231250.
Edmonds, L. A., & Babb, M. (2011). Effect of Verb Network Strengthening Treatment in moderate-to-severe
aphasia. American Journal of Speech-Language Pathology, 20, 131145.
Edmonds, L. A., & Mizrahi, S. (2011). Online priming of verbs and thematic roles in younger and older
adults. Aphasiology, 25(12), 14881506.
Edmonds, L. A., Mammino, K., & Ojeda, J. (2014). Effect of Verb Network Strengthening Treatment (VNeST)
in persons with aphasia: Extension and replication of previous findings. American Journal of Speech
Language Pathology. doi:10.1044/2014_AJSLP-13-0098
Edmonds, L. A., Nadeau, S., & Kiran, S. (2009). Effect of Verb Network Strengthening Treatment (VNeST) on
lexical retrieval of content words in sentences in persons with aphasia. Aphasiology, 23(3), 402424.
Ferretti, T. R., McRae, K., & Hatherell, A. (2001). Integrating verbs, situation schemas, and thematic role
concepts. Journal of Memory and Language, 44, 516547.
Flintbox. (2010). Northwestern assessment of verbs and sentences (NAVS). Retrieved from https://flintbox.
com/public/project/9299/
Furnas, D. W., & Edmonds, L. A. (2014). The effect of Computer Verb Network Strengthening Treatment on
lexical retrieval in aphasia. Aphasiology, 28, 401420.
Kertesz, A. (1982). Western Aphasia Battery. Austin, TX: Pro-ed.
Kertesz, A. (2006). Western aphasia batteryRevised. Austin, TX: Pro-ed.
Lomas, J., Pickard, L., Bester, S., Elbard, H., Finlayson, A., & Zoghaib, C. (1989). The communicative
effectiveness index: Development and psychometric evaluation of a functional communication measure for
adults aphasia. Journal of Speech and Hearing Disorders, 54, 113124.
McRae, K., Hare, E., & Ferretti, T. R. (2005). A basis for generating expectancies for verbs from nouns.
Memory and Cognition, 33(7), 11741184.
Moss Rehabilitation Research Institute. (2013). Philadelphia naming test (PNT). Retrieved from http://www.
mrri.org/philadelphia-naming-test
Nicholas, L. E., & Brookshire, R. H. (1993). A system for quantifying the informativeness and efficiency of the
connected speech of adults with aphasia. Journal of Speech and Hearing Research, 36, 338350.
Rogalski, Y., Edmonds, L. A., Daly, V. R., & Gardner, M. J. (2013). Attentive Reading and Constrained
Summarization (ARCS) discourse treatment for anomia in two women with moderate-severe Wernickes type
aphasia. Aphasiology, 27, 12321251.
Thompson, C. K. (2011). The Argument Structure Production Test/The Northwestern Assessment of Verbs and
Sentences. Northwestern University.
Webster, J., Franklin, S., & Howard, D. (2004). Investigating the sub-processes involved in the production of
thematic structure: An analysis of four people with aphasia. Aphasiology, 18, 4768.
86
Downloaded From: http://sig2perspectives.pubs.asha.org/pdfaccess.ashx?url=/data/journals/ashannsld/930947/ on 09/19/2017
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
read the words, or read the words for them, as needed. Fade out reading assistance as they
improve. Once they choose the correct word, they can put it under the who or what card (see
Figure 1).
If the participant chooses a foil, (e.g., dentist) say, Lets think about what it means to drive.
Now lets think about a dentist. Is it a dentists job to drive? Typically, people will acknowledge the
problem. If the participant does not understand, then explain that driving involves going from one
place to another in a car or other vehicle. Then ask if that is what a dentist does for his/her job.
We do not discuss what the foil (dentist) does, as this involves training another verb and can cause
some confusion, especially if the participant is already having difficulty.
You can alternate between maximal and minimal cues. For example, a maximal cue might
be required for the first response for a verb, and that might generate ideas so that the participant
may only need minimal cues for the other pairs (or have independent responses). The goal is to
encourage independent responses but to provide sufficient support when needed. However, all cues
should require that the participant choose a correct response rather than being given a response.
Once an agent is chosen, request a corresponding patient (e.g., If they said soldier, the
patient might be tank). Participants are encouraged to provide at least one personal pair (e.g.,
dad/boat for drive), and responses can change from week to week. (Early VNeST studies requested
a list of agents or patients and then the corresponding noun, but it is more natural to generate one
scenario at a time). Elicitation of the corresponding noun is relatively easy for participants, since
the possibilities are constrained. Once it is established that, for example, the driver is a farmer,
then a patient like tractor, or pickup truck comes much easier. If the participant cannot retrieve a
patient independently, provide cues as described above. Once you have one pair, you will repeat
Step 1 until 3 to 4 pairs of words are generated.
To Keep in Mind During Step 1.
1. A verbs meaning is somewhat loose (relative to nouns) (Black and Chiat, 2003), and
the variability in meaning often reflects different thematic role combinations. Thus, it is
important to encourage participants to generate multiple pairs of agents and patients
(e.g., carpenter-lumber, chef-sugar, seamstress-fabric for measure) to comprehensively
activate a verbs multi-dimensional meaning (i.e., semantic representation). It may be
necessary to explicitly elicit variety in responses. For example, if the participant only
discusses family members, say something like You have mentioned a lot of family members,
which is great, but lets think of some other people who might drive, bake, etc. Then cue
as needed.
2. Make sure participants produce at least one personally relevant scenario to activate
their own memories and knowledge of a verb/event. For example, one participant said
that her husband (and she) could chop a banjo. This is a banjo-playing technique
that was relevant to her and would not have been clinician-generated, and it meant a
lot to her and her husband that she was able to express this idea independently.
Frequently Asked Questions about Step 1. Do I always have to start with the agent
(who)? No. In some cases asking for the patient first can be advantageous because some verbs
lend themselves to more patients, or the patients are easier to retrieve. For example, it is easily
understood that cars are driven. Once that is established as a patient, it is easy to prompt a
familiar agent by asking, Who in your family drives? or more specifically Who drove you here
today? Such adaptations are sometimes needed when participants are first learning the protocol
or for participants who have more challenging linguistic or cognitive limitations. Typically,
participants begin to understand the objective and will generate more diverse responses with less
cueing over time.
What if a participant has difficulty with maximal cueing? Maximal cueing can be adapted
by reducing the number of choices from four to two (one foil and one correct response). Further,
82
Downloaded From: http://sig2perspectives.pubs.asha.org/pdfaccess.ashx?url=/data/journals/ashannsld/930947/ on 09/19/2017
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
making the foil as obviously correct as possible will promote learning and success (e.g., Does your
husband drive? or Does a cat drive?). Over time foils can be added and diversified.
Can the participant write the responses on the cards rather than the clinician? Yes. We have
included writing for a number of participants. Participant 2 in Edmonds and Babb (2011) had
severely impaired spoken output, but her written output was notably better. Thus, we required her
to try to say her response first, and if it was not understood by the clinician (due largely to neologistic
output), then she wrote her response on a card. After she wrote it, she read it aloud (with assistance,
if needed). She improved in both spoken and written output (see Edmonds & Babb, 2011). With
computerized VNeST, participants spoke and then typed their responses. Both participants had
AOS, so working on speech and typing was motivational and functional, and both participants
showed improvements across modalities (see Furnas & Edmonds, 2014). Overall, including writing
during this step is motivating and engages multiple modalities. However, if the primary goal is
improved spoken output, then writing should come after the spoken response. Additionally, feedback
regarding the written output should not distract from the goals of Step 1 (semantic engagement
and lexical retrieval), unless writing is a primary goal. Thus, if spelling errors are made, simply
provide a written model of the word and allow the participant to copy it correctly rather than engaging
in detailed spelling training (e.g., phoneme to grapheme correspondence).
Can I provide phonemic cues to help participants produce a response ( e.g., Someone can
bake coo____ to elicit cookies?)? We have not provided phonemic cues in treatment, because we
want to maximally engage the semantic system during cueing.
What if someone makes a phonological error in their response? We do not address minor
errors or distortions that do not interfere with comprehension of a response. However, if a response
contains more problematic errors or is frustrating to the participant, we model the word and allow
up to three repetitions. For our research purposes, we never give visual, tactile, or other types of
cues. In a clinical setting, therapists should use their own judgment regarding the needs of their
participants.
Can I use pictures and ask questions about the picture rather than having the participant
generate words? This is not encouraged. Using pictures changes the underlying premise of VNeST.
Also, it may promote learning or association of correct responses rather than engaging semantic
searches to generate diverse scenarios. However, we have noticed self-monitoring limitations in
some participants that seem to limit generalization of increased lexical retrieval abilities to sentence
or discourse contexts (Edmonds et al., in preparation). Thus, it may be useful to introduce picture
description tasks (or other types of production tasks) to provide participants with opportunities to
monitor for pronoun usage, light verbs (e.g., do, make) or general terms (e.g., thing, stuff) in order to
replace such words with more specific terms(see Rogalski, Edmonds, Daly, & Gardner, 2013) for
more details about this approach). Since we have not conducted research on a self-monitoring
phase of VNeST, we cannot make specific recommendations as to how it would be integrated.
However, in most cases it would make sense to do this once lexical retrieval abilities have improved
with VNeST. Also, it would be important to use different pictures or tasks, so that participants do
not learn rote responses.
Step 2. The Participant Reads the Rriads Aloud (e.g., chef-chop-onion)
Detailed Instructions. The instructions for this step are fairly straight-forward. The
participant is instructed to read each agent-verb-patient triad aloud. Move the card with the verb
on it down for each triad, so that the words form a subject-verb-object order (e.g., dad-drive-boat,
chauffeur-drive-limousine). If the participant cannot read independently, do choral reading (read
together) or have the participant repeat each word. Point to each word during choral reading or
repetition. Typically participants improve in oral reading, so fade out cues as appropriate.
Objectives of Step 2. Step 1 promoted activation and retrieval of the individual words that
compose each scenario. Step 2 consolidates the scenarios and units through oral reading. This
83
Downloaded From: http://sig2perspectives.pubs.asha.org/pdfaccess.ashx?url=/data/journals/ashannsld/930947/ on 09/19/2017
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
step also reinforces basic canonical subject-verb-object word order, which may be helpful for
participants who have difficulty with basic sentence frame construction.
Frequently Asked Questions for Step 2
Should I require morphology and function words when they are reading the scenarios?
We do not require morphology, inflection or function words (e.g., The chef is chopping the onion.).
However, we do not discourage it if participants include it naturally. We do not train or focus on
morphology/functors because the goal of VNeST is to promote sufficient activation and lexical
retrieval of content words for inclusion in a sentence, and focusing on morphology/functors
(especially for persons with agrammatic aphasia) can detract attention from content words. However,
participants with relatively good sentence construction abilities at pre-treatment tend to include
some or all of the morphology and functor words in sentences during this step as they improve in
retrieval of content words.
Step 3
The participant chooses one scenario that he/she generated in Step 1 and answers three
wh-questions about it (where, when, why).
Detailed Instructions. Ask the participant to choose one scenario that he/she would
like to discuss in more detail. There are no restrictions about which they choose, though it is
recommended to encourage choosing different scenarios from week to week. Move the cards that
correspond to the scenario that the participant has chosen away from the other responses. Then
lay the where, why, and when cards down one at a time, and with each one, ask the corresponding
wh-question (e.g., Where does your dad drive a boat? Then, Why does your dad drive a boat in
the bay behind your house? and, When does your dad drive a boat in the bay behind your house to
relax?; see Figure 1). Asking questions in this way reinforces that each response should relate
logically to the whole scenario being developed. We have found that the best order of presentation
is where, why, and, when, because location is usually the easiest for participants to retrieve, and
it constrains the event so participants can logically provide a reason (why) and time (when) for
the event. The purpose of this step is to more comprehensively engage semantic, world and/or
autobiographical knowledge around the event scenarios. Thus, the focus is on plausibility of
responses rather than syntactic correctness.
If the participant has difficulty understanding the wh-questions, then clarify the meaning:
(a) Where does your dad drive a boat? What is the location or place? (b) Why does your dad drive
a boat? What is the purpose? (c) When does your dad drive a boat? Is it on a certain day, during a
certain season, at a certain time of day (morning, afternoon, night)?
Because there are various reasons participants may have difficulty with this step (e.g.,
comprehension issues, trouble with word retrieval, etc.), cue as needed to address the difficulty.
For example, if a person has trouble understanding where, then you could provide a forced choice
with a plausible and implausible option (e.g., Does your dad drive a boat in a lake or on a football
field?) It is our experience that even participants with relatively poor comprehension of wh-questions
at the beginning of treatment will improve appreciably on comprehension. Also, sometimes
responses to the why question can be overly general or repeated for every verb. If time allows (and
if it is appropriate for your participant, as this is a fairly sophisticated distinction), try to connect
the reason for the action to the action in a more specific way (e.g., if a participant says a chef slices
tomatoes for a sandwich because it his job, then you can reinforce that this is true. Then you ask,
But why do we slice a tomato for a sandwich? Why not just put a whole tomato on the sandwich
and eat it? This distinction is typically very helpful).
Once the responses have been laid down, the participant should read them aloud. The
responses in Figure 1 would be read as follows: Dad drive boat in the bay by our house to relax
on Saturdays. Provide reading cues as needed (see Step 2). Also, similar to Step 2, inclusion
of morphology/verb inflections is not required, though some participants do include it.
84
Downloaded From: http://sig2perspectives.pubs.asha.org/pdfaccess.ashx?url=/data/journals/ashannsld/930947/ on 09/19/2017
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
Table 2. Examples of Goals Typically Linked to Impairment-Focused Assessments.
Assessment Example of Typically Linked Goal ASHA NOMS Levels
Data
Spoken Improve ability to match single, personally Initial: Level 1 (unable to follow simple
Language relevant spoken words to pictures from directions, even with cues)
Comprehension: 45% accuracy to 90% accuracy in an array
of four pictures.
Word-Picture Goal: Level 2 (able to respond to simple
Matching = 45% words or phrases relevant to personal
needs given consistent, maximal cues)
Sentence-Picture
Matching = 0%
Reading: Improve ability to match single, personally Initial: Level 1 (attends to written words)
relevant written words to pictures from
45% accuracy to 90% accuracy in an array
of four pictures.
