Professional Documents
Culture Documents
Clinical Medicine - Lecture: - Topic: - Date
Uploaded by
qselmm0 ratings0% found this document useful (0 votes)
50 views2 pagesComparison of Megaloblastic Anemias including Vitamin B12 and Folate Deficiency
Original Title
Megaloblastic Anemias Chart
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentComparison of Megaloblastic Anemias including Vitamin B12 and Folate Deficiency
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
50 views2 pagesClinical Medicine - Lecture: - Topic: - Date
Uploaded by
qselmmComparison of Megaloblastic Anemias including Vitamin B12 and Folate Deficiency
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 2
Clinical Medicine Lecture: _____ Topic: ____________________________________________________________ Date: ______________
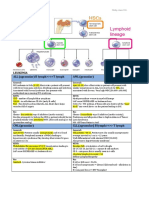
Cobalamin (Vitamin B12) Deficiency Folate Deficiency Anemia
Daily requirement is 1-3 mcg and body stores 2-3 mg. Daily requirement is ~100 mcg and total body folate level is ~10 mg
Active absorption of Intrinsic Factor (IF)-cobalamin complex at ileum. Only ~50% gets absorbed by upper small intestine and enters portal
Stomach becomes barren wasteland (makes no IF). circulation as 5-MTHF when 1/3 bound to albumin and 2/3 unbound
Cobalamin deficiency Folate deficiency
o Nutritional rare, but considered mostly in unfortified Vegans o Dietary particularly in old age, poverty, alcoholism, chronic
o Malabsorption pernicious anemia invalids, and the psychiatrically disturbed (esp. anorexia nervosa)
Pernicious anemia is anemia due to B12 deficiency, due to severe o Malabsorption
lack of IF, due to gastric atrophy Major causes of deficiency tropical sprue, gluten-induced
Common in north Europeans at peak age of 60 enteropathy in children and adults
Serum IF antibodies (autoimmune disease) in 50% of patients Minor causes of deficiency extensive jejunal resection, Crohns
Etiology
with pernicious anemia that prevent complex of IF & cobalamin disease
(Pathophysiology):
(Type I) or prevents attachment of complex to ileum (Type II) o Excessive utilization or loss
Gastric effects from other anti-gastric antibodies and CD4 cells Physiologic pregnancy and lactation, prematurity
atrophy of all layers of fundus and body with absence of parietal Pathologic chronic hemolytic anemias, sick cell anemia,
and chief cells, which leads to a lack of IF thalassemia major, myelofibrosis, exfoliative dermatitis, active
production/release/function/B12 absorption liver disease, hemodialysis, peritoneal dialysis
o Gastric causes total or partial gastrectomy o Antifolate drugs esp. phenytoin and sulfasalazine
H2RAs and PPIs prevent B12 and IF binding
o Intestinal causes ileal resection and Crohns disease
Metformin decreases absorption at ileum
Cobalamin metabolism abnormalities
Usually few/mild, if any, anemia symptoms Usually few/mild, if any, anemia symptoms
Vague GI disturbances like anorexia and diarrhea Vague GI disturbances like anorexia and diarrhea
Glossitis Glossitis
Complex neurological syndrome NO neurological syndrome
Clinical o Loss of myelin and neuronal cell death Skin changes
Manifestations Least likely to improve with repletion therapy o Darkening of the skin and mucous membranes, particularly at the
(Signs and o First have paresthesias of peripheral nerves and then progression to dorsal surfaces of the fingers, toes, and creases of palms and soles
Symptoms): posterior columns of spinal cord (balance difficulties, proprioception o Patchy distribution
impairment, pallesthesia) followed by cerebrum (dementia, o Should gradually resolve after weeks or months of folate treatment
neuropsychiatric abnormalities) if severe Modest temperature elevation (< 102 F)
