Professional Documents
Culture Documents
Adv Writing 2
Uploaded by
api-3817000370 ratings0% found this document useful (0 votes)
44 views4 pagesOriginal Title
adv writing 2
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
44 views4 pagesAdv Writing 2
Uploaded by
api-381700037Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 4
Lucas Duran n01045927
Advance Nutrition Science 1
Dr. Arikawa
11/06/2016
Dietary Fat and Contributors to Cardiovascular Disease
In a position stated by the Academy of Nutrition and Dietetics in 2014, it is in the
general populations best interest for 20%-35% of energy be provided by dietary fat; emphasizing
an increased recommendation for n-3 and n-6 polyunsaturated fatty acids (PUFA) and decrease
in trans fatty acids(TFA) and saturated fatty acids (SFA) with a diet approach that includes
consistent consumption of fish, nuts, seeds, lean meat, poultry, low fat dairy, vegetables, fruits,
whole grains, and legumes. How recommendations and intakes align with consumption patterns
are what can be learned from the Academys stance, one that shows chronic disease prevalence
from abiding by these recommendations over time. It is shown that among the Academys stance
the majority of organizations support the above mentioned target range. It is also emphasized and
recommended that sustainable health status can be aligned with adjusting saturated and
unsaturated fat consumption rather than lowering both all-together.
So many differing health implications come from the first double bond position
correlating to n-3 versus n-6 fatty acids. The academy states one must first understand the
benefits of both before adjusting intake levels while understanding the need for Trans and
saturated fatty acids to be lowered. Research suggests that inadequacy of n-3 fatty acids is
associated with cardiac death and not balancing the proper ratio can result in an increase disease
risk in healthy individuals (this stance is based on this population) [1]. Due to human inability to
synthesize these fatty acids obtaining them through the diet is very important as they are used for
a multitude of things. Recommendations have since 2005 changed drastically to show research
that includes 11 cohort studies from multiple countries that took years to conduct. The research
findings were noted to inform individuals that a focus needs to be made that replaces trans-fatty
acids (TFA) and saturated fatty acids (SFA) and promotes an increased n-3/n-6 PUFA
consumption. With recommendations showing such a drastic intake increase of PUFA results
show exactly why qualitative data associated directly supports cardiac health and a decreasing
risk of Cardiovascular heart disease.
Vannice and Rasmussens research indicates how these fatty acids contribute a high
amount of functional properties towards homeostatic regulation that are associated with the
following; activation and inhibition of inflammation, platelet formation, cell growth, cell
membrane production, cognitive function, bone metabolism, and organ muscle contraction that
largely equates to vasoconstrictive as well vasodilating factors [1]. While a-linolenic acid (ALA)
and linoleic acid (LA; most highly consumed PUFA) are of big emphasis due to their precursor
selectivity the importance of balance can regulate so many long term benefits or issues. A newer
diagnosis of chronic low-grade inflammation brings more of a long term analysis to the equation,
many of the subjects that took place in this research participated over a long period of time. With
fatty acid recognition being of much more importance now than just a few years ago,
supplements have entered the market with everything from flax and chia seeds to fish oils and
much more. A combination of studies completed in 2011 revealed fish or fish oil consumption
was consistent with a thirty six percent decrease in fatal heart disease [1].
In a stance similar to the academys the Journal of Biochemical Nutrition stands firm on
the idea of high circulation of SFA being a direct contributor to CVD. Also, with their not being
a RDA they too believe these fatty acids should be lowered or removed from the diet all together
and in comparison show a decrease in CVD risk when replaced with PUFA [1,2]. The research
findings are associated with systemic low-grade inflammation, insulin resistance, and metabolic
syndrome that can eventually lead to the development of CVD are consistent with the
academys. The Journal of Biochemical Nutrition states that a high intake of SFA can directly be
distinguished by a high circulating level of LDLs and lower concentration of HDLs [2]. Both of
their stances align with American intakes floating around 10 percent and state that optimal range
is consistently around five percent. All the evidence supporting this range is inconclusive
however due to both stating that SFA intake cant be specifically connected to cardiovascular
problems but otherwise a contributor.