Written Word- Goal: Level 2 (able to read common
Picture words given consistent, maximal cues)
Matching = 45%
Goals that map very clearly and specifically to the evaluation data are encouraged and
even required by most rehabilitation companies and facilities within their documentation systems
to facilitate reimbursement. Undeniably, the links between the initial evaluation data to the goal
and desired outcomes in Table 2 are straightforward, and because of their clarity and obvious
measurement, they are likely to be reimbursed.
Will these goals affect Mrs. Cs participation in life? Although initial performance on
impairment-focused assessments, like standardized aphasia batteries, may be related to activity
participation, change on impairment-based assessments is not necessarily related to change on
activity participation (Ross & Wertz, 1999, 2002). So, focusing our intervention on a specific
impairment, like impaired auditory comprehension, does not necessarily mean that the client will
now be equipped to participate in life activities.
If we want to increase the likelihood that we will facilitate life participation in our clients,
we have to assess current opportunities for improved participation and focus our intervention
efforts on those. Lets use Mrs. Cs performance on the Communication Activities of Daily Living
(CADL-2; Holland, Frattali, & Fromm, 1999) as an example. This assessment uses role play to
sample a number of activities that are likely to be relevant to a person with aphasia residing in
the community, such as shopping, going to a doctors appointment, ordering from a restaurant
menu, understanding a bus schedule, and filling out forms. The CADL-2 overall score for Mrs. C
was 17%. Since points on most items of the CADL-2 are given based on producing a fully
communicative message regardless of modality, her overall score tells us that Mrs. C is not able
to use many communication modalities very effectively to perform in these role-play activities.
We can analyze specific items within the CADL-2 that correspond to specific activities as
an informal way to track communicative performance. For example, we can analyze Mrs. Cs
ability to provide personal information such as name, address, and medical information with
items #36 of the CADL-2. Assuming that providing personal information is a valuable activity for
Mrs. C, then this can be targeted with a treatment goal. ASHA NOMS levels can be assigned
based on the likelihood that Mrs. C will use spoken language expression or writing to convey the
personal information. Possible goals derived from activities assessed on the CADL-2 are shown in
Table 3.
91
Downloaded From: http://sig2perspectives.pubs.asha.org/pdfaccess.ashx?url=/data/journals/ashannsld/930947/ on 09/19/2017
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
Move on to the Next Verb
After completion of all steps for one verb, move to another verb. We train 10 verbs. Once we
train all 10 verbs, we cycle through them again. It is ideal to get through all 10 verbs in one week,
if possible.
Treatment Settings
VNeST has only been evaluated in outpatient sessions with trained clinicians. We have not
trained family members or volunteers to conduct VNeST; therefore, we do not have information
on how participants respond in these cases. Provision of VNeST requires an understanding of the
treatments principles, including feedback. Thus, if family members are trained to do VNeST, they
should be highly involved in treatment sessions with the clinicians first. The information in this
article may be helpful for home use/practice and training of volunteers or family members as well.
References
Black, M., & Chiat, S. (2003). Nounverb dissociations: A multi-faceted phenomenon. Journal of
Neurolinguistics, 16, 231250.
Edmonds, L. A., & Babb, M. (2011). Effect of Verb Network Strengthening Treatment in moderate-to-severe
aphasia. American Journal of Speech-Language Pathology, 20, 131145.
Edmonds, L. A., & Mizrahi, S. (2011). Online priming of verbs and thematic roles in younger and older
adults. Aphasiology, 25(12), 14881506.
Edmonds, L. A., Mammino, K., & Ojeda, J. (2014). Effect of Verb Network Strengthening Treatment (VNeST)
in persons with aphasia: Extension and replication of previous findings. American Journal of Speech
Language Pathology. doi:10.1044/2014_AJSLP-13-0098
Edmonds, L. A., Nadeau, S., & Kiran, S. (2009). Effect of Verb Network Strengthening Treatment (VNeST) on
lexical retrieval of content words in sentences in persons with aphasia. Aphasiology, 23(3), 402424.
Ferretti, T. R., McRae, K., & Hatherell, A. (2001). Integrating verbs, situation schemas, and thematic role
concepts. Journal of Memory and Language, 44, 516547.
Flintbox. (2010). Northwestern assessment of verbs and sentences (NAVS). Retrieved from https://flintbox.
com/public/project/9299/
Furnas, D. W., & Edmonds, L. A. (2014). The effect of Computer Verb Network Strengthening Treatment on
lexical retrieval in aphasia. Aphasiology, 28, 401420.
Kertesz, A. (1982). Western Aphasia Battery. Austin, TX: Pro-ed.
Kertesz, A. (2006). Western aphasia batteryRevised. Austin, TX: Pro-ed.
Lomas, J., Pickard, L., Bester, S., Elbard, H., Finlayson, A., & Zoghaib, C. (1989). The communicative
effectiveness index: Development and psychometric evaluation of a functional communication measure for
adults aphasia. Journal of Speech and Hearing Disorders, 54, 113124.
McRae, K., Hare, E., & Ferretti, T. R. (2005). A basis for generating expectancies for verbs from nouns.
Memory and Cognition, 33(7), 11741184.
Moss Rehabilitation Research Institute. (2013). Philadelphia naming test (PNT). Retrieved from http://www.
mrri.org/philadelphia-naming-test
Nicholas, L. E., & Brookshire, R. H. (1993). A system for quantifying the informativeness and efficiency of the
connected speech of adults with aphasia. Journal of Speech and Hearing Research, 36, 338350.
Rogalski, Y., Edmonds, L. A., Daly, V. R., & Gardner, M. J. (2013). Attentive Reading and Constrained
Summarization (ARCS) discourse treatment for anomia in two women with moderate-severe Wernickes type
aphasia. Aphasiology, 27, 12321251.
Thompson, C. K. (2011). The Argument Structure Production Test/The Northwestern Assessment of Verbs and
Sentences. Northwestern University.
Webster, J., Franklin, S., & Howard, D. (2004). Investigating the sub-processes involved in the production of
thematic structure: An analysis of four people with aphasia. Aphasiology, 18, 4768.
86
Downloaded From: http://sig2perspectives.pubs.asha.org/pdfaccess.ashx?url=/data/journals/ashannsld/930947/ on 09/19/2017
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
Appendix A. Suggestions for Choosing Verbs to Use in Treatment
Suggestions for Choosing Verbs to Use in Treatment
1. Choose a variety of verbs that represent different types of actions. You can choose verbs together with
your participant. Just make sure you get a range of verbs.
Example: Chop, Kick, Deliver, Measure, Read, Erase, Watch, Fry, Stir, Sew
2. Avoid training verbs that are highly related or associated to avoid semantic interference.
Example: Chop/slice, Kick/throw, Stir/Shake
3. Generalization to (improvement of) untrained semantically related verbs (and nouns) is hypothesized
(and has been seen across VNeST studies), so you can evaluate potential improvement of related
verbs as generalization measures. The verb pairs and triads below are examples of semantically
related/associated verbs. The related word(s) are indicated by the arrow symbol ()) (so only one verb
in a pair/triad would need to be treated). This is not a comprehensive list of possibilities.
Example: ChopSlice, KickThrow, MeasureWeigh, ReadWrite, EraseScrub,
WatchExamine, FryBoilBake, StirShake, SewKnitCrochet, DeliverSend,
PushPull, PaintDraw
4. You can choose verbs that relate to a specific area of interest/functionality for the participant (e.g.,
cooking, sports), but it is recommended that you elicit a variety of scenarios about each verb beyond
the specific area of interest (to promote generalization). The example below shows how a verb like
watch and throw, which relate to activities surrounding a participants interest in a local football
team can be broadened to include more diverse language (Only Step 1 examples shown, not all
necessarily retrieved during one session).
VERB: Watch
Buckeye fan watch- football game/highlights
Coach watch tapes (from game)
Referees watch instant replay
Babysitter watch child/son/daughter
My wife and I watch sunset
Audience watch movie
VERB: Throw
Quarterback throw pass/hail Mary/football
Pitcher throw knuckle ball
Olympian throw javelin/shotput
Comedian throw pie
Baby throw tantrum
My son throw Frisbee (at beach)
5. Do not be afraid to try different verbs. In general, verbs should 1) require a subject and object and 2)
promote some diversity of responses (though verbs differ in this regard).
87
Downloaded From: http://sig2perspectives.pubs.asha.org/pdfaccess.ashx?url=/data/journals/ashannsld/930947/ on 09/19/2017
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
Appendix B. Sample Response Sheet to Use for Recording Responses
and Cueing Levels
Copy the answer sheet below and enlarge it to 8 11. Use one sheet per verb.
88
Downloaded From: http://sig2perspectives.pubs.asha.org/pdfaccess.ashx?url=/data/journals/ashannsld/930947/ on 09/19/2017
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
Facilitating Life Participation in Severe Aphasia with Limited
Treatment Time1
Jacqueline Hinckley
Department of Communication Sciences and Disorders, University of South Florida
Petersburg, FL
Financial Disclosure: Jacqueline Hinckley is Associate Professor Emeritus at the University of
South Florida.
Nonfinancial Disclosure: Jacqueline Hinckley has previously published in the subject area.
Abstract
Although the recovery course of severe aphasia is typically much lengthier and more
protracted than other forms of aphasia, availability of treatment time is often quite limited.
Focusing on one or more specific language domains, such as auditory comprehension, may
be indicated. When treatment time is limited, however, progress in an impairment-focused
approach may be insufficient to affect the individuals daily life. This paper provides a
process for selecting a daily activity, targeting that activity in a participation-focused
intervention, and measuring progress when treatment time is limited. Case examples
illustrate the process. A focus on even one activity that occurs daily can provide ongoing
opportunities for practice and interaction in spite of ongoing treatment.
Perhaps as many as 29% of individuals experiencing left hemisphere stroke and aphasia
experience severe or global aphasia, at least initially (Kang et al., 2010). Since aphasia can be
part of other medical diagnoses and diseases, it is not unusual for clinicians working in medical
settings to be faced with the challenge of selecting appropriate assessments and treatment for
someone with severe aphasia.
The course of severe aphasia can be much more protracted than the recovery patterns of
individuals with less severe aphasia. Published studies of individuals with severe aphasia suggest
that comprehension and repetition may improve the most during the first year after onset, but
that continuous improvement in all other language modalities including spoken language can
occur over many years (e.g., Bakheit, Shaw, Carrington, & Griffiths, 2007; Smania et al., 2010;
Stark & Pons, 2007). Other anecdotal reports suggest that the period of more rapid improvement
is also delayed, perhaps between 6 and 18 months, rather than during the first few months post
onset.
A Rationale for a Focus on Life Participation in Severe Aphasia
Most individuals with severe aphasia will not have access to the kind of long-term services
that have been associated with significant long-term improvement in severe aphasia (Smania
et al., 2010; Stark & Pons, 2007). Also, perceived quality of life and social functioning are
significantly more restricted among those with severe aphasia than those without aphasia or with
other forms of aphasia (Hilari, Needle, & Harrison, 2012; Hilari & Byng, 2009). The critical
question, then, is how to best use the limited treatment resources that are available to make a
potentially long-term impact.
An approach to treatment that is exclusively impairment-focused may not be the most
efficient way of maximizing very limited treatment time. Take, for example, a treatment emphasis
on auditory comprehension, which is often a needed area of improvement in severe aphasia. An
1
Content in this article was presented as part of a SIG 2 Invited Seminar at the ASHA
Convention, Chicago, 2013.
89
Downloaded From: http://sig2perspectives.pubs.asha.org/pdfaccess.ashx?url=/data/journals/ashannsld/930947/ on 09/19/2017
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
exclusively impairment-focused approach might narrow treatment efforts on tasks that isolate
auditory comprehension performance in an easily measurable way. Tasks such as matching
spoken words to pictures or following commands have often been used to determine how well
someone understands spoken language. This approach to treatment is likely to require a more
extensive number of treatment sessions in order to achieve a generalizable effect across contexts
in one particular language domain, such as auditory comprehension.
An immediate focus on participating in an activity that is personally relevant and will be
used on a daily basis is one way of widening the impact of our treatment time. Selecting an
activity that the client is already doing routinely, or could easily be helped to do daily, will build
in additional communication practice. It can also facilitate well-being and overall activity level by
immediately providing a successful and enjoyable task that occurs frequently.
For example, an intervention that focused on a particular activity, in this case ordering
clothing from a catalog, was administered in either a non-intensive (4 hours per week) or
intensive (2022 hours per week) treatment schedule to individuals with moderately-severe
aphasia. Accurate and durable performance on the targeted activity (ordering from a catalog) and
transfer to similar activities or contexts that utilized similar strategies (such as ordering pizza)
was achieved in 110 hours of treatment. This evidence suggests that a focus on a particular
activity can produce equally successful results when treatment time is limited as it does with
more treatment time (Hinckley & Carr, 2005; Hopper & Holland, 1998).
Emphasizing Life Participation in the Evaluation
Treatment goals and outcomes are linked to our initial evaluation, so our selection of
assessments tends to drive documented goals and treatment selection. Initial evaluation data
that are focused on modality-specific performance are more likely to lead to goals and treatments
that are impairment-focused. Initial evaluation data that are focused on life participation will
more readily be translatable to life participation-focused goals and intervention.
For example, take the assessment data for Mrs. C, shown in Table 1. Mrs. Cs ability to
match spoken single words with pictures was moderately impaired, and she was completely
unable to match auditory sentences to pictures. Reading comprehension was similarly impaired,
and she was unable to name a single picture in a naming task. Table 2 shows typical goals that
might be derived from these kinds of evaluation data.
Table 1. Assessment Data for Mrs. C, a Person With Severe Aphasia
Assessment Score
Spoken Word-Picture Matching 45%
Written Word-Picture Matching 45%
Sentence-Picture Matching 0%
Spoken Picture Naming 0%
Communicative Abilities in Daily Living2 17%
90
Downloaded From: http://sig2perspectives.pubs.asha.org/pdfaccess.ashx?url=/data/journals/ashannsld/930947/ on 09/19/2017
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
Table 2. Examples of Goals Typically Linked to Impairment-Focused Assessments.
Assessment Example of Typically Linked Goal ASHA NOMS Levels
Data
Spoken Improve ability to match single, personally Initial: Level 1 (unable to follow simple
Language relevant spoken words to pictures from directions, even with cues)
Comprehension: 45% accuracy to 90% accuracy in an array
of four pictures.
