Professional Documents
Culture Documents
Pediatric Skull Fractures
Uploaded by
ifanda80Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pediatric Skull Fractures
Uploaded by
ifanda80Copyright:
Available Formats
See the corresponding editorial in this issue, pp 203204.
J Neurosurg Pediatrics 14:205211, 2014
AANS, 2014
Pediatric skull fractures: the need for surgical intervention,
characteristics, complications, and outcomes
Clinical article
Christopher M. Bonfield, M.D.,1 Sanjay Naran, M.D., 2 Oluwaseun A. Adetayo, M.D., 2
Ian F. Pollack, M.D.,1 and Joseph E. Losee, M.D. 2
Departments of 1Neurological Surgery and 2Plastic Surgery, University of Pittsburgh, Pennsylvania
Object. Head trauma is a common cause of morbidity and mortality in the pediatric population and often results
in a skull fracture. Pediatric skull fractures are distinct from adult fractures. Pediatric fractures have a greater capac-
ity to remodel, but the pediatric brain and craniofacial skeleton are still developing. Although pediatric head trauma
has been extensively studied, there is sparse literature regarding skull fractures. The authors aim was to investigate
the characteristics, injuries, complications, and outcomes of the patients in whom surgical intervention was needed
for skull fractures.
Methods. The authors performed a retrospective review of patients presenting to the emergency department of
a pediatric Level I trauma center between 2000 and 2005 with skull fractures. Patient demographics, mechanism of
injury, associated injuries, fracture bone involvement, surgical intervention, complications, and outcomes were ana-
lyzed. Groups treated nonoperatively, for skull fracture repair, and for traumatic brain injury were compared.
Results. A total of 897 patients with a skull fracture were analyzed. Most patients (n = 772, 86.1%) were treated
nonoperatively (Non-Op group). Fifty-eight patients (6.5%) underwent repair of the fracture (Repair group) and 67
(7.5%) required intervention for treatment of traumatic brain injury (TBI group). The Non-Op group was significantly
younger, and the TBI group had a lower initial Glasgow Coma Scale (GCS) score. A fall (51.2%) was the most com-
mon mechanism of injury in the Non-Op group, whereas a motor vehicle crash (23.9%) and being hit in the head with
an object (48.2%) were most prevalent in the TBI and Repair groups, respectively. Associated injuries were seen in
all 3 groups, with brain injury (hematoma) being the most common. Frontal bone fracture was seen most in the Repair
and TBI groups, and the parietal bone was the most frequent bone fractured in the Non-Op group. Patients in the TBI
group were much more likely to have 2 or 3 skull bones fractured. In the Repair group, 36.2% had a complication
(38.0% intervention related and 62.0% trauma related), but no patient had a worsening of their neurological status.
In the TBI group, 48.7% of the patients suffered a complication, the vast majority (90.6%) of which were related to
the trauma.
Conclusions. The majority of pediatric skull fractures can be managed conservatively. Of those requiring surgi-
cal intervention, fewer than half of the surgeries are performed solely for skull fracture repair only. Patients hit in the
head with an object or involved in a motor vehicle crash are more likely to need surgical intervention either to repair
the skull fracture or for TBI management, respectively. Frontal bone fractures are more likely to necessitate repair,
and those patients treated for TBI have a greater incidence of 2 or 3 bones involved in the fracture. Complications
occurred but most were related to underlying trauma, not the surgery. No patients who underwent intervention for
repair of their skull fracture only had a worsening of their neurological status.
(http://thejns.org/doi/abs/10.3171/2014.5.PEDS13414)
Key Words pediatric skull fracture head injury trauma
surgical intervention
H
ead trauma is common in the pediatric population of 250 per 100,000 per year. It accounts for over 7000
and is an important cause of morbidity and mortal- deaths, 60,000 hospitalizations, and 600,000 emergency
ity in the United States, with an estimated incidence department visits annually among American children.8,12 In
children, between 10%30% of head injuries result in skull
Abbreviations used in this paper: EVD = external ventricular fracture,7,9 many with associated brain injury.2,13 Surgical
drain; GCS = Glasgow Coma Scale; ICU = intensive care unit; LOS intervention is largely performed in cases of skull fracture
= length of stay; MVC = motor vehicle crash; TBI = traumatic brain depression, frontal sinus involvement, and underlying mass
injury. lesion. In certain instances, especially in infants, conserva-
J Neurosurg: Pediatrics / Volume 14 / August 2014 205
C. M. Bonfield et al.
tive management has been advocated as treatment.5,15 Pedi- derwent repair of the fracture (Repair group) for fracture
atric skull fractures remain distinct from their adult coun- elevation, frontal sinus repair, open fracture debridement,
terparts. Pediatric skull fractures have a greater capacity to or cosmetic repair. Sixty-seven patients (7.5%) required
heal and remodel, but the pediatric brain and craniofacial intervention for treatment of a TBI (TBI group) including
skeleton are also still developing, which puts the children hematoma evacuation, EVD placement, or decompressive
at risk for unique complications, such as growing skull craniectomy.