The hesitancy to directly connect the types of SFA to cardiovascular health is
summarized by the variety of food consumed throughout the diet and complexity of ingredients
amongst the majority of dishes. Most importantly the western diet, and more specifically the
consumption of red meat and fatty dairy products. The Academy and Biochemical Journal of
Nutrition both agree that red meat has a SFA content that can be a contributor to increases in
disease risk but the moderations appear to be the question. A more general statement to make
from this information is how much is too much, their emphasis on percentage totals on what they
should be is the more important question. While CVD has shown high LDL circulation research
appears to only put light on an increase CVD risks. The question of other components comes into
play as well for example, sodium and iron are two other things commonly found in conjunction
with red meat that are contributors according to Vannice and Rasmussen.
In a research topic conducted by the American Journal of Clinical Nutrition the focus was
on the outcome of saturated fat effects on diets of men and women aged twenty-one to sixty with
moderate CVD risk. The results included little to no effect on flow-mediated dilation, fasting
serum lipids, microvascular reactivity, arterial stiffness, ambulatory blood pressure, markers of
insulin resistance, inflammation, and endothelial activation [3]. Among the results, replacing
these SFA with MUFA and PUFA showed promising results with a conclusion stating a
seventeen to twenty percent decrease in CVD risk. Similar to the other two sources listed
however there results were inconclusive enough to say that fat replacement is still unclear. The
types of diets that were included in this research were isoenergetic that targeted lowering
circulating LDLs and increasing HDLs. Another interesting result showed that nighttime
systolic blood pressure decreased which correlates to the Academys stance on chronic low grade
inflammation. Their position also aligns with the benefits of not replacing diets with
carbohydrates as that can have adverse effects on circulating cholesterol inadvertently.
In conclusion, it can be stated that since updated recommendations were established a
few years ago a tighter window has been created. As research shows that SFA contribute a high
amount of LDLs, an emphasis on their replacement with PUFA or MUFA (more specifically n-
3) being beneficial is fact. Lower CVD risk has been aligned with this but the question of chronic
low grade inflammation draws the most interest. When establishing target ranges of SFA the
major point of the academy is to slowly eliminate them from the diet with replacing them with
healthier PUFA that contribute many more healthy benefits. The second and third references
listed below support the academys stance with recommendations on what adequate intakes
should be. All three have inconclusive evidence however, genetics and other lifestyle factors
appear to play a bigger role in relation to CVD than what has been previously known especially
in the last few years.
References
1. Vannice G, Rasmussen H. From the Academy: Position of the Academy of Nutrition
and Dietetics: Dietary Fatty Acids for Healthy Adults. Journal Of The Academy Of
Nutrition And Dietetics [serial online]. January 1, 2014;114:136-153. Available from:
ScienceDirect, Ipswich, MA. Accessed November 2, 2016.
2. Ruiz-Nez B, Dijck-Brouwer D, Muskiet F. The relation of saturated fatty acids
with low-grade inflammation and cardiovascular disease. Journal Of Nutritional
Biochemistry [serial online]. October 2016;36:1-20. Available from: Environment
Complete, Ipswich, MA. Accessed November 4, 2016.
3. Katerina Vafeiadou, Michelle Weech, Hana Altowaijri, Susan Todd, Parveen
Yaqoob, Kim G Jackson, Julie A Lovegrove. Replacement of saturated with
unsaturated fats had no impact on vascular function but beneficial effects on lipid
biomarkers, E-selectin, and blood pressure. American Journal of Clinical Nutrition .
2015;102(1):40-48.