Word-Picture Goal: Level 2 (able to respond to simple
Matching = 45% words or phrases relevant to personal
needs given consistent, maximal cues)
Sentence-Picture
Matching = 0%
Reading: Improve ability to match single, personally Initial: Level 1 (attends to written words)
relevant written words to pictures from
45% accuracy to 90% accuracy in an array
of four pictures.
Written Word- Goal: Level 2 (able to read common
Picture words given consistent, maximal cues)
Matching = 45%
Goals that map very clearly and specifically to the evaluation data are encouraged and
even required by most rehabilitation companies and facilities within their documentation systems
to facilitate reimbursement. Undeniably, the links between the initial evaluation data to the goal
and desired outcomes in Table 2 are straightforward, and because of their clarity and obvious
measurement, they are likely to be reimbursed.
Will these goals affect Mrs. Cs participation in life? Although initial performance on
impairment-focused assessments, like standardized aphasia batteries, may be related to activity
participation, change on impairment-based assessments is not necessarily related to change on
activity participation (Ross & Wertz, 1999, 2002). So, focusing our intervention on a specific
impairment, like impaired auditory comprehension, does not necessarily mean that the client will
now be equipped to participate in life activities.
If we want to increase the likelihood that we will facilitate life participation in our clients,
we have to assess current opportunities for improved participation and focus our intervention
efforts on those. Lets use Mrs. Cs performance on the Communication Activities of Daily Living
(CADL-2; Holland, Frattali, & Fromm, 1999) as an example. This assessment uses role play to
sample a number of activities that are likely to be relevant to a person with aphasia residing in
the community, such as shopping, going to a doctors appointment, ordering from a restaurant
menu, understanding a bus schedule, and filling out forms. The CADL-2 overall score for Mrs. C
was 17%. Since points on most items of the CADL-2 are given based on producing a fully
communicative message regardless of modality, her overall score tells us that Mrs. C is not able
to use many communication modalities very effectively to perform in these role-play activities.
We can analyze specific items within the CADL-2 that correspond to specific activities as
an informal way to track communicative performance. For example, we can analyze Mrs. Cs
ability to provide personal information such as name, address, and medical information with
items #36 of the CADL-2. Assuming that providing personal information is a valuable activity for
Mrs. C, then this can be targeted with a treatment goal. ASHA NOMS levels can be assigned
based on the likelihood that Mrs. C will use spoken language expression or writing to convey the
personal information. Possible goals derived from activities assessed on the CADL-2 are shown in
Table 3.
91
Downloaded From: http://sig2perspectives.pubs.asha.org/pdfaccess.ashx?url=/data/journals/ashannsld/930947/ on 09/19/2017
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
Table 3. Examples of Goals Linked to Activity-Specific Assessments.
Sample CADL-2 Activity Example Goal
Performances
Providing personal Client will provide personal information using written information with
information, items #36 90% accuracy with minimal cues.
Using the phone, items Client will dial 911 and indicate emergency type with 90% accuracy given
4042, 44 minimal cues.
Shopping, items 3037 Client will identify written categories associated with shopping with 90%
accuracy with minimal cues.
A Patient-Centered Model of Assessment and Goal Selection
Application of a patient-centered model for assessment and goal selection can help us
foreground life goals in a more clinically efficient way (Leach, Fleming, & Haines, 2010). A
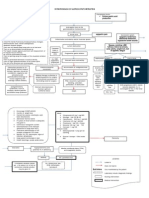
schematic of the process is shown in Figure 1.
Figure 1. A Patient-Centered Model for Goal Selection.
Source. Adapted from Leach, E., Cornwell, P., Fleming, J., & Haines, T. (2010).
92
Downloaded From: http://sig2perspectives.pubs.asha.org/pdfaccess.ashx?url=/data/journals/ashannsld/930947/ on 09/19/2017
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
Maximizing Outcomes in Group Treatment of Aphasia:
Lessons Learned From a Community-Based Center
Darlene Williamson
Stroke Comeback Center
Vienna, VA
Department of Speech and Hearing Science, George Washington University
Washington, DC
Financial Disclosure: Darlene Williamson is the Founder and Director of the Stroke Comeback
Center and Adjunct Professor at George Washington University.
Nonfinancial Disclosure: Darlene Williamson has previously published in the subject area.
Abstract
Given the potential of long term intervention to positively influence speech/language and
psychosocial domains, a treatment protocol was developed at the Stroke Comeback Center
which addresses communication impairments arising from chronic aphasia. This article
presents the details of this program including the group purposes and principles, the use of
technology in groups, and the applicability of a group program across multiple treatment
settings.
In 2014, the stark reality of treatment for individuals with aphasia is that clinicians
are being asked to do more with less: less time and fewer dollars. This limitation in treatment
necessitates solutions that stretch dollars while providing efficacious treatment. As a result
aphasia communities are growing in popularity and in numbers (Simmons-Mackie & Holland,
2011). One such aphasia community is the Stroke Comeback Center in Vienna, VA founded to
provide long-term communication support operating within a Life Participation Approach to
Aphasia. Participants in this program are welcome to attend programs for as long as they feel they
are receiving benefit, which results in a community of stroke survivors dedicated to improving and
from whom much can be learned. This article shares information that has been learned through
involvement with over 300 participants at the center and which might reasonably be applied
across settings, including group purposes and principles and the use of technology that facilitates
improved communication.
Group Treatment for Individuals with Aphasia
Services for individuals with aphasia can be conducted successfully in groups, particularly
if consideration is given to some fundamentals of group treatment. The overall purpose of group
sessions must be specified. One purpose of group treatment is to provide an opportunity to
communicate with peers with structure and support. A successful group is structured around a
theme or language skill, using appropriate supports to facilitate conversation. An example of this
will be discussed later in the article. A second purpose of communication groups is to teach
specific communication strategies. Many communication strategies used in a group setting are
verbal strategies, but other modes of communication can and should be used (e.g., written cueing,
body language including gestures and facial expressions, even an assistive device). All are
appropriate and promote natural communication. A third purpose of a group is to provide an
opportunity to practice the strategies that any individual is using to facilitate communication. It
has been our experience that the real-life atmosphere of a group provides an appropriate and safe
venue for developing and effectively using individualized strategies. Lastly, a fourth purpose of
communication groups is to observe successful communication strategies being used by others in the
group. This may seem elementary, but the value of this peer modeling cannot be overemphasized.
100
Downloaded From: http://sig2perspectives.pubs.asha.org/pdfaccess.ashx?url=/data/journals/ashannsld/930947/ on 09/19/2017
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
Table 5. The Four Categories Included in the LIV with Examples of Activities in Each Category.
Category Examples of Activities
Home & Community Cleaning the house, doing laundry, grocery shopping, going to the doctor,
Activities voting
Creative & Relaxing Using a computer, bird watching, drawing/painting, listening to music,
Activities going to the movies
Physical Activities Golfing, yoga, walking, swimming, fishing
Social Activities Family gatherings, eating out, picnic, storytelling, using the phone
The purpose of the LIV questionnaire is to allow individuals with restricted
communication ability and their family members to indicate activities that are most relevant to
them. As each pictured activity is presented, the interviewer asks, Do you do this now? If the
client answers no, the follow-up question is do you want to start doing this? If the client is
already doing the activity, the follow-up question is do you want to do this more? (Haley,
Womack, Helm-Estabrooks, Lovette, & Goff, 2012).
Matching Formal Assessments to Valued Activities
Once the client and/or family have identified the most valued and important activities, the
clinician will need to complete an assessment that will contribute to the goal-setting process, help
the clinician select an effective treatment approach, and serve as an initial status from which to
measure progress. When treatment time is limited, the selection of the formal assessment tool
needs to be well thought out in order to ensure that some aspects of the assessment will link
directly to one or more of the valued activities. It will also be important to select a tool that will
reveal as many strengths as possible given the presence of severe aphasia.
Lets return to the case of Mrs. C, some of whose assessment data are shown in Table 1.
When Mrs. C completed the LIV card sort, she indicated that she very much wanted to participate
in dinner conversations with her family, but felt left out, probably due to both her impaired
auditory comprehension and her limited expressive abilities.
In order to assess initial abilities in conversation, plan intervention, and report
appropriate initial and final measures, the clinician will need to select formal and informal
measures that directly relate to conversational abilities. Among the assessments shown in
Table 1, matching spoken words to pictures is indirectly linked to the ability to understand
comprehension due to its decontextualized nature. Ability to match spoken words to pictures
does not reveal the clients ability to grasp conversation with all of its environmental,
paralinguistic, and nonverbal context. Only a conversational task will reveal and measure
conversational performance, taking into account all of the conversational supports for
comprehension and expression that will be available.
Two formal assessment tools will provide the clinician the opportunity to assess
conversationally-related abilities with a scoring system that can capture the use of various
communication modalities such as gesture, writing, or speech and are appropriate for those with
severe aphasia. The first of these is the CADL-2 assessment (Holland et al., 1999) described
earlier in this article. The second is the Boston Assessment of Severe Aphasia (BASA; Helm-
Estabrooks, Ramsberger, Morgan, & Nicholas, 1989). Both of these tools allow the clinician to
calculate a score that will capture potential changes in conversational abilities and the use of
conversational supports, such as use of gesture, writing, or a communication notebook. This will
give the clinician an opportunity to document change in the use of appropriate strategies and
their effect on the valued activity of the client, in this case, conversation.
Informal assessment can also be very important in this process. If at all possible, it would
be highly desirable to observe Mrs. C in a conversation with one of her family members to identify
94
Downloaded From: http://sig2perspectives.pubs.asha.org/pdfaccess.ashx?url=/data/journals/ashannsld/930947/ on 09/19/2017
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
potential strategies for Mrs. C and the family member, and to measure their use in successful
conversational interactions.
An example of an informal measure that can help the clinician observe and rate
conversational performance are the measures associated with Supported Conversation for Adults
with Aphasia (SCA), a training technique designed to teach individuals tools for enabling effective
conversation by those with severe aphasia (Kagan et al., 2004).
The Measure of Participation in Conversation (Kagan et al., 2004) is an example of a
rating scale that can be applied to those with severe aphasia for documenting conversational
participation. Two five-point rating scales are provided. Ratings on the Interaction scale range
from 0 (no attempt to participate in conversation) to 4 (takes responsibility for conversational
interaction). Ratings on the Transaction scale related to how well the person with aphasia can
exchange pieces of information. The transaction scale ranges from 0 (no evidence of being able to
understand or get a message across), to 4 (able to understand and get a message across). It is
important to note that ratings are not dependent on how the person with aphasia accomplishes
the communication, and any strategies, tools, or supports can be subsumed in the rating scale.
Although other ways to rate or measure participation in conversation exist, these tools were
specifically designed for those with severe aphasia. The case of Mr. L will illustrate assessment and
goal selection to facilitate life participation in severe aphasia according to the model shown in Figure 1.
Case Example
Mr. L was diagnosed with a global aphasia 2.5 months ago when he was hospitalized with
a left hemispheric stroke. During that time, he underwent inpatient rehabilitation that
culminated in his discharge to home with home health services. He has continued to make
physical improvements along with some small improvements in his communication. Because of
his physical improvements, he was referred to outpatient services for continued therapy.
At this particular outpatient facility, outpatient visits are encouraged to last for only
30 minutes, and are scheduled three times per week. It is anticipated that Mr. L will be able to
receive approximately one month of outpatient speech therapy based on his supplemental
insurance. So, a total of 12 sessions is anticipated.
Mr. L attends his first outpatient session with his wife, Mrs. L, with whom he lives. They are
both retired and prior to Mr. Ls stroke, enjoyed an active social life in their retirement community.
Determine the Clients Priorities
Knowing that there are as few as 12 sessions available for intervention, it is important to
incorporate the clients priorities as much as possible. During the LIV card sort, Mr. L selected
the restaurant picture as an important one. During the interview, Mrs. L stated that going out
with these friends was very important to them, and now her only time to go out socially.
Mr. and Mrs. L routinely go out to dinner two times a week with friends from church (one day
a week) and a group of neighbors (another day a week). Each group goes to different restaurants each
time, but there is a limited set of restaurants because of distance and group preferences
Mrs. L reported that, on the last few occasions when they went out to a restaurant, Mr. L
seemed to get very upset, pushing the menu away, and using obscenities when she tried to order
for him. She knows he is embarrassed or uncomfortable since he is unable to order for himself,
but she doesnt know how to handle the social situation.
Complete Formal and Informal Assessment
Language assessment data at the time of discharge from home health approximately
3 weeks prior to Mr. Ls first outpatient appointment is provided in Table 6. Although Mr. Ls ability
to match spoken or written words to pictures is relatively good, he still has substantial difficulty
understanding sentences. His expression is severely limited, and he is unable to name pictures.
95
Downloaded From: http://sig2perspectives.pubs.asha.org/pdfaccess.ashx?url=/data/journals/ashannsld/930947/ on 09/19/2017
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
Table 6. Assessment Data for Mr. L., a Person With Severe Aphasia.
Assessment Score
Formal and informal assessment prior to outpatient therapy
Spoken Word-Picture 100%
Matching
Sentence-Picture Matching 25%
Written Word-Picture 97%
Matching
Spoken Picture Naming 0%
BDAE Severity Rating 12
(All communication is through fragmentary expression; Conversation
about familiar subjects is possible with help from the listener)
Formal and informal Initial Outpatient discharge
assessment at the (after 12 sessions)
beginning of outpatient
therapy
Communicative Abilities in 86% 90%
Daily Living2
Menu-ordering role play 40% 90%
(5 items; for each item,
CADL-2 scoring was
applied, where
2 = fully communicative
and successful response
for the context
1 = partially
communicative or effective
response for the context
0 = ineffective response for
the context)
Measure of Conversational 2 3
Participation: Interaction (clear attempts to be part (taking increased responsibility
of the conversation) for interaction)
Measure of Conversational 2 3
Participation: Transaction (evidence of ability to understand (able to understand and convey
and get a message across in some information in context most
way at least 50% of the time) of the time)
ASHA NOMS: Spoken 1 2
Language Comprehension (unable to respond even with cues) (with maximal cues, able to respond
to simple words or phrases
related to personal needs)
ASHA NOMS: Spoken 2 3
Language Expression (individual attempts to speak or (with consistent and moderate
communicate but few attempts cueing, individual can communicate
are appropriate) appropriately and meaningfully
in context)
96
Downloaded From: http://sig2perspectives.pubs.asha.org/pdfaccess.ashx?url=/data/journals/ashannsld/930947/ on 09/19/2017
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
Given the clients expressed interest in being able to order at the restaurant and
participate in restaurant outings, the CADL-2 was selected as a formal measure because it
includes two items that are role plays of ordering in a restaurant. Additional informal assessment
was done by using the CADL-2 scoring in an informal role play between the clinician and the
client, using a menu from one of the restaurants that he and his wife go to (see Table 6 for
scoring description). This role play will serve as an initial and final measure. The clinician also
used the Measure of Participation in Conversation ratings after observing a short conversation
between the client and his wife.
