Professional Documents
Culture Documents
IR-021 Postpartum Hemorrhage
Uploaded by
Muhammad ShakeelOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
IR-021 Postpartum Hemorrhage
Uploaded by
Muhammad ShakeelCopyright:
Available Formats
Shahida Khaliq
Faisalabad, Pakistan IR-021
Obstetrics
Postpartum Hemorrhage
O bstetric hemorrhage is the
world`s leading cause of
maternal mortality, causing 24% of, or
12 weeks post partum.6
Aetiology and Risk Factors
an estimated 127,000 maternal death PPH is commonly due to abnormalities
annually PPH is the most common type of one or a combination of four basic
of obstetric hemorrhage and accounts processes referred to in the 4 T's
for the majority of 14 million causes of mnemonic.
obstetric hemorrhage that occur each
year.PPH accounts for one quarter of Tone-Poor uterine contraction after
all maternal deaths world wide. l delivery.
Ti s s u e - Re t a i n e d Pr o d u c t s o f
Conception or Blood Clots.
In developing countries, PPH
Trauma- To Genital Tract.
accounts for over one third of all
Thrombin- Coagulation
maternal deaths. 2
Abnormalities.
Definition Common risk factors for PPH are
There is no single, satisfactory multiple Pregnancy, Poly-hydramnios,
definition of PPH. PPH is defined as F e t a l m a c r o s o m i a , o b e s i t y,
blood loss more than 500ml following Coagulation disorder, primigravidity,
vaginal delivery or more than 1000ml chorioamnionites, prolonged rupture
following Cesarean delivery.3 of membranes, fibroid uterus,
previous caesarean birth, antpartum
The Scottish confidential audit of hemorrhage, pre eclampsia,
severe maternal morbidity defines as induction of labour, prolonged labour,
major hemorrhage as estimated blood instrumental delivery and prior PPH,7
loss >2500ml or the transfusion of 5 halo-genated anesthetic agents,
or more units of blood or treatment for nitrates, non steroidal, and
Coagulopathy (Fresh Frozen Plasma, inflammatory drugs, magnesium
4
Cryoprecipitate, Platelets). sulfate, beta sympathomimetics,
nifedipine and hypothermia due to
Another definition is any blood loss massive rescuscitatation or prolonged
that causes hemodynamic instability uterus exteriorization.
e.g. a fall in blood pressure as the risk
of dying from PPH depends not only on In UK, there is an overall trend towards
the amount and rate of blood loss but later child bearing, increased
5
also on the health of the woman. maternal age at childbirth with
associated. Increased incidence of
TYPES OF PPH. caesarean and instrumental deliveries
PPH is classified as primary or as well as placenta previa.8, 9, 10
secondary. Primary PPH occurs within
the first 24hrs after delivery and Pathophysiology:-
secondary occurs between 24hr and The blood vessels that supply the
184 April to June 2010 INDEPENDENT REVIEWS
placental bed pass through an inter- include antenatal risk assessment and
lacing network of muscle fibres management that assures that anemia
(myometrium). The spiral arteriolar or other health problems are treated
arrangements in the uterus might lower and women are sufficiently healthy to
the arterial pressure with which the with stand PPH, as well as appropriate
blood enters the uterus. Myometiral management of labour and delivery.
contraction is the main driving force for
placental separation and constriction Components of active
for the blood vessels. This haemostatic management third stage of labor
mechanism is known as physiological The usual components include
sutures or living ligatures. When the 1. Administration of uterotonic
placenta separates, bleeding occurs agents with in 1 min of birth
from the placental bed. Uterine atony 2. Controlled Cord traction and
results in a failure of the living ligatures uterine message after delivery
to stop the bleeding. The active of placenta as appropriate.
management of the third stage of This approach reduces the risk
labour is associated with a reduction of of PPH and postpartum
the risk of PPH and less need for blood anemia, transfusion require-
transfusion by enhancing this ments, prolonged third stage
11
physiological process. of labour and use of thera-
Prevention peutic drugs of PPH.11
The prediction of PPH using antenatal
Clinical findings in obstetric hemorrhage.
Blood Pressure Degree of Shock
Blood Volume Loss Symptoms + Signs
(Systolic)
Palpitations, Tachycardia
500-1000(10-15%) Normal Compensated
Dizziness
Slight Fall Pale, Cool Skin, Weakness,
1500-2000ml(25-35%) Mild
(80-100mmhg) Sweating, Tachycardia
Blood Flow to vital organs
Moderate Fall (liver, Gut, Kidenys), Restlessness
1500-2000ml(25-35%) Moderate
(70-80mmhg) Pallor, Oliguria, Mottling of the skin
in the extremties especially the legs.
