Professional Documents
Culture Documents
1
Uploaded by
Hanii HunnCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
1
Uploaded by
Hanii HunnCopyright:
Available Formats
Research
Original Investigation | CLINICAL SCIENCES
Microphthalmia, Anophthalmia, and Coloboma and
Associated Ocular and Systemic Features
Understanding the Spectrum
Simon E. Skalicky, MPhil; Andrew J. R. White, FRANZCO; John R. Grigg, FRANZCO; Frank Martin, FRANZCO;
Jeremy Smith, FRANZCO; Michael Jones, FRANZCO; Craig Donaldson, FRANZCO; James E. H. Smith, FRANZCO;
Maree Flaherty, FRANZCO; Robyn V. Jamieson, FRACP
IMPORTANCE Microphthalmia, anophthalmia, and coloboma form an interrelated spectrum of
congenital eye abnormalities.
OBJECTIVE To document the ocular and systemic findings and inheritance patterns in
patients with microphthalmia, anophthalmia, and coloboma disease to gain insight into the
underlying developmental etiologies.
DESIGN, SETTING, AND PARTICIPANTS This retrospective consecutive case series was
conducted at a tertiary referral center. Included in the study were 141 patients with
microphthalmia, anophthalmia, and coloboma disease without a recognized syndromic
etiology who attended the Westmead Childrens Hospital, Sydney, from 1981-2012.
EXPOSURE Cases were grouped on the basis of the presence or absence of an optic fissure
closure defect (OFCD); those with OFCD were further subdivided into microphthalmic and
nonmicrophthalmic cases. Anophthalmic cases were considered as a separate group.
MAIN OUTCOMES AND MEASURES Associated ocular and systemic abnormalities and
inheritance patterns were assessed.
RESULTS Of 141 cases, 61 (43%) were microphthalmic non-OFCD (NOFCD), 34 (24%)
microphthalmic OFCD, 32 (23%) nonmicrophthalmic coloboma (OFCD), 9 (6%)
anophthalmic, and 5 (4%) were unclassified. Sixty-three (45%) had bilateral disease.
Eighty-four patients (60%) had an associated ocular abnormality; of these, cataract
(P < .001) and posterior segment anomalies (P < .001) were most common in the NOFCD
group. Forty-eight (34%) had an associated systemic abnormality, most commonly
neurological, musculoskeletal and facial, urological and genital, or cardiac. Neurological
abnormalities were most common in the anophthalmic group (P = .003), while urological
abnormalities were particularly seen in the OFCD groups (P = .009). Familial cases were
identified in both the OFCD and NOFCD groups, with a likely autosomal dominant inheritance
pattern in 9 of 10 families.
CONCLUSIONS AND RELEVANCE This series indicated that the OFCD/NOFCD distinction may
be useful in guiding evaluation for ocular and systemic associations, as well as the direction
and analysis of genetic investigation.
Author Affiliations: Author
affiliations are listed at the end of this
article.
Corresponding Author: Robyn V.
Jamieson, FRACP, Eye and
Developmental Genetics Research
Group, Western Sydney Genetics
Program, The Childrens Hospital at
Westmead, Sydney, New South
JAMA Ophthalmol. 2013;131(12):1517-1524. doi:10.1001/jamaophthalmol.2013.5305 Wales, Australia 2145 (rjamieson
Published online October 31, 2013. @cmri.org.au).
1517
Copyright 2013 American Medical Association. All rights reserved.
