Professional Documents
Culture Documents
Assessing The Value of Diagnostic Tests: A Framework For Designing and Evaluating Trials
Uploaded by
Marisela FuentesOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Assessing The Value of Diagnostic Tests: A Framework For Designing and Evaluating Trials
Uploaded by
Marisela FuentesCopyright:
Available Formats
RESEARCH METHODS AND REPORTING
Assessing the value of diagnostic tests:
a framework for designing and
evaluating trials
Lavinia Ferrante di Ruffano,1 Christopher J Hyde,2 Kirsten J McCaffery,3 Patrick M M Bossuyt,4
Jonathan J Deeks1
1
Department of Public Health, The value of a diagnostic test is not testing strategies; thus studies that compare test strategies
Epidemiology, and Biostatistics,
School of Health and Population simply measured by its accuracy, but and estimate differences in sensitivity and specificity are
more informative than those that evaluate the accuracy of
Sciences, University of Birmingham,
Birmingham B15 2TT, UK
depends on how it affects patient health. one test or diagnostic strategy.2 Thirdly, improvements in
2
PenTAG, Institute for Health This article presents a framework for the test accuracy will not benefit patients unless they lead to
Services Research, Peninsula
College of Medicine and Dentistry, design and interpretation of studies that changes in diagnoses and patient management, requiring
evaluations of the effect of improved accuracy on decision
University of Exeter, Exeter, UK
3
Screening and Test Evaluation
evaluate the health consequences of making.3 Finally, improved decision making is only one
Program, School of Public Health, new diagnostic tests route by which tests affect patient health, and empirical
University of Sydney, Sydney,
Australia
evaluations are needed to compare the effect of test strate-
4
Department of Clinical Most studies of diagnostic tests evaluate only their accu- gies on patient health.4
Epidemiology and Biostatistics, racy. Although such studies describe how well tests iden- Ideally, new tests should only be introduced into clini-
Academic Medical Centre, tify patients with disease (sensitivity) or without disease cal practice if evidence indicates that they have a better
University of Amsterdam,
Amsterdam, Netherlands (specificity), further evidence is needed to determine a chance of improving patient health than existing tests.5 6
Correspondence to: Jonathan J tests true clinical value. Firstly, since tests are rarely used Tests can be compared by evaluating the downstream con-
Deeks j.deeks@bham.ac.uk in isolation, studies are needed that evaluate the perform- sequences of testing on patient outcomes, either directly
Accepted: 30 November 2011
ance of testing strategies, accounting for when and how in a randomised controlled trial or by decision analysis
Cite this as: BMJ 2012;344:e686
doi: 10.1136/bmj.e686
a new test is used within a diagnostic pathway, and how models that integrate multiple sources of evidence. Test-
its findings are combined with results of other tests.1 Sec- treatment trials randomly allocate patients to tests, follow
ondly, decision making involves selecting among multiple up subsequent management, and measure outcomes only
after treatment has been received (fig 1).7 Decision models
Participants
use existing clinical data to extrapolate, through a number
Adults in intensive care receiving mechanical ventilation of assumptions, the link between intermediate outcomes
for at least 4 days and with suspected pneumonia (such as accuracy) and long term outcomes.8 A key issue
for trials and decision models is the selection of outcomes
Randomisation that need to be measured or modelled to evaluate how
Response on bmj.com
In order to practice evidence tests are affecting patients. This selection requires a priori
Tests for confirmation of
based medicine properly, the disease and identification knowledge of the mechanisms by which tests affect patient
diagnostic process leading to of causative organisms* health.
sensible selection of patients In this article, we provide a comprehensive review of the
likely to benefit from treatment Bronchoalveolar lavage Endotracheal aspiration mechanisms that can drive changes to patient health from
has to be understood more with quantitative culture with non-quantitative culture testing, and include a summary checklist to assist readers,
clearly, and especially if value researchers, and funders who wish to design or appraise
based pricing of drugs is to be Management
+ + studies evaluating diagnostic tests. We have based our
used in the NHS
Huw Llewelyn, Abergavenny, Stop Targeted Stop Targeted framework on a review of a large cohort of published test-
Wales antibiotics antibiotics antibiotics antibiotics treatment trials 9 and key methodological literature.
To respond to an article on
Primary outcome (measured at 28 days)
bmj.com, click Response to this Effect of tests on patient health
article) Mortality Mortality Mortality Mortality To establish whether a new diagnostic test will change
bmj.com Recent RMRs health outcomes, it must be examined as part of a broader
Clinical prediction rules management strategy. Testing represents the first step of
(BMJ 2012;344:d8312) Fig 1|Design of a test-treatment randomised trial assessing a test-treatment process: (1) a test is administered to iden-
How
to search for unpublished whether bronchoalveolar lavage reduces the rate of death from tify a target condition, (2) the test result is considered (3)
clinical trial evidence ventilator associated pneumonia compared with endotracheal
alongside other evidence to decide a diagnosis, and (4)
(BMJ 2012;344:d8013) aspiration.7 *All patients received broad spectrum antibiotics
The Cochrane Collaborations while waiting for test results. In patients with confirmed
a course of treatment is identified (5) and implemented
tool for assessing risk of bias pneumonia, antibiotics were adjusted using culture results (fig 2).10
in randomised trials (BMJ and sensitivities; in test negative patients, antibiotics were Changes to any aspect of this pathway after the introduc-
2011;343:d5928) discontinued tion of a new test could trigger changes in health outcomes.
