Professional Documents
Culture Documents
Research Article Use of Ginger Versus Stretching Exercises For The Treatment of Primary Dysmenorrhea: A Randomized Controlled Trial
Uploaded by
daypranitaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Research Article Use of Ginger Versus Stretching Exercises For The Treatment of Primary Dysmenorrhea: A Randomized Controlled Trial
Uploaded by
daypranitaCopyright:
Available Formats
Journal homepage:
www.jcimjournal.com/jim
www.elsevier.com/locate/issn/20954964
Available also online at www.sciencedirect.com.
Copyright 2017, Journal of Integrative Medicine Editorial Office.
E-edition published by Elsevier (Singapore) Pte Ltd. All rights reserved.
Research Article
Use of ginger versus stretching exercises for
the treatment of primary dysmenorrhea: a
randomized controlled trial
Marjan Ahmad Shirvani1, Narges Motahari-Tabari1, Abbas Alipour2
1. Department of Midwifery, School of Nursing & Midwifery, Mazandaran University of Medical Sciences, Sari
4816715793, Iran
2. Department of Community Medicine, School of Medicine, Mazandaran University of Medical Sciences, Sari
4847191971, Iran
ABSTRACT
BACKGROUND: Dysmenorrhea is a common gynecologic problem. In some cases, non-medical treatments
are considered to be more effective, with fewer side effects. Ginger and exercise are alternative treatments
for dysmenorrhea, but in the present study they were not combined.
OBJECTIVE: In this study, the effects of ginger and exercise on primary dysmenorrhea were compared.
DESIGN, SETTING, PARTICIPANTS AND INTERVENTIONS: This randomized controlled trial was
performed in Mazandaran University of Medical Sciences, Iran. Two groups of female students were recruited
by simple random allocation. In each group, 61 students with moderate to severe primary dysmenorrhea with
regular menstrual cycles and without a history of regular exercise were assessed. The ginger group received
250 mg ginger capsules from the onset of menstruation. In the exercise group, belly and pelvic stretching
exercises were performed for 10 min, 3 times per week.
MAIN OUTCOME MEASURES: Intensity of pain was assessed according to a visual analogue scale after
the first and the second month.
RESULTS: Exercise was significantly more effective than ginger for pain relief (31.57 16.03 vs 38.19
20.47, P = 0.02), severity of dysmenorrhea (63.9% vs 44.3% mild dysmenorrhea, P = 0.02) and decrease in
menstrual duration (6.08 1.22 vs 6.67 1.24, P = 0.006), in the second cycle.
CONCLUSION: Stretching exercises, as a safe and low-cost treatment, are more effective than ginger for
pain relief in primary dysmenorrhea.
TRIAL REGISTRATION: The trial was registered in www.IRCT.ir with No. 201203118822N2.
Keywords: ginger; pain; primary dysmenorrhea; stretching exercise
Citation: Shirvani MA, Motahari-Tabari N, Alipour A. Use of ginger versus stretching exercises for the treatment
of primary dysmenorrhea: a randomized controlled trial. J Integr Med. 2017; 15(4): 295301.
http://dx.doi.org/10.1016/S2095-4964(17)60348-0
Received January 12, 2017; accepted March 31, 2017.
Correspondence: Narges Motahari-Tabari; E-mail: narges_mth@yahoo.com
Journal of Integrative Medicine 295 July 2017, Vol. 15, No. 4
www.jcimjournal.com/jim
1 Introduction to May 2014. It involved female students of Mazandaran
University of Medical Sciences, Iran. The ethics
Dysmenorrhea refers to the occurrence of painful committee of this university approved the study protocol in
uterine cramps during menstruation.[13] It is characterized conformation with the Declaration of Helsinki.
by acute and cyclic pain in the midline of the lower Following a review of previous studies and the size
abdomen but it may be described as dull in the lumbar effects of physical activity (2.2 2.4) and ginger (2.3 2.8)
area and the thighs.[4,5] Pain usually begins from a few to with = 0.05, and b = 80%, the sample size was calculated
several hours before the onset of menstrual bleeding, and to be 61 for each group.[3,15,16]
continues until the first or the second day of the menstrual The participants were allocated to the groups by simple
cycle.[35] Diarrhea, nausea and vomiting are associated randomization. For this reason, we provided a list of
symptoms.[4,6] This pain can affect womens quality of life, eligible students (n = 122) with one number given to each
and may lead to absence from work or school, and time of them. Then they were sequentially allocated to two
spent on self-care and professional-care.[7] Between one- groups using the random number table. One group received
third and one-half of women presenting for primary care training for exercise, and the other group received ginger.