o Temperature typically falls within 24-48 hours of vitamin treatment
Neural tube defects in pregnant patients
1. CBC 1. CBC
o Hgb low o Hgb low
o Hct low o Hct low
o MCH. MCHC increased o MCH. MCHC increased
Diagnostic Studies:
o MCV usually elevated at 110-140 fL (can be normal) o MCV usually elevated at 110-140 fL (can be normal)
o WBC Leukopenia* o WBC Leukopenia*
o Platelets Thrombocytopenia* o Platelets Thrombocytopenia*
2. Peripheral Smear and Reticulocytes 2. Peripheral Smear and Reticulocytes
o RBC Appearance macrocytic, hyperchromic o RBC Appearance macrocytic, hyperchromic
See macro-ovalocytes and hypersegmented neutrophils (6 lobes See macro-ovalocytes and hypersegmented neutrophils (6 lobes
or mean lobe counts >4), anisopoikilocytosis on peripheral smear or mean lobe counts >4), anisopoikilocytosis on peripheral smear
In severe anemia, see Howell-Jolly bodies in RBCs, Cabot rings In severe anemia, will have basophilic stippling of the RBCs, but
in RBCs, and basophilic stippling of the RBCs NO Cabot rings in RBCs
o (Reticulocytes Too few: poor RBC production overall o (Reticulocytes Too few: poor RBC production overall
3. B12 and Folate Studies Iron Studies 3. B12 and Folate Studies Iron Studies
o Vitamin B12 (automated ELISA or competitive-binding o Vitamin B12 Assays normal
luminescence) assay decreased, <200 pg/mL (NL > 300 pg/mL) o Folate level (Normal: 2.5-20 ng/mL)
If borderline B12 assay (200-300 pg/mL) confirm dx with serum Cannot be used alone to establish diagnosis; only useful for ruling
methylmalonic acid level or homocysteine level out folate deficiency if > 5 ng/mL
o Folate level normal If < 5 ng/mL, serum homocysteine (reference range 5-16
4. IF antibodies (Types 1 and 2) Shilling test mmol/L) elevated in folate deficiency
o Specific for pernicious anemia (confirms dx) o RBC folate assay test of body folate stores
5. Bone marrow aspiration and biopsy Decreased (Normal range: 160-640 mcg/L of PRBCs) in folate
o If done find hypercellular megaloblasts, trilineage differentiation, deficiency and ~2/3 of patients with severe cobalamin deficiency
and erythroid precursors that are large and often oval 4. Bone marrow aspiration and biopsy
6. Other o If done find hypercellular megaloblasts, trilineage differentiation,
o Indirect hyperbilirubinemia (due to intramedullary hemolysis) and erythroid precursors that are large and often oval
o Serum lactate dehydrogenase (LDH) concentration markedly
increased
Eliminate cause of deficiency and treat with cobalamin Folic acid 1 mg PO daily usually continued x 4 months at least
o Parenteral vitamin B12 IM 1 mg QD x 1 week, weekly x 4 weeks, Prevention through proper diet or supplement PO (400-600 mcg dietary
then STOP or, if underlying disorder persists monthly for life folate equivalents as recommended daily allowance; max 1 mg)
o Oral and nasal vitamin B12 1-2 mg daily Response to treatment
Only use AFTER the patients vitamin B12 status has been o In 5-7 days, improved sense of well-being and reticulocytosis
normalized with parenteral treatment o In 2 months, total correction of hematological abnormalities (anemia
o Within first 1-2 days especially)
Serum iron, indirect bilirubin, and LDH fall rapidly
If anemic before treatment, reticulocytosis in 3-4 days, (peaking
Treatment (First & at 1 week, followed by a rise in hemoglobin and a fall in MCV)
Second Line): MCHC begins to rise within 10 days (normalizes in 8 weeks)
Hypersegmented neutrophils disappear at 10-14 days
Neurologic abnormalities improve over 3 months, with max
improvement attained at 6-12 months (the degree of improvement
is inversely related to the extent and duration of disease)
Blood transfusion for severe anemia (<6.5 g/dL?) or critically ill
patient/comorbid conditions (<8 g/dL?)