You might also like
- A Changing View On Sfas and Dairy: From Enemy To Friend: EditorialDocument2 pagesA Changing View On Sfas and Dairy: From Enemy To Friend: EditorialCaio Whitaker TosatoNo ratings yet
- Dietary Fats and Oils White PaperDocument25 pagesDietary Fats and Oils White Papermudassir qazalbashNo ratings yet
- Nutrients 10 01385Document16 pagesNutrients 10 01385Alex GutiérrezNo ratings yet
- Types of Dietary Fat and Risk of Coronary Heart Disease: A Critical ReviewDocument15 pagesTypes of Dietary Fat and Risk of Coronary Heart Disease: A Critical ReviewMegan KnightNo ratings yet
- Hypoglycemia in Diabetes: Pathophysiology, Prevalence, and PreventionFrom EverandHypoglycemia in Diabetes: Pathophysiology, Prevalence, and PreventionNo ratings yet
- Am J Clin Nutr 2015 Cespedes Ajcn.Document4 pagesAm J Clin Nutr 2015 Cespedes Ajcn.Jhon Sahatma SinagaNo ratings yet
- NIH Public Access: Artificial Sweeteners Produce The Counterintuitive Effect of Inducing Metabolic DerangementsDocument19 pagesNIH Public Access: Artificial Sweeteners Produce The Counterintuitive Effect of Inducing Metabolic DerangementsLuiggi D. Chambi MaidaNo ratings yet
- Siri-Tarino - Saturated Fat CHO e DCVDocument8 pagesSiri-Tarino - Saturated Fat CHO e DCVGracielaRecheNo ratings yet
- Review Article Effect of The Dietary Fat Quality On Insulin SensitivityDocument9 pagesReview Article Effect of The Dietary Fat Quality On Insulin SensitivityGilberto BicalhoNo ratings yet
- Articulo 45correctoDocument7 pagesArticulo 45correctoKarol Lizeth Paz ZuñigaNo ratings yet
- Nej M 199504133321512Document7 pagesNej M 199504133321512Sylvia IngridNo ratings yet
- Associations With Cardiometabolic Risk and Response To Weight LossDocument3 pagesAssociations With Cardiometabolic Risk and Response To Weight LossTeresa CuatecontziNo ratings yet
- Dietary Fat and Coronary Heart Disease - Summary of Evidence From Prospective Cohort and Random Is Ed Controlled TrialsDocument29 pagesDietary Fat and Coronary Heart Disease - Summary of Evidence From Prospective Cohort and Random Is Ed Controlled Trialsa_rogall7926No ratings yet
- Association of Dietary, Circulating, and Supplement Fatty Acids With Coronary RiskDocument7 pagesAssociation of Dietary, Circulating, and Supplement Fatty Acids With Coronary RiskVitor CordeiroNo ratings yet
- Decades of Diet Deception and the Spread of Non-Communicable Chronic DiseasesFrom EverandDecades of Diet Deception and the Spread of Non-Communicable Chronic DiseasesNo ratings yet
- Ultraprocessed Foods and Excess Heart Age Among Us AdultsDocument10 pagesUltraprocessed Foods and Excess Heart Age Among Us AdultsSaionara FranciscoNo ratings yet
- Busting The Myth of Saturated Fat in Heart Disease British Medical Journal 2013Document2 pagesBusting The Myth of Saturated Fat in Heart Disease British Medical Journal 2013jackjensen2852No ratings yet
- Stoke NutritionDocument14 pagesStoke Nutritionapi-150223943No ratings yet
- Caffeine Is Protective in Patients With Non-Alcoholic Fatty Liver DiseaseDocument7 pagesCaffeine Is Protective in Patients With Non-Alcoholic Fatty Liver DiseaseYelvi Novita RozaNo ratings yet