Downloaded From: on 11/05/2017
Research Original Investigation Microphthalmia, Anophthalmia, and Coloboma
M
icrophthalmia, anophthalmia, and coloboma (MAC) this classification system was applied to a cohort of patients
are related structural, congenital eye malforma- with MAC to determine the proportions of patients that may
tions that display a spectrum of severity and can oc- fall into these groupings and the associated ocular and sys-
cur in isolation or as part of a syndrome.1-3 They account for a temic features. Cases without a known genetic or syndromic
significant proportion of childhood visual impairment etiology were primarily investigated to determine pheno-
worldwide.4 Anophthalmia is the complete absence of the eye. typic and inheritance patterns. With the advent of broadly tar-
Microphthalmia is a small eye most usefully defined in terms geted next-generation and whole-genome approaches in ge-
of axial length and corneal diameter. The optic fissure clo- netic diagnosis,35,41,42 clear phenotypic characterization will
sure defect (OFCD) of coloboma is a segmental ocular defect, be critical to determine the likelihood that particular molecu-
affecting some or all of the iris, choroid, retina, and optic lar variations are disease causing. This clinical knowledge will
nerve.5,6 Microphthalmia may also be found in association with be useful in directing investigations for possible associated sys-
congenital cataracts, or when there is disruption of normal an- temic features and for genetic information for affected fami-
terior segment formation leading to abnormal irides, corneal lies.
opacification, and small abnormal lenses.1,7,8
Reported birth prevalence ranges from 0.6 to 4.2 per
100 000 births for anophthalmia4,9-15; 2 to 17 per 100 000 births
for microphthalmia4,9-16; and 2 to 14 per 100 000 births for
Methods
coloboma.4,5,10,11,15,17 In Australia, the incidence of MAC is ap- We performed a retrospective case report study of medical rec-
proximately 6 to 13 per 100 000 births.18 ords at the Childrens Hospital, Westmead, Sydney, Australia,
The genetic etiology of MAC spectrum disease is not well from between 1981 and 2012. Ethics approval was prospec-
understood. Clinical and experimental evidence increasingly tively granted by the Childrens Hospital, Westmead, re-
suggests a heterogenous genetic basis including a local dis- search ethics committee. Because data were collected retro-
ruption in eye development or as part of a more generalized spectively via a database, informed consent was not obtained
developmental anomaly.1,16,19,20 The early development of the from patients; all data collected were de-identified from hos-
eye is controlled by a complex network of diffusible signaling pital notes. Consecutive cases of microphthalmia, anophthal-
molecules, transcription factors, and downstream targets in- mia, and coloboma were obtained from the medical records.
cluding cell-cycle regulators, structural proteins, and adhe- Inpatient files, outpatient clinic files, and separate files from
sion factors.21-23 The molecular signals in early eye develop- the Department of Clinical Genetics at the Childrens Hospi-
ment interact in specific pathways, which may be tissue- and tal, Westmead, were identified via computer database. The
time-specific in their action. This complexity helps explain the search keywords were microphthalmia/microphthalmos, an-
overlapping clinical phenotypes and the underlying genetic ophthalmia/anophthalmos, nanophthalmia/nanophthal-
heterogeneity in these conditions.19 mos, coloboma, and anterior segment dysgenesis (including
In some cases, such as CHARGE (coloboma, heart de- sclerocornea).
fects, choanal atresia, retarded growth and development, geni- Cases irrelevant to the study, including Axenfield-Rieger
tal abnormalities, and ear anomalies) syndrome24 or anoph- spectrum anomalies, Peters anomaly, aniridia, retinopathy of
thalmia associated with pulmonary hypoplasia,25 syndrome prematurity, and Morning Glory anomaly, were excluded. Cases
identification or the presence of a chromosomal anomaly or with a recognized syndrome associated with MAC, such as
microdeletion may guide investigations. However, for most pa- CHARGE, oculo-auriculo-vertebral spectrum disease, or Jou-
tients, no syndrome or chromosomal anomaly is detected. In bert syndrome, were excluded.