Lifestyle modifications diet and activity
Delayed treatment permits progression of anemia and permanent
neurological complications
Hematology and Neurology PRN Dietician
Referral:
Hematology PRN
You might also like
- Family Medicine NotesDocument32 pagesFamily Medicine Noteslalee704100% (8)
- (CLINPATH) Lipids and DyslipoproteinemiaDocument5 pages(CLINPATH) Lipids and DyslipoproteinemiaJolaine ValloNo ratings yet
- Finals Trans (Hema)Document16 pagesFinals Trans (Hema)Ayesha CaragNo ratings yet
- Surgery PDFDocument4 pagesSurgery PDFJanine Maita BalicaoNo ratings yet
- TRANS - Pediatric Patient ProblemsDocument4 pagesTRANS - Pediatric Patient ProblemsRencel Hope Bañez100% (1)
- Chapter 7 Neoplasia 1 2 Robbins and Cotran Pathologic Basis of Disease PDFDocument9 pagesChapter 7 Neoplasia 1 2 Robbins and Cotran Pathologic Basis of Disease PDFChethranNo ratings yet
- OPTOMED-HW2-Diabetic Retinopathy PDFDocument3 pagesOPTOMED-HW2-Diabetic Retinopathy PDFDanalie SalvadorNo ratings yet
- Anemia and Hematologic Drugs - KatzungDocument4 pagesAnemia and Hematologic Drugs - Katzungsarguss14100% (1)
- LeukemiaDocument2 pagesLeukemiaAyeshaArifNo ratings yet
- Human Genetic Disorders PowerPointDocument48 pagesHuman Genetic Disorders PowerPointChewee Deane Salazar Mendez100% (5)
- Pharma Katzung - AlcoholsDocument5 pagesPharma Katzung - AlcoholsJoshua RemonNo ratings yet
- Anemia NotesDocument6 pagesAnemia NotesElstella Eguavoen Ehicheoya100% (2)
- Laboratory Investigations in Oral and Maxillofacial SurgeryDocument187 pagesLaboratory Investigations in Oral and Maxillofacial SurgeryTarun KashyapNo ratings yet
- Sickle Cell AnemiaDocument13 pagesSickle Cell Anemiamayra100% (1)
- Anemia Its Laboratory DiagnosisDocument146 pagesAnemia Its Laboratory DiagnosisCh M MushahidNo ratings yet
- Chapter 20Document10 pagesChapter 20AlyssaGrandeMontimorNo ratings yet
- Data Interpretation For Medical StudentDocument18 pagesData Interpretation For Medical StudentWee K WeiNo ratings yet
- Metabolic Disorders 01Document41 pagesMetabolic Disorders 01Brent LagartoNo ratings yet
- Iron Deficiency AnemiaDocument5 pagesIron Deficiency AnemiaLoiegy PaetNo ratings yet
- CMSE Question PapersDocument285 pagesCMSE Question PapersHari WaranNo ratings yet
- 4.02 - WBC, Lymph Nodes, Spleen & ThymusDocument5 pages4.02 - WBC, Lymph Nodes, Spleen & Thymusangel_sagun_1No ratings yet
- Hematology Trans 10Document6 pagesHematology Trans 10Claire GonoNo ratings yet
- Lecture 10 Vibrio, Aeromonas, Campylobacter and HelicobacterDocument4 pagesLecture 10 Vibrio, Aeromonas, Campylobacter and HelicobacterRazmine RicardoNo ratings yet
- Food and Waterborne Diseases Prevention and Control ProgramDocument3 pagesFood and Waterborne Diseases Prevention and Control ProgramJake PitosNo ratings yet
- WBC Lymph Node SpleenDocument12 pagesWBC Lymph Node Spleendr brijesh TiwariNo ratings yet
- Sickle Cell DiseaseDocument23 pagesSickle Cell Diseasealejandrino_leoaugusto100% (1)
- Examination of UrineDocument7 pagesExamination of UrineDaniel LamasonNo ratings yet
- Immunology ExamsDocument120 pagesImmunology ExamsThanuja SureshNo ratings yet
- HB EstimationDocument8 pagesHB Estimationmariet abraham100% (3)
- Hema AscpDocument5 pagesHema AscpDyne SabijonNo ratings yet
- NO Hazard Slight Moderate Serious Extreme: Hazard Hazard Hazard HazardDocument74 pagesNO Hazard Slight Moderate Serious Extreme: Hazard Hazard Hazard HazardCristy Jean100% (1)