- Association of Dietary Fatty Acids With Coronary RiskDocument17 pagesAssociation of Dietary Fatty Acids With Coronary Riskubiktrash1492No ratings yet
- Stress-Associated Eating Leads To ObesityDocument2 pagesStress-Associated Eating Leads To ObesityYoga Agung PNo ratings yet
- Plasma Lipids: Optimal Levels for HealthFrom EverandPlasma Lipids: Optimal Levels for HealthAmerican Health FoundationNo ratings yet
- Polyunsaturated Fatty Acids, Specialized Pro-Resolving Mediators, and Targeting Inflammation Resolution in The Age of Precision NutritionDocument8 pagesPolyunsaturated Fatty Acids, Specialized Pro-Resolving Mediators, and Targeting Inflammation Resolution in The Age of Precision NutritionAndrés Felipe Gutiérrez RodríguezNo ratings yet
- Meta-Analysis in Research On Nutrition: To The EditorDocument2 pagesMeta-Analysis in Research On Nutrition: To The EditorLUISNo ratings yet
- ACS Guidelines PDFDocument38 pagesACS Guidelines PDFGabriel MateusNo ratings yet
- Journal of Hypertension and Management JHM 5 037Document10 pagesJournal of Hypertension and Management JHM 5 037reducdyantaNo ratings yet
- Dietary Saturated Fats and Their Food Sources in Relation To The RiskDocument8 pagesDietary Saturated Fats and Their Food Sources in Relation To The RiskJohn SammutNo ratings yet
- Obesidade Rio de JaneiroDocument7 pagesObesidade Rio de JaneiroarianeoliNo ratings yet
- Annotated BibliographyDocument4 pagesAnnotated Bibliographyapi-439027462No ratings yet
- Excess Protein Intake Relative To Fiber and Cardiovascular Events in Elderly Men With Chronic Kidney DiseaseDocument6 pagesExcess Protein Intake Relative To Fiber and Cardiovascular Events in Elderly Men With Chronic Kidney Diseaseluis Gomez VallejoNo ratings yet
- 营养:疾病预防和治疗Document12 pages营养:疾病预防和治疗张芬No ratings yet
- NutrientsDocument19 pagesNutrientsDadi SindhuNo ratings yet
- Nutrition and HypertensionDocument3 pagesNutrition and HypertensionKajee GrantNo ratings yet
- Nutrition and Prevention of Chronic-Degenerative Diseases: Sciencedirect SciencedirectDocument5 pagesNutrition and Prevention of Chronic-Degenerative Diseases: Sciencedirect SciencedirectJustNay 'nuna' Arief HusadaNo ratings yet
- Nutrients 05 02019Document9 pagesNutrients 05 02019FITYOURBODYNo ratings yet
- Low Carb ResearchDocument31 pagesLow Carb ResearchMozHeartNo ratings yet
- Dash Diet For Beginners - Lower Your Blood Pressure For Healthy Weight LossFrom EverandDash Diet For Beginners - Lower Your Blood Pressure For Healthy Weight LossNo ratings yet
- A Riview of Nutritional Factor in Hypertension ManagementDocument13 pagesA Riview of Nutritional Factor in Hypertension Managementprawira heroNo ratings yet
- 2016 Lacroix S Nutrition in CV RehabDocument7 pages2016 Lacroix S Nutrition in CV RehabHumamuddinNo ratings yet
- Am J Clin Nutr 2014 Chung Ajcn.114.086314Document17 pagesAm J Clin Nutr 2014 Chung Ajcn.114.086314Daniel Lee Eisenberg JacobsNo ratings yet
- Non Pharmacological Management of Hypertension - PMCDocument16 pagesNon Pharmacological Management of Hypertension - PMCBrian TaylorNo ratings yet
- Nutrients: The Environmental Regulation of Cardiovascular Gene ExpressionDocument6 pagesNutrients: The Environmental Regulation of Cardiovascular Gene ExpressionTrismegisteNo ratings yet