fractures. Although pediatric head trauma has been ex- Patient demographics are listed in Table 1. In all
tensively studied, there is sparse literature regarding skull 3 groups, the majority of patients were male (63.5% in
fractures, the rate of operative management, and outcomes the Non-Op, 69.0% in the Repair, and 65.7% in the TBI
following surgical intervention in this population. Our goal group) and Caucasian (Non-Op 82.3%, Repair 81.0%,
was to investigate the characteristics, injuries, indications and TBI 85.1%). The mean age at the time of evaluation
for intervention, and outcomes of the pediatric patients in was significantly younger in the Non-Op group (5.5 5.0
whom surgical intervention was needed for cranial vault years, p < 0.001) compared with the Repair (8.5 4.8
skull fractures. years) and TBI (8.6 5.2) groups.
Hospital Stay Data
Methods
Hospital stay data are also reported in Table 2. The
The study was approved by the Institutional Review initial GCS score was significantly lower in the TBI
Board at the University of Pittsburgh. A database of all group (6.80 4.5, p < 0.001) in relation to the Non-Op
patients diagnosed with a skull fracture at the Childrens (13.6 3.4) and Repair (12.4 4.6) groups. In the TBI
Hospital of Pittsburgh from 2000 to 2005 was searched. group, 63 patients (94.0%) were admitted to the intensive
All patients diagnosed with a skull fracture were includ- care unit (ICU) and 42 patients (62.7%) were intubated.
ed regardless of treating specialty, treatment modality, In the Repair group, 24 patients (41.4%) were admitted
or need for hospital admission. Patient demographics, to the ICU and 12 patients (20.7%) were intubated. The
mechanism of injury, associated injuries, fracture bone Non-Op group had the lowest rates of ICU admissions
involvement, surgical intervention, complications, and (19.4%) and intubations (10.0%). The length of stay (LOS)
outcomes were recorded. Comparison was made between also varied between the groups. The TBI group had the
individuals who were treated nonoperatively (Non-Op longest LOS (16.0 13.0 days, p < 0.001), followed by the
group), those surgically treated for skull fracture repair Repair and Non-Op groups (5.3 7.0 days and 2.1 3.6
only (Repair group), and those surgically treated for trau- days, respectively).
matic brain injury (TBI) with or without repair of a skull
fracture (TBI group). Indications for intervention in the Mechanism of Injury
Repair group included displaced or depressed fracture,
open fracture, frontal sinus fracture, and cosmetic defor- The mechanisms of injury varied among the groups
mity. Patients in the TBI group had intervention for treat- (Table 3). The most common injuries sustained by the
Non-Op group were fall (n = 395, 51.2%), object to head
ment of the underlying trauma, and the group included
(n = 130, 16.8%), and motor vehicle crash (MVC; n = 85,
such operations as hematoma evacuation, decompres-
11.0%). In the Repair group, the most common mecha-
sive hemicraniectomy, external ventricular drain (EVD)
nisms of injury were object to head (n = 28, 48.2%), fall (n
placement. Skull fractures may have been repaired in
= 8, 13.8%), and MVC (n = 6, 10.3%). The most common
the TBI group, but that was not the principal indication injuries in the TBI group were MVC (n = 16, 23.9%), fall
for surgery. In general, for children younger than 2 years (n = 12, 17.9%), object to head (n = 12, 17.9%), and pedes-
of age, sutures were used to affix the bone. For children trian hit by motor vehicle (n = 8, 11.9%). The mechanisms
older than 2 years of age, titanium plates and screws were resulting in the highest percentage of surgical interven-
used. Data analysis was performed using SPSS version 17 tion (Table 4) were bicycle accident (33.3% of total bi-
(SPSS, Inc.). Chi-square tests were used for the between- cycle accidents), object to head (23.5% of total objects to
group comparisons of categorical variables. Since age, head), and pedestrian hit by motor vehicle (22.0% of total
length of hospital stay, and Glasgow Coma Scale (GCS) pedestrians hit by motor vehicle).
score were not normally distributed, Kruskal-Wallis tests
were used for the comparisons of continuous variables. Fracture Location
Mean values presented SD.
