Professional Documents
Culture Documents
2879 Full
Uploaded by
hendranuraminOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
2879 Full
Uploaded by
hendranuraminCopyright:
Available Formats
C O M M E N T A R Y ( S E E A C C O M P A N Y I N G A R T I C L E S , P P .
2 8 7 7 A N D 3 0 4 0 )
Diagnosing Gestational Diabetes
Mellitus: Rationed or Rationally
Related to Risk?
T
he much-anticipated, weather-plagued data collected by OSullivan and Mahan with the OGTT. These missed cases of
National Institutes of Health (NIH) (4) from 1956 to 1957 and published in GDM will result in adverse events, and
Consensus Development Confer- 1964, relating to the risk of developing the real burden and cost of these will
ence on Diagnosing Gestational Diabetes diabetes following pregnancy. The his- need to be factored and compared with
Mellitus, held in Bethesda, Maryland, 46 tory of their evolution since that time any hypothetical advantage of a two-stage
March 2013, led to publication of a con- has been summarized by Naylor (5) and procedure. Further, a recent Canadian au-
sensus panel report (1) that essentially more recently updated by Coustan (6). To dit (10) noted that only 36% of pregnant
maintains and promotes the status quo the dispassionate observer, it seems sur- women with dysglycemia on initial testing
regarding gestational diabetes mellitus prising that these criteria still predominate proceeded to the recommended follow-up
(GDM) diagnosis. The panel report con- and are favored by the NIH panel. This may 75-g OGTT. Two-step testing, promoted
tradicts current American Diabetes Asso- represent a form of clinical inertia (7). Sim- by the NIH panel to limit false positives,
ciation (ADA) recommendations (2). This ply stated, it is easier to continue an estab- clearly delays GDM diagnosis, misses
commentary addresses several areas of lished (arbitrary) pattern of practice than to 25% of GDM cases even with optimal
disagreement. embrace change. Further, the outdated follow-up, and gives the opportunity for
The only constant is change, and this and methodologically incorrect National multiple process errors.
is most apparent with the demography of Diabetes Data Group (NDDG) criteria are Another highly contestable, but com-
pregnancy. Perhaps the most disturbing still used in preference to the Carpenter- fortable, aspect of current practice has
omission from the NIH panels report (1) Coustan (CC) criteria (6) in many sites. been the requirement for $2 OGTT values
is the lack of clear acknowledgment of the One can speculate that this may be due to above threshold for the diagnosis of GDM.
importance of the increasing prevalence their higher diagnostic thresholds, which Anecdotal explanations of this practice (not
of prediabetes and undiagnosed type 2 conveniently lower the frequency of GDM used in other denitions of diabetes) refer
diabetes, outside pregnancy, in women diagnoses. Astoundingly, despite their con- to the poor reproducibility of 1950s whole
of childbearing age (2). This omission ef- voluted history, the CC criteria for GDM blood glucose assays (5) and concerns, ech-
fectively precludes any strategy for early diagnosis are numerically extremely close oed by the NIH panel, about labeling
detection of these potentially serious to those derived from associations with di- women as having diabetes on the basis
problems in pregnancy. Much of the NIH abetic fetopathy, recommended by the In- of a single test. At least 10 studies (11
report expresses grave concerns about the ternational Association of the Diabetes and 20) have compared women with one ab-
possibility of a two- to threefold increase in Pregnancy Study Groups (IADPSG) (8) and normal value (OAV) on the OGTT with
GDM prevalence from the current estimate endorsed by the ADA (2). those diagnosed as GDM and/or those con-
of 56%. However, the National Health and Should testing for GDM be a one-step sidered normal. All have concluded that
Nutrition Examination Survey (NHANES) or two-step procedure? The original studies OAV women risk increased pregnancy
20052008 data (3) regarding U.S. women of OSullivan involved uniform one-step complications, principally fetal overgrowth
aged 1844 years report frank diabetes in administration of a 100-g oral glucose tol- and hypertensive disorders of pregnancy.
4.5% of participants (1.7% undiagnosed) erance test (OGTT) (4,5), and diagnostic The one randomized controlled trial
and prediabetes in 26.4%. While the cur- cutoffs were derived from such data. Pro- (RCT) in this group of women (21) reported
rent ADA (2) criteria for the diagnosis of tocols for simplied testing were developed improved outcomes with active treatment.