- Dr. A. Samy TAG Bone Diseases - 1Document2 pagesDr. A. Samy TAG Bone Diseases - 1Herato MenaNo ratings yet
- Clinical Medicine - Lecture: - Topic: - DateDocument3 pagesClinical Medicine - Lecture: - Topic: - DateqselmmNo ratings yet
- Red Blood Cell Anomalies: Elliptocytes & Oval MacrocyteDocument12 pagesRed Blood Cell Anomalies: Elliptocytes & Oval MacrocyteSHUPATUSSAI100% (1)
- Classification of The Epilepsies: Purpose: For Clinical DiagnosisDocument25 pagesClassification of The Epilepsies: Purpose: For Clinical Diagnosisayu rifqiNo ratings yet
- Pediatrics SamplexDocument6 pagesPediatrics SamplexThea SansonNo ratings yet
- Vitamin B12 and FolateDocument12 pagesVitamin B12 and FolateAllessandria DimaggioNo ratings yet
- AnemiaDocument9 pagesAnemiaMila Canoza HerreraNo ratings yet
- Clinpath - : Red Blood CellsDocument14 pagesClinpath - : Red Blood CellsYolanda Primrosa NurhanNo ratings yet
- Chapter 23 SummaryDocument4 pagesChapter 23 SummaryMartin ClydeNo ratings yet
- 2021 Systemic Pathology S4T1 - RBC and Bleeding Disorders PDFDocument27 pages2021 Systemic Pathology S4T1 - RBC and Bleeding Disorders PDFAlexis Bondad100% (1)
- ENDOCRINE PATHOLOGY WebpathDocument35 pagesENDOCRINE PATHOLOGY Webpathapi-3766657No ratings yet
- Heamtology Reviewer (Midterm)Document15 pagesHeamtology Reviewer (Midterm)Johney DoeNo ratings yet
- Small Intestine 01 PDFDocument9 pagesSmall Intestine 01 PDFfadoNo ratings yet
- Screening Test For Phagocytic Engulfment: DiapedesisDocument2 pagesScreening Test For Phagocytic Engulfment: DiapedesisBianca ANo ratings yet
- Approach To Anemia: - Reticulocyte Count Is Most Important TestDocument15 pagesApproach To Anemia: - Reticulocyte Count Is Most Important TestJanella SuerteNo ratings yet
- Malassezia Furfur An-An Ap-Ap Naturally Found On The SkinDocument48 pagesMalassezia Furfur An-An Ap-Ap Naturally Found On The SkinNikki ValerioNo ratings yet
- Final DX ResultsDocument9 pagesFinal DX ResultszysheaiNo ratings yet
- UrinalysisDocument9 pagesUrinalysisSukma EffendyNo ratings yet
- (MED II) 1.05 Emergencies in Cancer PatientsDocument17 pages(MED II) 1.05 Emergencies in Cancer PatientsJearwin AngelesNo ratings yet
- Acute Lymphoblastic LeukemiaDocument25 pagesAcute Lymphoblastic Leukemiaapi-396564080No ratings yet
- Harrisons: Introduction To Infectious DiseasesDocument3 pagesHarrisons: Introduction To Infectious Diseasesapi-3704562No ratings yet
- Hemostasis and Thrombosis: OutlineDocument11 pagesHemostasis and Thrombosis: OutlineManila MedNo ratings yet
- CCII 8.0 - Clinical EnzymologyDocument2 pagesCCII 8.0 - Clinical EnzymologyWynlor AbarcaNo ratings yet
- Pancreatic Function TestDocument9 pagesPancreatic Function TestAyioKunNo ratings yet
- Blood and Tissue ProtozoaDocument32 pagesBlood and Tissue ProtozoaFort SalvadorNo ratings yet
- 4.1d - Pathology of The Pituitary - Nov.10 - Dr. GalangDocument4 pages4.1d - Pathology of The Pituitary - Nov.10 - Dr. GalangMiel Raphael AranillaNo ratings yet
- Female Genital TractDocument5 pagesFemale Genital Tractsarguss14100% (1)
- SubcutaneousDocument2 pagesSubcutaneousMary ChristelleNo ratings yet
- Anemia Type Pathogenesis Clinical Manifestations Diagnosis Peripheral Blood Lab FindingsDocument15 pagesAnemia Type Pathogenesis Clinical Manifestations Diagnosis Peripheral Blood Lab FindingsDanielle FosterNo ratings yet