Collaborative Goal-Setting
The clinician then engaged in a collaborative goal setting meeting with the client, integrating
formal and informal assessments with valued priorities expressed by the client and his wife.
Examples of goals derived after the collaborative session are shown in Table 7.
Table 7. Examples of Goals Related to Clients Desire to Participate in Restaurant Outings.
Goal #1 Client will request specific food items using speech, gesture, or writing in an
appropriate social context given minimal cues 80% of the time.
Goal #2 Client will use written choices to express basic personally relevant information
in conversation with familiar partners 80% of opportunities with minimal cues.
Goal #3 Client will request repetition using gesture as needed to improve auditory
comprehension in social interactions 80% of opportunities given minimal cues.
Goal #4 Client will request additional time to facilitate expression of personally relevant
information by using gesture 80% of opportunities given minimal cues.
Treatment Plan
Given the goals shown in Table 7, a few treatment approaches are viable options.
Beginning with the clients prioritized activity of ordering in a restaurant, using role play
as a means to practice successful strategies that will be realistic options within that particular
social context will be a good start (Hinckley & Carr, 2001, 2005). Menus from restaurants that
the client typically frequents with his wife can be downloaded or brought to the session and used
for a context-specific practice. The clinician should play the role of the wait staff, and coach the
client with the strategies that will work best for that client, including pointing to the items he
wants to order on the menu. This whole-task, context-specific practice should be completed at
each treatment session to achieve the desired level and to become long-lasting over time. The
critical elements of such an intervention are shown in Table 8. The clinician can also coach the
client to request repetition with a gesture to enhance auditory comprehension. A gesture that
indicates a request for more time should also be trained in the menu-ordering context. Finally, an
escape communication, perhaps a gesture, can be trained, with which the client can request
assistance from his wife.
Table 8. Critical elements of an activity-specific intervention (after Hinckley & Carr, 2005).
1. Establish compensatory strategies based on the participants strengths to achieve the task.
2. Use various means, including a variety of modalities, to achieve effective performance of the task.
3. Use problem-solving feedback interspersed within the targeted task.
4. Role-play the task.
5. Evaluation of performance should be based on communication adequacy and determined by the
listener receiving the message.
97
Downloaded From: http://sig2perspectives.pubs.asha.org/pdfaccess.ashx?url=/data/journals/ashannsld/930947/ on 09/19/2017
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
As time allows, each of these strategiesrequesting items by pointing to words, requesting
repetition through gesture, requesting more time to try again, and requesting assistancecan be
trained in other important contexts, such as in conversation with the clients wife.
Anticipated Long-Term Outcomes
Clinicians often wonder whether training strategies that are useful in one particular
context, and over training those strategies in that particular context, is a useful or a wise use of
treatment time. How much will Mr. L really benefit from being able to order for himself in a
restaurant, assuming he achieves that goal in 12 outpatient treatment sessions?
Mastery of strategies in one particular context will increase the likelihood that the client
will be able to readily transfer these strategies to other similar contexts, and will learn to
recognize when these strategies can be used. In this case, Mr. L has been trained to use one
strategy that facilitates expression (pointing to printed words), one strategy that facilitates
comprehension (requesting repetition), and two strategies that can be used in a variety of
situations (requesting more time and requesting assistance). By starting with a context that is
important and motivating to the client, the strategies are more likely to be clear in terms of
purpose and the training may be more likely to be successful. Once the strategies have been
learned in the restaurant context, transferring them to other situations that are less concrete,
such as conversation, may be more likely to succeed.
The selection of these four strategies is intended to facilitate ongoing improvement even
beyond the point of formal therapy. First, if Mr. and Mrs. L have positive social interactions, even
simply at their weekly restaurant outings, then they are more likely to continue socializing with
friends. Regular social interaction may play a large role in continued improvement for those with
aphasia, and will decrease the chances that they will lose their friends, which is common after
onset of aphasia (Northcutt & Hilari, 2011). A strategy for requesting repetition may facilitate
Mr. Ls practice of listening comprehension in context, and build in ongoing auditory comprehension
practice into his daily life. Similarly, requests for additional time provide Mr. L with the opportunity
to continue to try to express messages. Finally, pointing to written choices is an effective ramp to
participation in conversation, and this strategy will enable him to participate in social contexts and
relationships.
It is difficult to conceptualize what can be accomplished in some of the short treatment
times that clinicians are faced with today, particularly in the case of severe aphasia. It is unlikely
that an entire language domain, such as auditory comprehension, is going to be substantially
improved after only a few short outpatient sessions. If we follow a patient-centered approach to
goal-setting and treatment selection, then we can prioritize training that is of most importance
and relevance to the client. Thus our limited treatment time can produce a socially important,
personally meaningful outcome that can contribute to wellness and participation in life.
References
Bakheit, A. M. O., Shaw, S., Carrington, S., & Griffiths, S. (2007). The rate and extent of improvement with
therapy from the different types of aphasia in the first year after stroke. Clinical Rehabilitation, 21, 941949.
Haley, K. L., Womack, J., Helm-Estabrooks, N., Lovette, B., & Goff, R. (2012). Supporting autonomy for
people with aphasia: Use of the Life Interests and Values (LIV) Cards. Topics in Stroke Rehabilitation, 20(1),
2235.
Helm-Estabrooks, N., Ramsberger, G., Morgan, A. R., & Nicholas, M. (1989). Boston Assessment of Severe
Aphasia. Austin, TX: Pro-Ed.
Hilari, K., & Byng, S. (2009). Health-related quality of life in people with severe aphasia. International
Journal of Language and Communication Disorders, 44, 193205.
Hilari, K., Needle, J. J., & Harrison, K. L. (2012). What are the important factors in health-related quality of
life for people with aphasia? A systematic review. Archives of Physical Medicine & Rehabilitation, 93, S86S95.
98
Downloaded From: http://sig2perspectives.pubs.asha.org/pdfaccess.ashx?url=/data/journals/ashannsld/930947/ on 09/19/2017
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
(Vickers & Mehta, 2012). Use of technology such as internet-connecting devices for easy access to
pre-planned conversational activities and topics, and images are also encouraged (Lee, Funes,
Vickers, & Hagge, 2013). Students are also given access to CRGs virtual file storage so that they
can upload topics and activities to retrieve once on site and/or share with each other across
programs in the two locations (Hagge, Heard, Williams, & Vickers, 2014).
Offering groups in which spontaneous topics arise and cross talk occurs among members
versus one leader controlling the flow and interactions of the group is the goal (Bernstein-Ellis &
Elman, 1999). However, due to their newness in working with persons with aphasia, we find
students benefit from carefully sequenced training in the art of creating conversational topics and
activities to have ready as needed. First, students are encouraged to take into consideration the
age, gender, and cultural background of their group members and have access to the completed
Biographical Sketch forms for all members. Examples of key fringe vocabulary on the bio sketch
form are place of birth, early school and employment experiences, family and friend names, travel
and employment experiences, hobbies, and interests. Students review these forms in order to
select appropriate starting points for establishing context for conversation with their group members.
In addition, students are introduced to ice breaker questions, use of current events, reminiscence
topics, as well as topics to avoid. Examples include politics, religion, and other idiosyncratic sensitive
issues.
The last training session includes whole group viewing of recordings from members who
consented to be videotaped during prior CRG groups. Using whole group dynamics, students learn
to identify communication interactions that are successful and gain exposure to the many ways
that aphasia can present. All students also participate in regular weekly meetings to possible
themes for that week, available technology and how to implement in group, discuss needs of
particular groups or group members, debrief particularly successful or difficult groups from prior
weeks and to learn about incoming members who are joining during a given week.
Communication Recovery Groups in Action
CRG provides a variety of one hour, small conversation groups. Each group is co-led by two
or three undergraduate students and, at CRG-Fullerton, occasional graduate or speech-language
pathology assistant interns. Acceptance of nonverbal as well as verbal forms of communication is
the rule, rather than the exception. Communication using any modality is encouraged, supported,
and accepted for all interactions. Co-leaders overarching concern is facilitating conversation
between group members. A unique feature of CRG-Fullerton is its concurrent offering of a peer
support group for the significant others of its members with aphasia, with support groups led by
a professional from the Caregiver Resource Center associated with St. Jude. Family members
appreciate the chance to attend support group while members attend their respective groups.
CRG in the Medical Setting
In its early days, CRG met at St. Jude Medical Centers main campus and later at its day
treatment center, finally moving off the medical campus to rent space from a large church near the
hospital. Partial funding is provided by the Sisters of St. Joseph, the group that founded St. Jude
and its sister hospitals throughout the area. Additional support comes from nominal screening and
membership fees for new members. CRG received initial funding in 1997 after Vickers submitted
a grant proposal demonstrating how the program was an embodiment of the hospitals focus on
Healthy Communities (Centers for Disease Control and Prevention, 2013) and the core values of
dignity, justice, service, and excellence (St. Jude Medical Center, 2014). Hospital managers and
administrators appreciate CRGs ability to lessen the impact of reduced outpatient services as well
as how it demonstrates mandated community-based resources during Joint Commission audits
and accreditation reviews from the Commission on Accreditation of Rehabilitation Facilities (CARF,
2012).
110
Downloaded From: http://sig2perspectives.pubs.asha.org/pdfaccess.ashx?url=/data/journals/ashannsld/930947/ on 09/19/2017
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
Maximizing Outcomes in Group Treatment of Aphasia:
Lessons Learned From a Community-Based Center
Darlene Williamson
Stroke Comeback Center
Vienna, VA
Department of Speech and Hearing Science, George Washington University
Washington, DC
Financial Disclosure: Darlene Williamson is the Founder and Director of the Stroke Comeback
Center and Adjunct Professor at George Washington University.
Nonfinancial Disclosure: Darlene Williamson has previously published in the subject area.
Abstract
Given the potential of long term intervention to positively influence speech/language and
psychosocial domains, a treatment protocol was developed at the Stroke Comeback Center
which addresses communication impairments arising from chronic aphasia. This article
presents the details of this program including the group purposes and principles, the use of
technology in groups, and the applicability of a group program across multiple treatment
settings.
In 2014, the stark reality of treatment for individuals with aphasia is that clinicians
are being asked to do more with less: less time and fewer dollars. This limitation in treatment
necessitates solutions that stretch dollars while providing efficacious treatment. As a result
aphasia communities are growing in popularity and in numbers (Simmons-Mackie & Holland,
2011). One such aphasia community is the Stroke Comeback Center in Vienna, VA founded to
provide long-term communication support operating within a Life Participation Approach to
Aphasia. Participants in this program are welcome to attend programs for as long as they feel they
are receiving benefit, which results in a community of stroke survivors dedicated to improving and
from whom much can be learned. This article shares information that has been learned through
involvement with over 300 participants at the center and which might reasonably be applied
across settings, including group purposes and principles and the use of technology that facilitates
improved communication.
Group Treatment for Individuals with Aphasia
Services for individuals with aphasia can be conducted successfully in groups, particularly
if consideration is given to some fundamentals of group treatment. The overall purpose of group
sessions must be specified. One purpose of group treatment is to provide an opportunity to
communicate with peers with structure and support. A successful group is structured around a
theme or language skill, using appropriate supports to facilitate conversation. An example of this
will be discussed later in the article. A second purpose of communication groups is to teach
specific communication strategies. Many communication strategies used in a group setting are
verbal strategies, but other modes of communication can and should be used (e.g., written cueing,
body language including gestures and facial expressions, even an assistive device). All are
appropriate and promote natural communication. A third purpose of a group is to provide an
opportunity to practice the strategies that any individual is using to facilitate communication. It
has been our experience that the real-life atmosphere of a group provides an appropriate and safe
venue for developing and effectively using individualized strategies. Lastly, a fourth purpose of
communication groups is to observe successful communication strategies being used by others in the
group. This may seem elementary, but the value of this peer modeling cannot be overemphasized.
100
Downloaded From: http://sig2perspectives.pubs.asha.org/pdfaccess.ashx?url=/data/journals/ashannsld/930947/ on 09/19/2017
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
Lyon, J. (1992) Communication use and participation in life for adults with aphasia in natural settings: The
scope of the problem. American Journal of Speech Language Pathology, 1(3), 714.
Lyon, J. (1995). Drawing: Its value as a communicative aid for adults with aphasia. Aphasiology, 9, 3394.
Lyon, J. (1997). Volunteers and partners: Moving intervention outside the treatment room. In B. Shadden
(Ed.) Aging and Communication: For Clinicians by Clinicians (pp. 299323). Austin, TX: Pro-Ed.
Lyon, J. (1998a). Coping with aphasia. San Diego: Singular Publishing.
Lyon, J. (1998b). Treating real life functionality in a couple coping with severe aphasia. In N. Helm-Estabrooks
& A. Holland (Eds.) Approaches to the treatment of aphasia (pp. 203239). San Diego: Singular Publishing.
McCall, D. (2012). Steps to success with technology for individuals with aphasia. Seminars in Speech and
Language, 33(3), 234242.
National Aphasia Association. (2009). Lookin for me. DVD. Available at http://www.aphasia.org/content/
lookin-me
National Aphasia Association. (2009). Its Still Me! DVD. Available at http://www.aphasia.org/content/its-
still-me
National Aphasia Association. (2011). Welcome to Groups & Programs! Retrieved from www.aphasia.org/
Neuburger, S., Frison, C., & Crowley, R., National Aphasia Association. (1997). [VHS videotape]. Available
from www.aphasia.org/catalog/multimedia
Northcott, S., & Hilari, K. (2011). Why do people lose their friends after stroke? International Journal of
Language and Communication Disorders, 46(5), 524534.
Pound, C., Parr, S., Lindsay, J., & Woolf, C. (2000). Beyond aphasia; Therapies for living with communication
disability. United Kingdom: Winslow.
Rayner, H., & Marshall, J. (2003). Training volunteers as conversation partners for people with aphasia.
International Journal of Language and Communication Disorders, 38(2), 149164.