Location of the fractures was also recorded (Table
5). Overall, the most common location was the parietal
Results bone (n = 269, 30.0%), followed by the frontal bone (n =
Patient Characteristics 242, 27.0%). However, the most common bone fractured
differed among groups (p < 0.001). The parietal bone
A total of 897 patients presented to Childrens Hospi- was the most common fracture location in the Non-Op
tal of Pittsburgh between 2000 and 2005 with a diagnosis group (n = 251, 32.5%), whereas the frontal bone was the
of a skull fracture. Of these patients, 772 (86.1%) were most injured in the Repair and TBI groups (n = 36, 62.1%,
treated nonoperatively (Non-Op group). The remaining and n = 18, 26.9%, respectively). In the repair group, 8
patients were grouped according to the indication for (22.2%) of 36 required surgery for frontal sinus repair
their surgical intervention. Fifty-eight patients (6.5%) un- and 28 (77.8%) of 36 had treatment for elevation of a de-
206 J Neurosurg: Pediatrics / Volume 14 / August 2014
Surgery for pediatric skull fractures
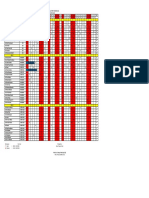
TABLE 1: Summary of patient demographics
Treatment Group (%)
Variable Non-Op Repair TBI All
sex*
male 490 (63.4) 40 (69.0) 44 (65.7) 574 (64.0)
female 282 (36.5) 18 (31.0) 23 (34.3) 323 (36.0)
total 772 (100) 58 (100) 67 (100) 897 (100)
race
white 635 (82.3) 47 (81.0) 57 (85.1) 739 (82.4)
black 86 (11.1) 8 (13.8) 6 (9.0) 100 (11.1)
other/unknown 51 (6.7) 3 (5.2) 4 (6.0) 58 (6.5)
age (yrs)
mean 5.5 8.5 8.6 5.9
range 0.121.7 0.117.7 0.117.6 0.121.7
SD 5.0 4.8 5.2 5.1
* p = 0.67.
p = 0.92.
p < 0.001.
pressed fracture and cosmetic indications. The 18 patients most common associated injury in all 3 groups (Non-Op
in the TBI group had underlying brain injuries that neces- group: n = 326, 42.2%; Repair group: n = 23, 39.7%; and
sitated intervention. The TBI group had the highest rate TBI group: n = 57, 85.1%). The next most encountered
of injuries involving 2 (23.9%) and 3 (7.5%) bones. The associated injury was orthopedic (n = 82, 10.6%) in the
Non-Op group (2 bones in 11.0% and 3 bones in 1.4%) Non-Op group, face (n = 9, 15.5%) in the Repair group,
and the Repair group (2 bones in 13.8% and 3 in bones and cardiac/pulmonary (n = 19, 28.3%) in the TBI group.
0.0%) had lower rates of multiple bone involvement in
fractures. The fractured bones most likely to result in a Procedures
patient undergoing surgical treatment (Table 6) were 3 The types of intervention in the surgical groups were
bones involved (31.3% of total 3 boneinvolved injury), reviewed. All fractures, except one, in the Repair group
frontal bone (22.3% of total frontal bone injury) and 2 were depressed (n = 57, 98.3%), and 21 fractures (36.2%)
bones involved (22% of total 2 boneinvolved injury). were open. These fractures underwent procedures for
elevation, repair, or debridement. The remaining patient
Associated Injuries
underwent the repair of a growing skull fracture 8 months
Many patients sustained injuries to other areas of after the initial injury. In the TBI group, the most com-
body besides the skull. Associated injury rates are re- mon procedure was the insertion of an EVD (77.6%).
ported in Table 7. Intracranial hemorrhage (epidural, The most common open surgical intervention was a de-
subdural, subarachnoid, or intraparenchymal) was the compressive craniectomy (22.4%), followed by epidural
TABLE 2: Hospital stay data
Treatment Group (%)
Variable Non-Op Repair TBI All
GCS score on admission*
mean 13.6 12.4 6.8 13.0
range 315 315 315 315
SD 3.4 4.6 4.5 4.0
ICU admission* 150 (19.4) 24 (41.4) 63 (94.0) 237 (26.4)
intubated* 77 (10.0) 12 (20.7) 42 (62.7) 131 (14.6)
LOS (days)*
mean 2.1 5.3 16.0 3.4
range 040.0 137 065 065
SD 3.6 7.0 13.0 6.4
* p < 0.001.
J Neurosurg: Pediatrics / Volume 14 / August 2014 207
C. M. Bonfield et al.
TABLE 3: Mechanism of injury*
Treatment Group (%)
Injury Mechanism Non-Op Repair TBI All
ATV 23 (3.0) 2 (3.4) 4 (6.0) 29 (3.2)
bicycle accident 18 (2.3) 5 (8.6) 4 (6.0) 27 (3.0)
fall 395 (51.2) 8 (13.8) 12 (17.9) 415 (46.3)
gunshot wound 1 (0.1) 0 (0.0) 1 (1.5) 2 (0.2)
lawnmower accident 0 (0.0) 1 (1.7) 0 (0.0) 1 (0.1)
motorbike accident 9 (1.2) 1 (1.7) 1 (1.5) 11 (1.2)
MVC 85 (11.0) 6 (10.3) 16 (23.9) 107 (11.9)
NAT 33 (4.3) 0 (0.0) 6 (9.0) 39 (4.3)
object to head 130 (16.8) 28 (48.2) 12 (17.9) 170 (19.0)
pedestrian vs MVC 39 (5.1) 3 (5.2) 8 (11.9) 50 (5.6)
rollerblading/skateboarding accident 12 (1.6) 0 (0.0) 2 (3.0) 14 (1.6)
sledding accident 0 (0.0) 2 (3.4) 0 (0.0) 2 (0.2)
sports collision 27 (3.5) 2 (3.4) 1 (1.5) 30 (3.3)
total 772 (100) 58 (100) 67 (100) 897 (100)
* ATV = all-terrain vehicle; NAT = nonaccidental trauma.
p < 0.001 for all mechanisms between groups.
hematoma evacuation (17.9%). Other procedures in the infection or painful hardware necessitating removal.