Marked Restlessness, Agitation collapse,
2000-3000ml(35-50%) Severe
(50-70mmhg) Air hanger, Anuria
risk assessment is poor only 40% of Use of Oxytocics:
women who develop PPH have an Injectable oxytocin is used mostly. It is
identified risk factor. However, PPH if first line agent because it is effective 2-
often a predictable event, women with 3 mins after injection and has minimal
identified risk factors should be secondary effects, it can be used in all
transferred to centers with transfusion women. Other uterotonics can be used
facilities and an intensive care unit for e.g. ergometrine 500ug 1M with 5 1U
delivery if these are not available / ml.12
locally. Prevention of PPH should
April to June 2010 INDEPENDENT REVIEWS 185
Misoprostol, it can be used by oral, Treatment
sublingual and rectal routes. The A systematic and step wise
misuse of misoprostol can lead to management of PPH can be achieved
significant maternal morbidity and with the use of the following measures.
even death. A recent Cochrane review
on the use of prostaglandins nor General Medical Management
misoprostal is preferable to Ask for Help
conventional Injectable uterotonics as Massive PPH should be managed with
part of the management of the third multi disciplinary input. Senior
stage of labour especially for low risk obstetricians, anesthetist and theatre
13
women. staff, hematologist and the blood bank
and hospital porters and intensive care
Carbetocin, a long acting oxytocin unit should be alerted.
agonist has been used for prevention of
PPH. Nevertheless, Carbetocin is Assess
associated with reduced need for Vital parameters, monitoring the
additional uterotonics agents and patient's vital signs, Level of
uterine message and there are no Consciousness, blood pressure, pulse,
significant differences in adverse effects Oxygen, saturation, estimation of
between carbetocin and oxytocin. 14 blood loss.
The WHO recommends that: Different methods of estimation have
1. Active management of the third been evaluated and guidelines to
stage of labour include admi- improve accuracy of the visual
nistration of a uterotonic soon estimation of blood loss have been
after birth of the baby, delay suggested.15
cord clamping and delivery of
the placenta by controlled cord
Resuscitation
traction followed by uterine
Two large bore cannula pass. Send
message.
blood for full blood count, group and
2. Active management of the third
cross match. Coagulation Screen.
stage of labour should be
Renal and Liver Profile,
offered by skilled attendants as
I. Raising the legs,
potential risks such as uterine
ii. Administer oxygen at 10-
inversion may result from
151/m.
inappropriate cord traction.
iii. A loss of 1 liter of blood
3. Oxytocin should be offered for
requires replacement with 4-5
prevention of PPH in
liters of crystalloid (0.9%
preference to oral, sublingual
normal saline and lactated
or rectal misoprostol.
ringers solution) or colloids
4. In the absence of active
until cross matched blood is
management of the third stage
available as most infused fluid
of labour, a uterotonic drug
shifts from the intravascular to
(oxytocin or misoprostol) 16
the interstitial space.
should be offered.
186 April to June 2010 INDEPENDENT REVIEWS
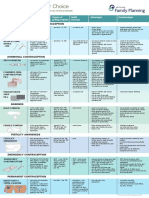
Management of Postpartum Hemorrhage
Abdominal pain Oozing from Massive Bleeding
and shock without venipuncture sites(rare)
vaginal bleeding (rare)
Consultation for consider coagulopathy call for help
possible retroperitoneal or (coagulation studies) Evaluate ABCs
paravaginal hematoma Administer Fluids
Administer oxygen
Consider transfusion
Placenta Delivered?
Yes No
Vigorous fundal message Manual Exploration
Oxytocin 10-30 unit rapidly in 1 litre of uterus
of intravenous fluid
Firm fundus, uterus contracted Indistinct Distinct
still bleeding bleeding stop claeavage plane cleavage plane
Explore for cervical,
vaginal, or vulvar lesions consider placenta Manual extraction
accereta of placenta
Vaginal, or vulvar Vaginal, or cervical No lesion
hematoma leceration consultation for probable
urgent hystrectomy
Manual exploration
of uterus.