Simmons-Mackie, S., & Holland, A. L. (2011). Aphasia Centers in North America: A survey. Seminars in
Speech and Language, 32(3), 203215.
Silverman, M. (2011). Community: the key to building and extending engagement for individuals with
aphasia. Seminars in Speech and Language, 32(3), 256267.
St. Joseph Health System: St. Jude Medical Center (2014). Retrieved from http://www.stjudemedicalcenter.
org/For-Community.aspx
Vickers, C. (1998). Communication Recovery: Group conversation activities for adults. San Antonio, TX:
Communication Skill Builders.
Vickers, C. (2010). Social networks after the onset of aphasia: The impact of aphasia group attendance.
Aphasiology, 24(68), 902913.
Vickers, C., & Hagge, D. (2013, May). Tracking social connection versus isolation in aphasia. Poster
presentation for the Clinical Aphasiology Conference, Tucson, AZ.
Vickers, C., & Mehta, S. (2012, Nov). Mobile technology: Impact on conversational interactions. Poster
presentation for the American Speech Language Hearing Association, Atlanta, GA.
Williamson, D., Richman, M., & Redmond, S. (2011). Applying the correlation between aphasia severity and
quality of life measures to a life participation approach to aphasia. Topics in Stroke Rehabilitation, 18(2),
101105.
World Health Organization. (2001). International classification of functioning, disability and health (ICF).
Geneva, Switzerland: World Health Organization, Author.
113
Downloaded From: http://sig2perspectives.pubs.asha.org/pdfaccess.ashx?url=/data/journals/ashannsld/930947/ on 09/19/2017
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
Group Treatment at the Stroke Comeback Center
The Stroke Comeback Center uses a hierarchical group model for communication groups.
When using this model participants are grouped according to communication ability within three
levels of communication. The supported level accommodates individuals benefit from or need
support to participate in communicative interactions. Activities are designed to move at a slow
pace that allows for increased processing and response formulation time. Typical outcomes of
group participation at this level are to increase comprehension of specific vocabulary, express
ideas using multi modal communication, or to use aspects of circumlocution or semantic feature
analysis. Tasks might include yes/no question format, completion of open-ended stimuli,
modeling and use of carrier phrases. All activities are supported with appropriate materials that
promote multimodal communication.
The functional level is for participants who possess emerging functional communication
typically phrase level speech output and are fairly independent with compensatory communication
strategies (gestures, drawing, and writing). Typical outcomes would include being able to express
ideas via expanding verbal output, use aspects of multimodal communication to achieve specificity
in communicative interactions, or to complete functional tasks using individualized strategies.
Activities in functional level groups move at a faster pace than in supported level groups, while giving
appropriate cueing and modification of pace, as required, to assist all group participants. Examples
of tasks at this level would include practicing affirmative and negative sentence structure, using
semantic feature analysis for describing and categorizing, and functional tasks promoting sentence
length verbal expression.
Conversation level groups accommodate participants who use verbal output at a sentence
or conversational level. The pace of the group can move faster and activities are designed to flow as
a discussion. Outcomes at this level might be to expand verbal output to multi-sentence level or
to expand the amount and specificity of vocabulary related to a specific topic. Examples of specific
tasks at this level include item generation within a category within a specified (30 seconds) time
limit, use of descriptive words to communicate a theme-related item to other group members, and
group discussion of a theme-related concept, question, article, or video.
All three levels of groups can participate in the same theme or skill and the same format
for the hour; materials and outcomes are altered to promote communication at each level. The
format begins with a brief period of socialization which is critical to building the group dynamic
and peer relationships. This approximate 510 minute segment helps establish and maintain
focus as the group progresses. Without an opportunity to share personal thoughts and feelings
either the group can lose cohesion or individual group members can be distracted by a thought that
they wished to communicate to their peers. It also provides the group leader with an opportunity
to take the pulse of the groupdetermining who has intervening personal issues, or is being
affected by the weather or transportation issues? It is an absolutely necessary component of
successful group outcomes, but should not dominate the allotted group time except in extenuating
circumstances when a group member communicates personal information that is compelling to
other members and the leader senses the need to come to completion with the issue. This social
time is followed by a 1015 minute segment that introduces and builds context for the group theme
or skill. This segment involves structured tasks such as automatics, cloze tasks, matching. or
open-ended tasks. The primary group segment focuses on prescribed language tasks supporting
the theme or skill for the day, as well as addressing communication level and individualized goals.
This portion of the group is approximately thirty minutes in duration and can focus on a single
communication task (e.g., reacting to a video, ordering from a menu) or multiple language tasks as
previously mentioned. The group leader determines the tasks and focus of this segment based on
group dynamics, time constraints or interest level. The final segment of this suggested group flow
is a 510 minute wrap up of the theme or skill and typically includes suggestions for functional
102
Downloaded From: http://sig2perspectives.pubs.asha.org/pdfaccess.ashx?url=/data/journals/ashannsld/930947/ on 09/19/2017
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
usage of the vocabulary used during the group and discussion or specific assignments for carrying
over the language from group into members personal environments.
In addition to promoting targeted use of language, groups have been found to enhance
overall life participation. One project conducted at the Stroke Comeback Center asked members
to use a self-rating scale to rate 20 areas of Body Function and Activity & Participation within
the International Classification of Functioning. Areas of functioning found to be most impacted
by participating in group sessions were: Energy and Drive, Attention, and Mental Functioning
(Williamson & Richman, 2007). While these kinds of outcomes are ancillary to participation in
treatment groups, they suggest additional value in providing group support for individuals with
aphasia.
Use of Technology to Assist Communication in Aphasia/Apraxia
within a Community-Based Setting
The use of technology, particularly iPad-based, is a hot topic within our profession and is
another means of supplementing treatment in an efficacious and cost-effective way. As a preliminary
and cautionary note, the same individualized attention and selection must be given to providing
technology-based treatment as is given to any selection of tasks and activities for clients. The
technology applications available are not recommended or selected based solely on content or
availability; they must be matched to clients specific needs and abilities.
Nonetheless, an ongoing, long-term community aphasia center provides the opportunity
to experiment with various technologies and receive ongoing feedback from users. Many
technology-based tasks are also completely appropriate to be addressed in a group setting.
The first use of technology worthy of mention is an augmentative and alternative
communication (AAC) device. While specific AAC/SGD information is beyond the scope of this
article, it is significant that groups are a perfect venue for practicing use of a device. Groups provide
a naturalistic real-life environment requiring a device user to find or create specific vocabulary,
expand on simple communications, and use the device in a timely manner in order to keep pace
with group dynamics. Individuals who use devices for communication should not be excluded
from group participation, rather they should be encouraged to attend and participate as a means
of facilitating use of the device. CPUs or laptops are generally accepted adjuncts to any speech
therapy treatment and there are a variety of computer-based programs that allow for home practice
of basic speech and language functions. These computer-based programs should always be given
consideration when formulating a comprehensive plan of treatment. Computers can also be
successfully infused into group sessions. One obvious use within a group treatment format is use
in writing groups. Participants can be given the option of written production of thoughts and
information via Word processing as opposed to pencil and paper. Dictation software and software
with text-to-speech functions are two examples of computer-based uses. If an individuals verbal
output exceeds their graphic output, using dictation software can be an efficient and helpful
tool. There are several alternatives for commercially available dictation software, some quite
expensive, some available for free in Windows 7 or Google Chrome. A text-to-speech function on
the computer is helpful when an individuals auditory comprehension permits hearing errors or
incompleteness in thoughts. A client can word process a thought, highlight it, then listen as many
times as necessary to determine the level of accuracy. A particularly user-friendly software program
that allows for both speech recognition and text-to-speech is WordQ/SpeakQ (GoQ Software, n.d.)
When using this kind of software in a group setting, it is always recommended to use headphones
with a microphone to minimize interference with other group members. If clients can bring their
own laptops, the software and techniques can be practiced in a group leading to more successful
use at home.
Of course, mobile device technology has rapidly become a readily available and extremely
valuable adjunct to traditional therapy. There has been much written within our field about best
103
Downloaded From: http://sig2perspectives.pubs.asha.org/pdfaccess.ashx?url=/data/journals/ashannsld/930947/ on 09/19/2017
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
use of mobile technology and recommended applications, from games to functional everyday uses,
to applications developed for specific therapeutic use. Groups can be designed around and focused
on mobile technology. Members who use iPad/iPhones can bring and share games and applications
that they have discovered and use. Alternatively, the group leader can suggest appropriate
applications for group members. Group members can be challenged to search for word games or
language-based games and share them.
The Stroke Comeback Center uses mobile technology extensively within groups and has
developed some uses of technology specifically designed to help our members. Using traditional
imitative techniques for apraxia of speech and combining technology resulted in a program termed
VAST (Video Assisted Speech Technology). This is a process of individuals speaking simultaneously
with a close-up video of a model mouth carefully articulating word, phrase, or sentence length
utterances. Combining the VAST technique with aphasia scripting allows individuals to produce
entire scripts. These scripts can be practiced within a group setting. Clinical practice of VAST
scripts at the Stroke Comeback Center yielded results that indicated that all levels of speakers can
use the technique, that use of the technique resulted in improved articulatory precision, and that
the ability to produce personal information generalized after practicing with the technique. Most
notable was the finding that confidence in using the technique appeared to be a larger contributor
to success than amount of practice (Williamson, 2012). Group practice provides a platform for
increasing confidence in using the VAST technique. Community Outing groups at the Stroke
Comeback Center practice using functional scripts within the community, ordering at restaurants,
requesting information at businesses, etc. (Additional information regarding use of the VAST
technique can be found at www.speakinmotion.com) The VAST technique was further examined
at the University of South Carolina Aphasia Lab with results that supported use of the technique
(termed speech entrainment in these studies) in Brocas aphasia, noting that there was greater
bilateral cortical activation for speech while using the technique (Fridriksson et al., 2012).
Applicability Across Multiple Settings
The information described or suggested thus far has originated in a community-based
setting that operates outside third party reimbursement. Group therapy can qualify for third party
reimbursement, and the same principles and methodologies can be used. In order to qualify for
third party reimbursement, group speech language pathology services must be a covered benefit,
documented as part of a treatment plan with goals specifically identified and updated based on
progress, and be part of a medically necessary plan of care. Group therapy is covered by most
third party insurances (except Cigna and Tricarealthough they are open to exceptions in certain
cases), and Medicaid. Per the Medicare definition of group services, there must be two or more
individuals involved simultaneously who can be, but need not be, performing the same activity. A
speech-language pathologist (SLP) must be present. Additionally, Medicare sets additional guidelines
related to the number of participants per group and percentage of services. Medicare stipulates
that no more than four people can be in a group (Center for Medicare and Medicaid Services, n.d.).
This contradicts the information presented above which suggests that five participants is ideal,
but a group can be successful with four participants and four is also a number which makes a
treatment group profitable vs. an individual reimbursement rate. Some third party reimbursers
count visits rather than sessions which allows for more therapy for the same co-pay or use of benefit.
The group CPT code is 92508, which is a non time-based code. Group treatment can be billed on
the same day as individual treatment using the -59 modifier to indicate distinct procedures; for
example, 92507-59, 92508-59 on a day when both are performed.
Documentation becomes the key issue in third party reimbursement for group treatment.
The initial evaluation report must justify group treatment. For example, Individual SLP treatment
is recommended 2 times/week with participation in Communication Strategies group to facilitate
carryover of strategies 1 time/week for 8 weeks. Goals must be identified for group treatment.
They can be the same as goals identified for individual treatment or they can be group specific goals.
104
Downloaded From: http://sig2perspectives.pubs.asha.org/pdfaccess.ashx?url=/data/journals/ashannsld/930947/ on 09/19/2017
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
For example, specific goals may include amount of assistance required, number of demonstrated
behaviors, or accuracy of demonstrated behaviors. Lastly, group sessions must be documented
as separate procedures. Performance on goals in the group must be documented in daily notes or
on a separate flow sheet. Group performance must also be included in progress and/or discharge
summaries.
When giving consideration to implementing groups in any setting, it is important to note
that groups are a venue for providing new product lines to existing individual services. Groups can
also provide some scheduling flexibility to accommodate staffing changes. Also as an important
consideration, groups can generate more revenue while increasing frequency or intensity of sessions
for your patients. It is always recommended that clinicians check with any third party reimbursement
source for guidelines related to group treatment reimbursement and the ASHA website and National
office can also provide valuable guidance.
While the Stroke Comeback Center is a community-based, nonprofit organization operating
outside third party reimbursement, the model used for group treatment and the use of technology
has been shown to be an efficacious model and one that can be translated to other reimbursable
settings. This type of ongoing treatment will maximize communication outcomes and promote
quality of life for individuals with aphasia.
Acknowledgements
The author wishes to acknowledge professional colleagues Melissa S. Richman, M.S.,
CCC-SLP, Suzanne C. Redmond, M.S. CCC-SLP, and Brooke Hatfield, M.S., CCC-SLP for their
assistance in compiling the clinical information.
References
Bernstein-Ellis, E., & Elman, R. (1999). Aphasia group communication treatment: The Aphasia Center of
California approach. In R. Elman (Ed.), Group treatment of neurogenic communication disorders: The expert
clinicians approach (pp. 4756). Boston: Butterworth-Heinemann.
Centers for Medicare & Medicaid Services (n.d.). Medicare benefit policy manual. Chapter 15- Covered
medical and other health services. Retrieved from www.cms.gov/Regulations-and-Guidance/Guidance/
Manuals/downloads/bp102c15.pdf
deRuiter, J., Weston, G., & Lyon, S. M. (2011). Dunbars Numbers: Group Size and Brain Physiology in
Human Reexamined. American Anthropologist, 113(4), 557568.
GoQ Software (n.d.). Available from www.goqsoftware.com
Fridriksson, J., Hubbard, H. I., Hudspeth, S. G., Holland, A. L., Bonilha, L., Fromm, D., & Rorden, C. (2012)
Speech entrainment enables patients with Brocas aphasia to produce fluent speech, Brain, 135(12),
38153829.
Simmons-Mackie, S., & Holland, A. L. (2011). Aphasia Centers in North America: A survey. Seminars in
Speech and Language, 32(3), 203215.
Williamson, D. S. (2012, November). Treatment of Apraxia of Speech Using Static and Dynamic Modeling.
Seminar presented at the American Speech-Language-Hearing Association, Atlanta, GA.
