Professional Documents
Culture Documents
Clinical Medicine - Lecture: - Topic: - Date
Uploaded by
qselmm0 ratings0% found this document useful (0 votes)
56 views3 pagesComparison between Thalassemia alpha and beta
Original Title
Thalassemias Chart
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentComparison between Thalassemia alpha and beta
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
56 views3 pagesClinical Medicine - Lecture: - Topic: - Date
Uploaded by
qselmmComparison between Thalassemia alpha and beta
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 3
Clinical Medicine Lecture: _____ Topic: ____________________________________________________________ Date: ______________
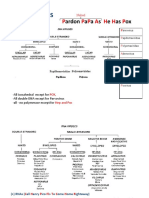
Alpha Thalassemias Beta Thalassemias
Hereditary anemias (autosomal recessive inheritance) characterized by Hereditary anemias (autosomal recessive inheritance) characterized by
reduced or absent production of 1 or more of the alpha globulin chains: reduced or absent production of 1 or more of the beta globulin chains:
1. Alpha Thalassemia Silent Carrier (Alpha Thalassemia Minima) Normal: beta/beta (homozygous beta, normal normal), neither + nor
o No clinical abnormalities may be hematologically normal or have 0
slight reductions in MCV and MCH 1. Beta Thalassemia Minor
o 3 functional alpha globin genes o Heterozygous beta/beta0
2. Alpha Thalassemia Minor (Alpha Thalassemia Trait) Production = 50% of normal
o Clinically normal, but frequently have minimal microcytic, o Heterozygous beta/beta+
Etiology hypochromic anemia and reduced MCV and MCH (RBC count is Production = close but not normal
(Pathophysiology): usually increased >5.5x1012/L) 2. Beta Thalassemia Intermedia
o 2 functional alpha globin genes o Homozygous beta+/beta+
3. Hemoglobin H Disease (Alpha Thalassemia Intermedia) High rate of beta globin synthesis (but not as good as beta/beta+)
o Moderate to severe alpha thalassemia 3. Beta Thalassemia Major (Cooley Anemia)
o 1 functional alpha globin genes o Homozygous beta+/beta+
4. Hydrops Fetalis Very low rate of beta globin synthesis
o Most severe (almost all fetuses die in utero) all 4 alpha globin o Homozygous beta0/beta0
genes are missing Absent beta globin synthesis
o 0 functional alpha globin genes Beta+ results in an increase in the proportions of Hemoglobin A2 and F
Alpha thalassemias with 2 missing genes on a given allele are more Most commonly reported in Mediterranean, African, and Southeast
Risk Factors common in Asian ancestry Asian populations
(Demographics): Ancestry from regions where malaria is endemic (Asian, Mediterranean,
or Middle Eastern descent)
Clinical Typical S/S of anemia for Silent Carrier and Trait Beta Thalassemia Intermedia and Cooley Anemia (Beta Thalassemia
Manifestations In Hemoglobin H Disease, symptoms are consistent with a chronic Major) are normal at birth, but 6 mo. = Lifelong Hemolytic State
(Signs and hemolytic anemia o Cooley Anemia is a severe anemia requiring transfusion, whereas
Symptoms): o Episodes of severe pallor and anemia Beta Thalassemia Intermedia usually only requires transfusions
o Exacerbations of hemolysis may occur when patients are exposed to during stress or during aplastic crises
stressors (pregnancy, infections, fever, ingestion of oxidative o Both are associated with hepatosplenomegaly and bony deformities
compounds, or drug use) o In Cooley Anemia, also have stunted growth, jaundice, and
o History of transfusions to treat the above thrombophilia
Beta Thalassemia Minor is clinically insignificant
Complications can include the following: o Lifelong hemolytic, mild, microcytic anemias
o Hepatosplenomegaly
o Leg ulcers
o Gallstones
o Prominent frontal bossing
o Marked overgrowth of the maxillae