report moderate or severe dysmenorrhea.[1] Among Iranian The purpose and method of the study and the participants
women, the prevalence of moderate to severe dysmenorrhea rights (e.g., voluntary participation and ability to leave the
is 50%.[8] Physiologically, the pain is caused by excessive study) were explained in a handout. Then written informed
amounts of prostaglandins, which introduce abnormal consent was obtained from all participants.
uterine contractions and reduce uterine blood flow.[7] Inclusion criteria: students who lived in the dormitory
Medication by nonsteroidal anti-inflammatory drugs and were interested in participating in the study; history of
(NSAIDs), inhibitors of cyclooxygenase enzymes and primary dysmenorrhea which had affected daily activities
prostaglandins, is one of the conventional treatments for in at least 50% of their cycles through the past 6 months;
primary dysmenorrhea.[3] Current medical therapies offer and pain intensity over 40 mm, based on the 100-mm
inadequate treatment, with a failure rate of 20%25%.[4] Some visual analogue scale (VAS). Exclusion criteria: irregular
women prefer not to use NSAIDs because they perceive menstrual cycles; the use of intra-uterine devices and oral
no benefit and have adverse side effects or for cultural contraceptive pills; history of regular exercise (3 times
reasons.[4,9,10] Thus, alternative treatments with low toxicity, weekly for 3045 min); diseases of the genitourinary
such as traditional medicine, are recommended.[9] Several system (e.g., pelvic inflammatory disease and urinary tract
studies have reported that ginger, an inhibitor of prostaglandin infections) and secondary dysmenorrhea.[6]
synthesis, with a long history of use in traditional medicine, 2.2 Measures
has beneficial effects on primary dysmenorrhea.[1113] On The participants completed a demographic form. The
the other hand, physical activity stimulates the release of primary treatment outcome was pain intensity, measured
-endorphin, which functions as an analgesic, and reduces with VAS. Pain intensity was classified as follows: 40
the frequency and severity of primary dysmenorrhea.[6] 60 mm (moderate), more than 60 mm (severe) and under
Because alternative treatments may reduce some symptoms 40 mm (mild). In addition, duration of pain and some other
of dysmenorrhea during the menstrual period, without the side menstruation characteristics (e.g., length of menstruation
effects of conventional treatments, they have been considered and menstrual cycle and change in bleeding) were assessed
for the management of dysmenorrhea.[10,14,15] as secondary outcomes. In both groups, participants were
Few studies have compared herbal drugs with physical asked to record pain intensity and other variables at the end
activity for the treatment of dysmenorrhea. This comparison of the first and the second menstruation cycles.
helps both practitioners and patients make decision about the 2.3 Interventions
treatment, when several choices are available. In one group, exercise programs were taught by two
Although, some herbal drugs and non-pharmacological trained instructors. First, they were trained by a qualified
treatments have been suggested for primary dysmenorrhea, sport sciences instructor. Then they performed the exercise
there is a lack of information about comparison of these programs with students in the fitness hall of the dorm for
approaches. The aim of this study was to compare the several sessions, until they were sure that all participants
effectiveness of exercise and ginger on primary dysmenorrhea. could do the exercises correctly. Furthermore, pamphlets
including images and instructions for the exercises were
2 Materials and methods given to each of the participants in the exercise group. The
exercise programs included 5 min of warm-up movements
2.1 Study design and subjects in a standing position, followed by 6 stretching exercises
This article reports some of the results of a randomized for the abdomen and pelvis for 10 min. This program
clinical trial, with parallel design, conducted from January was performed for 15 min, 3 times per week, for two
July 2017, Vol. 15, No. 4 296 Journal of Integrative Medicine
www.jcimjournal.com/jim
consecutive menstrual cycles (8 weeks). Exercises were Smirnov test. In addition to descriptive statistics (means,
not performed during menstruation.[16,17] The instructors standard deviations and frequency) and Chi-square, the
contacted the participants weekly to ensure that they Friedman test was used for dependent variables (longitudinal
were following the exercise program, and to answer any assessment in the three time periods for the same group) and
questions. In the second group, students took 250 mg ginger the Mann-Whitney U test was used for independent variables
capsules (Zintoma 250 mg, Goldaru Co, Iran). Capsules (ginger and exercise groups in each period). The SPSS
were taken at the onset of menstruation and then every 6 h version 20.0 was used for statistical analysis. The significant
until pain relief for 2 consecutive cycles.[15] The duration level was considered less than 0.05.
of interventions was determined according to the results of
other studies.[15,16] 3 Results
The students in both groups did not exercise regularly
before the interventions, and they were asked to limit any 3.1 Demographic characteristics
exercise during the study period except the prescribed Data were completed for 122 students, with 61 participants
stretching movements in the exercise group. in each group (Figure 1). Demographic characteristics were
2.4 Statistical analysis not significantly different between the groups (P > 0.05,
Data normality was assessed with the Kolmogorov- Table 1).