Williamson, D. S., & Richman, M. S. (2007). Outcomes Within the International Classification of Functioning,
Disability and Health at a Community-Based Stroke Center. Paper presented at the American Speech-
Language-Hearing Association Convention, Boston, MA.
105
Downloaded From: http://sig2perspectives.pubs.asha.org/pdfaccess.ashx?url=/data/journals/ashannsld/930947/ on 09/19/2017
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
Communication Recovery Groups for Persons with Aphasia:
A Replicable Program for Medical and University Settings
Candace Vickers
Department of Health Sciences, Speech Language Pathology, California Baptist University
Riverside, CA
Darla Hagge
Department of Speech Language Pathology, California State University Sacramento
Sacramento, CA
Financial Disclosure: Candace Vickers is Program Director of Speech-Language Pathology at
California Baptist University. Darla Hagge is an Assistant Professor at California State University
Sacramento.
Nonfinancial Disclosure: Candace Vickers has previously published in the subject area. Darla
Hagge has previously published in the subject area.
Abstract
This article describes Communication Recovery Groups (CRG), an aphasia group program
that is sponsored by a medical setting and more recently a university setting. CRGs history
and approach and its model of service in light of current healthcare challenges are summarized.
The article also provides a detailed discussion regarding the logistics of offering conversation
groups to persons with aphasia which are sponsored by medical and/or university settings,
the intake process for new group members, and the training of student volunteers to help
lead conversation groups.
According to figures from the American Medical Association (2007) there are over one million
Americans living with aphasia each year. These sobering figures coincide with current challenges
in healthcare for outpatient rehabilitation clinicians providing services under the Medicare Cap
(Centers for Medicare and Medicaid Services, 2014). When formal therapy for aphasia ends,
persons with aphasia (PWA) may experience a void in terms of the chance to experience satisfying
and supportive communication in meaningful interactions with others. Below, we describe several
factors which highlight the critical need for more availability of aphasia friendly communication
programming for persons with chronic aphasia after discharge from formal therapy.
While Elman and Bernstein-Ellis (1999) report strong evidence that group communication
treatment is efficacious and there has been some growth in numbers of groups for PWA over the
last decade nationwide, options for ongoing assistance with aphasia after discharge from traditional
therapy remain limited. Simmons-Mackie and Holland (2011) report there are only 26 aphasia
centers in North America. The National Aphasia Association (NAA, 2011) lists 13 intensive aphasia
programs in North America and more than 200 aphasia-related groups in North America. Some
groups are designed for the PWA and others for partners, but not all groups meet weekly.
In addition, Hilari and Northcott report reduced social networks (2006) and loss of friendships
for PWA (Northcott & Hilari, 2011) in the United Kingdom after aphasia. In the United States, there
is evidence that after the onset of aphasia, social network size and amount of regular contact with
communication partners reduce by approximately 50% from pre-aphasia levels (Vickers, 2010).
This social isolation combined with a lack of available aphasia programming at the community
level in many areas of the United States perpetuates the loneliness and frustration for many with
aphasia (Vickers & Hagge, 2013).
As a response to the lack of opportunities for PWA in the Southern California area, in 1994
Vickers launched the first hospital based Communication Recovery Group (CRG) using trained
106
Downloaded From: http://sig2perspectives.pubs.asha.org/pdfaccess.ashx?url=/data/journals/ashannsld/930947/ on 09/19/2017
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
communication partner volunteers at St. Jude Medical Center in Fullerton, California (Vickers,
1998). This year marks the 20 year anniversary of the original CRG, which offers conversation
practice to adults with chronic aphasia after discharge from outpatient therapy. It also marks the
birth of another Communication Recovery Group (CRG), launched in 2013 at California State
University Sacramento (CRG-SAC) by Darla Hagge. CRGs original Fullerton location (CRG-Fullerton)
serves over 60 members and uses 2530 student volunteers. After only one semester, CRG-SAC
already serves 26 members and uses 19 students, the majority of whom receive college credit for
their work in the program. This article describes CRG as it is now offered in both locations.
Communication Recovery Group (CRG): History and Approach
CRG was inspired by aphasiologist Jon Lyon, who described the positive impact of trained
communication partners during interactions with persons with aphasia as part of the individual
therapy process (Lyon, 1992). Lyon was an early advocate for incorporating the World Health
Organizations concept of participation in life (WHO, 2001) into therapy with persons with aphasia.
As one of the original authors of the Life Participation Approach to Aphasia (LPAA; Chapey
et al., 2000), Lyons work has had a far ranging impact on the field. Lyon initiated an organization
called Living with Aphasia that served PWA and their partners outside of medical reimbursement
settings (Lyon, 1998a). In his early writings about the use of communication partner volunteers,
Lyon stressed the inherent value of a trained communication partner for PWA, emphasizing the
benefit of PWAs interactions with volunteers who interacted out of choice, not obligation (Lyon,
1997). In addition to his own individual work with individuals and couples, Lyon successfully
partnered with the United Way organization to recruit and train community-based Communication
Partner volunteers who would, after initial training sessions, meet with PWA regularly to engage
them in preferred activities in the community (Lyon, 1997). Lyon (1998b) also anticipated shrinking
healthcare resources and warned that speech-language pathologists (SLPs) would need to use new
approaches to meet the challenge of providing sufficient services to PWA. This concern was echoed
by the NAA (Klein, 1996). As an outpatient clinician, Vickers observed firsthand the significant
changes in healthcare services (e.g., implementation of managed care) which resulted in reduced
length and duration of sessions for PWA. Opportunities for discharged individuals to attend
aphasia groups were almost nonexistent in the Orange County area of Southern California in the
mid-1990s. Due to its hospital setting and official volunteer service guidelines, CRG-Fullerton was
unable to pair volunteers with PWA in the community. However, Lyons concept of using nonobligated
trained communication partner volunteers with PWA seemed valuable and doable in a small
conversation group format. CRG-Fullerton has grown steadily since 1994, from two to over
60 members, confirming the need for ongoing access to conversation experiences for PWA.
Lyons contributions regarding communication partner volunteers and related communication
support methods such as communicative drawing (Lyon, 1995), as well as Written Choice
Communication (Garrett & Beukelman, 1992) and Supported Conversation (SCA; Kagan, Black,
Duchan, Simmons-Mackie, & Square, 2001) became the framework for how CRG groups are offered.
These communication support techniques, along with an emphasis on enhancing life participation
after aphasia, have taken root in the United States and internationally, and are fundamental
in interactions with PWA in multiple programs in North America and Europe (Elman & Bernstein-
Ellis, 1999; Glista & Pollens, 2007; Kagan et al., 2001; McCall, 2012; Pound, Parr, Lindsay, &
Woolf, 2000; Silverman, 2011; Williamson, Richman, & Redmond, 2011).
CRG Model of Service
Elman (2011) points out the complexities of opening an aphasia center, and suggests that
hospital sponsored aphasia groups may work well in many communities if founding a center is
not possible. Simmons-Mackie and Holland (2011) state that there is no specific definition for an
actual aphasia center, but identified shared priorities by many centers measured in their survey
research. Examples are a focus on conversation groups, building community, and promoting
107
Downloaded From: http://sig2perspectives.pubs.asha.org/pdfaccess.ashx?url=/data/journals/ashannsld/930947/ on 09/19/2017
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
increased life participation. CRGs model of service fits well with what Silverman (2011) terms
a center without walls, and utilizes one to two SLPs that design and guide the program using
trained volunteers and/or students to provide weekly conversation groups. In its simplicity of
structure, CRG may be an affordable and replicable model for SLPs to implement at the medical,
community; and university levels. Specifically, groups meet weekly in rented or owned space and
have low budgetary needs in terms of equipment (e.g., cabinet for storage, AV, portable room dividers)
and furniture (e.g., tables designed for 46 persons, non-rolling chairs).
In order to meet the ever increasing need and demand for PWA to attend our groups, we
find that consistent access to interested students or other adult volunteers is essential. In the
medical setting, the volunteer services department has a rehabilitation volunteer designation that
is used for CRG-Fullerton, while CRG-SAC is often able to provide students with college credit and
clinical hours.
Utilizing trained volunteers to be conversation partners is supported in the literature in terms
of increasing participation of PWA in conversation (Kagan et al., 2001; Rayner & Marshall, 2003).
Use of volunteers does require additional work of the SLP and has its own challenges. Medical
settings may offer the advantage of a volunteer service department which provides volunteers with
a general orientation to safety and Health Insurance Portability and Accountability Act (HIPAA)
and enforces background checks and tuberculosis skin test clearances. Although requests to
work as a volunteer in CRG-Fullerton always outnumber the spots available, one challenge for
CRG-Fullerton is ensuring that only the most committed and diligent persons are recruited and
trained. Also, consistent volunteer attendance can be problematic when students academic demands
conflict. CRG-SACs ability to offer college credit to many of the students involved offers a way to
increase accountability. Despite the extra work and training involved, we find it valuable to use
volunteers in that it allows us to reach more persons with aphasia. In the hope that some elements
of CRGs format may help others find an accessible way to expand services outside formal therapy,
we delineate key aspects of operating CRGs.
CRG Intake Process for New Members
To begin, prospective members and their significant others (SO) are scheduled for a screening
with the CRG director. The screening process takes place in a comfortable, professional environment,
but is conducted using an informal agenda. This allows for: (a) personal contact and establishment
of rapport, (b) the opportunity to note residual language skills for communication in groups and
trial of strategies, and (c) a chance to provide detailed description of the purpose and design of CRG.
We also confirm that the PWA desires to participate in the program and understands that he/she
is not entering into one-to-one traditional therapy. At times, the need for specific types of advocacy
or referrals becomes evident as well. All incoming members are also asked for written permission
to be included in pictures for a group roster to help volunteers know them more easily, to have
their images appear in photos in slide shows for social events, and possibly to be videotaped for
inclusion in professional presentations related to group treatment.
CRGs intake packet for prospective members asks that the Biographical Sketch (Garrett &
Beukelman, 1992) be completed prior to the screening. Access to this information allows establishment
of familiar context for conversation during the screening process and highlights possible common
ground with other members. Based on the screening, new members are assigned into already existing
conversational groups, or a new group may be created to accommodate the member. Although
aphasia type and severity are weighted factors in determining group placement, we also carefully
consider all prospective members personal factors, such as age, hobbies, interests, culture, and
personal history. This step is an integral part of the success of the individual members enjoyment
in the program and ensures ongoing cohesion for the program as a whole.
A further priority in CRG is that all members (e.g., PWA) and students experience a safe
and respectful environment. The following are exclusion criteria for prospective members: (a) lack
of desire/interest to participate, (b) significant lability, (c) displays of significant depression and/or
108
Downloaded From: http://sig2perspectives.pubs.asha.org/pdfaccess.ashx?url=/data/journals/ashannsld/930947/ on 09/19/2017
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
uncontrollable outbursts of anger or rage, and/or (d) concurrent enrollment in formal speech
therapy.
CRG Intake and Training Process for Student Group Co-Leaders
Both locations for CRG benefit from being in metropolitan areas that contain large
universities with undergraduate students desiring to participate in the rich experiential learning
opportunity with adults with aphasia that CRG provides. Both programs also usually have a waiting
list of at least five to ten students waiting to interview for the opportunity to volunteer. The trained
communication partner curriculum for students was designed jointly by both co-authors over many
years, and students in both locations participate in six hours of training at regular intervals.
Graduate students at CRG-SAC are able to earn clinical clock hours as part of their experience,
while at CRG-Fullerton, only graduate student interns earn hours. Students at CRG-Fullerton
earn volunteer hours which are carefully recorded by St. Judes Volunteer Services Department.
Recently, Hagge designed a training curriculum using a top-down approach and provides
the instruction using a variety of teaching pedagogies and strategies. First, the students receive
instruction concerning a brief history of persons with disabilities (Albrecht, Seelman, & Bury,
2001), the World Health Organizations International Classification of Functioning, Disability, and
Health (WHO, 2001), the American Speech-Language-Hearing Associations Scope of Practice
(ASHA, 2007), and a discussion of the medical model versus the social model approach to aphasia
(Kaplan, 2000).
Both programs include a brief overview of the history and purpose of CRG (Vickers, 1998)
and provide viewing of one or more of the following DVDs: (a)Supported Conversation for Adults
with Aphasia (SCA) (Aphasia Institute, n.d.a.), (b) Looking for Me (Neuburger, Frison, Crowley,
National Aphasia Association, 1997) and, (c) Its Still Me! (NAA, 2009). Next, students are
introduced to conversational support tools for aphasia through viewing examples of Supported
Conversation through the SCA video (Aphasia Institute, n.d.a.), and discussion of the reproducible
partner training handout Written Choice Communication Technique for Adults with Severe
Communication Disability (Garrett & Beukelman, 1992).
Together, students practice for an interaction with an individual with aphasia by learning
to provide augmented input in the form of key topic words and/or written choice relevant to an
authentic communication exchange (Garrett & Beukelman, 1992). For example, students are
provided with and instructed to use scratch paper or a dry board to present key words and choices
without delay by writing or drawing upside down (e.g., keeping the dry board facing the PWA
rather than towards themselves while writing). Thereafter, each student practices the use of written
key terms and written forced choice in a structured conversation activity. For example, the instructor
walks the students through a familiar, functional, and concrete communicative interaction (e.g.,
choosing a restaurant for lunch). Using markers and paper or dry erase boards and markers,
students identify and write appropriate key terms (e.g., lunch) and choices (e.g., fast food, restaurant).
The goal is to enhance communication partner/group leader skills by providing the chance to learn
and practice collectively in a supportive and positive environment.
Immediately thereafter, students are assigned to dyads and given several role playing
scenarios representing interactions between a PWA with nonfluent aphasia and the SO. Dyads
perform interactions collectively as a way to decrease any performance pressure and often-resultant
anxiety. After everyone has finished their assigned role playing activity, students share their
experiences using a whole group discussion. Additional training occurs in weekly training meetings
and through direct modeling and mentoring by the directors before, during, and after group
sessions.
Students are introduced to a robust list of materials that support conversation in aphasia
groups. These items include access to a large supply of scratch paper, markers, white boards,
erasers, markers, conversation cards, magazine pictures, and maps (Bernstein-Ellis & Elman,
1999). Mobile technology is incorporated into groups and has been found to enhance interaction
109
Downloaded From: http://sig2perspectives.pubs.asha.org/pdfaccess.ashx?url=/data/journals/ashannsld/930947/ on 09/19/2017
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
(Vickers & Mehta, 2012). Use of technology such as internet-connecting devices for easy access to
pre-planned conversational activities and topics, and images are also encouraged (Lee, Funes,
Vickers, & Hagge, 2013). Students are also given access to CRGs virtual file storage so that they
can upload topics and activities to retrieve once on site and/or share with each other across
programs in the two locations (Hagge, Heard, Williams, & Vickers, 2014).