- Hematology Lectures 1 5 DR - TuyDocument10 pagesHematology Lectures 1 5 DR - TuyMiguel Cuevas DolotNo ratings yet
- Red Blood Cell Disorders Anemia: Anemia Is A Laboratory DiagnosisDocument3 pagesRed Blood Cell Disorders Anemia: Anemia Is A Laboratory DiagnosisAnonymous 8hJAATBNo ratings yet
- Rabies: Ragina AguilaDocument55 pagesRabies: Ragina AguilaCharles Lester AdalimNo ratings yet
- Protein Metab 2 Dra. SantosDocument7 pagesProtein Metab 2 Dra. SantosMelissa SalayogNo ratings yet
- NSAIDs, DMARDs & Antigout1Document69 pagesNSAIDs, DMARDs & Antigout1Melissa SalayogNo ratings yet
- Erythrocytes Related Abnormalities and Diseases: Erythrocytic Morphology and Associated Disease (Size and Shape)Document5 pagesErythrocytes Related Abnormalities and Diseases: Erythrocytic Morphology and Associated Disease (Size and Shape)rona hilarioNo ratings yet
- HematologyDocument4 pagesHematologyliesel_12No ratings yet
- RBC DisordersDocument27 pagesRBC Disordersbpt2100% (1)
- 3rd Year TipsDocument5 pages3rd Year TipsDianne Joy PascuaNo ratings yet
- Pathology DR - Subh ACD & Megaloblastic Anemia Lec 26: PathogenesisDocument5 pagesPathology DR - Subh ACD & Megaloblastic Anemia Lec 26: PathogenesisS ANo ratings yet
- Equino PiroplasmoseDocument13 pagesEquino PiroplasmoseRogério Oliva CarvalhoNo ratings yet
- Anemia 1Document30 pagesAnemia 1Aishwarya JeeNo ratings yet
- Geron Sas 15Document8 pagesGeron Sas 15SSA CommissionNo ratings yet
- Case Scenario Drug Study - VicenteDocument4 pagesCase Scenario Drug Study - VicenteLouraine VicenteNo ratings yet
- Compendium of Transfusion MedicineDocument50 pagesCompendium of Transfusion MedicineLudmilla MartinsNo ratings yet
- HEMATOLOGY Chapter 20 Rodaks Hematology, 5E (2016)Document14 pagesHEMATOLOGY Chapter 20 Rodaks Hematology, 5E (2016)Sachi Xandria de LaraNo ratings yet
- Anemia in CKDDocument9 pagesAnemia in CKDM. Ryan RamadhanNo ratings yet
- Beplex Forte Tablet - Uses, Side Effects, Composition, Price & DosagesDocument12 pagesBeplex Forte Tablet - Uses, Side Effects, Composition, Price & Dosagesmaharshi DaddyNo ratings yet
- Interpretation of CBCDocument35 pagesInterpretation of CBCnth1992No ratings yet
- (M3) Approach To Full Blood Count (FBC)Document93 pages(M3) Approach To Full Blood Count (FBC)azs8t1No ratings yet
- Anaemia Policy BriefDocument7 pagesAnaemia Policy BriefAini DjunetNo ratings yet
- 1 Hema LecDocument5 pages1 Hema LecAngela ReyesNo ratings yet
- O Slide Method - Most Commonly Used o Cover Glass Method o Spin MethodDocument5 pagesO Slide Method - Most Commonly Used o Cover Glass Method o Spin MethodAngela ReyesNo ratings yet
- Management of Myelofibrosis: Alessandro M. VannucchiDocument9 pagesManagement of Myelofibrosis: Alessandro M. VannucchifrnksusNo ratings yet
- Case Scenarios University DR - NerveDocument24 pagesCase Scenarios University DR - NerveSREE NITHINNo ratings yet
- Hemat.Q - 1Document27 pagesHemat.Q - 1aliaaNo ratings yet
- Lab Value MnemonicsDocument10 pagesLab Value MnemonicsSophia CuertoNo ratings yet
- Evan's SyndromeDocument94 pagesEvan's SyndromeKristine Joy Vivero BillonesNo ratings yet
- Dental Considerations in Thalassemic PatientsDocument6 pagesDental Considerations in Thalassemic PatientsInternational Organization of Scientific Research (IOSR)No ratings yet