Repair
up to 4cm 4cm or later
and stable and expanding bi manual compression
of uterus while awaiting help
Retained uterine uterine uterine
Placenta Repture inversion atony
ice packs incise, or clots
and observe drain+pack
Remove Resuscitation Resuscitation Resuscitation
+ urgent lapororomy Correction of inversion apply uterotonics
Apply tamponade
Uterine artery embolization
Laporotomy with compression
suture
Hystrectomy
April to June 2010 INDEPENDENT REVIEWS 187
The Golden Hour Negative blood should be transfused
The golden hour is the time at which until cross-matched blood become
resuscitation must be commenced to available. 1 liter of fresh frozen plasma
ensure the best chance of survival. The should be administrated with every 6
probability of survival decreases units of blood transfused.
sharply after the first hour if the patient
is not effectively resuscitated.17 Platelet Concentration should be kept
9
at more than 50* 10 / liter or more
9
A rule of 30 has been used for acute than 80-100* 10 /liter if surgical
management of shock. If the patient's intervention is likely.
systolic blood pressure fall by
30mmHg, heart rate (HR) rises by 30 Cryoprecipitate and other clothing
beats/min, RR increases to > 30 factor (VI11, XIII, Von Willebrand
beats/min and hemoglobin (Hb) or Factor) may be required if there is DIC
haematocrit (HCT) drop by 30% and or if the fibrinogen levels is less than
urinary output is < 30ml/hr, then the 10g/l. Recombinant factor VII may be
patient is most likely to have lost at least used in hemophilic patient's.
30% of her blood volume and is the
moderate shock leading to severe The incidence of thrombotic
shock. Shock index may also be used in complication occur in 1-2% with use of
the monitoring of the woman with PPH. recombinant factor VII.
It refers to heart rate divided by the
systolic blood pressure (SBP). The Treatment of Atony
normal value is 0.5 - 0.7 with In case of uterine atony, following
significant hemorrhage, it increases to measures should be taken to control
0.9 - 1.1.18 postpartum hemorrhage.
Establish aetiology, ecbolic, ensure Message the uterus, either manually
availability of blood. (hand on the fundus) or bimanually
(vaginal hand in the anterior fornix,
Establish Aetiology abdominal hand on the posterior
Identify the cause of bleeding by using aspect of the fundus) is a simple and
mnemonic 4T's. Through assessment of effective first line measure and reduces
the uterine size and tone should be bleeding.
followed by vigorous uterine message
and administration of therapeutic Oxytocin infusion, prostagtandins: I/V
uterotonic agents. bolus 10 units of oxytocin adminis-
tered. 40 units in 500ml of 0.9%
Manually exploration of the uterine normal saline, infused at a rate of
cavity under anesthesia to exclude 125ml/hr.
RPOC's and to look for extended tears
in the cervix and high in the vaginal If the uterus remains atonic after initial
wall excluded Coagulopathy. oxytocic therapy, syntometrine or
ergometrine should be repeated.
Treatment of Coagulopathy Carboprost is a prostaglandin F2α
Group specific or group O, Rh- analogue which is administered
188 April to June 2010 INDEPENDENT REVIEWS
intramuscularly and intramyometrially until a hospital can be reached. A pilot
0.25mg repeated every 15min to a study showed that compared with
maximum dose of 2mg. This is 80-90% women in a control group, bleeding
effective in stopping PPH. It has bronc- decreased by 50% in women
hoconstrictive properties, therefore experiencing various forms of obstetric
contra-indicated in asthma. Side haemorrhage in whom the NASG was
effects include diarrhea, vomiting, used. 21
fever, headache and flushing.
T- Tissue and trauma to be
Dinoprostone is a prostaglandin E2 excluded and to proceed to
analogue which may be used vaginally tamponade with balloon or
or rectally. It has effect on hypothalamic uterine packing.
thermoregulation and can cause
temperature elevation. Previously, uterine packing was
considered that
Misoprostol is a synthetic prosta- I. It was a potentially traumatic
glandin E1 analogue misoprostol use and time consuming proce-
was associated with a significant dure.
increase of maternal pyrexia and ii. Might conceal on-going
shivering.19 A recent Cochrane review hemorrhage.
concluded that there is insufficient iii. Might predispose to the
evidence to show that the addition of develop-ment of infection.
misoprostol is superior to the iv. Non physiological approach.
combination of oxytocin and
ergometrine for the treatment of But now, Maier concluded that unterine
primary PPH20. A combination of these packing is a safe, quick and effective
two agents could provide a sustained procedure for controlling PPH. 22
uterotonic effect.
Uterine balloon tamponade
Surgical Number of devices, including the
When medical treatment fail then foley's catheter, a condom, the
surgical treatment applied. sengstaken-blackmore oesophageal
catheter (SBOC), the rush urological
S- Shift to operating theatre (anti-shock hydrostatic balloon and the bakri
garment, especially if transfer is ballon has been used. The SBOC has
required and bimanual compression). been the most frequently reported
device. Overall, the reported success
23
From low resource settings transfer to a rates vary between 70-100%, Use of
centre with facilities is indicated. balloon tamponade in the successful
Antishock garment can reverse the management of PPH secondary to
effect of shock on the body's blood extensive vaginal lacerations has been
24
distribution by applying external recently been reported.
counter pressure to the legs and
abdomen and returning blood to the Balloon is inserted and uterine fundus
vital organs, thus stablizing women is palpated abdominally and mark.