o Ribs and long bones becoming boxlike and convex
o Premature closure of epiphyses resulting in shortened limbs
o Osteopenia and fractures
o Intellectual disability syndromes
Diagnostic Studies: 1. CBC 1. CBC
o Silent Carrier o Beta Thalassemia Minor
Hgb normal Hgb 10-12 g/dL
MCH normal (27-33 pg/cell) to slightly decreased (~26 pg/cell) Hct 20-40%
MCV normal (80-96 fL/cell) to slightly decreased (75-85 MCV 55-75 fL
fL/cell) RBC count normal or increased
o Trait o Beta Thalassemia Intermedia
Hgb normal Hgb 6-11 g/dL
MCH more decreased than silent carrier (22 pg) Hct 17-33%
MCV more decreased than silent carrier (65-75 fL) MCV 55-75 fL
o Hemoglobin H Disease RBC count normal or increased
Hgb moderate to severe decrease (7-10 g/dL) o Beta Thalassemia Major (Cooley Anemia)
MCH more decreased than trait (55-65 fL) Hgb may be <3 g/dL
MCV more decreased than trait (20 pg) Hct may be <10%
o Hydrops Fetalis MCV <55 fL
Hgb severe decrease (~44 g/dL) 2. Peripheral Smear and Reticulocytes
MCV increased (110-120 fL) o RBC Appearance microcytic, hypochromic (or normochromic)
2. Peripheral Smear and Reticulocytes Beta Thalassemia Minor mildly abnormal: above + target cells
o RBC Appearance microcytic, hypochromic Beta Thalassemia Intermedia abnormal: above + basophilic
In hemoglobin H Disease get small misshapen red cells, stippling
hypochromia, microcytosis, and targeting. With brialliant Beta Thalassemia Major (Cooley Anemia) bizarre: above +
cresyl blue stain with see Hb H inclusion bodies. severe microcytosis (very pale), severe poikilocytosis, and
o Reticulocytes Too many: good marrow response to RBC loss or nucleated RBCs
destruction BY MARROW THAT HAS BUILDING BLOCKS (iron, o Reticulocytes Too many: good marrow response to RBC loss or
etc.) destruction BY MARROW THAT HAS BUILDING BLOCKS AND
Silent Carrier normal (not decreased) RESPONDING TO HEMOLYSIS
Trait normal (not decreased) Beta Thalassemia Minor normal or slightly elevated
Hemoglobin H Disease 5-10% elevated (the higher the count, Beta Thalassemia Intermedia elevated
the more severe the hemolysis) Beta Thalassemia Major (Cooley Anemia) elevated
3. Iron Studies should be NORMAL 3. Iron Studies should be NORMAL
o Microcytic, hypochromic + NL iron studies = order 4. Hemoglobin electrophoresis Abnormal (DIAGNOSTIC)
electrophoresis! Might be thalassemia!! 5. Prenatal Diagnosis
4. Hemoglobin electrophoresis Abnormal (quantitates and identifies o DNA analysis for the presence of thalassemia mutation of chorionic
different hemoglobin types) villi at 8-10 weeks gestation or amniocentesis at 14-20 weeks.
o Hydrops fetalis
Hemoglobin Barts 80%
Hemoglobin Portland 10-20%
Hemoglobin H 0-10%
o Hemoglobin H Disease
Hemoglobin Barts/H at birth, 25-40% of hemoglobin is
Hemoglobin Barts (decreases later and is replaced by excess
Hemoglobin H)
Remainder is Hemoglobin A, A2, and F
o Trait
Hemoglobin A 85-95%
Hemoglobin Barts 5-15% at birth
No significant Hemoglobin A2, F, or H
o Silent carriers
Hemoglobin A 96-98%
Hemoglobin Barts 0-2% at birth
Hemoglobin A2 low or normal amounts
No significant Hemoglobin F or H
5. Alpha Thalassemia Mutations Panel
o Definitive/Gold Standard
6. Other
o Indirect hyperbilirubinemia, elevated lactate dehydrogenase levels,
reduced haptoglobin
o Imaging studies ultrasonography of the liver, gallbladder, and
spleen (hepatosplenomegaly and gallstones are common in
Hemoglobin H Disease)
If mild, (trait and silent carriers) may not need treatment Beta Thalassemia Minor and Intermedia often do not require any specific
If severe anemia (<7 g/dL), may require lifelong transfusion therapy treatment (may require transfusion support)
o Hemoglobin H Beta Thalassemia Major (Cooley Anemia) will require chronic