18 BMJ | 10 MARCH 2012 | VOLUME 344
RESEARCH METHODS AND REPORTING
Table 1 lists the mechanisms that commonly affect health
outcomes. (1) Patient given diagnostic test (2) Test result produced
Direct test effects (3) Diagnosis made
Test procedure
Some diagnostic procedures carry a risk of harm, hence (4) Management decided
alternatives that offer reduced procedural morbidity will
be of immediate benefit to patients. For example, use of Patient outcome (5) Treatment implemented
sentinel lymph node biopsy rather than dissection of the
axillary node to investigate metastatic spread in patients Fig 2| Simplified test-treatment pathway showing each
with early breast cancer results in much lower rates of post- component of a patients management that can affect health
outcomes10
operative swelling of the arm, seroma formation, numb-
ness, and paraesthesia.11
Test accuracy, diagnostic yield, therapeutic yield, and
Altering clinical decisions and actions treatment efficacy
Feasibility and interpretability More accurate tests will improve patient outcomes if the
The downstream value of a test will be impaired at the out- reductions in false positive or false negative results lead to
set if there are contraindications to its use or if it is prone more people receiving appropriate diagnoses (diagnostic
to technical failure (feasibility), while tests that are more yield) and appropriate treatment (therapeutic yield). The
difficult to interpret (interpretability) could produce fewer degree to which appropriate treatment can improve patient
definitive results. Either problem could require additional outcomes depends on its efficacy (treatment efficacy). In
investigations, increasing the time to diagnosis, or reduc- a trial evaluating the effect of fluorescence cystoscopy on
ing diagnostic and therapeutic yields through incorrect the recurrence of bladder carcinoma in situ, the enhanced
decision making or poor diagnostic confidence. accuracy of fluorescence cystoscopy compared with white
We observed this in a trial evaluating the diagnosis of light cystoscopy alone led to a substantial increase in lesions
coronary artery disease. Patients with acute chest pain being identified and treated at initial diagnosis, which signifi-
who were allocated to exercise electrocardiography were cantly reduced the rate of recurrence.13
significantly more likely to be referred for further investiga-
tion (coronary angiography) than those allocated to stress Diagnostic and therapeutic confidence
echocardiography.12 This finding was caused by the higher Although diagnostic yield generally increases with accuracy,
frequency of inconclusive diagnoses produced by exercise it is also affected by a doctors confidence in the diagnostic
electrocardiography, some of which were because the test test. Tests inducing greater confidence could benefit patients
was contraindicated. by reducing the need for further investigations and shorten-
ing the time to treatment. The results of a trial evaluating
Table 1|Attributes of the test-treatment pathway that affect patient health the triage of patients with non-small cell lung cancer who
Pathway component were referred for operative staging with positron emission
and mechanism Definition tomography (PET), show how a lack of diagnostic confidence
(1) Diagnostic test delivered
can over-ride the benefits of improved accuracy.14 PET identi-
Timing of test Speed with which a test is performed within the management strategy
fied patients for whom surgery was not indicated because of
Feasibility Completion of test process. Reasons for non-completion are: patient acceptability (patients
refusal to have test), test was contraindicated (clinical reason not to administer test), and incurable mediastinal disease, but no difference was found
technical failure (ability of diagnostic equipment to produce data) in the proportion of patients avoiding a thoracotomy (the pri-
Test process Patients interaction with test procedure, potentially causing physical or psychological mary outcome) because surgeons still preferred to confirm
harms or benefits
PET findings using standard operative staging.
(2) Test result produced
Doctors confidence in the ensuing success of a treat-
Interpretability Degree to which test data can be used to inform a diagnostic classification
Accuracy Ability of a test to distinguish between patients who have disease and those who do not ment plan can affect treatment effectiveness by influencing
Timing of results Speed with which test results are available the approach to treatment, particularly in surgery. Digital
(3) Diagnosis made subtraction angiography (DSA) and multidetector row
Timing of diagnosis Speed with which a diagnostic decision is made computed tomographic angiography (MDR-CTA) can both
Diagnostic yield Degree to which the test contributes to a patient diagnosis in any form, including: provision determine the location and degree of vascular narrowing in
of a definitive diagnosis, confirmation of a suspected diagnosis, ruling out a working patients with symptomatic hardening of peripheral arter-
diagnosis, and distinguishing between alternative diagnoses with different treatment
implications. Diagnostic yield is different from accuracy because it also incorporates any ies. Doctors using DSA were significantly more confident of
other information used by a doctor to make a diagnosis (such as previous test results) plans for surgery, owing to the tests clearer vascular images;
Diagnostic confidence Degree of confidence that doctors and patients have in the validity or applicability of a test however, MDR-CTA images were found to obscure interpreta-
result
tion and decrease confidence in the presence of vessel wall
(4) Management decided
calcifications.15
Therapeutic yield Degree to which diagnostic decisions affect treatment plans
Therapeutic confidence Certainty with which doctors and patients pursue a course of treatment
(5) Treatment implemented Changing timeframes of decisions and actions
Timing of treatment Speed with which patients receive treatment Tests that are undertaken earlier or produce results more
Treatment efficacy Ability of the treatment intervention to improve patient outcomes quickly can improve health outcomes. For example,
Adherence Extent to which patients participate in the management plan, as advised by their doctor, to patients with unstable angina and non-ST segment elevated
attain therapeutic goal myocardial infarction allocated to receive early coronary
BMJ | 10 MARCH 2012 | VOLUME 344 19
RESEARCH METHODS AND REPORTING
Table 2|Checklist to determine clinically important differences between test-treatment pathways of new and existing diagnostic test strategies
Test-treatment pathway Outcome to
Component Mechanism Questions Yes/no Notes capture difference
(1) Test delivery Timing of test
Time to test delivery Do the strategies provide testing within comparable timeframes (or does one strategy deliver a
diagnostic test considerably earlier than the other)?
Feasibility
Acceptability Is the new test likely to be as acceptable to patients as the existing test (or does one test cause
increased discomfort, for example)?
Clinical Is the new test likely to be suitable in similar proportions of the relevant patient group (or will the
contraindications new test be contraindicated in more or fewer patients than the existing test)?
Technical failure Do the two tests produce similar proportions of failed procedures (or does the process of one test
rates tend to fail more frequently than the other)?
Test process
Procedural harms or Are the two tests similar in how they affect patients during their application, physically or
benefits psychologically (or is one test more intrusive than the other or has a higher procedural morbidity
than the other)?
Placebo effect Does the new strategy give patients a similar perspective on being investigated (or could the new
strategy encourage patients as to the thoroughness of their investigation)?
(2) Test result Interpretability
Ease of Do the two processes produce similar frequencies of clearly interpretable test results (or once
interpretation completed successfully, does one test tend to produce a higher frequency of indeterminate or
unreadable results than the other)?
Accuracy
Accuracy Do the tests correctly identify the target condition in the same number of patients (or does one
test correctly identify a higher proportion of patients with disease or without disease than the
other)?
Timing of results
Time to produce a Is the speed with which results are processed similar between tests (or does the new test have a
result shorter turnaround time between testing and production of results than the existing test)?
(3) Diagnostic Timing of diagnosis
decision Speed of diagnosis Do the strategies produce diagnoses in comparable timeframes (or do patients given one test
receive a diagnosis more quickly than patients given the other test)?