TBI group were intraparenchymal hematoma evacuation Thirteen patients (62.0%) had complications related to the
(7.5%), penetrating injury exploration and repair (4.5%), trauma, such as new headaches or learning disabilities.
subdural hematoma evacuation (3.0%), and posterior fos- Of note, no patient in the Repair group had worsening of
sa hematoma evacuation (1.5%). any neurological condition (weakness, visual loss, hear-
ing loss, and so on) after repair of the fracture. Similarly,
Outcomes 32 patients (42.8%) in the TBI group had complications:
The length of follow-up was similar in the two surgi- 3 (9.4%) were surgery related, and included cranioplasty
cal groups (Repair 1.1 1.8 years, TBI 1.0 1.8 years). resorption and infection, and 29 (90.6%) were a result of
Complications in the surgical groups are recorded in Ta- the trauma, such as death, hydrocephalus, or weakness.
ble 8. In the Repair group, 21 patients (36.2%) had a re-
corded complication. Eight patients (38.0%) had compli- Discussion
cations related to the surgical procedure, such as wound
Head trauma is very common in the pediatric popula-
TABLE 4: Mechanism of injury and patients requiring operative tion and 10%30% of the injuries result in skull fractures.
intervention As in our series, there is a male predominance in most re-
ports on skull fracture.1,3,9,10,16 The most common cause of
Injury Mechanism No. of Cases* injury varies among reports, but mainly lists MVCs,1,10,15
ATV 6 (20.7)
falls,3,9,13 and assaults16 as the predominant mechanisms.
However, many of these studies do not differentiate be-
bicycle accident 9 (33.3) tween the age of the patients or those who received sur-
fall 20 (4.8) gical treatment for the fracture. In their large series on
gunshot wound 1 (50.0) surgical management of depressed skull fractures in
lawnmower accident 1 (100.0) children, Erahin et al. found falls and traffic accidents
motorbike accident 2 (18.2) to be the most common causes of injury.3 In our study,
MVC 22 (20.6) although a fall was the most common injury in patients
overall, those who most frequently had their fracture re-
NAT 6 (15.4)
paired were hit in the head by an object, and patients who
object to head 40 (23.5) required treatment for their trauma were mostly involved
pedestrian vs MVC 11 (22.0) in an MVC. High-impact injuries cause more force to the
rollerblading/skateboarding accident 2 (14.3) brain, so it is not surprising that these mechanisms, like
sledding accident 2 (100.0) MVC, lead to more traumatic injuries. Equally, getting
sports collision 3 (10.0) hit in the head directly with an object, such as a baseball,
a golf club, a tree branch, or a brick, has a high potential
* Parenthetical values are the percentage of the total of the respective to cause a depressed or open skull fracture. These are the
mechanism. fracture types that routinely undergo surgical repair.
208 J Neurosurg: Pediatrics / Volume 14 / August 2014
Surgery for pediatric skull fractures
TABLE 5: Fracture location
Treatment Group (%)
Fracture Location* Non-Op Repair TBI All
frontal bone 188 (24.4) 36 (62.1) 18 (26.9) 242 (27.0)
temporal bone 129 (16.7) 5 (8.6) 11 (16.4) 145 (16.2)
parietal bone 251 (32.5) 8 (13.8) 10 (14.9) 269 (30.0)
occipital bone 108 (14.0) 1 (1.7) 7 (10.4) 116 (12.9)
2 bones 85 (11.0) 8 (13.8) 16 (23.9) 109 (12.2)
3 bones 11 (1.4) 0 (0.0) 5 (7.5) 16 (1.8)
* p < 0.001 for all fracture types between groups.
It is important to note that most patients in our large frontal sinuses, surgical repair is common. Parietal bone
series did not require surgical intervention for their skull lesions are generally covered by hair and have a good
fracture. At birth, the skull is at 25% of its growth po- chance of at least partially being remodeled without inter-
tential, which expands rapidly to 75% by age 2 and to vention. Having 2 or more bones involved in fractures is
95% by the age of 10.4,14 The rapid expansion and growth a factor associated with needing surgery, as well. Likely,
allow for a greater healing and molding capacity in this the increased rate of intervention is a result of a more
population. However, skull fractures, specifically those widespread fracture causing a larger cosmetic defect or a
involving the anterior cranial fossa base can also have greater area in need of repair. Also, having multiple bones
implications for orbital development. The growth of the injured is a harbinger of a more serious and forceful trau-
upper face is secondary to cerebral and ocular growth, matic event to the head, causing more damage to the skull
which is not completed until the age of 68 years, as well and underlying brain.
as the frontal sinus, which begins the process of aeration The majority of complications were a result of the
around age 45 years and progresses until puberty.4 It is trauma, rather than the surgical procedure. The rate of
this lack of an aerated frontal sinus that makes it possible posttraumatic epilepsy has not been shown to decrease
to treat frontal bone fractures conservatively in the young after elevation of a fracture.1,6 Posttraumatic headaches,
patient, unlike the teenage or adult patient. Intervention learning disabilities, and behavioral problems are unlike-
should be performed with the goals of improved cosme- ly to be caused or improved by surgical intervention. Ten
sis, decreased infection, and improvement of neurological patients did die during their hospital admission as a result
defect that is the result of a depressed bone fragment or of the severe brain trauma; however, no deaths occurred
underlying hematoma. after the initial hospitalization in any group.