PRBC transfusion therapy transfusion therapy (goal is to maintain hemoglobin at 9-10 g/dL) with
Allogeneic hematopoietic stem cell transplantation curative iron chelation to prevent transfusional iron overload (hemosiderosis),
Treatment (First & o Hydrops fetalis which results in a clinical picture similar to hemochromatosis
Second Line): Requires uterotransfusions for survival and then continued o Splenectomy
lifelong transfusions o Cholecystectomy
Allogeneic hematopoietic stem cell transplantation (curative) if o Allogenic bone marrow or hematopoietic transplantation may be
survive after birth curative in some patients
If symptoms of hypersplenism, splenectomy (Hemoglobin H) o Supportive measures diet and activity
o Other emerging therapies
Hematology for all, esp. Hemoglobin H Disease and Hydrops fetalis Hematology for all, esp. for Beta Thalassemia Major (Cooley Anemia)
Referral:
Genetic counseling for all
You might also like
- DNA Viruses: P P P A H H PDocument2 pagesDNA Viruses: P P P A H H PKimberly KanemitsuNo ratings yet
- Indoor Air Quality AnalysisDocument21 pagesIndoor Air Quality AnalysisAshmit DubeyNo ratings yet
- HT 43 Jan PDFDocument36 pagesHT 43 Jan PDFSohail LatifNo ratings yet
- Decreased Levels of Iron by Diet or Hemorrhage Impaired Heme SynthesisDocument8 pagesDecreased Levels of Iron by Diet or Hemorrhage Impaired Heme SynthesisSamuel RothschildNo ratings yet
- Pathology - Lab: Pathology of The HeartDocument8 pagesPathology - Lab: Pathology of The HeartRazel PerezNo ratings yet
- 15 - Toronto Notes 2011 - HematologyDocument58 pages15 - Toronto Notes 2011 - HematologyWaiwit Chotchawjaru100% (1)
- Table of Genetic Disorders: Download A Copy of This Study GuideDocument11 pagesTable of Genetic Disorders: Download A Copy of This Study Guideerica perezNo ratings yet
- Cocci Rod 4 Main Classifications: Gram Staph, Strep Bacillus Clostridium Neisseria Pleiomorphic Enterobact-EriceaeDocument2 pagesCocci Rod 4 Main Classifications: Gram Staph, Strep Bacillus Clostridium Neisseria Pleiomorphic Enterobact-EriceaeKimberly KanemitsuNo ratings yet
- Leukemia and Lymphoma OverviewDocument2 pagesLeukemia and Lymphoma OverviewAyeshaArifNo ratings yet
- Lymphomas and Leukemias ChartDocument2 pagesLymphomas and Leukemias ChartPA2014No ratings yet
- Liver Function Tests Diagnostic GuideDocument2 pagesLiver Function Tests Diagnostic GuideostarburstoNo ratings yet
- Pathology B - Gastrointestinal Tract (Esguerra, 2015)Document18 pagesPathology B - Gastrointestinal Tract (Esguerra, 2015)Ars MoriendiNo ratings yet
- OPTOMED-HW2-Diabetic Retinopathy PDFDocument3 pagesOPTOMED-HW2-Diabetic Retinopathy PDFDanalie SalvadorNo ratings yet
- Pharmacology of EthanolDocument5 pagesPharmacology of EthanolJoshua RemonNo ratings yet
- Chart - WBC DisordersDocument1 pageChart - WBC DisordersSamuel RothschildNo ratings yet
- Uw Step 2 CK Im H ODocument67 pagesUw Step 2 CK Im H OAilyn MNo ratings yet
- Ophthalmology Explorer 1st EditionDocument373 pagesOphthalmology Explorer 1st EditionAaron French100% (3)
- Endocrine ChartDocument28 pagesEndocrine ChartNiki NikolićNo ratings yet
- Hematology SummaryDocument9 pagesHematology SummaryJovielle Hayden100% (1)
- WBC Lymph Node SpleenDocument12 pagesWBC Lymph Node Spleendr brijesh TiwariNo ratings yet
- Provision MCQ by Dr. Osama ShalabyDocument5 pagesProvision MCQ by Dr. Osama Shalabyapi-383014680% (10)
- Heart Failure - Notes From "Cardiology" (Timmis Et Al) : Main CausesDocument3 pagesHeart Failure - Notes From "Cardiology" (Timmis Et Al) : Main CausesPrarthana Thiagarajan100% (3)
- Nephrotic Nephritic SyndromsDocument4 pagesNephrotic Nephritic SyndromsKimiwari100% (2)
- Pathology Finals Reviewer on WBCs, Lymph Nodes, Spleen & ThymusDocument5 pagesPathology Finals Reviewer on WBCs, Lymph Nodes, Spleen & Thymusangel_sagun_1No ratings yet