GDM are based primarily on considera- later and generally involved a nonfasting Insisting on two abnormal OGTT values for
tions of fetopathy, they still have an impor- glucose challenge test (GCT). At some un- the diagnosis of GDM limits GDM diagno-
tant role in identifying women with current certain point in the evolution of GDM di- ses, principally by excluding OAV women
or future abnormalities of glucose metabo- agnosis, the idea of the GCT as a screening who are at similar risk of adverse outcomes.
lism. Given the NHANES prevalence esti- test for low-risk women followed by a di- This appears irrational in the face of such
mates for impaired glucose metabolism of agnostic OGTT appears to have metamor- consistent contrary evidence.
;30% in women of childbearing age and phosed into a two-step approach. The NIH The NIH consensus panel identies
the general acknowledgment that glu- panel argues that two-step testing is less as a priority the conduct of a new RCT
cose tolerance worsens and that glucose burdensome for women but provides no evaluating outcomes in women currently
control is more important during preg- data or evidence for this. By the panels classied as normal according to preva-
nancy, it seems bafing that the NIH panel own summation, two-step testing involves lent U.S. criteria, but who would be con-
(1) wishes to ration GDM prevalence to an additional laboratory visit and collection sidered abnormal by the IADPSG (8) and
56% of pregnant women. of four additional blood draws for up to ADA (2). They wish such a trial to address
Currently, the most commonly used 23% of women. A recent systematic review clinically important health and patient-
criteria for GDM in the U.S. and in other (9) concluded that a two-step strategy centered outcomes, without providing any
parts of the world are derived from the misses ;25% of GDM cases diagnosed denitions of these terms. They implicitly
care.diabetesjournals.org DIABETES CARE, VOLUME 36, OCTOBER 2013 2879
Commentary
criticize previous high-quality RCTs by Available from http://prevention.nih.gov/ 14. Schfer-Graf UM, Dupak J, Vogel M, et al.
Crowther et al. (22) and Landon et al. cdp/conferences/2013/gdm/resources.aspx. Hyperinsulinism, neonatal obesity and
(23), for including highly motivated in- Accessed 24 May 2013 placental immaturity in infants born to
dividuals and being conducted in aca- 2. American Diabetes Association. Standards women with one abnormal glucose toler-
of medical care in diabetes2013. Diabe- ance test value. J Perinat Med 1998;26:
demic medical centers. Presumably their
tes Care 2013;36(Suppl. 1):S11S66 2736
ideal trial would involve unmotivated par- 3. Metzger BE, Gabbe SG, Persson B, et al.; 15. Gruendhammer M, Brezinka C, Lechleitner
ticipants and untrained, inexperienced International Association of Diabetes & M. The number of abnormal plasma glu-
investigators. Given the known graded Pregnancy Study Groups (IADPSG) Con- cose values in the oral glucose tolerance test
relationship between maternal glycemia sensus Panel Writing Group and the Hyper- and the feto-maternal outcome of preg-
and pregnancy outcomes and the fact that glycemia & Adverse Pregnancy Outcome nancy. Eur J Obstet Gynecol Reprod Biol
the two RCTs took 10 (22) and 6 (23) years (HAPO) Study Steering Committee. The 2003;108:131136
to conduct, these proposals appear little diagnosis of gestational diabetes mellitus: 16. Di Cianni G, Seghieri G, Lencioni C, et al.
more than procrastination dressed up as new paradigms or status quo? J Matern Normal glucose tolerance and gestational
science. Fetal Neonatal Med 2012;25:25642569 diabetes mellitus: what is in between? Di-
4. OSullivan JB, Mahan CM. Criteria for the abetes Care 2007;30:17831788
No diagnostic process or set of OGTT
oral glucose tolerance test in pregnancy. 17. Lapolla A, Dalfr MG, Bonomo M, et al.