Diagnostic yield
Diagnoses made Do the tests contribute to patient diagnosis to similar degrees (or do the results of one test tend to
be given more weight than the other)?
Diagnostic confidence
Doctors confidence Is the degree of confidence that doctors have in the validity or applicability of a test result similar
in diagnosis to that of its comparator test (or does a new test provide greater reassurance to doctors, or are its
results considered less reliable by doctors)?
Patients confidence Is the degree of confidence that a patient has in the diagnostic process, or the diagnosis itself,
in diagnosis likely to vary between strategies (or does a new test provide greater or lesser reassurance to
patients, owing to doctors confidence, the testing experience, or understanding of test results)?
(4) Treatment Therapeutic yield
decision Treatment choices Do the comparative tests contribute to the formulation of a management plan to similar degrees
(or does one test lead to more patients receiving appropriate treatment than the other)?
Therapeutic confidence
Doctors confidence Do doctors have similar confidence in pursuing a treatment plan between intervention arms (or
in treatment choice does a test improve treatment success)?
Patients confidence Do patients have similar confidence in treatment plans based on diagnostic testing (or does the
in treatment choice new test improve patients understanding of the choice in management)?
(5) Treatment Timing of treatment
implementation Time to treatment Do the diagnostic strategies lead to patients receiving treatment within comparable timeframes
(or do patients given one test receive treatment earlier than those given the other test)?
Treatment efficacy
Efficacy of treatment Does use of the intervention in patients identified to have disease lead to improvements in
patient outcomes (or is the intervention ineffective)?
Adherence
Adherence to Are patients as likely to adhere to treatment plans regardless of the test strategy used (or does
treatment one strategy lead to more refusals or poorer compliance with treatment)?
angiography had a reduced risk of death, non-fatal cardiac However, quicker results are beneficial only if they produce
events, and readmission.16 Patients with ventilator associ- earlier diagnosis or treatment. The addition of polymerase
ated pneumonia allocated to a rapid antimicrobial suscep- chain reaction (PCR) to conventional analysis of nasopha-
tibility test received definitive results on average 2.8 days ryngeal swabs for distinguishing between viral and bacterial
earlier than those receiving the standard susceptibility test causes of lower respiratory tract infection failed to decrease
and experienced significantly fewer days of fever, bouts of time to treatment, because physicians were unwilling to base
diarrhoea, and days on mechanical ventilation.17 treatment decisions solely on PCR, preferring to wait for slower
20 BMJ | 10 MARCH 2012 | VOLUME 344
RESEARCH METHODS AND REPORTING
bacterial results.18 Earlier diagnosis can provide psychological might modify management to reassure and satisfy patients or
benefit by dispelling anxiety or providing earlier reassurance to prevent perceived threats of malpractice, often by request-
but can also cause psychological harm, particularly if effective ing additional diagnostic information.26 This defensive medi-
treatments are unavailable. The psychosocial impacts of an cine tends to raise the diagnostic threshold needed to trigger
earlier diagnosis have been highlighted in women following a change in management,27 and if additional tests are less
a positive cervical smear test19 or mammogram.20 accurate, harmful, or lead to treatment delays, patients will
be adversely affected.
Influencing patient and clinician perceptions
The patients perspective and the doctors personal perspec- Systemic approach to evaluating tests
tive can also influence decision making, sometimes in unex- These examples establish that diagnostic tests often affect
pected ways. These unpredictable responses can eliminate or patient health outcomes in many complex ways. Although test
enhance potential improvements gained from other aspects accuracy is commonly regarded as the main mechanism to
of the test-treatment pathway. influence clinical effectiveness,28 we caution against its use as
a surrogate for patient health. Only by looking at the test-treat-
Patients ment pathway as a whole can we identify which outcomes
Patients perceptions of testing, their experience of the test- need to be evaluated to fully capture a tests health effects.
ing process, and their understanding of the test result can all Sound evaluations of healthcare demand explanation of
affect downstream health. Many studies show social, emo- how the intervention will improve patient health.29 This is
tional, cognitive, and behavioural effects of testing across equally true of diagnostic tests, although they are consider-
various clinical conditions.21 ably more challenging to evaluate because so many interme-
Test-treatment pathways will be unsuccessful if patients diate, interacting factors are at stake. The need to identify
are unwilling to undergo a procedure. This is especially which of these factors will exert an effect and how, is a key
important if multiple testing is required; an unpleasant first tenet of complex intervention guidance.30 Table 2 provides a
test can adversely influence patients willingness to attend list of questions to guide the structured assessment of which
follow-up testing or treatment. The experience of undergoing processes are relevant and need to be measured within a given
tests can also influence illness beliefs. In a randomised trial, diagnostic comparison. This approach highlights precisely
women who were able to observe their diagnostic hysteros- where in a test-treatment pathway important differences
copy on a screen were reportedly less optimistic about the might originate, and will be useful for designing studies,
effectiveness of treatment offered, experienced more anxiety, appraising existing research, and determining what new
but were better able to deal with procedural discomfort than evidence is needed to formulate diagnostic guidelines (box).
women who could not see the screen.22 We identify three benefits from using this framework.
Diagnostic placebo effects might occur if the impression Firstly, it presents a structure for carefully developing a
of a thorough investigation improves perceptions of health rationale that underpins the performance of a putative test-
status. This could account for the significant improvements ing strategy. Secondly, it guides the identification of out-
in health utility that were reported by patients with acute comes for randomised controlled trials, and will also assist in
undifferentiated chest pain diagnosed in a specialist unit, constructing appropriate decision models, particularly when
compared with those diagnosed in emergency departments, trials are not practicable.32 Finally, the approach supports a
despite having equivalent treatment and rates of adverse car- full interpretation of empirical results by enabling trialists
diac events.23 to distinguish between true ineffectiveness, poor protocol
Receiving a diagnosis can have behavioural and health implementation, and methodological flaws in the study
consequencesfor example, by confirming patients negative design.33 These tasks are particularly important for trials
health beliefs. Patients with lower back pain reported higher of tests, where sample sizes often need to be several orders
pain scores and poorer health status after receiving an x ray of magnitude larger than they do in trials of treatments to
than those who received only a standard consultation.24 The detect differences in patient outcomes (fig 3).34 Findings of no
incidental diagnosis of non-pathological abnormalities may effect are all too often interpreted as evidence of absence,
have given patients a reason for their pain and encouraged when in reality studies rarely make provision for being able
illness behaviour despite the absence of an organic cause. to attribute negative results to the diagnostic intervention,
the study design, or (importantly) an inconsistently imple-
Adherence to treatment mented test-treatment strategy. By identifying all relevant
Patients experiences and perceptions of the test-treatment mechanisms, and measuring how they exert their effect,
pathway will also affect downstream health behaviours, test-treatment trials are more likely to contribute important
such as the willingness or motivation to adhere to medical evidence to the use of tests in clinical practice.