Then oxytocin infusion administered to
April to June 2010 INDEPENDENT REVIEWS 189
keep the uterus contracted and monitor artery embolisation done where facili-
vitals every 30mins. Antibiotic cover ties available to control bleeding.
should be given.
Arterial embolisation under fluoros-
After 6-8 hrs, the uterine fundus copic guidance is also used. The
remains at the same level and there is success rates may be as high as 70-
no active bleeding then catheter 100% and the procedure has the
removed, keep the patient fasting for potential to preserve fertility.
2hrs after removing balloon.
Prophylatic embolisation may have a
Apply Compression Sutures role in a planned caesarean section
If the patient is stable and bimanual when the placenta is thought to be
compression sutures may be used. B- morbidly adherent.27
25
Lynch suture techniques is used. The
ease of application of such sutures is a Complications include, hematoma
β-lynch suture major advantage and fertility is formation, infection, contrast related.
conserved. The disadvantage are the Side effects and ischemia resulting in
need for laparotomy and hysterectomy. uterus and bladder necrosis. The need
Complications include erosion through for specialized equipment and an
the uterine wall, pyometra and uterine interventional radiologist with a high
necrosis. degree of expertise are limitations of
this procedure.
Systemic Pelvic devascularisation
Systemic Pelvic devascularisation done Subtotal or total abdominal
where facilities available to control hysterectomy
bleeding. Subtotal or total abdominal hyste-
rectomy as usually the final option in
Pelvic devascularisation requires the management of PPH and should
laparotomy and progressive, step wise not be delayed if the conservative
devascularisation.
26
measures have failed. Hysterectomy is
associated with numerous post-
Whereby the uterine ovarian and finally operative complications, including
internal iliac arteries are ligated. urinary tract injury, fistula formation,
bowel injury, vascular injury, pelvic
Vaginal ligation of the uterine arteries haematoma and sepsis. The loss of
has also been described. Prerequisite child bearing potential and the
include a haemodynamically stable psychological consequences should
patient substantial surgical expertise also be considered.
and a desire to preserve fertility. The
reported success rates are between 90- All these surgical techniques (Uterine
100%. tamponade, devascularisation,
compression sutures and hyste-
Interventional radiology with rectomy) requires the ready availability
uterine artery embolisation. of specific instruments and equipment.
Interventional radiology with uterine For this purpose, an obstetric
hemorrhage equipment tray in the
190 April to June 2010 INDEPENDENT REVIEWS
labour ward will facilitate prompt hysterectomy.28
surgical management of severe
obstetric hemorrhage and may reduce Long Term Complications
the need of blood transfusion and Pa t i e n t ' s w h o h a v e m a s s i v e
REFERENCES
1. World Health Organization. The multivariate analysis of 10,053
world health report 2005, Make every Cases. J Perinat Med 2003; 31: 209-
mother and child count. Geneva: 215.
WHO, 2005.
10. Cleary-Goldman J, Malone FD,
2. K h a n K S, Wo j d y l a D, S a y l , Vidaver J et al. Impact of maternal
gulmezoglu AM, VAN COOK age on obstetric outcome. Obstet
PF.WHO analysis of causes of gynecol 2005; 105 : 983-990.
maternal death: a systematic review-
Lancet 2006; 367: 1066-1074. 11. Pr e n d i v i l l e W J, E l b o u r n e D,
McDonald S. Active Versus Expectant
3. Baskelt TF. Complications of the third management in the third stage of
stage of labour. In: Essential labour. Cochrane Database Syst Rev
Management of Obstetrical 2000(3): CD 000007.
Emergencies. 3rd ed. Bristol, England,
Clinical Press; 1999; 196-201. 12. H o f m e y r G J , Wa l r a v e n G ,
Gulmezoglu AM, Maholwana B,
4. Penney G, Kernaghan D, Adamson L. Alfirevic Z, Villar J. Misoprostol to
Scottish Confidential audit of severe Treat Post-Pactum Hemorrhage: a
maternal morbidity 3rd Annual Report systematic review Br J Obstet Gynecol
2005. Edinburgh: Scottish 2005; 112:547-553.
Programme for Clinical Effectiveness
in Reproductive Health, 2005. 13. Gulmezoglu A, Forna F, Villar J,
Hofmeyr G. Prostaglandins for
5. D u n l o p W i l l i a m , L e d g e r. L . preventing Post-Pactum Hemorrhage,
William. Recent advances in Cochrane Database Syst Rev
obstetrics and Gynecology 24, 2007(3): CD 005494.
2008; 89-104.