- Adherence To A Healthy Diet in Relation To Cardiovascular Incidence and Risk Markers Evidence From The Caerphilly Prospective StudyDocument14 pagesAdherence To A Healthy Diet in Relation To Cardiovascular Incidence and Risk Markers Evidence From The Caerphilly Prospective StudyRobet Agung wicaksonoNo ratings yet
- Pathophysiology of Obesity-Induced Health ComplicationsFrom EverandPathophysiology of Obesity-Induced Health ComplicationsParamjit S. TappiaNo ratings yet
- Prostaglandins, Leukotrienes and Essential Fatty AcidsDocument12 pagesProstaglandins, Leukotrienes and Essential Fatty AcidsNatália LopesNo ratings yet
- DASH DIET COOKBOOK: Nourishing Recipes to Lower Blood Pressure, Boost Heart Health, and Achieve Long-Term Well-Being (2024 Guide)From EverandDASH DIET COOKBOOK: Nourishing Recipes to Lower Blood Pressure, Boost Heart Health, and Achieve Long-Term Well-Being (2024 Guide)No ratings yet
- Research Open Access: Adi Lukas Kurniawan, Chien-Yeh Hsu, Hsiao-Hsien Rau, Li-Yin Lin and Jane C.-J. ChaoDocument11 pagesResearch Open Access: Adi Lukas Kurniawan, Chien-Yeh Hsu, Hsiao-Hsien Rau, Li-Yin Lin and Jane C.-J. ChaoLeonardo AzevedoNo ratings yet
- Nuts and Coronary Heart DiseaseDocument8 pagesNuts and Coronary Heart DiseasejparanotiNo ratings yet
- Dietary Fiber Intake and Glycemic Control: Coronary Artery Calcification in Type 1 Diabetes (CACTI) StudyDocument8 pagesDietary Fiber Intake and Glycemic Control: Coronary Artery Calcification in Type 1 Diabetes (CACTI) StudyLeonardo AzevedoNo ratings yet
- Ultra Processed Foods and Cardiovascular Diseases Poten - 2021 - Advances in NuDocument8 pagesUltra Processed Foods and Cardiovascular Diseases Poten - 2021 - Advances in NuMauricio RebolloNo ratings yet
- Shan. Association of Low-Carbohydrate and Low-Fat Diets With MortalityDocument20 pagesShan. Association of Low-Carbohydrate and Low-Fat Diets With MortalityMaria Julia Ogna EgeaNo ratings yet
- Term Paper 609Document10 pagesTerm Paper 609api-532399186No ratings yet
- Adherence To A Healthy Diet in Relation To Cardiovascular Incidence and Risk Markers - Evidence From The Caerphilly Prospective StudyDocument14 pagesAdherence To A Healthy Diet in Relation To Cardiovascular Incidence and Risk Markers - Evidence From The Caerphilly Prospective StudyXochitl PonceNo ratings yet
- Dean Ornish Mostly PlantsDocument2 pagesDean Ornish Mostly Plantsipman0100% (2)
- The Dash Diet: Lower Blood Pressure Lose Weight And Feel GreatFrom EverandThe Dash Diet: Lower Blood Pressure Lose Weight And Feel GreatNo ratings yet
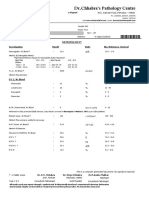
- DR - Chhabra's Pathology Centre: E-ReportDocument6 pagesDR - Chhabra's Pathology Centre: E-ReportHimanshu KalaNo ratings yet
- Modification of Fat and OilDocument18 pagesModification of Fat and OilPawan ShresthaNo ratings yet
- Drug Nutrient Depletions - Interactions ChartDocument2 pagesDrug Nutrient Depletions - Interactions ChartEygenia PapadpoulouNo ratings yet
- Excel Fro Payment LinkDocument7 pagesExcel Fro Payment LinkSanjay NadekarNo ratings yet
- CPT Code 99091 Alexander LDocument6 pagesCPT Code 99091 Alexander LBryan MorteraNo ratings yet