advice.25 Negative perceptions or experiences of testing and
clinical diagnosis could cause patients to lose confidence in Conclusion
the diagnosis or management plan, making them reluctant Establishing benefit to patient health must be the priority
to have subsequent testing or treatment. for diagnostic evaluations. Test accuracy is one component
of test evaluation, but does not capture the impact of tests
Doctors on patients. By considering the ways in which tests affect
Doctors emotional, cognitive, social, or behavioural perspec- patients health, we reiterate the complex intervention per-
tives, although external to objective medical concerns, are spective30 that it is not sufficient to measure outcomes, but
nevertheless important in decision making. Referring doctors rather it is essential to understand how these outputs are
BMJ | 10 MARCH 2012 | VOLUME 344 21
RESEARCH METHODS AND REPORTING
9 Ferrante di Ruffano L, Davenport C, Eisinga A, Hyde C, Deeks JJ. A
Randomised to test 1 Randomised to test 2 Comparison of randomised capture-recapture analysis demonstrated that randomized controlled
(patient numbers (patient numbers groups (patient numbers trials evaluating the impact of diagnostic tests on patient outcomes are
proportional to areas) proportional to areas) proportional to areas) rare. J Clin Epidemiol 2012;65:282-7.
Patients Patients Patients Patients Patients Patients 10 Bossuyt PMM, Lijmer JG. Traditional health outcomes in the evaluation of
with without with without with without diagnostic tests. Acad Radiol 1999;6:S77-80.
disease disease disease disease disease disease 11 Purushotham AD, Upponi S, Klevesath MB, Bobrow L, Millar K, Myles J, et al.
True False positive True False positive All All false Morbidity after sentinel lymph node biopsy in primary breast cancer: results
positive result positive result true positive results from a randomized controlled trial. J Clin Oncol 2005;23:4312-21.
result result positive B 12 Jeetley P, Burden L, Senior R. Stress echocardiography is superior to exercise
True negative results
True negative result All true ECG in the risk stratification of patients presenting with acute chest pain
result negative results
with negative Troponin. Eur J Echocardiogr 2006;7:155-64.
False A 13 Babjuk M, Soukup V, Petrk R, Jirsa M, Dvorcek J. 5-aminolaevulinic
False All false
negative negative negative acid-induced fluorescence cystoscopy during transurethral resection
result result results reduces the risk of recurrence in stage Ta/T1 bladder cancer. BJU Int
2005;96:798-802.
14 Viney RC, Boyer MJ, King MT, Kenny PM, Pollicino CA, Mclean JM, et al.
Fig 3| Sample size calculations for test-treatment randomised controlled trials. In randomised Randomized controlled trial of the role of positron emission tomography
trials of interventions, all participants in a study group are allocated to receive the same in the management of stage I and II non-small-cell lung cancer. J Clin Oncol
2004;22:2357-62.
intervention. In test-treatment trials, participants in each group receive a variety of interventions,
15 Kock MC, Adriaensen ME, Pattynama PM, van Sambeek MR, van Urk
depending on the test results and ensuing diagnosis. The magnitude of the observed treatment H, Stijnen T, et al. DSA versus multi-detector row CT angiography in
effect depends on the differences in proportions of patients who receive interventions peripheral arterial disease: randomized controlled trial. Radiology
appropriate to their condition in each group. This proportion would be expected to be quite 2005;237:727-37.
small. The figure identifies those participants who contribute statistical power in a randomised 16 Cannon CP, Weintraub WS, Demopoulos LA, Vicari R, Frey MJ, Lakkis N, et al.
Comparison of early invasive and conservative strategies in patients with
trial comparing two tests (where the difference in outcome originates entirely from a difference unstable coronary syndromes treated with the glycoprotein IIb/IIIa inhibitor
in diagnostic accuracy). Test 2 has higher sensitivity than test 1 (difference shown in A). Test 2 tirofiban. N Engl J Med 2001;344:1879-87.
also has higher specificity than test 1 (difference shown in B). Different widths of diseased and 17 Bouza E, Torres MV, Radice C, Cercenado E, de Diego R; Snchez-Carrillo
non-diseased columns indicate the prevalence of disease in the study sample. Only participants C, et al. Direct E-test (AB Biodisk) of respiratory samples improves
antimicrobial use in ventilator-associated pneumonia. Clin Infect Dis
in A and B would have different test results if they received test 2 rather than test 1 and therefore 2007;44:382-7.
the potential for different outcomes (all other participants in the study would have the same test 18 Oosterheert JJ, van Loon AM, Schuurman R, Hoepelman AI, Hak E, Thijsen S,
result, irrespective of which test they were allocated to). Statistical power therefore depends on et al. Impact of rapid detection of viral and atypical bacterial pathogens by
only the numbers of participants in A and B (particularly A); for example, if disease prevalence real-time polymerase chain reaction for patients with lower respiratory tract
infection. Clin Infect Dis 2005;41:1438-44.
was 20%, and test 2 improved sensitivity by 20%, only 4% of the total sample size would fall in A34 19 McCaffery KJ, Irwig L, Turner R, Chan SF, Macaskill P, Lewicka M, et al.
Psychosocial outcomes of three triage methods for the management
created, by conducting analyses of their workings and the of borderline abnormal cervical smears: an open randomised trial. BMJ
mechanisms that underpin them. Clearly, this process must 2010;340:b4491.
20 Barton MB, Morley DS, Moore S, Allen JD, Kleinman KP, Emmons KM et al.
be undertaken with expert and stakeholder consultation to Decreasing womens anxieties after abnormal mammograms: a controlled
ensure all influential mechanisms are identified. trial. J Natl Cancer Inst 2004;96:529-38.
Contributors: JJD conceived the idea for this project with support from CJH. 21 Bossuyt PMM, McCaffery K. Multiple pathways and additional patient
SUMMARY POINTS LFR did most of the primary research for the paper. The initial framework outcomes in evaluations of testing. Med Decis Making 2009;29:E30-8.