14. SUL, Chong Y, Samuel M.oxytocin
6. ACOG Practice Bulletin: Clinical agonists for preventing Post-Pactum
Management, Guidelines for Hemorrhage, Cochrane Database
obstetrics and gynecology number Syn Rev 2007(3): CD 005457.
76, October 2006: Post-Partum
Hemorrhage. Obstetric Gynecol 15. Bose P, Regan F, Paterson-Brown S.
2006;108:1039-1047. improving the accuracy of estimated
blood loss at obstetric hemorrhage
7. Kominiarck MA, Kilpatrick SJ. Post- using clinical reconstructions. Br J
Partum Hemorrhage recurring Obstet Gynecol 2006; 113:919-
pregnancy complication semen 924.
perinatal 2007;31:159-166.
16. Ramanathan G, Arulkumaran
8. Office For National Statistics. S. Post-Pactum Hemorrhage. JObstet
Average age of mother at childbirth: Gynecol Can 200628:967-973.
S o c i a l Tr e n d s 3 3 . 2 0 0 3
<WWW.Statistics.Gov.UK.> 17. Lalonde A, Daviss BA Acosta A,
H e r s c h d e r f e r K ; Po s t- Pa c t u m
9. Ohkuch A, Onagawa T, Usui R et al. Hemorrhage today: ICM / F1GO
Effect of maternal age on blood loss initiative 2004-2006. Int J Gynecol
during parturition a retrospective Obstet 2006; 94: 243-253.
April to June 2010 INDEPENDENT REVIEWS 191
when medical treatment fails. Obstet
18. Chandraharan E, Arulkumaran S. Gynecol Surv 2007; 62: 540-547.
Massive Post-Pactum Hemorrhage 24. Tattersall M, Braithwaite W. Ballon
and Management of Coagulopathy. Tamponade for Vaginal Lacerations
Obstet Gynecol Report Med 2007; c a u s i n g S e v e r Po s t - Pa c t u m
17: 119-122. Hemorrhage Br J Obstet Gynecol
2007; 1 14: 647-648.
19. Walraven G, Dampha Y, Bittaye D,
Sowe M, Hofmeyrt, Misoprostol in 25. Pereira A, Nunes F, Peelroso S,
the treatment of Post-Pactum Saraiva J, Retto H, Meirinho M,
Hemorrhage in addition to routine Compressive Uterine Sutures to treat
management: a placebo Post-Patum Bleeding Secondary to
randomized controlled trail. BrJ Uterine atony. Obstet Gynecol 2005;
Obstet Gynecol 2004; 111: 1014- 106:569-572.
1017.
26. AbdRabbo SA. Stepwise uterine
20. Mousa HA, Alfirevic Z. Treatment for devascularisation: a novel technique
Primary Post-Pactum Hemorrhage. for management of uncontrollable
Cochrane Database Syst Rev Post-Pactum Hemorrhage with
2007(1): CD003249. Preservation of the uterus. Am J
Obstet Gynecol 1994; 171: 694-
21. Milter S, Hamza S, Bray EH et al. First 700.
aid for obstetric hemorrhage: the pilot
study of the non-pneumatic anti shock 27. Cheng YY, Hwang JI, Hung SW et al.
garment in Egypt. Br J Obstet Gynecol Angiographic embolization for
2006; 1 13: 424-429. emergent and prophylactic
management of obstetric
22. Maier RC.Control of Post-Pactum hemorrhage: a four year experience. J
Hemorrhage with uterine packing. Chin Med Assoc 2003; 66: 727-734.
Am J Obstet Gynecol 1993; 169:
317-321. discussion 321-323. 28. BasKett TF. Surgical management of
sever obstetric hemorrhage:
23. Doumouchtasis SK, Papageorghiou experience with an obstetric
AT, Arulkumarran S. Systematic review hemorrhage equipment tray. J
of Conservative management of Post- Obstet Gynecol Can 2004, 26:
Pactum Hemorrhage: What to do
The author :
Shahida Khaliq MBBS, FCPS
is Senior Register
(Gynaecology/Obstetrics)
Independent Medical
College Faisal-abad.