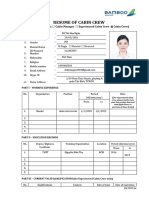
Assessed for eligibility (N = 227)
Enrollment
Excluded (n = 105)
Not meeting inclusion criteria (n = 37)
Use of another drug (n = 61)
Declined to participate (n = 7)
Randomized (n = 122)
Allocation
Allocated to ginger group (n = 61) Allocated to exercise group (n = 61)
Received allocated intervention Received allocated intervention
Analysis
Analysed (n = 61) Analysed (n = 61)
Figure 1 Flowchart of participants enrollment in the study
Table 1 Demographic characteristics of students with dysmenorrhea in the study groups
Ginger group Exercise group
Variable P value
(n = 61) (n = 61)
Age (mean standard deviation, years) 21.60 2.14 21.32 1.96 0.45
BMI (mean standard deviation, kg/m2) 21.65 3.08 22.56 3.56 0.13
Year level in the university (n (%))
1st & 2nd 33 (54.1) 24 (39.3)
0.07
3rd 28 (45.9) 37 (60.7)
Family history of dysmenorrhea (n (%))
Yes 39 (63.9) 34 (55.7)
No 14 (23.0) 20 (32.8) 0.48
Unknown 8 (13.1) 7 (11.5)
BMI: body mass index.
Journal of Integrative Medicine 297 July 2017, Vol. 15, No. 4
www.jcimjournal.com/jim
3.2 Pain and menstruation characteristics case of severe dysmenorrhea was seen at the end of the
As shown in Table 2, decrease in pain intensity was second month. The occurrence of mild dysmenorrhea
significant within both groups (P < 0.001). However, the was significantly higher in the exercise group in the
reduction of pain was more significant in the exercise second month (Table 3). The change in bleeding was not
group than in the ginger group in the second month of significantly different between groups during the study
intervention (P = 0.02). Pain duration was not significantly (Table 3).
different between the groups during the study, though it
decreased significantly in the exercise group (P = 0.02). 4 Discussion
The length of the menstrual cycle was not significantly
different between the groups, but it increased in the Currently, various medical and non-medical treatments
ginger group during the study (P = 0.02). There was a are suggested for the treatment of primary dysmenorrhea.
significant reduction in the duration of menstruation in Although the use of NSAIDs is common,[3] because of
the exercise group during the study (P < 0.001). This some reports of poor efficacy and side effects, alternative
reduction was more than the ginger group in the second approaches, such as herbal drugs and physical activities,
month (P = 0.006). are recommended.[1,3,6,1820]
3.3 Menstruation outcomes The results of this study showed that the stretching
Although there were no cases of mild dysmenorrhea exercises had a greater effect than ginger in treatment
at the beginning of the study, some cases appeared after of primary dysmenorrhea after two months. Although
the first month, as participant symptoms improved. No no case of severe dysmenorrhea was seen in either
Table 2 Comparison of pain and menstruation characteristics within and between the ginger and exercise groups
Ginger group (n = 61) Exercise group (n = 61)
Variable
Mean SD P value Mean SD P value
Pain intensity (VAS score)
Baseline 58.01 15.16 60.26 14.45
1st month 43.49 19.99 < 0.001 45.42 19.21 < 0.001
2nd month 38.19 20.47 31.57 16.03
Comparing changes between baseline and 1st month (intergroup) P = 0.95
Comparing changes between baseline and 2nd month (intergroup) P = 0.02
Pain duration (d)
Baseline 1.62 0.85 1.78 0.70
1st month 1.60 0.80 0.69 1.59 0.78 0.02
2nd month 1.49 0.78 1.50 0.72
Comparing changes between baseline and 1st month (intergroup) P = 0.12
Comparing changes between baseline and 2nd month (intergroup) P = 0.16
Menstrual cycle duration (d)
Baseline 27.44 3.15 29.16 3.47
1st month 28.85 2.92 0.02 29.01 4.29 0.47
2nd month 28.95 2.67 29.16 2.88
Comparing changes between baseline and 1st month (intergroup) P = 0.23
Comparing changes between baseline and 2nd month (intergroup) P = 0.07
Duration of menstruation (d)
Baseline 6.70 1.22 6.77 1.30
1st month 6.50 1.19 0.35 6.50 1.14 < 0.001
2nd month 6.67 1.24 6.08 1.22
Comparing changes between baseline and 1st month (intergroup) P = 0.78