22 Ogden J, Heinrich M, Potter C, Kent A, Jones S. The impact of viewing a
The value of diagnostic was devised by LFR, CJH, and JJD, and further refined by all authors. All the
hysteroscopy on a screen on the patients experience: a randomised trial.
tests ultimately lies in their authors drafted, revised, and gave final approval to the article. JJD is the
BJOG 2009;116:286-93.
guarantor.
effect on patient outcomes 23 Goodacre SW, Nicholl J, Dixon S, Cross E, Angelini K, Arnold J, et al.
Funding: The development of the framework was funded partly by the UK Randomised controlled trial and economic evaluation of a chest pain
Tests can affect patient Medical Research Council Methodology Programme (grant G0600545, observation unit compared with routine care. BMJ 2004;328:254-60.
health by changing awarded to JJD), as part of a wider investigation into the use of randomised 24 Djais N, Kalim H. The role of lumbar spine radiography in the outcomes
diagnostic and treatment trials for evaluating the clinical effectiveness of diagnostic tests. The of patients with simple acute low back pain. APLAR J Rheumatol
decisions, affecting time funders had no involvement in the research project. JJD is partly supported 2005;8:45-50.
by the Medical Research Council Midland Hub for Trials Methodology 25 Haynes RB, Ackloo E, Sahota N, McDonald HP, Yao X. Interventions
to treatment, modifying
Research, University of Birmingham (grant G0800808). for enhancing medication adherence. Cochrane Database Syst Rev
patient perceptions and 2008;2:CD000011.
Competing interests: All authors have completed the ICJME unified
behaviour, or putting disclosure form at www.icmje.org/coi_disclosure.pdf and declare: the 26 Summerton, N. Positive and negative factors in defensive medicine: a
patients at risk of direct work was funded partly by the UK Medical Research Council Methodology
questionnaire study of general practitioners. BMJ 1995;310:27-9.
harm 27 Hauser MJ, Commons ML, Bursztajn HJ, Gutheil TG. Fear of malpractice
Programme; no financial relationships with any organisations that might
liability and its role in clinical decision making. In: Gutheil TG, Bursztajn HJ,
Improved accuracy is have an interest in the submitted work in the previous three years; and no Brodsky A, Alexander V, eds. Decision making in psychiatry and the law. 1st
not always a necessary other relationships or activities that could appear to have influenced the ed. Williams and Wilkins, 1991.
submitted work. 28 Hunink MGM, Krestin GP. Study design for concurrent development,
prerequisite for improving
Provenance and peer review: Not commissioned; externally peer reviewed. assessment, and implementation of new diagnostic imaging technology.
patient health, nor Radiology. 2002;222:604-14.
1 Bossuyt PM, Irwig L, Craig J, Glasziou P. Comparative accuracy: assessing
does it guarantee new tests against existing diagnostic pathways. BMJ 2006;332:1089-92. 29 Moher D, Hopewell S, Schultz KF, Montori V, Gtzsche PC, Devereaux PJ, et
other downstream 2 Leeflang MMG, Deeks JJ, Gatsonis C, Bossuyt PMM, on behalf of the al. CONSORT 2010 explanation and elaboration: updated guidelines for
improvements Cochrane Diagnostic Test Accuracy Working Group. Systematic reviews of reporting parallel group randomised trials. BMJ 2010;340:c869.
diagnostic test accuracy. Ann Intern Med 2008;149:889-97. 30 Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing
All elements of the 3 Fryback DG, Thornbury JR. The efficacy of diagnostic imaging. Med Decis and evaluating complex interventions: new guidance. Medical Research
management process Making 1991;11:88-94. Council, 2008.
(including decision 4 Lijmer JG, Bossuyt PMM. Various randomized designs can be used to 31 Pennant M, Takwoingi Y, Pennant L, Davenport C, Fry-Smith A, Eisinga A, et
making and treatment) evaluate medical tests. J Clin Epidemiol 2009;62:364-73. al. A systematic review of positron emission tomography (PET) and positron
5 Fineberg HV. Evaluation of computed tomography: achievement and emission tomography/computed tomography (PET/CT) for the diagnosis of
must be considered when challenge. Am J Roentgenol 1978;131:1-4. breast cancer recurrence. Health Technol Assess 2010;14:1-103.
evaluating a diagnostic test 6 Schnemann HJ, Oxman AD, Brozek J, Glasziou P, Jaeschke R, Vist GE, 32 Pletcher MJ, Pignone M. Evaluating the clinical utility of a biomarker:
Randomised controlled et al. Grading quality of evidence and strength of recommendations for a review of methods for estimating health impact. Circulation
diagnostic tests and strategies. BMJ 2008;336:1106-10. 2011;123:1116-24.
trials of tests can measure 7 Canadian Critical Care Trials Group. Randomized trial of diagnostic 33 Rychetnik L, Frommer M, Hawe P, Shiell A. Criteria for evaluating
these processes directly to techniques for ventilator-associated pneumonia. N Engl J Med evidence on public health interventions. J Epidemiol Community Health
understand why and how 2006;355:2619-30. 2002;56:119-27.
changes to patient health 8 Sutton AJ, Cooper NJ, Goodacre S, Stevenson M.Integration of meta- 34 Deeks JJ. Assessing outcomes following tests. In: Price CP, Christenson
analysis and economic decision modeling for evaluating diagnostic tests. EH, eds. Evidence-based laboratory medicine: principles, practice and
have occurred Med Decis Making 2008;28:650-67. outcomes. 2nd ed. AACC Press; 2007;95-111.