these cases, molecular diagnosis can be especially challeng- All cases were reviewed by a senior pediatric ophthalmolo-
ing because many genes have been identified that are indi- gist as were first-degree relatives, when possible. The embryo-
vidually responsible for a small number of cases. Currently, the logical classification proposed by Morrison et al16 was ex-
2 most frequently mutated genes known to cause monogenic tended as follows: cases were grouped into microphthalmia
MAC are SOX2 and OTX2, accounting for 10% and 3% of cases, with OFCD, microphthalmia without OFCD (NOFCD), microph-
respectively, when anophthalmia or severe microphthalmia is thalmia unclassified, coloboma isolated in 1 or both eyes (OFCD
present.19,26-31 Mutations in VSX2 (CHX10),32 PAX6,33 RAX,34 with normal axial length), and anophthalmia in 1 or both eyes,
FOXE3,35 BMP4,36 and GDF631 are less commonly detected. Fa- in keeping with similar studies. Coloboma was defined as a pre-
milial clustering and successful linkage analysis in a small num- dominantly inferior deficiency of iris, chorioretinal, or optic
ber of families have demonstrated segregation in autosomal disc tissue. An iris coloboma was a full-thickness iris defect or
recessive37 or autosomal dominant38 patterns. X-linked reces- anterior stromal deficiency, a chorioretinal coloboma was an
sive or dominant inheritance is associated with some syn- area of absent chorioretinal tissue that may or may not ex-
dromic forms of MAC.39,40 Many patients are the first af- tend continuously or discontinuously to the optic disc, and an
fected individual in their family and this, in combination with optic disc coloboma was a focally enlarged optic disc with de-
the lack of availability of a route to clear-cut genetic diagno- ficiency of neuroretinal tissue.5 Microphthalmia was defined
sis, hampers informative recurrence risk counseling. as an abnormally small eye or cornea (microcornea) (axial
A classification system based on embryological develop- length <16 mm at birth and <19 mm at 12 months of age; and
ment of the eye may be useful. Morrison et al16 classified MAC corneal diameter <10 mm at birth).15 Anophthalmia was de-
based on the presence or absence of an OFCD. In this study, fined as no evidence of a globe or ocular tissue in the orbit on
1518 JAMA Ophthalmology December 2013 Volume 131, Number 12 jamaophthalmology.com
Copyright 2013 American Medical Association. All rights reserved.
Downloaded From: on 11/05/2017
Microphthalmia, Anophthalmia, and Coloboma Original Investigation Research
clinical examination since birth.15,16 Cases were deemed un-
Table 1. Patient Characteristics and Treatment Data
classifiable if the presence or absence of an OFCD was unable
to be ascertained; for example, if there was an opaque cornea Characteristic Patients, No. (%)
or indeterminate on ultrasonography. Age at diagnosis, median (range), mo 11.0 (0-72)
Cases were further assessed on the basis of the presence Better-eye visual acuity, mean (range), LogMAR 0.88 (0.2 to 4)
or absence of the following features: congenital cataract, an- Sex
terior or posterior segment morphological abnormality, glau- Male 73 (52)
coma, persistent fetal vasculature (PFV), orbital or nasolacri- Female 68 (48)
mal duct abnormality, ocular motility disorder, and systemic Laterality
abnormalities. Anterior segment abnormality included sclero- Unilateral 78 (55)
cornea (defined as a congenital nonprogressive, noninflamma- Bilateral 63 (45)
tory scleralization of the peripheral and sometimes entire cor- MAC group
nea, without underlying iris or angle abnormality or iridocorneal Anophthalmia 9 (6)
adhesion), abnormal iris (excluding iris coloboma), and disor- Microphthalmic NOFCD 61 (43)
ganized angle. Posterior segment abnormality included cho- Microphthalmic OFCD 34 (24)
rioretinal or optic disc abnormalities (excluding PFV and cho- Nonmicrophthalmic OFCD 32 (23)
rioretinal and/or optic nerve coloboma); examples included Microphthalmic unclassified 5 (4)
vascular abnormality, chorioretinal atrophy, and hypoplastic
Ocular anomaly
and dysplastic optic discs. Visual acuity data were converted
Anterior segment abnormality 21 (15)
into logarithm of the minimal angle of resolution; the visual acu-
Cataract 45 (32)
ity of the better eye was recorded for each patient.