- Daftar Harga Qca Kimia Klinik Name of Products Catalog Packing Size Price Configuration Rp/kitDocument3 pagesDaftar Harga Qca Kimia Klinik Name of Products Catalog Packing Size Price Configuration Rp/kitKiki ItaNo ratings yet
- Total+Allowable+Error+Limits+Table+Example Rev20120725Document4 pagesTotal+Allowable+Error+Limits+Table+Example Rev20120725Meidina Siti HanifahNo ratings yet
- The Endocrine Pancreas: Regulation of Carbohydrate MetabolismDocument61 pagesThe Endocrine Pancreas: Regulation of Carbohydrate MetabolismNona AsolaNo ratings yet
- Lab Values 1Document30 pagesLab Values 1Ezekiel John GarciaNo ratings yet
- Primary Prevention of CVDDocument53 pagesPrimary Prevention of CVDYibeltal AssefaNo ratings yet
- The Latest News About AvocadosDocument4 pagesThe Latest News About Avocadosq wNo ratings yet
- Hapalan KardiovaskulerDocument3 pagesHapalan KardiovaskulerMithaNo ratings yet
- Effectof Educational Programfor Health Promoting LifestyleDocument11 pagesEffectof Educational Programfor Health Promoting LifestylePawan MishraNo ratings yet
- Clinical Chemistry 2Document65 pagesClinical Chemistry 2Jennifer BaluarteNo ratings yet
- 4 +basic+nutritionDocument71 pages4 +basic+nutritionJasmine CorreosNo ratings yet
- TDS-Liquid Margarine 105615 (8545 - 1)Document2 pagesTDS-Liquid Margarine 105615 (8545 - 1)Javier MoralesNo ratings yet
- 1 s2.0 S0955286317303868 MainDocument14 pages1 s2.0 S0955286317303868 MainAdib FraNo ratings yet
- T2DM PracticalGuide 20190718 FA Ebook2Document80 pagesT2DM PracticalGuide 20190718 FA Ebook2Nokoline HuNo ratings yet
- Co DR Rajagopal, 4Th Street Arokiya Nagar, NK Road, Near Eb Colony, Thanjavur, Tamilnadu.,613005Document16 pagesCo DR Rajagopal, 4Th Street Arokiya Nagar, NK Road, Near Eb Colony, Thanjavur, Tamilnadu.,613005Rahul GNo ratings yet
- Prioritization of ProblemsDocument3 pagesPrioritization of ProblemsBLABLEBLIBLOBLUUUNo ratings yet
- Https Tdiagnostics - Telangana.gov - in ViewFiles - Aspx ReportId 04IJ4X6CFze8WreRm1UotQDocument9 pagesHttps Tdiagnostics - Telangana.gov - in ViewFiles - Aspx ReportId 04IJ4X6CFze8WreRm1UotQvanitha vemulaNo ratings yet
- HDL DirectDocument2 pagesHDL DirectDinesh SreedharanNo ratings yet
- 8 Benefits of Mustard OilDocument10 pages8 Benefits of Mustard OilArshad Rezwan AbidNo ratings yet
- Lesson Plan - Cardiovascular DiseaseDocument5 pagesLesson Plan - Cardiovascular DiseaseNasimaNo ratings yet
- Doctors Testimonials For Gamma OryzanolDocument8 pagesDoctors Testimonials For Gamma OryzanolRAJESH ANNAMALAI ALNo ratings yet
- Cholesterol, The Mind, and The Brain - Harvard HealthDocument4 pagesCholesterol, The Mind, and The Brain - Harvard HealthArthur100% (2)
- J. Lipid Res.-1968-Glomset-155-67Document13 pagesJ. Lipid Res.-1968-Glomset-155-67Stefania CristinaNo ratings yet
- Diabetes Related CKD 2Document1 pageDiabetes Related CKD 2Jia-PeiWuNo ratings yet
- Tube Collection GuideDocument2 pagesTube Collection GuidePrincess JanNo ratings yet
- Time: 1 Hr. 30 Min. Total Marks: 60: Important InformationDocument9 pagesTime: 1 Hr. 30 Min. Total Marks: 60: Important Informationrishab KumarNo ratings yet