criteria will ever be able to perfectly identify Diabetes 1964;13:278285 Can plasma glucose and HbA1c predict
all women at risk for adverse pregnancy 5. Naylor CD. Diagnosing gestational diabetes fetal growth in mothers with different glu-
outcomes. However, synthesis of avail- mellitus. Is the gold standard valid? Diabe- cose tolerance levels? Diabetes Res Clin
able epidemiologic and clinical trial data tes Care 1989;12:565572 Pract 2007;77:465470
suggests that the IADPSG- and ADA- 6. Coustan DR. Clinical Chemistry Review: 18. Biri A, Korucuoglu U, Ozcan P, Aksakal N,
recommended criteria (refs. 8 and 2, re- gestational diabetes mellitus. Clin Chem. Turan O, Himmetoglu O. Effect of different
spectively) represent a reasonable and 27 March 2013 [Epub ahead of print] degrees of glucose intolerance on maternal
responsible approach to identifying women 7. Phillips LS, Branch WT, Cook CB, et al. and perinatal outcomes. J Matern Fetal
with hyperglycemia in pregnancy who are Clinical inertia. Ann Intern Med 2001;135: Neonatal Med 2009;22:473478
825834 19. Landon MB, Mele L, Spong CY, et al.;
likely to benet from treatment.
8. Metzger BE, Gabbe SG, Persson B, et al.; Eunice Kennedy Shriver National Institute
International Association of Diabetes and of Child Health and Human Development
HAROLD DAVID MCINTYRE, MD Pregnancy Study Groups Consensus Panel. (NICHD) MaternalFetal Medicine Units
International Association of Diabetes and (MFMU) Network. The relationship be-
From the Mater Clinical School, University of Pregnancy Study Groups recommenda- tween maternal glycemia and perinatal out-
Queensland and Mater Health Services, South tions on the diagnosis and classication come. Obstet Gynecol 2011;117:218224
Brisbane, Queensland, Australia. of hyperglycemia in pregnancy. Diabetes 20. Cok T, Tarim E, Bagis T. Isolated abnor-
Corresponding author: Harold David McIntyre, Care 2010;33:676682 mal value during the 3-hour glucose tol-
david.mcintyre@mater.org.au. 9. van Leeuwen M, Louwerse MD, Opmeer erance test: which value is associated with
DOI: 10.2337/dc13-1250 BC, et al. Glucose challenge test for detect- macrosomia? J Matern Fetal Neonatal Med
2013 by the American Diabetes Association. ing gestational diabetes mellitus: a system- 2011;24:10391041
Readers may use this article as long as the work is atic review. BJOG 2012;119:393401 21. Langer O, Anyaegbunam A, Brustman L,
properly cited, the use is educational and not for
prot, and the work is not altered. See http://
10. Sievenpiper JL, McDonald SD, Grey V, Divon M. Management of women with one
creativecommons.org/licenses/by-nc-nd/3.0/ for Don-Wauchope AC. Missed follow-up op- abnormal oral glucose tolerance test value
details. portunities using a two-step screening ap- reduces adverse outcome in pregnancy.
proach for gestational diabetes. Diabetes Am J Obstet Gynecol 1989;161:593599
Res Clin Pract 2012;96:e43e46 22. Crowther CA, Hiller JE, Moss JR, McPhee
AcknowledgmentsH.D.M. is currently 11. Langer O, Brustman L, Anyaegbunam A, AJ, Jeffries WS, Robinson JS; Australian
chair of the IADPSG and was a principal Mazze R. The signicance of one abnormal Carbohydrate Intolerance Study in Preg-
investigator on the Hyperglycemia and Ad- glucose tolerance test value on adverse out- nant Women (ACHOIS) Trial Group. Ef-
verse Pregnancy Outcome Study. come in pregnancy. Am J Obstet Gynecol fect of treatment of gestational diabetes
No potential conicts of interest relevant to 1987;157:758763 mellitus on pregnancy outcomes. N Engl
this article were reported. 12. Berkus MD, Langer O, Piper JM, Luther J Med 2005;352:24772486
MF. Efciency of lower threshold criteria 23. Landon MB, Spong CY, Thom E, et al.;
c c c c c c c c c c c c c c c c c c c c c c c c for the diagnosis of gestational diabetes. Eunice Kennedy Shriver National Institute
References Obstet Gynecol 1995;86:892896 of Child Health and Human Development
1. National Institutes of Health. National In- 13. Lindsay MK, Graves W, Klein L. The rela- Maternal-Fetal Medicine Units Network.