- 3-7 Osteoarthritis ThumbDocument58 pages3-7 Osteoarthritis ThumbProfesseur Christian Dumontier100% (3)
- Complement SystemDocument4 pagesComplement SystemFait HeeNo ratings yet
- Genetic and Pediatric Diseases Chapter SummaryDocument16 pagesGenetic and Pediatric Diseases Chapter SummaryJustine HungNo ratings yet
- Phylum NematodaDocument285 pagesPhylum NematodaBrielleNo ratings yet
- Hem-Onc: AnswerDocument3 pagesHem-Onc: AnswerAman Raj KNo ratings yet
- Concise SEO-Optimized Title for Clotting DocumentDocument3 pagesConcise SEO-Optimized Title for Clotting DocumentRyan TurnerNo ratings yet
- Antenatal Care & ManagementDocument23 pagesAntenatal Care & ManagementPabhat Kumar100% (1)
- Micro Buzz Words - KEY WordsDocument8 pagesMicro Buzz Words - KEY WordsKris GulleyNo ratings yet
- Sources of Parasitic InfectionDocument74 pagesSources of Parasitic InfectionCristy Jean100% (1)
- HaematinicsDocument2 pagesHaematinicsGerardLum100% (2)
- Test CentreDocument178 pagesTest CentreShaik Nizam Uddin100% (1)
- Community Health Nursing Questions ADocument11 pagesCommunity Health Nursing Questions AFleur Jenne100% (1)
- Clinical Medicine - Lecture: - Topic: - DateDocument2 pagesClinical Medicine - Lecture: - Topic: - DateqselmmNo ratings yet
- Anemia Type Pathogenesis Clinical Manifestations Diagnosis Peripheral Blood Lab FindingsDocument15 pagesAnemia Type Pathogenesis Clinical Manifestations Diagnosis Peripheral Blood Lab FindingsDanielle FosterNo ratings yet
- ENDOCRINE PATHOLOGY WebpathDocument35 pagesENDOCRINE PATHOLOGY Webpathapi-3766657No ratings yet
- Haematology-Summary My NotesDocument24 pagesHaematology-Summary My NotesToria053No ratings yet
- AtelectasisDocument3 pagesAtelectasisLouis FortunatoNo ratings yet
- Acute Myeloproliferative Acute Lymphoproliferative Chronic Myeloproliferative Chronic Lymphoproliferative Plasma Cell NeoplasmDocument1 pageAcute Myeloproliferative Acute Lymphoproliferative Chronic Myeloproliferative Chronic Lymphoproliferative Plasma Cell NeoplasmAudreySlitNo ratings yet
- Diseases - BiochemDocument4 pagesDiseases - BiochemJay FeldmanNo ratings yet
- Heamtology Reviewer (Midterm)Document15 pagesHeamtology Reviewer (Midterm)Johney DoeNo ratings yet
- Overview of AnaemiaDocument2 pagesOverview of AnaemiaGerardLumNo ratings yet
- Dr. A. Samy TAG Bone Diseases - 1Document2 pagesDr. A. Samy TAG Bone Diseases - 1Herato MenaNo ratings yet
- Pathology - Chapter 14Document14 pagesPathology - Chapter 14Cory GrayNo ratings yet
- Malassezia Furfur An-An Ap-Ap Naturally Found On The SkinDocument48 pagesMalassezia Furfur An-An Ap-Ap Naturally Found On The SkinNikki ValerioNo ratings yet
- 4.1d - Pathology of The Pituitary - Nov.10 - Dr. GalangDocument4 pages4.1d - Pathology of The Pituitary - Nov.10 - Dr. GalangMiel Raphael AranillaNo ratings yet
- Respi PhysioDocument7 pagesRespi PhysioAmal JohnsonNo ratings yet
- Breast CancerDocument6 pagesBreast Cancersarguss14No ratings yet
- Pediatrics SamplexDocument6 pagesPediatrics SamplexThea SansonNo ratings yet
- Red Blood Cell Disorders Anemia: Anemia Is A Laboratory DiagnosisDocument3 pagesRed Blood Cell Disorders Anemia: Anemia Is A Laboratory DiagnosisAnonymous 8hJAATBNo ratings yet
- Tumor Markers: Blood Group AntigenDocument5 pagesTumor Markers: Blood Group AntigenAngela ReyesNo ratings yet
- Pathology Description/Buzz Words DiseaseDocument5 pagesPathology Description/Buzz Words Diseasebea manzanoNo ratings yet
- Cell Adaptation and Necrosis: Hypertrophy, Atrophy, MetaplasiaDocument8 pagesCell Adaptation and Necrosis: Hypertrophy, Atrophy, MetaplasiaivankcurryNo ratings yet
- DISC, Drugs, Infection, Thick Basal MembraneDocument5 pagesDISC, Drugs, Infection, Thick Basal MembraneHOPENo ratings yet