PFV 16 (11)
A detailed systemic clinical evaluation was performed on
Posterior segment abnormality, non-PFV 19 (13)
all patients by a senior pediatrician; further investigation for
Orbital or nasolacrimal abnormality 7 (5)
systemic abnormality was determined by clinical findings.
Oculomotility disorder 38 (27)
Significance testing was performed using the 2 Fisher ex-
Total 84 (59)
act probability test and analysis of variance across groups. Pedi-
gree analysis was performed to study the pattern of inheri- Nil 57 (41)
tance. Systemic abnormality
Neurological 22 (16)
Musculoskeletal 16 (11)
Cardiac 9 (6)
Results Urological 13 (9)
Case Selection Integumentary 7 (5)
A total of 182 case files were examined, of which 41 were ex- Other systemic abnormality 5 (4)
cluded from the study because they did not have MAC spec- Total 48 (34)
trum disease. Of those excluded, 19 were anophthalmic sec- Nil 93 (66)
ondary to enucleation due to an unrelated cause such as Ocular surgery
retinoblastoma. A further 22 cases were excluded because they Bilateral lensectomy 16
had either a documented congenital infection (3 cases) or a rec- Unilateral lensectomy 13
ognized genetic syndrome (19 cases: 7 with CHARGE syn- Intraocular lens insertion 18
drome, 2 with oculo-auriculo-vertebral spectrum disease, and Pupilloplasty 3
1 each of Aicardi Syndrome, Gorlin Syndrome, Jacobsen Syn-
Glaucoma surgery 8
drome, Nance-Horan Syndrome, Rubenstein-Taybi Syn-
Strabismus surgery 3
drome, Waardenburg Syndrome, Norrie Disease, Down Syn-
Orbital and eyelid surgery 6
drome, Velocardiofacial Syndrome, and Joubert Syndrome),
Enucleation 1
leaving 141 cases in the study. Based on Australian Institute
Total 38 (27)
of Health and Welfare data,18 approximately 235 live births with
Nil 103 (73)
MAC would be expected in New South Wales during the study
period, indicating a 60% capture rate of all New South Wales Abbreviations: MAC, microphthalmia, anophthalmia, and coloboma; NOFCD,
nonoptic fissure closure defect; OFCD, optic fissure closure defect; PFV,
cases in this study.
persistent fetal vasculature.
Descriptive Data
Most cases were detected in the first 18 months of life, with microphthalmic NOFCD and 66 cases with OFCD, in whom 34
the median age at presentation being 11 months (Table 1). The (24%) had an eye size meeting the definition for microphthal-
mean better-eye visual acuity corresponded to Snellen 6/45 mia and 32 (23%) where the eye size did not meet the microph-
(range, 6/4.5 to no light perception). The sex distribution was thalmia definition. In 5 cases, the presence or absence of an
broadly equal, with 73 males and 68 females. There were 63 OFCD could not be determined. Nine patients had anophthal-
bilateral and 78 unilateral cases. There were 61 cases (43%) with mia; this was bilateral in 7 cases. In the 2 patients with unilat-
jamaophthalmology.com JAMA Ophthalmology December 2013 Volume 131, Number 12 1519
Copyright 2013 American Medical Association. All rights reserved.
Downloaded From: on 11/05/2017
Research Original Investigation Microphthalmia, Anophthalmia, and Coloboma
Table 2. Relative Prevalence of Associated Ocular Abnormalities Within MAC Subgroups
No. (%)
Microphthalmic Nonmicrophthalmic
NOFCD OFCD Unclassified OFCD
Ocular Abnormality (n = 61) (n = 34) (n = 5) (n = 32) P Value
Anterior segment 11 (18) 7 (21) 1 (20) 2 (6) NS
Cataract 37 (61) 7 (21) 0 (0) 1 (3) <.001
Abbreviations: MAC, microphthalmia,
Posterior segment 27 (44)a 6 (18) 1 (20) 1 (3) <.001
anophthalmia, and coloboma;
Glaucoma 10 (16) 1 (3) 1 (20) 1 (3) NS NOFCD, nonoptic fissure closure
Orbital/nasolacrimal duct 3 (5) 2 (6) 1 (20) 1 (3) NS defect; NS, not significant; OFCD,
optic fissure closure defect.