Comparing changes between baseline and 2nd month (intergroup) P = 0.006
VAS: visual analogue scale. SD: standard diviation
July 2017, Vol. 15, No. 4 298 Journal of Integrative Medicine
www.jcimjournal.com/jim
Table 3 Comparison of menstruation outcomes between the ginger and the exercise groups
Menstruation outcomes (n (%)) Ginger group (n = 61) Exercise group (n = 61) P value
Severity of dysmenorrhea
Baseline
Moderate 40 (65.6) 39 (63.9) 0.50
Severe 21 (34.4) 22 (36.1)
1st month
Mild 19 ( 31.1) 20 (32.8) 0.95
Moderate 33 (54.1) 33 (54.1)
Severe 9 (14.8) 8 (13.1)
2nd month
Mild 27 (44.3) 39 (63.9) 0.02
Moderate 34 (55.7) 22 (36.1)
Bleeding
1st month
Increase 8 (13.1) 6 (9.8) 0.39
Decrease 10 (16.4) 16 (26.2)
No change 43 (70.5) 39 (63.9)
2nd month
Increase 9 (14.8) 9 (14.8) 0.10
Decrease 11 (18.0) 21 (34.4)
No change 41 (67.2) 31 (50.8)
group by the second month, mild dysmenorrhea was exercise protocols on pain relief in dysmenorrhea.[17,26,27]
significantly more prevalent in the exercise group. Pain Additionally, it has been reported that regular exercise
reduction in the ginger group was also considerable. is more effective than occasional exercise.[28] Further,
Traditionally, ginger has been used for the treatment of greater than one hour of daily physical activity was
pain[13] and has been introduced as an effective treatment associated with lower prevalence of dysmenorrhea.[29] In
for dysmenorrhea. [21,22] Recently, authors reported the the current study, pain duration decreased in the exercise
effects of various dosages of ginger on pain relief in group during the study, but the difference was not
dysmenorrhea. [11,12,15,23,24] Also, the effects of various significant between the groups. There are some reports
types of exercise, such as stretching movements, on of reduced pain duration with exercise, which may cause
dysmenorrhea have been confirmed.[7,16,17,25] In a study a more rapid transfer of prostaglandins.[16,17,30,31] Rahnama
comparing active exercise with a combination of active and co-workers[12] reported a decrease in pain duration
exercise and dietary ginger, Gupta et al.[9] reported that when ginger was prescribed from 2 d before menstruation.
the efficacy of combined ginger and exercise was higher Thus, a lack of significant reduction in pain duration in
than that of exercise alone for the relief of pain from the ginger group compared with the exercise group in our
primary dysmenorrhea. In the current study, we did not study may be due to the later prescription of ginger.
compare the combination of ginger and exercise, but the Some of the mechanisms of pain relief in dysmenorrhea
effect of exercise was higher than that of ginger alone. are common between ginger and exercise. Exercise
Thus, for increasing the effect of ginger, taking it in improves pelvic blood circulation, which prevents
combining with an exercise program may be effective. prostaglandins aggregation. [7,28] Also, ginger has the
Similar to the study by Gupta et al., [9] in the present same effect via decreasing endothelin-1 and increasing
study, though pain intensity decreased in both groups nitrous oxide, which lead to expansion of vessels
in the first month, the difference was not significant. and, as a result, improvement of blood circulation.[32]
Those authors concluded that the effect of exercise on Prostaglandins stimulate myometrium contractions
dysmenorrhea increased over time. Shahr-jerdy et al.[16] and are important factors in the induction of primary
reported the effectiveness of 8 weeks of stretching dysmenorrhea.[7] In addition, ginger activates endorphin
exercises on pain reduction in primary dysmenorrhea. receptors by the inhibition of thromboxane synthesis
Other researchers showed the effects of prolonged and suppresses hyperactivity of neuroadrenergics; [33]
Journal of Integrative Medicine 299 July 2017, Vol. 15, No. 4
www.jcimjournal.com/jim
exercise leads to hormonal changes in the uterus and Research Deputy of Mazandaran University of Medical
activates endorphins, [7,16,17] which can relieve pain. Sciences (grant number: H-92-24), Iran.