192 April to June 2010 INDEPENDENT REVIEWS
You might also like
- Algorithm For HPPDocument7 pagesAlgorithm For HPPnoor ainNo ratings yet
- Post-Partum Haemorrhage: Causes and Risk FactorsDocument12 pagesPost-Partum Haemorrhage: Causes and Risk FactorsLindha GraNo ratings yet
- B41. Su-Et-Al PPH PDFDocument21 pagesB41. Su-Et-Al PPH PDFjhon heriansyahNo ratings yet
- Postpartum CollapseDocument54 pagesPostpartum Collapsemedical chroniclesNo ratings yet
- 62 PPH Including Coagulation Failure in ObstetDocument46 pages62 PPH Including Coagulation Failure in ObstetcollinsmagNo ratings yet
- Postpartum Hemorrhage PDFDocument21 pagesPostpartum Hemorrhage PDFLillian HerreraNo ratings yet
- Antepartum and Postpartum Hemorrhage: Fitsum AshebirDocument64 pagesAntepartum and Postpartum Hemorrhage: Fitsum Ashebirzuzuyasi65No ratings yet
- Maedica 11 55 PDFDocument6 pagesMaedica 11 55 PDFM Iqbal EffendiNo ratings yet
- Antepartum HemorrhageDocument6 pagesAntepartum HemorrhageEsam EsamNo ratings yet
- Physiological Changes in PregnancyDocument7 pagesPhysiological Changes in PregnancyFarid DjafarNo ratings yet
- Coagulation Management and Transfusion in Massive Postpartum HemorrhageDocument7 pagesCoagulation Management and Transfusion in Massive Postpartum HemorrhageAlberto LiraNo ratings yet
- Thrombo Embolism and PregnancyDocument9 pagesThrombo Embolism and Pregnancysangeetha francisNo ratings yet
- Massive PPHDocument7 pagesMassive PPHCatherine PingNo ratings yet
- Eclampsia PPHDocument43 pagesEclampsia PPHizafamirna743No ratings yet
- Prevention and Management of Postpartum Hemorrhage: Regional Campus, Monroeville, PennsylvaniaDocument8 pagesPrevention and Management of Postpartum Hemorrhage: Regional Campus, Monroeville, PennsylvaniaTap TitanNo ratings yet
- Hemo Obstetrica PDFDocument10 pagesHemo Obstetrica PDFMayra caplaNo ratings yet
- Obstetrics and GyenacologyDocument37 pagesObstetrics and GyenacologySharoon KumarNo ratings yet
- Obstetrics Maternal Haemorrhage: M. Walfish, A. Neuman and D. WlodyDocument10 pagesObstetrics Maternal Haemorrhage: M. Walfish, A. Neuman and D. WlodySakena NurzaNo ratings yet
- Hem 2020000139 CDocument5 pagesHem 2020000139 CA.21-AH0602- VINA SHALSABINANo ratings yet
- Late Pregnancy Bleeding: Kareem Ayman Sultan 200008Document67 pagesLate Pregnancy Bleeding: Kareem Ayman Sultan 200008200008No ratings yet
- An Overview On The Cause Andmanagement of PostparDocument6 pagesAn Overview On The Cause Andmanagement of Postparmusyawarah melalaNo ratings yet
- Resume Luar Negeri Dita FebriyantiDocument9 pagesResume Luar Negeri Dita FebriyantiDita FebriyantiNo ratings yet
- 5.bleeding During PXDocument34 pages5.bleeding During PXBekeNo ratings yet
- Hipertension en El EmbarazoDocument12 pagesHipertension en El EmbarazofsitoNo ratings yet
- Postpartum HemorrhageDocument21 pagesPostpartum HemorrhageCintya PradyanthiNo ratings yet
- Postpartum HemorrhageDocument7 pagesPostpartum HemorrhageRivano Frits Henry PandalekeNo ratings yet
- Postpartum Haemorrhage Dr. G. Al-ShaikhDocument51 pagesPostpartum Haemorrhage Dr. G. Al-ShaikhRaphzid InurfaceNo ratings yet
- Obstetric HaemorrhageDocument4 pagesObstetric Haemorrhageapi-142637023No ratings yet
- Postpartum HemorrhageDocument22 pagesPostpartum HemorrhageReynaldiReikyHadiwijayaNo ratings yet
- Antepartum HemorrhageDocument43 pagesAntepartum HemorrhageFedlu SirajNo ratings yet
- Postpartum Hemorrhage, Update 2016Document31 pagesPostpartum Hemorrhage, Update 2016Marthin Fernandes PasaribuNo ratings yet
- 123 PDFDocument14 pages123 PDFSachin SinghNo ratings yet
- Postpartum HaemorrhageDocument44 pagesPostpartum Haemorrhageella_28No ratings yet
- 17pages405 414Document15 pages17pages405 414ragil putra jNo ratings yet
- 3 - ICM 2 - PPH - NotesDocument6 pages3 - ICM 2 - PPH - NotesthaniaNo ratings yet