The location of the fracture on the skull is also im- Only 1 patient (0.1%), initially treated conservatively,
portant in determining the fracture treatment strategy. developed a growing skull fracture requiring a delayed
In concordance with past reports, the parietal bone was repair. In this case, the patient was an 8-year-old boy who
the most common bone fractured overall and in the Non-
suffered a linear, nondisplaced fracture of his frontal
Op group. However, individuals sustaining frontal bone
fractures were more likely to require surgical interven- bone that extended into the orbit. He returned to the out-
tion, whether for skull fracture repair or the treatment of patient clinic 8 months after the injury with a noticeable
the underlying trauma. Frontal bone fractures are more defect in his frontal bone and swelling over the site. A CT
likely to involve the frontal sinus, skull base, and orbit scan revealed a growing skull fracture and leptomeninge-
and to have an increased chance of causing a CSF leak, al cyst. He underwent open repair of his frontal fracture
ocular complications, and cosmetic deformity of the fore- and orbital rim. Approximately 22 months later, he pre-
head. Therefore, especially in older children with aerated sented with CSF rhinorrhea, which was repaired through
an endonasal endoscopic approach and a nasoseptal flap.
TABLE 6: Fracture location and patients requiring operative The patient required no further intervention. To prevent
intervention these growing fractures, Sanford recommends surgically
exploring wide fractures in children in whom imaging
Fracture Location No. of Cases* demonstrates brain herniation through the dura mater.11
Wound infection and complaints of painful hardware
frontal bone 54 (22.3) did occur, and must be discussed when counseling the pa-
temporal bone 16 (11.0) tient and family regarding the management options. The
parietal bone 18 (6.7) complications requiring hardware removal all occurred
occipital bone 8 (6.9) in patients in whom titanium plates were used. More re-
2 bones 24 (22.0) cently, absorbable plates and screws have been used more,
3 bones 5 (31.3) which could prevent these hardware complications. Im-
portantly, no patients who underwent surgery for repair of
* Parenthetical values are the percentage of the total of the respective the fracture only had a worsening of neurological status
mechanism. after the intervention.
J Neurosurg: Pediatrics / Volume 14 / August 2014 209
C. M. Bonfield et al.
TABLE 7: Associated injuries
Treatment Group (%)
Associated Injury Non-Op Repair TBI All p Value
intracranial hematoma 326 (42.2) 23 (39.7) 57 (85.1) 406 (45.3) <0.0001
facial fracture 34 (4.4) 9 (15.5) 12 (17.9) 55 (6.1) <0.0001
spine 22 (2.9) 1 (1.7) 1 (1.5) 24 (2.7) 1.0
ophthalmological 31 (4.0) 6 (10.3) 12 (17.9) 49 (5.5) <0.0001
cardiac/pulmonary 24 (3.1) 1 (1.7) 19 (28.3) 44 (4.9) <0.0001
orthopedic 82 (10.6) 1 (1.7) 14 (20.9) 97 (10.8) <0.0001
abdominal/pelvic 22 (2.9) 1 (1.7) 17 (25.4) 40 (4.5) <0.0001
Conclusions Disclosure
Although the vast majority of children with skull The authors report no conflict of interest concerning the mate-
fractures do not require surgical intervention, it is im- rials of methods used in this study or the findings specified in this
paper.
portant to understand the characteristics, indications, and Author contributions to the study and manuscript preparation
patterns of those patients who do. Of the fractures requir- include the following. Conception and design: Bonfield, Losee.
ing intervention, fewer than half are treated on the basis Acquisition of data: Bonfield, Naran, Adetayo. Analysis and inter-
of skull fracture elevation repair only. Being hit in the pretation of data: all authors. Drafting the article: Bonfield. Critically
head by an object is by the most common mechanism of a revising the article: all authors. Reviewed submitted version of man-
fracture needing repair and an MVC is the most common uscript: all authors. Approved the final version of the manuscript on
mechanism resulting in management of TBI. Patients sus- behalf of all authors: Bonfield. Statistical analysis: Bonfield. Study
supervision: Pollack, Losee.