Offering groups in which spontaneous topics arise and cross talk occurs among members
versus one leader controlling the flow and interactions of the group is the goal (Bernstein-Ellis &
Elman, 1999). However, due to their newness in working with persons with aphasia, we find
students benefit from carefully sequenced training in the art of creating conversational topics and
activities to have ready as needed. First, students are encouraged to take into consideration the
age, gender, and cultural background of their group members and have access to the completed
Biographical Sketch forms for all members. Examples of key fringe vocabulary on the bio sketch
form are place of birth, early school and employment experiences, family and friend names, travel
and employment experiences, hobbies, and interests. Students review these forms in order to
select appropriate starting points for establishing context for conversation with their group members.
In addition, students are introduced to ice breaker questions, use of current events, reminiscence
topics, as well as topics to avoid. Examples include politics, religion, and other idiosyncratic sensitive
issues.
The last training session includes whole group viewing of recordings from members who
consented to be videotaped during prior CRG groups. Using whole group dynamics, students learn
to identify communication interactions that are successful and gain exposure to the many ways
that aphasia can present. All students also participate in regular weekly meetings to possible
themes for that week, available technology and how to implement in group, discuss needs of
particular groups or group members, debrief particularly successful or difficult groups from prior
weeks and to learn about incoming members who are joining during a given week.
Communication Recovery Groups in Action
CRG provides a variety of one hour, small conversation groups. Each group is co-led by two
or three undergraduate students and, at CRG-Fullerton, occasional graduate or speech-language
pathology assistant interns. Acceptance of nonverbal as well as verbal forms of communication is
the rule, rather than the exception. Communication using any modality is encouraged, supported,
and accepted for all interactions. Co-leaders overarching concern is facilitating conversation
between group members. A unique feature of CRG-Fullerton is its concurrent offering of a peer
support group for the significant others of its members with aphasia, with support groups led by
a professional from the Caregiver Resource Center associated with St. Jude. Family members
appreciate the chance to attend support group while members attend their respective groups.
CRG in the Medical Setting
In its early days, CRG met at St. Jude Medical Centers main campus and later at its day
treatment center, finally moving off the medical campus to rent space from a large church near the
hospital. Partial funding is provided by the Sisters of St. Joseph, the group that founded St. Jude
and its sister hospitals throughout the area. Additional support comes from nominal screening and
membership fees for new members. CRG received initial funding in 1997 after Vickers submitted
a grant proposal demonstrating how the program was an embodiment of the hospitals focus on
Healthy Communities (Centers for Disease Control and Prevention, 2013) and the core values of
dignity, justice, service, and excellence (St. Jude Medical Center, 2014). Hospital managers and
administrators appreciate CRGs ability to lessen the impact of reduced outpatient services as well
as how it demonstrates mandated community-based resources during Joint Commission audits
and accreditation reviews from the Commission on Accreditation of Rehabilitation Facilities (CARF,
2012).
110
Downloaded From: http://sig2perspectives.pubs.asha.org/pdfaccess.ashx?url=/data/journals/ashannsld/930947/ on 09/19/2017
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
CRG in the University Setting
The speech-language and audiology program (SPA) in the College of Health and Human
Services at California State University Sacramento (CSUS) supports an on-campus speech and
hearing clinic. PWA may participate in CRG-SAC in addition to or as an alternative to traditional,
impairment-focused therapy services and are officially enrolled as clients. Traditional speech-
language services are provided twice a week, while CRG-SAC meets for one hour each week within
the regular ten month university schedule.
In alignment with the CSU Graduation Initiatives (CSUS, n.d.a.), CRG-SAC recruits,
educates, and trains a small cadre of speech-language and audiology undergraduate students to
serve as trained communication partners. At the beginning of each semester, the selected students
receive more than six hours of education and training, participate in HIPAA training, and pass a
comprehensive background check. Students are required to prepare weekly conversational topics
and scripts, along with determining a variety of ways to supplement the content with augmented
input. For example, students may design power point presentations and use as visual scene
displays (Lee et al., 2013). Age and culturally-appropriate conversational topics with corresponding
forced choice questions are prepared in advance and submitted to the instructor for feedback.
In addition, CRG-SAC offers small conversation groups facilitated by graduate students in
the speech-language pathology program. These small groups are reserved for those individuals
with aphasia who needs cannot be met through the primary CRG-SAC. For example, some
individuals with aphasia have difficulty transitioning to a large aphasia program, and benefit from
a group housed in a more traditional location (e.g., therapy room). Graduate students also have
the opportunity to provide a hybrid version of small group services, integrating conversational
and functional goals. For example, a PWA with apraxia of speech may prefer to participate in a
conversation while also given the opportunity to practice speaking functional words and phrases.
The graduate students have the opportunity to practice designing and providing client driven
services, a model supported by the Life Participation Approach to Aphasia (Chapey et al., 2000).
Interprofessional Education Opportunities
CRG-SAC is uniquely positioned to offer students from across the universitys healthcare
disciplines the opportunity to receive aphasia education and group observation. Currently, this
interprofessional education experience is offered to students from nursing, but will soon be offered
to physical therapy, social work, and recreation therapy students. Interested students meet
with the director, watch a training video, participate as a guest communication partner, and
debrief afterwards with the entire CRG-SAC team. The whole group processing supports peer
learning across disciplines and promotes aphasia awareness. For example, one nursing student
identified her professional mandate to advocate for all patients, and the value in using the modeled
communication tools as a way to successfully advocate for her patients with aphasia.
Conclusion
Since October of 2013, outpatient rehabilitation centers have felt the impact of the Medicare
Cap very keenly. The impact of the Cap and managed care, along with the aging of the population
and rate of aphasia in the United States, make programs like CRG even more important for PWA
after discharge from formal services. It is possible to replicate the CRG model of groups using trained
volunteers in other places to provide a needed outlet for PWA to find meaningful communication
and social connection which may enhance their quality of life.
In the medical setting, we often add complimentary sessions of CRG-Fullerton to an
individuals weekly program as part of his/her discharge planning. CRG-Fullerton supports the
often delicate transition from outpatient services to community re-entry, and often serves to
encourage individuals as they meet other PWA have travelled further down the road of improvement.
The additional social network of friends which develops also appears to aid recovery. In the university
111
Downloaded From: http://sig2perspectives.pubs.asha.org/pdfaccess.ashx?url=/data/journals/ashannsld/930947/ on 09/19/2017
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
setting, CRG-SAC also supports PWA in their transition from formal on-campus clinic services
to a community-based program. Both programs provide a much needed outlet for PWA in the
community.
References
Albrecht, G. L., Seelman, K. D., & Bury, M. (2001). Handbook of Disability Studies. Thousand Oaks, CA:
Sage Publications, Inc.
American Medical Association. (2007). From the Centers for Disease Control and Prevention: Prevalence of
Stroke -United States, 2005. Journal of the American Medical Association, 298(3), 279281.
American Speech Language Hearing Association. (2007). Scope of Practice in Speech-Language Pathology
[Scope of Practice]. Available from www.asha.org/policy
Aphasia Institute (n.d.a.). DVD: Supported Conversation for Adults with Aphasia. Retrieved from http://www.
aphasia.ca/shop/dvd-supported-conversation-for-adults-with-aphasia/
Bernstein-Ellis, E., & Elman, R. (1999). Aphasia group communication treatment: The Aphasia Center of
California approach. In R. Elman (Ed.) Group treatment of neurogenic communication disorders: The expert
clinicians approach (pp. 4756). Boston: Butterworth-Heinemann.
California State University Sacramento (CSUS; n.d.a.). Graduation Initiative Strategic Plan. Retrieved from
http://saweb.csus.edu/students/download/GraduationInitiativeReportOctober21.pdf
Centers for Disease Control and Prevention. (2013). Healthy Communities Program. Retrieved from http://
www.cdc.gov/nccdphp/dch/programs/healthycommunitiesprogram/
Centers for Medicare & Medicaid Services. (2014). Therapy Cap. Retrieved from http://www.cms.gov/
Research-Statistics-Data-and-Systems/Monitoring-Programs/Medicare-FFS-Compliance-Programs/
Medical-Review/TherapyCap.html
Chapey, R., Duchan, J., Elman, R., Garcia, L., Kagan, Lyon, J., & Simmons-Mackie, N. (2000). Life
participation approach to aphasia: A statement of values for the future. ASHA Leader, 5(3), 46.
Commission on Accreditation of Rehabilitation Facilities (CARF; 2012). CARF: Accreditation Focuses on
Quality, Results. Retrieved from www.carf.org/home/
Elman, R. (2011). Starting an aphasia center? Seminars in Speech and Language, 32, 268272.
Elman, R., & Bernstein-Ellis, E. (1999). The efficacy of group communication treatment in adults with
chronic aphasia, Journal of Speech and Hearing Research, 42(2), 411419.
Garrett, K. L., & Beukelman, D. R. (1992). Augmentative communication approaches for persons with severe
aphasia. In K. Yorkston (Ed.) Augmentative communication in the medical setting (pp. 245338). Tucson, AZ:
Communication Skill Builders.
Glista, S., & Pollens, R. (2007). Educating clinicians for meaningful, relevant and purposeful aphasia group
therapy. Topics in Language Disorders, 27(1), 351371.
Hagge, D., Heard, M., Williams, L., & Vickers, C. (2014). Training aphasia group student volunteers: Virtual
file access and storage. Poster presentation for the California Speech-Language-Hearing Association, March
2014, San Francisco, CA.
Hilari, K., & Northcott, S. (2006). Social support in people with chronic aphasia. Aphasiology, 20(1), 1736.
Kagan, A., Black, S., Duchan, J., Simmons-Mackie, N., & Square, P. (2001) Training volunteers as
conversation partners using Supported conversation for adults with aphasia (SCA): A controlled trial,
Journal of Speech, Language and Hearing Research, 44, 624638.
Kaplan, D. (2000). The definition of disability: Perspective of the disability community. Journal of Health
Care Law and Policy, 3(2), 352364.
Klein, K. (1996). Coping With the End of Third-Party Reimbursement for Individual Speech-Language
Pathology Services. National Aphasia Association Newsletter, 8, 2. Retrieved from http://www.aphasia.org/
article-naacoping.php
Lee, S., Funes, B., Vickers, C., & Hagge, D. (2013). Technology and aphasia groups: Enhancing participation.
A poster session presented at the American Speech-Language-Hearing Association, November, 2013,
Chicago, IL.
112
Downloaded From: http://sig2perspectives.pubs.asha.org/pdfaccess.ashx?url=/data/journals/ashannsld/930947/ on 09/19/2017
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
Lyon, J. (1992) Communication use and participation in life for adults with aphasia in natural settings: The
scope of the problem. American Journal of Speech Language Pathology, 1(3), 714.
Lyon, J. (1995). Drawing: Its value as a communicative aid for adults with aphasia. Aphasiology, 9, 3394.
Lyon, J. (1997). Volunteers and partners: Moving intervention outside the treatment room. In B. Shadden
(Ed.) Aging and Communication: For Clinicians by Clinicians (pp. 299323). Austin, TX: Pro-Ed.
Lyon, J. (1998a). Coping with aphasia. San Diego: Singular Publishing.
Lyon, J. (1998b). Treating real life functionality in a couple coping with severe aphasia. In N. Helm-Estabrooks
& A. Holland (Eds.) Approaches to the treatment of aphasia (pp. 203239). San Diego: Singular Publishing.
McCall, D. (2012). Steps to success with technology for individuals with aphasia. Seminars in Speech and
Language, 33(3), 234242.
National Aphasia Association. (2009). Lookin for me. DVD. Available at http://www.aphasia.org/content/
lookin-me
National Aphasia Association. (2009). Its Still Me! DVD. Available at http://www.aphasia.org/content/its-
still-me
National Aphasia Association. (2011). Welcome to Groups & Programs! Retrieved from www.aphasia.org/
Neuburger, S., Frison, C., & Crowley, R., National Aphasia Association. (1997). [VHS videotape]. Available
from www.aphasia.org/catalog/multimedia
Northcott, S., & Hilari, K. (2011). Why do people lose their friends after stroke? International Journal of
Language and Communication Disorders, 46(5), 524534.
Pound, C., Parr, S., Lindsay, J., & Woolf, C. (2000). Beyond aphasia; Therapies for living with communication
disability. United Kingdom: Winslow.
Rayner, H., & Marshall, J. (2003). Training volunteers as conversation partners for people with aphasia.
International Journal of Language and Communication Disorders, 38(2), 149164.
Simmons-Mackie, S., & Holland, A. L. (2011). Aphasia Centers in North America: A survey. Seminars in
Speech and Language, 32(3), 203215.
Silverman, M. (2011). Community: the key to building and extending engagement for individuals with
aphasia. Seminars in Speech and Language, 32(3), 256267.
St. Joseph Health System: St. Jude Medical Center (2014). Retrieved from http://www.stjudemedicalcenter.
org/For-Community.aspx
Vickers, C. (1998). Communication Recovery: Group conversation activities for adults. San Antonio, TX:
Communication Skill Builders.
Vickers, C. (2010). Social networks after the onset of aphasia: The impact of aphasia group attendance.
Aphasiology, 24(68), 902913.
Vickers, C., & Hagge, D. (2013, May). Tracking social connection versus isolation in aphasia. Poster
presentation for the Clinical Aphasiology Conference, Tucson, AZ.
Vickers, C., & Mehta, S. (2012, Nov). Mobile technology: Impact on conversational interactions. Poster
presentation for the American Speech Language Hearing Association, Atlanta, GA.
Williamson, D., Richman, M., & Redmond, S. (2011). Applying the correlation between aphasia severity and
quality of life measures to a life participation approach to aphasia. Topics in Stroke Rehabilitation, 18(2),
101105.
World Health Organization. (2001). International classification of functioning, disability and health (ICF).
Geneva, Switzerland: World Health Organization, Author.