stitutes of Health Consensus Development tionship of one abnormal glucose tolerance A multicenter, randomized trial of treat-
Conference on Diagnosing Gestational Di- test value and pregnancy complications. ment for mild gestational diabetes. N Engl
abetes Mellitus: Final Statement, 2013. Obstet Gynecol 1989;73:103106 J Med 2009;361:13391348
2880 DIABETES CARE, VOLUME 36, OCTOBER 2013 care.diabetesjournals.org
You might also like
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- List of Must-BringsDocument1 pageList of Must-BringshendranuraminNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Boehringer Ingelheim Page 2 of 14 Trajenta Linagliptin, 5 MG Film Coated Tablet Response DocumentDocument1 pageBoehringer Ingelheim Page 2 of 14 Trajenta Linagliptin, 5 MG Film Coated Tablet Response DocumentHendra Wana Nur'aminNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Ukmppd 2016Document8 pagesUkmppd 2016hendranuraminNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Boehringer Ingelheim Page 14 of 14 Trajenta Linagliptin, 5 MG Film Coated Tablet Response DocumentDocument1 pageBoehringer Ingelheim Page 14 of 14 Trajenta Linagliptin, 5 MG Film Coated Tablet Response DocumenthendranuraminNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
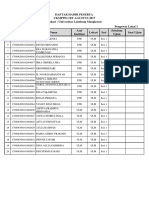
- Daftar Hadir Peserta Ukmppd CBT Agustus 2017 Lokasi: Universitas Lambung Mangkurat Pengawas Lokal 1Document2 pagesDaftar Hadir Peserta Ukmppd CBT Agustus 2017 Lokasi: Universitas Lambung Mangkurat Pengawas Lokal 1hendranuraminNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- KKD 2 GradesDocument2 pagesKKD 2 GradeshendranuraminNo ratings yet
- KelompokDocument5 pagesKelompokhendranuraminNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Itinerary BrisbaneDocument2 pagesItinerary BrisbanehendranuraminNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- BSM Latihan Soal (Shuffle) GradesDocument3 pagesBSM Latihan Soal (Shuffle) GradeshendranuraminNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Imatinib For Philadelphia Chromosome Positive CML, First LineDocument4 pagesImatinib For Philadelphia Chromosome Positive CML, First LinehendranuraminNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- Adjuvant PeDocument1 pageAdjuvant PeAlexandru IacobanNo ratings yet
- 161Document6 pages161hendranuraminNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- FTPDocument8 pagesFTPhendranuraminNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Airbnb Travel Itinerary, Confirmation Code HM2YZQFRYXDocument1 pageAirbnb Travel Itinerary, Confirmation Code HM2YZQFRYXhendranuraminNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- B121 6-EnDocument4 pagesB121 6-EnhendranuraminNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- WHO HSE GAR DCE 2010.2 EngDocument6 pagesWHO HSE GAR DCE 2010.2 Engangelabety88No ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- KKD 2 GradesDocument2 pagesKKD 2 GradeshendranuraminNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Effects Urn NBN Si Web YeezxdodDocument9 pagesEffects Urn NBN Si Web YeezxdodhendranuraminNo ratings yet
- 1toxicology 2Document56 pages1toxicology 2Luci PaunescuNo ratings yet
- List of Must-BringsDocument1 pageList of Must-BringshendranuraminNo ratings yet
- Gout 1Document51 pagesGout 1hendranuraminNo ratings yet
- Student Tox LectureDocument49 pagesStudent Tox LecturehendranuraminNo ratings yet
- ReceiptDocument1 pageReceipthendranuraminNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Your Electronic Ticket ReceiptDocument2 pagesYour Electronic Ticket ReceipthendranuraminNo ratings yet
- Dose Conversion Table For Statins:: (Mevacor ) (Pravachol ) (ZOCOR )Document1 pageDose Conversion Table For Statins:: (Mevacor ) (Pravachol ) (ZOCOR )hendranuraminNo ratings yet
- Effects - URN NBN SI WEB YEEZXDOD PDFDocument9 pagesEffects - URN NBN SI WEB YEEZXDOD PDFhendranuraminNo ratings yet
- Hendra WN, Hanoi-Jkt 27 Feb 2017 PDFDocument2 pagesHendra WN, Hanoi-Jkt 27 Feb 2017 PDFhendranuraminNo ratings yet