taining a frontal bone fracture or having multiple skull
bones involved in the fracture are more likely to require
surgical intervention. The majority of complications are a References
direct result of the traumatic event, not the surgical inter- 1. Braakman R: Depressed skull fracture: data, treatment, and
vention. No patients had worsening of a neurological defi- follow-up in 225 consecutive cases. J Neurol Neurosurg Psy-
cit after fracture repair, but complications such as painful chiatry 35:395402, 1972
hardware and wound infections did necessitate further 2. Erlichman DB, Blumfield E, Rajpathak S, Weiss A: Associa-
interventions. An understanding of this population with tion between linear skull fractures and intracranial hemor-
rhage in children with minor head trauma. Pediatr Radiol
fractures will enable practitioners to better identify pa- 40:13751379, 2010
tients who may need surgical intervention and to counsel 3. Erahin Y, Mutluer S, Mirzai H, Palali I: Pediatric depressed
patients regarding late sequelae of the trauma, fracture, skull fractures: analysis of 530 cases. Childs Nerv Syst 12:
and intervention. 323331, 1996
TABLE 8: Complications in surgical groups
Patient Treatment Group
Repair* TBI
Surgery Related Trauma Related Surgery Related Trauma Related
concern over craniotomy defect deep venous thrombosis cranioplasty revision after resorption behavioral problems
CSF leak after growing skull fracture repair new headaches (5) hardware removal for pain 18 mos later death (10)
painful hardware learning disability (2) wound infection, split thickness skin graft deep venous thrombosis (2)
removal of hardware 6 mos later multiple procedures for face/ headaches
forehead soft tissue injury
salmonella meningitis postop seizures (2) motor weakness (4)
scalp revision 4 yrs later due to dehiscence worsening of migraines learning disability (4)
wound revision & hardware removal 3 yrs motor weakness seizures (2)
later due to widening scar & pain
wound infection spasticity (2)
hydrocephalus (3)
* In the Repair group, 21 (36.2%) of 58 patients experienced a complication: 8 complications (38.0%) were surgery related and 13 complications (62.0%)
were injury related.
In the TBI group, 32 (47.8%) of 67 patients experienced a complication: 3 complications (9.4%) were surgery related and 29 complications (90.6%)
were trauma related.
210 J Neurosurg: Pediatrics / Volume 14 / August 2014
Surgery for pediatric skull fractures
4. Haug RH, Foss J: Maxillofacial injuries in the pediatric pa- 12. Schneier AJ, Shields BJ, Hostetler SG, Xiang H, Smith GA:
tient. Oral Surg Oral Med Oral Pathol Oral Radiol Endod Incidence of pediatric traumatic brain injury and associated
90:126134, 2000 hospital resource utilization in the United States. Pediatrics
5. Hung KL, Liao HT, Huang JS: Rational management of sim- 118:483492, 2006
ple depressed skull fractures in infants. J Neurosurg 103 (1 13. Shane SA, Fuchs SM: Skull fractures in infants and predic-
Suppl):6972, 2005 tors of associated intracranial injury. Pediatr Emerg Care
6. Jennett B, Miller JD, Braakman R: Epilepsy after monmissile 13:198203, 1997
depressed skull fracture. J Neurosurg 41:208216, 1974 14. Singh DJ, Bartlett SP: Pediatric craniofacial fractures: long-
7. Mann KS, Chan KH, Yue CP: Skull fractures in children: their term consequences. Clin Plast Surg 31:499518, vii, 2004
assessment in relation to developmental skull changes and acute 15. Steinbok P, Flodmark O, Martens D, Germann ET: Manage-
intracranial hematomas. Childs Nerv Syst 2:258261, 1986 ment of simple depressed skull fractures in children. J Neu-
8. National Center for Injury Prevention and Control: Traumatic rosurg 66:506510, 1987
Brain Injury in the United States: Assessing Outcomes in 16. van den Heever CM, van der Merwe DJ: Management of de-
Children. Atlanta: Centers for Disease Control and Preven- pressed skull fractures. Selective conservative management of
tion, 2000 (http://www.cdc.gov/traumaticbraininjury/assess nonmissile injuries. J Neurosurg 71:186190, 1989
ing_outcomes_in_children.html) [Accessed May 7, 2014]
9. Nelson EL, Melton LJ III, Annegers JF, Laws ER, Offord KP:
Incidence of skull fractures in Olmsted County, Minnesota.
Neurosurgery 15:318324, 1984 Manuscript submitted August 11, 2013.
10. Saadat S, Rashidi-Ranjbar N, Rasouli MR, Rahimi-Movaghar Accepted May 5, 2014.
V: Pattern of skull fracture in Iran: report of the Iran National Please include this information when citing this paper: pub-
Trauma Project. Ulus Travma Acil Cerrahi Derg 17:149151, lished online June 6, 2014; DOI: 10.3171/2014.5.PEDS13414.
2011 Address correspondence to: Christopher M. Bonfield, M.D., 200
11. Sanford RA: Prevention of growing skull fractures. Report of Lothrop St., Ste. B400, Pittsburgh, PA 15213. email: bonfieldcm@
2 cases. J Neurosurg Pediatr 5:213218, 2010 upmc.edu.