However, exercise may affect dysmenorrhea by some
additional mechanisms. Psychological conditions 7 Acknowledgements
influence dysmenorrhea and its severity.[3436] There is a
correlation between dysmenorrhea and stress levels. [16] We thank the vice-Chancellor for Research of Mazandaran
Stress increases uterine contractions, with an effect on University of Medical Sciences for supporting this project
the nervous system.[36,37] Exercise has a positive effect (grant number: H-92-24). We also appreciate all the
on dysmenorrhea by decreasing stress and improving students who participated in this study.
mood.[7,38,39] Also, exercise decreases spasms and pressure
on the nerves.[1,18,25] 8 Conflicts of interest
Although the duration of the menstrual cycle was
shorter in the ginger group, the difference in cycle length There is no conflict of interest.
between groups was not significant during the study. The
duration of menstruation was reduced in the exercise REFERENCES
group during the study and was significantly lower than
that of the ginger group in the second month. In addition, 1 Dawood MY. Primary dysmenorrhea: advances in pathogenesis
during the study, more women in the exercise group and management. Obstet Gynecol. 2006; 108(2): 428441.
reported decreased bleeding compared to the ginger 2 Lefebvre G, Pinsonneault O, Antao V, Black A, Burnett
group, but the difference was not significant. Similarly, M, Feldman K, Lea R, Robert M; SOGC. Primary
dysmenorrhea consensus guideline. J Obstet Gynaecol Can.
Shavandi et al.[31] reported no change in bleeding with
2005; 27(12): 11171146. English and French.
8 weeks of exercise. In contrast, reduction in bleeding
3 Marjoribanks J, Proctor M, Farquhar C, Derks RS.
was reported by Abbaspour et al.[17] in the 4th cycle after Nonsteroidal anti-inflammatory drugs for dysmenorrhoea.
initiation of exercise, and by Mahvash et al.[30] 8 weeks Cochrane Database Syst Rev. 2010; (1): CD001751.
after beginning a program of stretching plus resistance 4 Abdul-Razzak KK, Ayoub NM, Abu-Taleb AA, Obeidat
exercise for 90 min 3 times per week. Thus, it seems BA. Influence of dietary intake of dairy products on
that the effect of exercise on bleeding may be increased dysmenorrhea. J Obstet Gynaecol Res. 2010; 36(2): 377
with prolonged duration and higher-intensity exercise 383.
programs, probably because of hormonal changes.[30] 5 Banikarim C, Middleman AB, Geffner M, Hoppin AG.
In this study, we compared two alternative treatments, Primary dysmenorrhea in adolescents. (2015-11-10) [2017-
01-16]. https://www.uptodate.com/contents/primary-
ginger and exercise, for primary dysmenorrhea. To the
dysmenorrhea-in-adolescents.
best of our knowledge, this has not been considered 6 Brown J, Brown S. Exercise for dysmenorrhoea. Cochrane
previously. Because primary dysmenorrhea usually affects Database Syst Rev. 2010; (2): CD004142.
young women and this study included a young population 7 Collins Sharp BA, Taylor DL, Thomas KK, Killeen MB,
of female students, these findings are especially Dawood MY. Cyclic perimenstrual pain and discomfort: the
relevant for young women with primary dysmenorrhea. scientific basis for practice. J Obstet Gynecol Neonat Nurs.
Limitations of the study included: no comparison with 2002; 31(6): 637649.
control or placebo groups; no investigation of the role of 8 Tavallaee M, Joffres MR, Corber SJ, Bayanzadeh M, Rad
timing of ginger dose with the onset of menstruation or MM. The prevalence of menstrual pain and associated risk
the dose effect of ginger supplements; and no exploration factors among Iranian women. J Obstet Gynaecol Res.
2011; 37(5): 442451.
of the role of intensity, duration and type of exercise on
9 Gupta R, Kaur S, Singh A. Comparison to assess the effectiveness
improvement of symptoms. of active exercises and dietary ginger vs. active exercises
on primary dysmenorrhea among adolescent girls. Nurs
5 Conclusions Midwifery Res J. 2013; 9(4): 153.
10 Proctor ML, Murphy PA. Herbal and dietary therapies for
It appears that stretching exercises, as a safe and low- primary and secondary dysmenorrhoea. Cochrane Database
cost approach, are more effective than ginger for the Syst Rev. 2001; (3): CD002124.
reduction of pain and menstrual duration in primary 11 Jenabi E. The effect of ginger for relieving of primary
dysmenorrhea. dysmenorrhoea. J Pak Med Assoc. 2013; 63(1): 810.