- m06807 SynopsisDocument6 pagesm06807 SynopsishendranuraminNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Japan Itinerary Travel ScheduleDocument1 pageJapan Itinerary Travel SchedulehendranuraminNo ratings yet
- ABpsych NewpppDocument15 pagesABpsych NewpppMarbie Aliyah B. PagadorNo ratings yet
- Multiple Births Carrying Multiples:-Triplets, Quadruplets, Quintuplets, SextupletsDocument5 pagesMultiple Births Carrying Multiples:-Triplets, Quadruplets, Quintuplets, SextupletsSheryll Almira HilarioNo ratings yet
- Baby SensesDocument2 pagesBaby SensesCamille LiqueNo ratings yet
- Nice Neotech - Accessories - 20Document1 pageNice Neotech - Accessories - 20David Gnana DuraiNo ratings yet
- Nephritic SyndromeDocument19 pagesNephritic SyndromesangheetaNo ratings yet
- Roleplay Procedure Nasogastric Incubation (NGT)Document3 pagesRoleplay Procedure Nasogastric Incubation (NGT)naimathur rodiyahNo ratings yet
- 11.efficacy and Stability of The Alar Base Cinch SutureDocument4 pages11.efficacy and Stability of The Alar Base Cinch SutureFabian Camelo OtorrinoNo ratings yet
- WEEK 1 Lecture - Introduction - Student'sDocument54 pagesWEEK 1 Lecture - Introduction - Student'smike angelo albacieteNo ratings yet
- Als CapstoneDocument9 pagesAls Capstoneapi-514758382No ratings yet
- E383 Full PDFDocument11 pagesE383 Full PDFBarryNo ratings yet
- Listening d1Document4 pagesListening d1Ebin PauloseNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Introduction to ImmunohematologyDocument16 pagesIntroduction to ImmunohematologyJoshua TrinidadNo ratings yet
- RENBUT BHN LAB 2022 SD Agt 2023Document3 pagesRENBUT BHN LAB 2022 SD Agt 2023ajisNo ratings yet
- Scientists transform spinach leaf into beating human heart tissueDocument4 pagesScientists transform spinach leaf into beating human heart tissueSkye M. PetersNo ratings yet
- RSP20110601Document64 pagesRSP20110601Abhinav SinghalNo ratings yet
- Act 1. PhobiasDocument2 pagesAct 1. PhobiasRoxanne CastilloNo ratings yet
- Comparative-Study-Of-Four-Methods-Of-Clinical-Estimation-Of-Fetal-Weight 2Document9 pagesComparative-Study-Of-Four-Methods-Of-Clinical-Estimation-Of-Fetal-Weight 2Abegail Fermanejo-GeneraoNo ratings yet
- Ultimate Final CoachingDocument79 pagesUltimate Final CoachingCarlo Montejo100% (1)
- Role of CPAP in ICUDocument21 pagesRole of CPAP in ICUheriNo ratings yet
- Essential Intrapartum and Newborn Care (EINC) Bulletin 1Document10 pagesEssential Intrapartum and Newborn Care (EINC) Bulletin 1maxicap7386% (7)
- Differences Between T.solium and T.saginata: Taeniasis or CysticercosisDocument3 pagesDifferences Between T.solium and T.saginata: Taeniasis or CysticercosisVenkatapradeepNo ratings yet
- Private Practice and Public School Speech Therapy Options in AustinDocument2 pagesPrivate Practice and Public School Speech Therapy Options in Austiniese027No ratings yet
- Ncp-Ineffective Breathing PatternDocument4 pagesNcp-Ineffective Breathing PatternRoxanne Ganayo Claver100% (1)
- Procedures in Obstetrics and Gynaecology TextbookDocument272 pagesProcedures in Obstetrics and Gynaecology TextbookPriyaNo ratings yet
- GERD Nursing CareDocument9 pagesGERD Nursing CareTrisha ArizalaNo ratings yet
- Intubasi Sulit: Nur Hajriya BrahmiDocument26 pagesIntubasi Sulit: Nur Hajriya BrahmiFathiah HusainNo ratings yet
- Fetal Assessment DRDocument1 pageFetal Assessment DRMicah Lou CalambaNo ratings yet
- Fever and Rash: Dr. Karwan Hawez Sulaiman MBCHB, Ficms, FM Family Medicine Specialist College of MedicineDocument20 pagesFever and Rash: Dr. Karwan Hawez Sulaiman MBCHB, Ficms, FM Family Medicine Specialist College of MedicinesamiNo ratings yet
- Clinical Profile of Indian Children With Down SyndromeDocument5 pagesClinical Profile of Indian Children With Down SyndromeRicky Wahyu setiawanNo ratings yet
- Susan Mathews Case NotesDocument2 pagesSusan Mathews Case NotesHarshit Aggarwal80% (5)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (402)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (13)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 3.5 out of 5 stars3.5/5 (2)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (78)