22 BMJ | 10 MARCH 2012 | VOLUME 344
You might also like
- Data and Analysis Considerations in Oncology Clinical TrialsDocument7 pagesData and Analysis Considerations in Oncology Clinical Trialsimk_mithunNo ratings yet
- Chapter 12 Systematic Review of Prognostic TestsDocument13 pagesChapter 12 Systematic Review of Prognostic TestsMuammar EmirNo ratings yet
- Diagnostic Evidence Cooperatives: Bridging The Valley of Death in Diagnostics DevelopmentDocument3 pagesDiagnostic Evidence Cooperatives: Bridging The Valley of Death in Diagnostics DevelopmentNadia AyuningtiasNo ratings yet
- TENS - ArticleDocument10 pagesTENS - ArticleMickael LopesNo ratings yet
- 1 - Outcomes ResearchDocument12 pages1 - Outcomes ResearchMauricio Ruiz MoralesNo ratings yet
- Analisis RCT Continuous Outcome - Google SearchDocument13 pagesAnalisis RCT Continuous Outcome - Google SearchRaudhatulAisyFachrudinNo ratings yet
- Best Practice & Research Clinical RheumatologyDocument13 pagesBest Practice & Research Clinical RheumatologydrharivadanNo ratings yet
- The Limitations of Observation StudiesDocument5 pagesThe Limitations of Observation StudiesalbgomezNo ratings yet
- Part 6Document4 pagesPart 6nguyendung0917No ratings yet
- NIH Public Access: Author ManuscriptDocument16 pagesNIH Public Access: Author ManuscriptMarvin BundoNo ratings yet
- Reviewing a Decision AnalysisDocument13 pagesReviewing a Decision AnalysisKevin Mora BañosNo ratings yet
- Improving Oncology Trials Through Adaptive Trial Design - ACT-Oncology-eBook-2016-MayDocument7 pagesImproving Oncology Trials Through Adaptive Trial Design - ACT-Oncology-eBook-2016-MayRaviprakash MadhyasthaNo ratings yet
- An extension of the CONSORT statementDocument8 pagesAn extension of the CONSORT statementgfguevaraNo ratings yet
- A Framework For Evaluating The Appropriateness of Clinical Decision Support Alerts and ResponsesDocument8 pagesA Framework For Evaluating The Appropriateness of Clinical Decision Support Alerts and ResponsesSocorro Moreno LunaNo ratings yet
- Stat & ResearchDocument276 pagesStat & ResearchSYED ALI HUSSAINNo ratings yet
- A Systematic Review of Studies Comparing Diagnostic Clinical Prediction Rules With Clinical JudgmentDocument25 pagesA Systematic Review of Studies Comparing Diagnostic Clinical Prediction Rules With Clinical JudgmentCambriaChicoNo ratings yet
- Malone - CH 5Document70 pagesMalone - CH 5kola belloNo ratings yet
- Why Clinical Trial Outcomes Fail To Translate Into Benefits For PatientsDocument7 pagesWhy Clinical Trial Outcomes Fail To Translate Into Benefits For PatientsLaura Larrea MantillaNo ratings yet
- (Surgery (Oxford) 2009-Sep Vol. 27 Iss. 9) - MCQs (2009) (10.1016 - J.mpsur.2009.08.016) - Libgen - LiDocument2 pages(Surgery (Oxford) 2009-Sep Vol. 27 Iss. 9) - MCQs (2009) (10.1016 - J.mpsur.2009.08.016) - Libgen - LiSaleh El BarasiNo ratings yet
- Clinical Trial DesignsDocument18 pagesClinical Trial DesignsVenkatesh Gavini100% (1)
- Murphy 2021Document11 pagesMurphy 2021okNo ratings yet
- Health Technology Assessment To Assess Value of Biomarkers in The Decision-Making ProcessDocument8 pagesHealth Technology Assessment To Assess Value of Biomarkers in The Decision-Making Processgeo4maryNo ratings yet
- Scaphoid Fracture: A Case ReportDocument5 pagesScaphoid Fracture: A Case Reportrapannika100% (2)
- 11.1 Diagnostic Tests 1-S2.0-S0001299818300941-MainDocument7 pages11.1 Diagnostic Tests 1-S2.0-S0001299818300941-MainHelioPassulequeNo ratings yet
- Use of Patient Preference Studies in HTA Decision Making: A NICE PerspectiveDocument5 pagesUse of Patient Preference Studies in HTA Decision Making: A NICE Perspectiveaxel pqNo ratings yet
- Procalcitonin-Guided Antibiotic Therapy in Intensive Care Unit Patients: A Systematic Review and Meta-AnalysisDocument10 pagesProcalcitonin-Guided Antibiotic Therapy in Intensive Care Unit Patients: A Systematic Review and Meta-AnalysisYesenia MBNo ratings yet
- Potential Pitfalls of Clinical Prediction RulesDocument3 pagesPotential Pitfalls of Clinical Prediction RulesMaximiliano LabraNo ratings yet
- Sexton 2011Document19 pagesSexton 2011koushikNo ratings yet
- Indirect Methods For Reference Interval Determination - Review and RecommendationsDocument10 pagesIndirect Methods For Reference Interval Determination - Review and RecommendationsDuy HoangNo ratings yet
- Treatment Based Subgroups LBP 2010Document11 pagesTreatment Based Subgroups LBP 2010Ju ChangNo ratings yet
- oncology-clinical-trialsDocument7 pagesoncology-clinical-trialsgskcl429No ratings yet
- Randomized Clinical TrialDocument5 pagesRandomized Clinical TrialEditor IJTSRDNo ratings yet
- Clinical Trials BookDocument11 pagesClinical Trials BookMaria SpatariNo ratings yet
- The Science of Clinical Practice - Disease Diagnosis or Patient Prognosis - Croft Et Al 2015Document8 pagesThe Science of Clinical Practice - Disease Diagnosis or Patient Prognosis - Croft Et Al 2015Bipul RajbhandariNo ratings yet
- Clinical Research MethodologyDocument11 pagesClinical Research MethodologymisganaNo ratings yet
- Tevis2018 Article Patient-ReportedOutcomesForBreDocument7 pagesTevis2018 Article Patient-ReportedOutcomesForBreGonzalo ZieglerNo ratings yet
- Review Bias in Clinical Intervention ResearchDocument9 pagesReview Bias in Clinical Intervention ResearchHesed VirtoNo ratings yet
- Un Poquito de Lectura 1607631682Document12 pagesUn Poquito de Lectura 1607631682franNo ratings yet
- Effect of CDSSDocument20 pagesEffect of CDSSMia Md. RaihanNo ratings yet
- Reglas de Predicción ClínicaDocument7 pagesReglas de Predicción ClínicaCambriaChicoNo ratings yet