12 Rahnama P, Montazeri A, Huseini HF, Kianbakht S, Naseri
M. Effect of Zingiber officinale R. rhizomes (ginger) on
6 Funding pain relief in primary dysmenorrhea: a placebo randomized
trial. BMC Complement Altern Med. 2012; 12(1): 92.
This study has been supported by a grant from the 13 Terry R, Posadzki P, Watson LK, Ernst E. The use of ginger
July 2017, Vol. 15, No. 4 300 Journal of Integrative Medicine
www.jcimjournal.com/jim
(Zingiber officinale) for the treatment of pain: a systematic J Physiol Pharmacol. 2013; 57(2): 114122.
review of clinical trials. Pain Med. 2011; 12(12): 1808 27 Rezvani S, Taghian F, Valiani M. The effect of aquatic
1818. exercises on primary dysmenorrhoea in nonathlete girls.
14 Blumenthal M, Busse W, Goldberg A. The complete Iran J Nurs Midwifery Res. 2013; 18(5): 378383.
German Commission E monographs: therapeutic guide 28 Izzo A, Labriola D. Dysmenorrhoea and sports activities in
to herbal medicines. Austin: American Botanical Council. adolescents. Clin Exp Obstet Gynecol. 1991; 18(2): 109
1998: 683. 116.
15 Ozgoli G, Goli M, Moattar F. Comparison of effects of 29 Maruf FA, Ezenwafor NV, Moroof SO, Adeniyi AF, Okoye
ginger, mefenamic acid, and ibuprofen on pain in women EC. Physical activity level and adiposity: are they associated
with primary dysmenorrhea. J Alternat Complement Med. with primary dysmenorrhea in school adolescents? Afr J
2009; 15(2): 129132. Reprod Health. 2013; 17(4): 167174.
16 Shahr-jerdy S, Hosseini RS, Gh ME. Effects of stretching 30 Mahvash N, Eidy A, Mehdi K, Zahra MT, Mani M, Shahla
exercises on primary dysmenorrhea in adolescent girls. H. The effect of physical activity on primary dysmenorrhea
Biomed Human Kinetics. 2012; 4: 127132. of female university students. World Appl Sci J. 2012;
17 Abbaspour Z, Rostami M, Najjar S. The effect of exercise 17(10): 12461252.
on primary dysmenorrhea. J Res Health Sci. 2006; 6(1): 31 Shavandi M, Taghian F, Soltani V. The effect of isometric
2631. exercise on primary dysmenorrhea. Arak Med Univ J. 2010;
18 Blakey H, Chisholm C, Dear F, Harris B, Hartwell R, 13(1): 7177. Persian.
Daley AJ, Jolly K. Is exercise associated with primary 32 Yang JJ, Sun LH, She YF, Ge JJ, Li XH, Zhang RJ.
dysmenorrhoea in young women? BJOG. 2010; 117(2): Influence of ginger-partitioned moxibustion on serum NO
222224. and plasma endothelin-1 contents in patients with primary
19 Higuchi K, Umegaki E, Watanabe T, Yoda Y, Morita dysmenorrhea of cold-damp stagnation type. Zhen Ci
E, Murano M, Tokioka S, Arakawa T. Present status Yan Jiu. 2008; 33(6): 409412. Chinese with abstract in
and strategy of NSAIDs-induced small bowel injury. J English.
Gastroenterol. 2009; 44(9): 879888. 33 Backon J. Mechanism of analgesic effect of clonidine in the
20 Shi S, Klotz U. Clinical use and pharmacological properties treatment of dysmenorrhea. Med Hypotheses. 1991; 36(3):
of selective COX-2 inhibitors. Eur J Clin Pharmacol. 2008; 223224.
64(3): 233252. 34 Alonso C, Coe CL. Disruptions of social relationships
21 Altman R, Marcussen K. Effects of a ginger extract on knee accentuate the association between emotional distress and
pain in patients with osteoarthritis. Arthritis Rheum. 2001; menstrual pain in young women. Health Psychol. 2001;
44(11): 25312238. 20(6): 411416.
22 Mills S, Bone K. Principles and practice of phytotherapy: 35 G o l o m b L M , S o l i d u m A A , Wa r r e n M P. P r i m a r y
modern herbal medicine. London: Churchill Livingstone. dysmenorrhea and physical activity. Med Sci Sports Exerc.
2000. 1998; 30(6): 906909.
23 Halder A. Effect of progressive muscle relaxation versus 36 Wang L, Wang X, Wang W, Chen C, Ronnennberg A,
intake of ginger powder on dysmenorrhoea amongst the Guang W, Huang A, Fang Z, Zang T, Wang L, Xu X. Stress
nursing students in Pune. Nur J India. 2011; 103(4): 152 and dysmenorrhoea: a population based prospective study.