- Emily B. Baglione CRNA, BSN, MS,: Chief OB CRNA, Anesthesia Group of AlbanyDocument55 pagesEmily B. Baglione CRNA, BSN, MS,: Chief OB CRNA, Anesthesia Group of AlbanyAsyfiyaTami100% (1)
- Thrombocytopenia in PregnancyDocument12 pagesThrombocytopenia in PregnancyzoyaNo ratings yet
- 1 PPH & Placenta DRDocument126 pages1 PPH & Placenta DRGetaneh LiknawNo ratings yet
- Hypertensive Disorders of Pregnancy PDFDocument9 pagesHypertensive Disorders of Pregnancy PDFMohammed AbdNo ratings yet
- Prevalence of Obstetric Haemorrhage On A Teaching HospitalDocument7 pagesPrevalence of Obstetric Haemorrhage On A Teaching Hospitalodunze augustusNo ratings yet
- Coagulation Disorders in ObsDocument33 pagesCoagulation Disorders in Obsapule geraldhumbleNo ratings yet
- Care of HemophiliaDocument7 pagesCare of HemophiliaBasant karn100% (4)
- Obstetrical EmergenciesDocument39 pagesObstetrical EmergenciesDani AsmareNo ratings yet
- Postpartum Haemorrhage (PPH) : DR - Shameem R. AlaasamDocument41 pagesPostpartum Haemorrhage (PPH) : DR - Shameem R. Alaasamمصطفى محمدNo ratings yet
- PPH AlgorithmDocument69 pagesPPH AlgorithmMadhumithaNo ratings yet
- Identification, Prevention and Management of Postpartum HaemorrhageDocument11 pagesIdentification, Prevention and Management of Postpartum HaemorrhageCaitlynNo ratings yet
- Post Partum Haem.Document90 pagesPost Partum Haem.rachael annor100% (1)
- Obstetrics V13 Obstetric Emergencies Chapter Diagnosis and Management of Shock in Postpartum Hemorrhage 1682196492Document14 pagesObstetrics V13 Obstetric Emergencies Chapter Diagnosis and Management of Shock in Postpartum Hemorrhage 1682196492lizzieNo ratings yet
- Nejmra 1513247Document11 pagesNejmra 1513247Jose BoderoNo ratings yet
- Bleeding During PregnancyDocument5 pagesBleeding During PregnancyMaryela Maceda GalozoNo ratings yet
- Amniotic Fluid Embolism (AFE)Document26 pagesAmniotic Fluid Embolism (AFE)sanjivdas100% (1)
- The Role of Fibrinogen in Postpartu - 2022 - Best Practice - Research Clinical ADocument12 pagesThe Role of Fibrinogen in Postpartu - 2022 - Best Practice - Research Clinical APaulHerreraNo ratings yet
- Postpartum HaemorrhageDocument51 pagesPostpartum HaemorrhageAisha AuliaNo ratings yet
- Emergency Implementation For Bleeding in PregnancyDocument6 pagesEmergency Implementation For Bleeding in PregnancyAmethystNo ratings yet
- Piis0007091217315908 PDFDocument13 pagesPiis0007091217315908 PDFJothy DeepakNo ratings yet
- Antepartum Haemorrhage: Common Causes of APHDocument7 pagesAntepartum Haemorrhage: Common Causes of APHdeweNo ratings yet
- ITPDocument27 pagesITPYosuaNo ratings yet
- Postpartum HemorrhageDocument53 pagesPostpartum HemorrhageDr_Soranus100% (2)
- Post Partum HaemorrhageDocument6 pagesPost Partum Haemorrhagenancy jeyakumarNo ratings yet
- M. Shakeel Talat: ObjectiveDocument2 pagesM. Shakeel Talat: ObjectiveMuhammad ShakeelNo ratings yet
- Ir-038 Examination of Common Peroneal NerveDocument2 pagesIr-038 Examination of Common Peroneal NerveMuhammad ShakeelNo ratings yet
- 014 Breast ExaminationDocument10 pages014 Breast ExaminationMuhammad ShakeelNo ratings yet
- Clinical ClerkingDocument17 pagesClinical ClerkingMuhammad ShakeelNo ratings yet
- Ir-029 Fluid and Electrolytes - 4Document9 pagesIr-029 Fluid and Electrolytes - 4Muhammad ShakeelNo ratings yet
- IR - 036 Sciatic NerveDocument2 pagesIR - 036 Sciatic NerveMuhammad ShakeelNo ratings yet
- Ir-024 GangreneDocument5 pagesIr-024 GangreneMuhammad ShakeelNo ratings yet
- Participation Evaluation CriteriaDocument1 pageParticipation Evaluation CriteriaMuhammad ShakeelNo ratings yet
- FormularyDocument123 pagesFormularyMuhammad Shakeel100% (3)
- Possible Interview Questions For NursesDocument32 pagesPossible Interview Questions For NursesElisabeta Ivan75% (4)