J Neurosurg: Pediatrics / Volume 14 / August 2014 211
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Workplace Site Audit Checklist PharmacyDocument3 pagesWorkplace Site Audit Checklist PharmacyWaqar LatifNo ratings yet
- NCM 107 Module 2M Ethico Moral Aspects of NursingDocument18 pagesNCM 107 Module 2M Ethico Moral Aspects of NursingTrisha ApillanesNo ratings yet
- Mapping Mina 2 MEI 2022: No. Kamar Identitas Subjektif Diagnosis Laboratorium Terapi Planing Keluhan GCS TD K1B1Document22 pagesMapping Mina 2 MEI 2022: No. Kamar Identitas Subjektif Diagnosis Laboratorium Terapi Planing Keluhan GCS TD K1B1ifanda80No ratings yet
- Mapping MINA 1 24-05-2022Document29 pagesMapping MINA 1 24-05-2022ifanda80No ratings yet
- DR DR SYAHRUL, SP.S (K)Document28 pagesDR DR SYAHRUL, SP.S (K)ifanda80No ratings yet
- Mapping Dr. ImranDocument12 pagesMapping Dr. Imranifanda80No ratings yet
- Bone MalformationDocument6 pagesBone Malformationifanda80No ratings yet
- Mapping Dr. Nur Astini, SP.S (K) : Mina 1Document8 pagesMapping Dr. Nur Astini, SP.S (K) : Mina 1ifanda80No ratings yet
- Raber DS Lantai Bawah Dan Pinere 09-03-22 GHDocument14 pagesRaber DS Lantai Bawah Dan Pinere 09-03-22 GHifanda80No ratings yet
- Mapping Luar Mina Lantai 2-24 Mei 2022Document31 pagesMapping Luar Mina Lantai 2-24 Mei 2022ifanda80No ratings yet
- Mustafa M. Amin, LK, 53 THNDocument3 pagesMustafa M. Amin, LK, 53 THNifanda80No ratings yet
- Raber Pasien dr. Desi Salwani KGHDocument10 pagesRaber Pasien dr. Desi Salwani KGHifanda80No ratings yet
- Dr. Dr. Nova Dian Lestari, SP.S (K) 06/11/2021: Mina 1Document4 pagesDr. Dr. Nova Dian Lestari, SP.S (K) 06/11/2021: Mina 1ifanda80No ratings yet
- Raudha 2: N O Kamar Identitas Subjektif Diagnosis Laboratorium Terapi Planing Keluhan GCS TDDocument3 pagesRaudha 2: N O Kamar Identitas Subjektif Diagnosis Laboratorium Terapi Planing Keluhan GCS TDifanda80No ratings yet
- MAPPING PATIENTS' MEDICAL RECORDSDocument11 pagesMAPPING PATIENTS' MEDICAL RECORDSifanda80No ratings yet
- MAPPING DR Elsa 30211016Document7 pagesMAPPING DR Elsa 30211016ifanda80No ratings yet
- Dr. Dr. Nova Dian Lestari, SP.S (K) 06/11/2021: Mina 1Document4 pagesDr. Dr. Nova Dian Lestari, SP.S (K) 06/11/2021: Mina 1ifanda80No ratings yet
- DR DR SYAHRUL, SP.S (K)Document28 pagesDR DR SYAHRUL, SP.S (K)ifanda80No ratings yet
- Raudha 2: N O Kamar Identitas Subjektif Diagnosis Laboratorium Terapi Planing Keluhan GCS TDDocument3 pagesRaudha 2: N O Kamar Identitas Subjektif Diagnosis Laboratorium Terapi Planing Keluhan GCS TDifanda80No ratings yet
- Mapping Dr. ImranDocument12 pagesMapping Dr. Imranifanda80No ratings yet
- Jadwal Jaga Ppds Neurologi Agustus 2021 Revisi IIDocument1 pageJadwal Jaga Ppds Neurologi Agustus 2021 Revisi IIifanda80No ratings yet
- JADWAL JAGA PPDS NEUROLOGI AGUSTUS 2021 REVISI II-dikonversiDocument4 pagesJADWAL JAGA PPDS NEUROLOGI AGUSTUS 2021 REVISI II-dikonversiifanda80No ratings yet
- Intracerebral Hemorrhage ICHDocument52 pagesIntracerebral Hemorrhage ICHStaporn KasemsripitakNo ratings yet
- DR DR SYAHRUL, SP.S (K)Document28 pagesDR DR SYAHRUL, SP.S (K)ifanda80No ratings yet
- Mapping Mina 2 Patient RecordsDocument9 pagesMapping Mina 2 Patient Recordsifanda80No ratings yet
- Dr. Dr. Nova Dian Lestari, SP.S (K) 06/11/2021: Mina 1Document4 pagesDr. Dr. Nova Dian Lestari, SP.S (K) 06/11/2021: Mina 1ifanda80No ratings yet
- Mina 1 (K6, 7.1-3)Document9 pagesMina 1 (K6, 7.1-3)ifanda80No ratings yet
- MAPPING AQSA 2, Kamis 29 April 2021 (BARU)Document21 pagesMAPPING AQSA 2, Kamis 29 April 2021 (BARU)ifanda80No ratings yet