- Clinical Trials and BiostatisticsDocument16 pagesClinical Trials and BiostatisticsArumugam RamasamyNo ratings yet
- Maas 2007Document11 pagesMaas 2007Caroline FelicianoNo ratings yet
- Approach To Developing GradingDocument8 pagesApproach To Developing GradingSalem RawashdahNo ratings yet
- Chapter 3 - Evidence-Based Endocrinology and Clinical EpidemiologyDocument32 pagesChapter 3 - Evidence-Based Endocrinology and Clinical Epidemiology張宏軒No ratings yet
- Patient-Reported Outcome Measures in Plastic Surgery An Introduction and Review of Clinical ApplicationsDocument6 pagesPatient-Reported Outcome Measures in Plastic Surgery An Introduction and Review of Clinical Applicationsdoctorshomare1No ratings yet
- Evidence Based Medicine in Neonatology: DefinitionDocument6 pagesEvidence Based Medicine in Neonatology: DefinitionAhmedAOmarNo ratings yet
- Muzii Et Al., 2020Document9 pagesMuzii Et Al., 2020Jonathan LucisNo ratings yet
- Diagnostic Infectious Diseases Testing Outside ClinicsDocument9 pagesDiagnostic Infectious Diseases Testing Outside ClinicsDiana PachónNo ratings yet
- CAP Treatamnet AcortadoDocument8 pagesCAP Treatamnet Acortadoapi-3707490No ratings yet
- MEDECIELO MELO - Chapter 8 SummaryDocument7 pagesMEDECIELO MELO - Chapter 8 SummaryMelo MedecieloNo ratings yet
- An To Patient-Reported Outcome Measures (Proms) in PhysiotherapyDocument7 pagesAn To Patient-Reported Outcome Measures (Proms) in PhysiotherapyAline VidalNo ratings yet
- 215 ArticleText 430 1 10 20170629Document6 pages215 ArticleText 430 1 10 20170629star warNo ratings yet
- Principles of The Patient-Centered Medical Home and Preventive Services DeliveryDocument9 pagesPrinciples of The Patient-Centered Medical Home and Preventive Services DeliverysudartoNo ratings yet
- Journal Club Presentation: Presented by Sunitha Elza Mathew Ra1422281010014 Pharmd InternDocument18 pagesJournal Club Presentation: Presented by Sunitha Elza Mathew Ra1422281010014 Pharmd InternManali DNo ratings yet
- Clinical Trial Design and Dissemination: Comprehensive Analysis of Clinicaltrials - Gov and Pubmed Data Since 2005Document11 pagesClinical Trial Design and Dissemination: Comprehensive Analysis of Clinicaltrials - Gov and Pubmed Data Since 2005Prateek Kumar PandaNo ratings yet
- Coleman 2021Document10 pagesColeman 2021Pratul TiwariNo ratings yet
- Basic Study Design Influences The Results of Orthodontiinvestigations PDFDocument11 pagesBasic Study Design Influences The Results of Orthodontiinvestigations PDFemadNo ratings yet
- Parkinson AccDocument13 pagesParkinson AccAlfiatur RizkiNo ratings yet
- The Use of Clinical Trials in Comparative Effectiv PDFDocument9 pagesThe Use of Clinical Trials in Comparative Effectiv PDFSilverio CasillasNo ratings yet
- Econometric Analysis of Health DataDocument231 pagesEconometric Analysis of Health DataMarisela FuentesNo ratings yet
- Climate and Climate ChangeDocument367 pagesClimate and Climate ChangeMarisela Fuentes100% (1)
- Four Myths of Data PresentationDocument3 pagesFour Myths of Data PresentationMarisela FuentesNo ratings yet
- GeodaworkbookDocument244 pagesGeodaworkbookjorocio02No ratings yet
- Images Presentation and Publication of Official Statistics Tcm97 27562Document27 pagesImages Presentation and Publication of Official Statistics Tcm97 27562Marisela FuentesNo ratings yet
- Spatial Epi BookDocument178 pagesSpatial Epi BookMarisela FuentesNo ratings yet
- Designing Persausive Tables and GraphsDocument2 pagesDesigning Persausive Tables and GraphsMarisela FuentesNo ratings yet
- Health Effects of Woodsmoke WA 2004 142269 7Document15 pagesHealth Effects of Woodsmoke WA 2004 142269 7Marisela FuentesNo ratings yet
- Oakes Neighbourhood Effects PDFDocument24 pagesOakes Neighbourhood Effects PDFMarisela FuentesNo ratings yet
- Young Duncan PT 2 PDFDocument218 pagesYoung Duncan PT 2 PDFMarisela FuentesNo ratings yet
- Guide to Identification and Distribution of Lutzomyia Sand Flies in the AmericasDocument231 pagesGuide to Identification and Distribution of Lutzomyia Sand Flies in the AmericasMarisela FuentesNo ratings yet
- GS+ User's GuideDocument179 pagesGS+ User's GuideIgnacio_Franci_7102No ratings yet
- 108-Epidemiological Studies - A Practical Guide, 2nd Edition-Alan J. Silman Gary J. Macfarlane-05 PDFDocument256 pages108-Epidemiological Studies - A Practical Guide, 2nd Edition-Alan J. Silman Gary J. Macfarlane-05 PDFMarisela Fuentes100% (1)
- Computing Ndvi in Arcgis Image AnalystDocument4 pagesComputing Ndvi in Arcgis Image AnalystMarisela FuentesNo ratings yet
- Introduction To Publishing For Ecr in Latam 256267Document52 pagesIntroduction To Publishing For Ecr in Latam 256267Marisela FuentesNo ratings yet
- Wiley-Blackwell House Style Guide 2007 PDFDocument60 pagesWiley-Blackwell House Style Guide 2007 PDFDEShifNo ratings yet
- Measure Instructions Leena For Women: Back WidthDocument4 pagesMeasure Instructions Leena For Women: Back WidthMarisela FuentesNo ratings yet
- Visual Analytics of Spatial Scan Statistic Results: Jxc93@psu - Edu Maceachren@psu - EduDocument4 pagesVisual Analytics of Spatial Scan Statistic Results: Jxc93@psu - Edu Maceachren@psu - Edujbsimha3629No ratings yet
- Predicting in Climate Changes ScenariesDocument10 pagesPredicting in Climate Changes ScenariesMarisela FuentesNo ratings yet
- Geostatistical Software PDFDocument10 pagesGeostatistical Software PDFMarisela FuentesNo ratings yet
- GIS DemographiC Health Surveys Data PDFDocument4 pagesGIS DemographiC Health Surveys Data PDFMarisela FuentesNo ratings yet