- Cardiology Arteritis ChartDocument3 pagesCardiology Arteritis ChartM PatelNo ratings yet
- Midterm Chapter7Document43 pagesMidterm Chapter7Frances FranciscoNo ratings yet
- Small Intestine Lesions Comparison ChartDocument9 pagesSmall Intestine Lesions Comparison ChartfadoNo ratings yet
- (MED II) 1.05 Emergencies in Cancer PatientsDocument17 pages(MED II) 1.05 Emergencies in Cancer PatientsJearwin AngelesNo ratings yet
- UrinalysisDocument9 pagesUrinalysisSukma EffendyNo ratings yet
- Genetic Disorders-Www - Qworld.co - inDocument13 pagesGenetic Disorders-Www - Qworld.co - inQworld100% (1)
- Laboratory Approach To AnemiasDocument23 pagesLaboratory Approach To AnemiasDr. Ashish JawarkarNo ratings yet
- HAEMOPOIESISDocument6 pagesHAEMOPOIESISDiyana ZahariNo ratings yet
- Haematology - Blood Films.Document6 pagesHaematology - Blood Films.kkkssbbNo ratings yet
- Major Bacterial Genera TableDocument12 pagesMajor Bacterial Genera TablemojdaNo ratings yet
- Problem-based Approach to Gastroenterology and HepatologyFrom EverandProblem-based Approach to Gastroenterology and HepatologyJohn N. PlevrisNo ratings yet
- Communicable Disease Table: Southern Luzon State University College of Allied Medicine Lucban, Quezon SY.2017-2018Document11 pagesCommunicable Disease Table: Southern Luzon State University College of Allied Medicine Lucban, Quezon SY.2017-2018Casilda FranciscoNo ratings yet
- Communicable Diseases: Roberto M. Salvador Jr. R.N.,M.D. Infectious and Tropical Disease SpecialistDocument846 pagesCommunicable Diseases: Roberto M. Salvador Jr. R.N.,M.D. Infectious and Tropical Disease SpecialistGrn Mynjrkxz100% (1)
- Standard Treatment GuidelineDocument261 pagesStandard Treatment GuidelineEmaNo ratings yet
- 1000 Genomas RusiaDocument9 pages1000 Genomas RusiaDamarisNo ratings yet
- 353 - Adverbial Clauses Conjunctions Inversion Advanced Level Test Quiz Online Exercise With Answers 1Document5 pages353 - Adverbial Clauses Conjunctions Inversion Advanced Level Test Quiz Online Exercise With Answers 1Dana Elisabeta PironNo ratings yet
- Homeo MedicinesDocument8 pagesHomeo Medicinespjindal000No ratings yet
- 6th Simposium de LutzomyaDocument131 pages6th Simposium de LutzomyaWilfredoNo ratings yet
- Guillain-Barre Syndrome: Practice EssentialsDocument16 pagesGuillain-Barre Syndrome: Practice EssentialsUKMBasketNo ratings yet
- DepEd Minimum Health StandardsDocument33 pagesDepEd Minimum Health StandardsRyan Q. BlancoNo ratings yet
- Survey DesignDocument66 pagesSurvey DesignAbdul HadiNo ratings yet
- PompholyxDocument3 pagesPompholyxSuci Dika UtariNo ratings yet
- Annoted Bibliography ObesityDocument8 pagesAnnoted Bibliography Obesityapi-451532782No ratings yet
- Dry Eye Syndrome OverviewDocument7 pagesDry Eye Syndrome OverviewhaninamaulianiNo ratings yet
- Megaloblastic Anemia PanelDocument5 pagesMegaloblastic Anemia PanelAnggie AnggriyanaNo ratings yet
- (2021) Factors Mediating The PWB of Healthcare Workers Responding To Global Pandemics - A Systematic ReviewDocument22 pages(2021) Factors Mediating The PWB of Healthcare Workers Responding To Global Pandemics - A Systematic ReviewDiyah CandraNo ratings yet
- Non-Contact TonometryDocument6 pagesNon-Contact Tonometrypcorpora409No ratings yet
- Mumps and Red Tide PoisoningDocument4 pagesMumps and Red Tide PoisoningBex LavurghNo ratings yet
- Manual Triage BagusDocument79 pagesManual Triage BagusHengkyNo ratings yet
- Presentation, Interpretation, and Analysis of DataDocument24 pagesPresentation, Interpretation, and Analysis of DataLara GatbontonNo ratings yet
- Adult Obesity CausesDocument9 pagesAdult Obesity CausesAntoNo ratings yet
- 8995 GU Infosys Mock-3Document23 pages8995 GU Infosys Mock-3Jason WestNo ratings yet