156. Occup Environ Med. 2004; 61(12): 10211026.
24 Kashefi F, Khajehei M, Tabatabaeichehr M, Alavinia M, 37 Gannon L. The potential role of exercise in the alleviation
Asili J. Comparison of the effect of ginger and zinc sulfate of menstrual disorders and menopausal symptoms: a
on primary dysmenorrhea: a placebo-controlled randomized theoretical synthesis of recent research. Women Health.
trial. Pain Manag Nurs. 2014; 15(4): 826833. 1988; 14(2): 105127.
25 Daley A. The role of exercise in the treatment of menstrual 38 Locke RJ, Warren MP. Curbside Consult: what is the effect
disorders: the evidence. Br J Gen Pract. 2009; 59(561): of exercise on primary dysmenorrhea? West J Med. 1999;
241242. 171(4): 264265.
26 Chaudhuri A, Singh A, Dhaliwal L. A randomised controlled 39 Metheny WP, Smith RP. The relationship among exercise,
trial of exercise and hot water bottle in the management of stress, and primary dysmenorrhea. J Behav Med. 1989;
dysmenorrhoea in school girls of Chandigarh, India. Indian 12(6): 569586.
Journal of Integrative Medicine 301 July 2017, Vol. 15, No. 4
You might also like
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Omj D 15 00199Document7 pagesOmj D 15 00199Dewi Kartika SariNo ratings yet
- 0194599816657045Document7 pages0194599816657045daypranitaNo ratings yet
- Guidelines TBC TerbaruDocument160 pagesGuidelines TBC TerbaruSutoto MoeljadiNo ratings yet
- 38 31394nsj141216 245 249Document5 pages38 31394nsj141216 245 249daypranitaNo ratings yet
- Parrish Scoring Snake BiteDocument1 pageParrish Scoring Snake BitedaypranitaNo ratings yet
- Hsu2018 PDFDocument11 pagesHsu2018 PDFdaypranitaNo ratings yet
- International Pediatric Sepsis Consensus Conference-PediatrCritCar2005-eDocument7 pagesInternational Pediatric Sepsis Consensus Conference-PediatrCritCar2005-eAna Belén VizcarraNo ratings yet
- Kashani 2016Document5 pagesKashani 2016daypranitaNo ratings yet
- Pa Potti 2014Document14 pagesPa Potti 2014daypranitaNo ratings yet
- Lughezzani 2010Document7 pagesLughezzani 2010daypranitaNo ratings yet
- Nej Mo A 1113216Document11 pagesNej Mo A 1113216daypranitaNo ratings yet
- Berman 2013Document7 pagesBerman 2013daypranitaNo ratings yet
- Genetics of Primary Macronodular Adrenal Hyperplasia: ReviewDocument13 pagesGenetics of Primary Macronodular Adrenal Hyperplasia: ReviewdaypranitaNo ratings yet
- R51 Full PDFDocument14 pagesR51 Full PDFdaypranitaNo ratings yet
- Holyoak2016 PDFDocument14 pagesHolyoak2016 PDFdaypranitaNo ratings yet
- MDV 329Document7 pagesMDV 329daypranitaNo ratings yet
- R51 Full PDFDocument14 pagesR51 Full PDFdaypranitaNo ratings yet
- Luo 2013Document4 pagesLuo 2013daypranitaNo ratings yet
- Carbohydrate Polymers: Lili Zhao, Mengrui Liu, Juan Wang, Guangxi ZhaiDocument9 pagesCarbohydrate Polymers: Lili Zhao, Mengrui Liu, Juan Wang, Guangxi ZhaidaypranitaNo ratings yet
- Inatani 2000Document4 pagesInatani 2000daypranitaNo ratings yet
- 11Document11 pages11daypranitaNo ratings yet
- International Pediatric Sepsis Consensus Conference-PediatrCritCar2005-eDocument7 pagesInternational Pediatric Sepsis Consensus Conference-PediatrCritCar2005-eAna Belén VizcarraNo ratings yet
- Hyaluronate-Covered Nanoparticles For The Therapeutic Targeting of CartilageDocument7 pagesHyaluronate-Covered Nanoparticles For The Therapeutic Targeting of CartilagedaypranitaNo ratings yet
- Dwivedi 2015Document7 pagesDwivedi 2015daypranitaNo ratings yet