- Raudha 2: N O Kamar Identitas Subjektif Diagnosis Laboratorium Terapi Planing Keluhan GCS TDDocument3 pagesRaudha 2: N O Kamar Identitas Subjektif Diagnosis Laboratorium Terapi Planing Keluhan GCS TDifanda80No ratings yet
- Mapping Mina 2 Patient RecordsDocument9 pagesMapping Mina 2 Patient Recordsifanda80No ratings yet
- Mina 1 (K6, 7.1-3)Document9 pagesMina 1 (K6, 7.1-3)ifanda80No ratings yet
- Mapping Dr. Ika Sp.s (K)Document3 pagesMapping Dr. Ika Sp.s (K)ifanda80No ratings yet
- Barangay Klinan6 Bhs - Continuous Monitoring and Surveillance For Covid-19 Symptoms On All PuroksDocument3 pagesBarangay Klinan6 Bhs - Continuous Monitoring and Surveillance For Covid-19 Symptoms On All PuroksInchic MirandaNo ratings yet
- Funda Lec p1 ReviewerDocument12 pagesFunda Lec p1 ReviewerJhever Niesas AlmadinNo ratings yet
- The Effect of Drugs On PregnancyDocument26 pagesThe Effect of Drugs On PregnancyVictoria MarionNo ratings yet
- Disseminated Intravascular CoagulationDocument19 pagesDisseminated Intravascular CoagulationAnna MilliziaNo ratings yet
- Ebr2 CunananDocument2 pagesEbr2 CunananAbbyNo ratings yet
- HRI ResearchArticle 18 Harrison HELATDocument3 pagesHRI ResearchArticle 18 Harrison HELATChalida HayulaniNo ratings yet
- O Pt's Do NOT Move Gradually Through The Phases-Pt's Eb and Flow-Much More FluidDocument4 pagesO Pt's Do NOT Move Gradually Through The Phases-Pt's Eb and Flow-Much More FluidKaitlyn ProbascoNo ratings yet
- Psychiatric Mental Health Nursing Question PDF DownloadDocument2 pagesPsychiatric Mental Health Nursing Question PDF DownloadCharles Obaleagbon100% (1)
- Migmar Tsering (Mike) S ResumeDocument3 pagesMigmar Tsering (Mike) S Resumeapi-284044370No ratings yet
- Advance Your Health Through Lifestyle ChangesDocument74 pagesAdvance Your Health Through Lifestyle ChangesMohammadEhtashamNo ratings yet
- Sujok Therapy FAQDocument9 pagesSujok Therapy FAQProbodh1100% (5)
- What We Need From You: Please Return Page 2 Via Fax To (512) 738-8397Document2 pagesWhat We Need From You: Please Return Page 2 Via Fax To (512) 738-8397Tàrár ŁàráibNo ratings yet
- EPIDEMIOLOGY OF HEAD INJURY IN COIMBATOREDocument6 pagesEPIDEMIOLOGY OF HEAD INJURY IN COIMBATOREArjun CVNo ratings yet
- Healthways WholeHealth LivingDocument1 pageHealthways WholeHealth LivingHealthways, Inc.No ratings yet
- Interview QuestionsDocument13 pagesInterview QuestionsDimash100% (1)
- New Drug Application HardDocument37 pagesNew Drug Application HardGANESH KUMAR JELLA100% (1)
- NEET MDS 2021 Recall 151-200 Questions PDFDocument183 pagesNEET MDS 2021 Recall 151-200 Questions PDFMahima Mishra100% (1)
- Removable Partial Dentures - Principles of DesignDocument34 pagesRemovable Partial Dentures - Principles of DesignRalf GuscottNo ratings yet
- The Imperial College of Australia: Sitxwhs003 - Implement and Monitor Work Health and Safety Practices WorksheetsDocument6 pagesThe Imperial College of Australia: Sitxwhs003 - Implement and Monitor Work Health and Safety Practices WorksheetsgunnNo ratings yet
- Cancer Ms LecDocument16 pagesCancer Ms LecJulia Rae Delos Santos100% (1)
- ENT Notes For Med StudentsDocument4 pagesENT Notes For Med Studentsnikki100% (1)
- Perf. PeritonitisDocument5 pagesPerf. PeritonitisChiriţoiu AnamariaNo ratings yet
- KaileyDocument7 pagesKaileyapi-470964508No ratings yet
- Anemia FetalDocument9 pagesAnemia FetalCarolina Cabrera CernaNo ratings yet
- National Health MissionDocument70 pagesNational Health Missionprabha krishnanNo ratings yet
- Open Letter To AASDDocument4 pagesOpen Letter To AASDWBAYNo ratings yet
- Clinical Assessment and Examination in OrthopedicsDocument196 pagesClinical Assessment and Examination in OrthopedicsMom of twoNo ratings yet