- Pulmonary RehabilitationDocument86 pagesPulmonary RehabilitationJuanitoCabatañaLimIIINo ratings yet
- MSC Project Presentation 29 MarchDocument36 pagesMSC Project Presentation 29 MarchdreamroseNo ratings yet
- Microbiologist: 3.1.5 Isolation & Gram StainingDocument5 pagesMicrobiologist: 3.1.5 Isolation & Gram Stainingapi-534896073No ratings yet
- Parents Consent AY 2022 2023Document2 pagesParents Consent AY 2022 2023Jayloid AlteaNo ratings yet
- American Medical Society For Sports MedicineDocument13 pagesAmerican Medical Society For Sports MedicineAlvaroNo ratings yet
- 19-26 Faktor Risiko Kejadian Hipertensi Pada Wanita Usia Subur Di Wilayah Kerja Puskemas NaibonatDocument8 pages19-26 Faktor Risiko Kejadian Hipertensi Pada Wanita Usia Subur Di Wilayah Kerja Puskemas Naibonatlidya inaNo ratings yet
- Marijuana: Aron H. Lichtman Professor Department of Pharmacology and ToxicologyDocument67 pagesMarijuana: Aron H. Lichtman Professor Department of Pharmacology and Toxicologyunknown racerx50No ratings yet
- RCSI Bahrain ConnectED Newsletter Winter 2022-23Document32 pagesRCSI Bahrain ConnectED Newsletter Winter 2022-23Yousif YousifNo ratings yet
- Leprosy TiarmaDocument23 pagesLeprosy TiarmaFadhilannisaNo ratings yet
- IontophoresisDocument4 pagesIontophoresisDr GowrishankarPotturi PTNo ratings yet
- SpecialistDocument1 pageSpecialistShashiNo ratings yet
- PatellofemuralDocument216 pagesPatellofemuralandrei_costea100% (2)
- Clinical Documentation Improvement For Physician E/M CodingDocument5 pagesClinical Documentation Improvement For Physician E/M CodingAudioEducatorNo ratings yet
- Prevenção de Trauma Perineal Revisão Cochranne 2017Document89 pagesPrevenção de Trauma Perineal Revisão Cochranne 2017Francine XavierNo ratings yet
- The Effectiveness of Cognitive Behavioral Therapy (CBT) On Generalized Anxiety Disorder (GAD)Document8 pagesThe Effectiveness of Cognitive Behavioral Therapy (CBT) On Generalized Anxiety Disorder (GAD)nadia rukmanaNo ratings yet
- Module 6.2 - 2022Document36 pagesModule 6.2 - 2022Bogdan Roxana-MariaNo ratings yet
- Immunology of Transplant RejectionDocument8 pagesImmunology of Transplant Rejectionxplaind100% (1)
- Turner P. Clinical Guide To Oral Implantology... 3ed 2018Document226 pagesTurner P. Clinical Guide To Oral Implantology... 3ed 2018Daniel EmilevNo ratings yet
- DSM5 Clasification Diagnostic Criteria Changes PDFDocument7 pagesDSM5 Clasification Diagnostic Criteria Changes PDFlilomersNo ratings yet
- Myco Viro Notes Module 6Document6 pagesMyco Viro Notes Module 6Kyle Jude Roberts SanesNo ratings yet
- Serviciile Sociale in Situatii de RiscDocument15 pagesServiciile Sociale in Situatii de RiscAlina HoaraNo ratings yet
- Contraception Options in New ZealandDocument2 pagesContraception Options in New ZealandStuff NewsroomNo ratings yet
- Facts Speak Louder Than The Silent Scream 03-02Document6 pagesFacts Speak Louder Than The Silent Scream 03-02ProgressTXNo ratings yet
- End The Insomnia Struggle - A Step-by-Step Guide To Help You Get To Sleep and Stay Asleep PDFDocument234 pagesEnd The Insomnia Struggle - A Step-by-Step Guide To Help You Get To Sleep and Stay Asleep PDFBella Donna100% (1)
- 【Invitation】Educational Webinar Series for Asia-Pacific Pediatrics EP physicians and early career EPsDocument7 pages【Invitation】Educational Webinar Series for Asia-Pacific Pediatrics EP physicians and early career EPsSantoso 9JimmyNo ratings yet
- Broad Spectrum AntibioticsDocument17 pagesBroad Spectrum AntibioticsRabi ShahNo ratings yet
- Class 12 Physical Education Chapter 1 Planning in Sports Question/AnswerDocument7 pagesClass 12 Physical Education Chapter 1 Planning in Sports Question/AnswerPihoo MohanNo ratings yet
- ResumeDocument5 pagesResumeJuvie Dawn MaquilanNo ratings yet
- Epid 1.1Document194 pagesEpid 1.1devtarioNo ratings yet