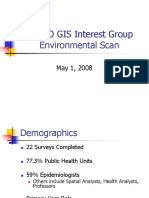
- APHEO GIS Interest Group Environmental ScanDocument16 pagesAPHEO GIS Interest Group Environmental ScanMarisela FuentesNo ratings yet
- Spatial Statistics and GISDocument43 pagesSpatial Statistics and GISMarisela FuentesNo ratings yet
- Aedes Albopictus Risk Maps: Development ofDocument52 pagesAedes Albopictus Risk Maps: Development ofMarisela FuentesNo ratings yet
- PisatiDensityestimationforspatialdata PDFDocument48 pagesPisatiDensityestimationforspatialdata PDFMarisela FuentesNo ratings yet
- Minamisava - Spatial Clustering of Violent DeathsDocument10 pagesMinamisava - Spatial Clustering of Violent DeathsMarisela FuentesNo ratings yet
- On Epidemiology and Geographic Information Systems - A Review and DiscussionDocument9 pagesOn Epidemiology and Geographic Information Systems - A Review and DiscussionMarisela FuentesNo ratings yet
- Leishmaniasis GISDocument27 pagesLeishmaniasis GISMarisela FuentesNo ratings yet
- Using A Quick-Basic Application Based On The Dac Statistic To Detect Spatial Clusters PDFDocument10 pagesUsing A Quick-Basic Application Based On The Dac Statistic To Detect Spatial Clusters PDFMarisela FuentesNo ratings yet
- The Emerging Role and Benefits of Boundary Analysis in Spatiotemporal Epidemiology and Public HealthDocument6 pagesThe Emerging Role and Benefits of Boundary Analysis in Spatiotemporal Epidemiology and Public HealthMarisela FuentesNo ratings yet
- Ice Berg Phenomenon of DiseaseDocument50 pagesIce Berg Phenomenon of DiseaseMan BoruahNo ratings yet
- Clinical Evidence Requirements According To The IVDocument8 pagesClinical Evidence Requirements According To The IVDr.Sivakumar SelvarajNo ratings yet
- Pract 2Document26 pagesPract 2ShalomAnithaNo ratings yet
- Ea F080 CH 4 X 20 ML Ea F245 CH 12 X 20 ML: in Vitro Diagnostic Medical DeviceDocument1 pageEa F080 CH 4 X 20 ML Ea F245 CH 12 X 20 ML: in Vitro Diagnostic Medical DeviceNguyễn ThơiNo ratings yet
- The GRE Issue EssayDocument5 pagesThe GRE Issue EssayAlizeh ANo ratings yet
- Essentials of Pediatric Nursing 2e Kyle TBDocument17 pagesEssentials of Pediatric Nursing 2e Kyle TBGene Mendoza100% (31)
- Concept of Disease CausationDocument44 pagesConcept of Disease CausationShivani Dhillon100% (2)
- UNIT 1 - PathophysiologyDocument8 pagesUNIT 1 - PathophysiologyEricBuguinaNo ratings yet
- Charisma Medical Software - Detailed DescriptionDocument57 pagesCharisma Medical Software - Detailed DescriptionTotal SoftNo ratings yet
- In Vitro Diagnostic Medical Devices - Evaluation of Stability of in Vitro Diagnostic Reagents (ISO 23640:2011)Document12 pagesIn Vitro Diagnostic Medical Devices - Evaluation of Stability of in Vitro Diagnostic Reagents (ISO 23640:2011)LenuinsaNo ratings yet
- TGS2 Estabilishing Stability of An in Vitro Diagnostic For WHO PrequalificationDocument55 pagesTGS2 Estabilishing Stability of An in Vitro Diagnostic For WHO Prequalificationmohammad reza mirzababaeeNo ratings yet
- FULL Download Ebook PDF Laboratory and Diagnostic Tests With Nursing Implications 10th Edition 2 PDF EbookDocument41 pagesFULL Download Ebook PDF Laboratory and Diagnostic Tests With Nursing Implications 10th Edition 2 PDF Ebookjennifer.liotta529100% (28)
- Diagnostic Test: DR Sajeena SDocument32 pagesDiagnostic Test: DR Sajeena SSajeena Rabees0% (1)
- Journal Homepage: - : IntroductionDocument6 pagesJournal Homepage: - : IntroductionIJAR JOURNALNo ratings yet
- Virginia PCRDocument3 pagesVirginia PCRdandude505No ratings yet
- Clinical Aspect of Exercise PhysiologyDocument34 pagesClinical Aspect of Exercise PhysiologyAnn LoricaNo ratings yet
- Piis0190962223001639 PDFDocument8 pagesPiis0190962223001639 PDFLighthopeNo ratings yet
- BMR 2111 Pathology For RadiographersDocument2 pagesBMR 2111 Pathology For RadiographersQanita RehmanNo ratings yet
- IQIPS Standards and Criteria for Audiology ServicesDocument30 pagesIQIPS Standards and Criteria for Audiology ServicesTharshiniNo ratings yet
- User Requirements Example OCt 23Document13 pagesUser Requirements Example OCt 23mohamedkhaterNo ratings yet
- BS-240 New Service Manual V2.0 enDocument378 pagesBS-240 New Service Manual V2.0 enAji Abdulah100% (2)
- Appropriateness For Ldts Companion DX Assays: Perspectives On To Be Used AsDocument16 pagesAppropriateness For Ldts Companion DX Assays: Perspectives On To Be Used AsfdablogNo ratings yet
- Best Practices and Current Implementation of Emerging SM - 2023 - TrAC Trends inDocument17 pagesBest Practices and Current Implementation of Emerging SM - 2023 - TrAC Trends infeNo ratings yet
- Diagnostic Test: Person Diagnostic Auto Correct: Oracle Fusion Human Capital ManagementDocument10 pagesDiagnostic Test: Person Diagnostic Auto Correct: Oracle Fusion Human Capital Managementtonismarg2014No ratings yet
- Pathology Report Molecular Department ResultsDocument1 pagePathology Report Molecular Department ResultsAnoy ChowdhuryNo ratings yet
- CAP Lab General Checklist 2017Document144 pagesCAP Lab General Checklist 2017Fee KuNo ratings yet
- BS-230 - New Service Manual - V2.0 - ENDocument338 pagesBS-230 - New Service Manual - V2.0 - ENJose Villamizar gomez79% (19)
- Diagnosing Neonatal EncephalopatyDocument11 pagesDiagnosing Neonatal EncephalopatyLalo LanNo ratings yet
- Evaluating Diagnostics: A Guide For Diagnostic EvaluationsDocument5 pagesEvaluating Diagnostics: A Guide For Diagnostic EvaluationsYanneLewerissaNo ratings yet
- Wesgardrules & MultirulesDocument18 pagesWesgardrules & MultirulesElvan Dwi WidyadiNo ratings yet