- Nanoparticles For Improved Local Retention After Intra-Articular Injection Into The Knee Joint PDFDocument12 pagesNanoparticles For Improved Local Retention After Intra-Articular Injection Into The Knee Joint PDFdaypranitaNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- WEB VTH 01292009Document28 pagesWEB VTH 01292009Dave L100% (1)
- NCP Ineffective Airway Clearance Related To Lung Impairment PNEUMOTHORAXDocument5 pagesNCP Ineffective Airway Clearance Related To Lung Impairment PNEUMOTHORAXMa. Elaine Carla Tating0% (2)
- Antifungal Susceptibility Pattern Against Dermatophytic Strains Isolated From Humans in Anambra State, NigeriaDocument8 pagesAntifungal Susceptibility Pattern Against Dermatophytic Strains Isolated From Humans in Anambra State, NigeriaIJAERS JOURNALNo ratings yet
- Four Legs of Dharma / Religion (Duties For Mankind) : Austerity Cleanliness Mercy TruthfulnessDocument1 pageFour Legs of Dharma / Religion (Duties For Mankind) : Austerity Cleanliness Mercy TruthfulnessShyam SundarNo ratings yet
- Hospital PharmacyDocument13 pagesHospital PharmacySridivya SrihariNo ratings yet
- Medicinal Plant (Rahul Sharma) ChambaDocument17 pagesMedicinal Plant (Rahul Sharma) ChambaRahul SharmaNo ratings yet
- 4 2Document39 pages4 2Anonymous GWPdocUtNo ratings yet
- AscarisDocument16 pagesAscarisRommy Kurniawan DeskyNo ratings yet
- Obstetric NursingDocument36 pagesObstetric NursingpauchanmnlNo ratings yet
- Ground Floor PlanDocument1 pageGround Floor PlanjrsourisNo ratings yet
- Shaws Text Book of GynecologyDocument438 pagesShaws Text Book of GynecologySumeera Nirmal Samarakkody100% (2)
- MBLEx Practice ExamsDocument268 pagesMBLEx Practice ExamsTrace Thuma100% (9)
- The Women-S Fitness Book PDFDocument338 pagesThe Women-S Fitness Book PDFKaren Jennifer Beltrán Taipe95% (21)
- Family Case Study On The Billones Family 1Document63 pagesFamily Case Study On The Billones Family 1Ivy Mae DecenaNo ratings yet
- Oral 5Document236 pagesOral 5Iodeh1985 OdehNo ratings yet
- L10 ToleranceDocument19 pagesL10 Tolerancesara garciaNo ratings yet
- The Tactical Combat Casualty Care Casualty Card - TCCC Guidelines - Proposed Change 1301Document9 pagesThe Tactical Combat Casualty Care Casualty Card - TCCC Guidelines - Proposed Change 1301Paschalis DevranisNo ratings yet
- 2006 TOUCH FOR HEALTH Annual Meeting ReporDocument80 pages2006 TOUCH FOR HEALTH Annual Meeting Reporlectavares100% (2)
- Strengths Based NursingDocument22 pagesStrengths Based NursingTHOHAROH0% (1)
- Emergency Psychiatry Other Than Suicide: Dr. Pooja Singh, MD Assistant ProfessorDocument45 pagesEmergency Psychiatry Other Than Suicide: Dr. Pooja Singh, MD Assistant Professorpooja singhNo ratings yet
- Sports NutritionDocument78 pagesSports NutritionnpurdonNo ratings yet
- Phenylephrine HydrochlorideDocument5 pagesPhenylephrine HydrochlorideRoger Jr PumarenNo ratings yet
- NABH ChecklistDocument3 pagesNABH ChecklistMargretSnehaNo ratings yet
- BCS RadiologiDocument46 pagesBCS RadiologiHananya Manroe100% (1)
- Curriculum Vitae of Dr. Ankur BaruaDocument38 pagesCurriculum Vitae of Dr. Ankur BaruaANKUR BARUA100% (1)
- Rab297cen - Yumizen H500 OT Daily Guide PDFDocument42 pagesRab297cen - Yumizen H500 OT Daily Guide PDFZhafira Afsheen Niesa100% (2)
- Herpes Brochure Body High ResDocument16 pagesHerpes Brochure Body High ResHeza MudahNo ratings yet
- Application Form 1Document3 pagesApplication Form 1thienndhNo ratings yet
- Curriculum VitaeDocument7 pagesCurriculum VitaeRossy Del ValleNo ratings yet
- Red Biotechnology ProjectDocument5 pagesRed Biotechnology ProjectMahendrakumar ManiNo ratings yet