113
Downloaded From: http://sig2perspectives.pubs.asha.org/pdfaccess.ashx?url=/data/journals/ashannsld/930947/ on 09/19/2017
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
Alternative Service Delivery Model: A Group Communication
Training Series for Partners of Persons with Aphasia
Darla Hagge
Department of Speech Language Pathology, California State University Sacramento
Sacramento, CA
Financial Disclosure: Darla Hagge is an Assistant Professor at California State University
Sacramento.
Nonfinancial Disclosure: Darla Hagge has previously published in the subject area.
Abstract
Providing education and partner training for the primary communication partners of
persons with aphasia is often challenging for medical-based speech-language pathologists
(SLPs). Todays healthcare environment is fraught with barriers to obtaining services for
individuals with aphasia and their significant others. This article describes a proposed
alternative service delivery model for the partners of persons with aphasia.
Aphasia impacts the communication of a person with aphasia (PWA) but its presence may
also negatively affect the significant other (SO) of the PWA, including permanent life changes and
health-related issues such as depression or anxiety. The World Health Organization (WHO, 2001)
refers to this phenomenon as a third-party disability and calls for continued research in this
area. This line of inquiry is imperative because the supporting SO may be the most critical person
in the PWAs life (Threats, 2010).
Formal Therapy Sessions
A variety of accreditation agencies publish policies that mandate family-inclusive therapy
services (Commission on Accreditation of Rehabilitation Facilities [CARF], 2012; The Joint
Commission, 2010). Speech-language pathologists (SLPs) reportedly agree on the importance of
integrating family members in direct patient care, and providing partner education and training
services (Johansson, Carlsson, & Sonnander, 2012; Vickers, Hagge, & Tsuma, 2005).
Nevertheless, many SLPs continue to provide intervention primarily to the PWA, while providing
only nominal attention to the partner (Johansson, Carlsson, & Sonnander, 2011; Threats, 2010).
This reveals a disparity between formally established policy and the application of policy in
therapeutic practices, and may occur because of several barriers.
First, third-party payers limit the frequency and duration of therapy sessions and often
deny requests for additional sessions. As a result, the clinician must determine the most effective
plan of care given only 68 sessions, and may design an impairment-focused care plan rather
than including partner education and training. Second, SLPs must provide evidence-based
intervention. Although there are data supporting the efficacy of a variety of partner education and
training programs (Simmons-Mackie, Raymer, Armstrong, Holland, & Cherney, 2010),
commercially available standardized programs are limited. Third, reimbursement from third-
party payers is contingent on outcome measures. Although communication tools are published
across the literature, there are no standardized outcome measures that are consistently
administered to evaluate partner training. Finally, graduate program curriculums may not
include partner training for PWA. If provided, graduate training programs may offer inconsistent
or limited training (Vickers, Hagge, & Tsuma, 2005).
114
Downloaded From: http://sig2perspectives.pubs.asha.org/pdfaccess.ashx?url=/data/journals/ashannsld/930947/ on 09/19/2017
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
An Alternative Service Delivery Model
One possible response to the current healthcare climate is the purposeful creation of
alternative service delivery models for adults with acquired neurogenic disorders or third-party
disability. Individuals with disabilities may have decreased access to healthcare services and as a
result live with unmet health care needs (WHO, 2013, p. 1). Recommended ways to mitigate
these healthcare disparities include the provision of information, training, and peer support
through a variety of vehicles including communication-based rehabilitation or alternative
service delivery models (WHO, 2013, p. 1). Further, the WHO (2013) purports the value of
identifying those populations who need alternative service delivery models and within these
models to provide creative ways to identify the participants needs and support the coordination
of formal services. ASHA acknowledges that with the evolving implementation of the Affordable
Care Act, new community service programs may increasingly become viable alternatives (ASHA,
2014; CMS, 2014).
Communication Training Series
In an effort to meet the needs of the SOs of PWA, a weekly 2 hour group communication
training series was offered to the primary communication partners of PWA for six weeks (Hagge,
2012). A convenience sample was used to recruit participants, who were randomly-assigned into
the treatment or a wait-listed/comparison group. A SLP specializing in aphasia facilitated the
communication training series (Vickers, 2002).
A learner-centered approach was chosen and principles from the field of adult education
informed the use of teaching strategies. Similarly, the curriculum for the communication training
series was guided by the literature. For example, researchers report that the partners of PWA
desire the following: (a) written and oral information regarding aphasia, (b) learned skills
including role changes and communication strategies, and (c) support such as self-care and
opportunities to meet other families living with aphasia (Dalemans, de Witte, Wades, & van den
Heuvel, 2010; Manders, Marien, & Janssen, 2011).
Each weekly session included a variety of activities, including a reflection task, direct
instruction, group discussion, and a hands-on activity. The communication tools and strategies
that were presented during each weekly session were designed to support the assigned homework
activities (Boles, 2010). Ongoing opportunities for individual reflection, small group interactions
and sharing, and whole group discussions were also used each week.
By using a group training program, it was expected that the partners would benefit from
ongoing peer support and/or experience a decrease in social isolation. For example, two bilingual
partners who met during the training series were seen walking the halls together during the
breaks, holding hands, laughing, and chatting.
Concurrent Program for PWAs
In an effort to support recruitment, concurrent aphasia-friendly conversation groups were
provided as an attendance option for the individuals with aphasia. Many of the PWA attended
these conversation groups while their primary communication partners participated in the
communication training series. Eighty percent of the partners with aphasia attended the
conversation groups regularly.
Although not a formal component of the study, the conversation group provided an
optional concurrent activity to support the partners participation in the treatment group (Sterner
et al., 2012). Partners expressed appreciation and value for the conversation aphasia groups.
Further, many of the partners expressed satisfaction in knowing their PWAs were laughing and
socializing with others while they attended the series.
115
Downloaded From: http://sig2perspectives.pubs.asha.org/pdfaccess.ashx?url=/data/journals/ashannsld/930947/ on 09/19/2017
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
Weekly Survey Results
A total of 38 dyads were initially enrolled in the study. Each dyad consisted of a PWA and
the SO. Dyads were randomly assigned to either the treatment (n = 20 dyads) or comparison
(n = 18 dyads) groups. The treatment group attrition rate was 1 dyad, and the comparison group
attrition rate was 5 dyads (see Figure 1). The participants completed a satisfaction survey at the
conclusion of each weekly training meeting. The participants weekly survey responses were
positive and indicated a valued learning experience (Table 1).
Figure 1. Participant Retention Rate for Treatment and Comparison Groups.
Table 1. Summary-Six Week Communication Training Series Weekly Survey.
Survey Statement Strongly Agree Neutral Disagree
Agree
1. Todays session was informative. 48% 50% 2% 0%
2. I enjoyed talking with other spouses/partners. 50% 46% 4% 0%
3. I learned a communication strategy to use with my partner 35% 45% 16% 4%
with aphasia.
4. I experienced a new insight during todays session. 44% 42% 12% 2%
5. I would recommend this session to other partners of 65% 34% 1% 0%
persons with aphasia.
Conclusion
Clearly, healthcare and the traditional service delivery model will continue to evolve and
change over time. It is likely that alternative service delivery models will become an integral
vehicle for speech-language pathology services. A group-based communication training series for
the partners of PWA may offer a viable option for partner education and training. In addition to
the core training curriculum, a group program may provide partners with peer support and
learning, as well as supporting the coordination of care including referrals.
116
Downloaded From: http://sig2perspectives.pubs.asha.org/pdfaccess.ashx?url=/data/journals/ashannsld/930947/ on 09/19/2017
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
References
American Speech-Language-Hearing Association. (2014). Providing More Community-Based Care. Retrieved
from http://www.asha.org/practice/Health-Care-Reform/Providing-More-Community-Based-Care/
Boles, L. (2010). Aphasia couples therapy (ACT) workbook. San Diego, CA: Plural Publishing.
Centers for Medicare & Medicaid Services. (2014). Community-Based Long-Term Services & Supports.
Retrieved from http://www.medicaid.gov/AffordableCareAct/Provisions/Community-Based-Long-Term-
Services-and-Supports.html
Commission on Accreditation of Rehabilitation Facilities. (2012). CARF: Accreditation focuses on quality,
results. Retrieved from http://www.carf.org/home/
Dalemans, R., de Witte, L., Wades, D., & van den Heuvel, W. (2010). Social participation through the eyes of
people with aphasia. International Journal of Language & Communication Disorders, 45(5), 537550.
Hagge, D. (2012). Partners of persons with aphasia: Communication training series and quality of life
(Unpublished doctoral dissertation). Chapman University, Orange, CA
Johansson, M. B., Carlsson, M., & Sonnander, K. (2012). Communication difficulties and the use of
communication strategies: From the perspective of individuals with aphasia. International Journal of
Language and Communication Disorders, 47(2), 144155.
Manders, E., Marien, A., & Janssen, V. (2011). Informing and supporting partners and children of persons
with aphasia: A comparison of supply and demand. Logopedics Phoniatrics Vocology, 36(4), 139144.
Simmons-Mackie, N., Raymer, A., Armstrong, E., Holland, A., & Cherney, L. R. (2010). Communication partner
training in aphasia: A systematic review. Archives of physical medicine and rehabilitation, 91, 18141836.
Sterner, A., Wenkart, P., Ayala, K., Helfrich, S., Junyk, K., Leon, A., . . . Hagge, D. (2012). Student volunteers
and nonfluent aphasia: Creating thematic conversation activities. A poster session presented at the American
Speech-Language-Hearing Association National Convention, Atlanta, GA.
The Joint Commission. (2010). The Joint Commission: Advancing Effective Communication, Cultural
Competence, and Patient- and Family-Centered Care: A Roadmap for Hospitals. Oakbrook Terrace, IL.
Retrieved from http://www.jointcommission.org/roadmap_for_hospitals/
Threats, T. T. (2010). The ICF framework and third party disability: Application to the spouses of persons
with aphasia. Topics in Stroke Rehabilitation, 17(6), 451457.
Vickers, C. (2002). Help for couples coping with aphasia: A partner training series. Unpublished raw data
Vickers, C., Hagge, D., & Tsuma, N. (2005). Availability of partner training for couples coping with aphasia.
Poster session presented at the American Speech- Language-Hearing Association National Convention,
San Diego, CA.
World Health Organization. (2013). Disability and Health. Retrieved from http://www.who.int/mediacentre/
factsheets/fs352/en/#
World Health Organization. (2001). International Classification of Functioning, Disability, and Health. Geneva:
WHO.
117
Downloaded From: http://sig2perspectives.pubs.asha.org/pdfaccess.ashx?url=/data/journals/ashannsld/930947/ on 09/19/2017
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Pathophysiology of GooDocument2 pagesPathophysiology of GooTania Noviza100% (1)
- Pharmacology HandoutDocument5 pagesPharmacology HandoutMark Elben Teodoro100% (1)
- Drug Dosage Calculations NCLEX Exam 4Document4 pagesDrug Dosage Calculations NCLEX Exam 4Heather ClemonsNo ratings yet
- Neligan Vol 3 Chapter 03 MainDocument55 pagesNeligan Vol 3 Chapter 03 MainisabelNo ratings yet
- NSO Monthly Report FormDocument5 pagesNSO Monthly Report Formrose_almonteNo ratings yet
- Case Study FormatDocument6 pagesCase Study FormatChristian LlerinNo ratings yet
- Guideline Massive PPHDocument27 pagesGuideline Massive PPHSarah SabrinaNo ratings yet
- Sitting Balance ScaleDocument4 pagesSitting Balance ScaleFaishol Reza AdiyaksaNo ratings yet
- PQCNC New Initiative Proposal CLABSIDocument17 pagesPQCNC New Initiative Proposal CLABSIkcochranNo ratings yet
- Rights and Obligations of PatientsDocument10 pagesRights and Obligations of PatientsRey BenítezNo ratings yet
- Muscle Grading and Testing ProceduresDocument5 pagesMuscle Grading and Testing Proceduresshodhganga100% (1)
- Congenital Muscular TorticollisDocument5 pagesCongenital Muscular TorticollisKevin Paul ZuñigaNo ratings yet
- Circulating SerotoninDocument17 pagesCirculating Serotoninnihilx27374No ratings yet
- Did You Know?: Nama: Alfa Innersia Zahada NIM: 1897194042 Prodi: Pend. Bahasa Inggris A Semester: 2Document2 pagesDid You Know?: Nama: Alfa Innersia Zahada NIM: 1897194042 Prodi: Pend. Bahasa Inggris A Semester: 2Abu Bakar Ar-Rasa'ilNo ratings yet
- Attachments For Removable Partial Dentures Prostho 6Document10 pagesAttachments For Removable Partial Dentures Prostho 6Melika DNo ratings yet
- Hiv 101Document33 pagesHiv 101Hend Al-RamahiNo ratings yet
- 12 Little Known Facts About CoffeeDocument3 pages12 Little Known Facts About CoffeeBulgare de SoareNo ratings yet
- Bartolo Renjie Daniel CDocument8 pagesBartolo Renjie Daniel CAlexa Anne Louise BercillaNo ratings yet
- Infection ControlDocument6 pagesInfection ControlhiyahninjaNo ratings yet
- Effects of Adoption 1Document10 pagesEffects of Adoption 1api-353918742No ratings yet
- Truncus ArteriosusDocument4 pagesTruncus ArteriosuskemalahmadNo ratings yet
- Ab Population Health Disparities Module 1Document4 pagesAb Population Health Disparities Module 1api-643329064No ratings yet
- Rachelle Manuel PobleteDocument4 pagesRachelle Manuel PobleteRachelle MondidoNo ratings yet
- Pub1566 WebDocument124 pagesPub1566 WebRadoi Sandina RodicaNo ratings yet
- Physician Assisted Suicide (Pros & Cons, Arguments For and Against, Advantages & Disadvantages of Euthanasia or Doctor-Assisted Suicice)Document5 pagesPhysician Assisted Suicide (Pros & Cons, Arguments For and Against, Advantages & Disadvantages of Euthanasia or Doctor-Assisted Suicice)Lyana MahaliNo ratings yet
- Advanced Diagnostic AidsDocument54 pagesAdvanced Diagnostic AidsAhmed Tawfig GamalNo ratings yet
- Tissue PerfusionDocument2 pagesTissue Perfusionnursezey100% (3)
- SSJ TenDocument5 pagesSSJ TenSelviana SudarmanNo ratings yet
- Fixed AppliencieswebDocument48 pagesFixed Appliencieswebabcder1234No ratings yet
- Dr. Qadeer's CV PDFDocument1 pageDr. Qadeer's CV PDFQadeermwmNo ratings yet