Ocular motility 23 (38) 10 (30) 2 (40) 3 (9) .04
a
Including 16 cases with persistent
Any ocular abnormality 53 (87) 20 (59) 4 (80) 7 (22) <.001
fetal vasculature.
eral anophthalmia, the other eye had an OFCD in one patient Sibling Recurrence
and there was an NOFCD in the other eye in the other patient. Microphthalmia, anophthalmia, and coloboma disease was re-
Eighty-four patients (60%) had an associated ocular abnor- corded in 23 individuals from 10 families in our cohort. Expres-
mality in their involved eye(s); 48 (34%) had an associated sys- sion within families remained consistently either NOFCD or
temic abnormality. Thirty-eight individuals received surgical OFCD; however, within families, some individuals were mi-
intervention, the most common procedure being a lensec- crophthalmic and others had normal ocular size. This indi-
tomy. cates variable phenotypic expression of the genetic defect. Six
of the families had NOFCD, with cataracts and microphthal-
MAC Subgroup Analysis mia running in an autosomal dominant inheritance pattern. Off-
There were no differences between MAC subgroups in terms spring in 1 of these families had associated features of iridocor-
of bilaterality; however, on subgroup analysis of the NOFCD neal adhesions and sclerocornea. Four of the familial cases had
group, microphthalmic eyes with PFV had fewer bilaterally af- OFCD and these followed an autosomal dominant inheritance
fected cases (P < .007). Table 2 demonstrates the distribution pattern in 3 cases. In the other OFCD family, nonconsanguine-
of associated ocular abnormalities within the subgroups. As- ous unaffected parents had 2 affected children, 1 female and 1
sociated ocular abnormalities were most common in the male. This may be owing to autosomal recessive inheritance or
NOFCD (53 of 61) and microphthalmic OFCD (20 of 34) groups, to germline mosaicism with or without somatic mosaicism in 1
and they were less common in the nonmicrophthalmic OFCD of the phenotypically unaffected parents.
group (7 of 32) (P < .001). The most common abnormality was
congenital cataract (45 of 141), which was the most fre-
quently associated ocular anomaly in the NOFCD group (37 of
61). However, it was also present in some cases in both the mi-
Discussion
crophthalmic (7 of 34) and nonmicrophthalmic (1 of 32) OFCD There have been a variety of classification systems for MAC
groups, indicating some overlap in phenotypic features be- spectrum disorders43,44 but, to our knowledge, few have at-
tween the groups. Other associated ocular features in the tempted to classify the phenotypic features based on embry-
NOFCD group were posterior segment anomalies (27 of 61), in- ology and possible genetic etiology.16 The early embryology
cluding persistent fetal vasculature, and anterior segment ab- of the eye includes several important events (optic vesicle for-
normalities, such as opacifications of the cornea in 11 of 61 pa- mation, optic cup formation, and optic fissure closure), which
tients. Ocular motility disorders were least prevalent in the provide points for consideration of the responsible molecu-
nonmicrophthalmic coloboma (OFCD) group (P = .04). lar signals, pathways, and genetic coordinators.3,21-23 From a
An associated systemic abnormality was identified in 34% clinical perspective, the microphthalmic NOFCD group may
of cases. The frequency and type of systemic abnormality did represent either a very severe phenotype suggesting disrup-
not vary between unilateral and bilateral cases. The distribu- tion at the optic vesicle or optic cup stage or, if mild, then in-
tion of systemic abnormalities found in our cohort is shown in terruption to differentiation and maturation. The presence of
Table 3, and several patients had more than 1 associated sys- OFCD implies disruption to events around the time of optic fis-
temic feature. The most common abnormalities were neuro- sure closure. There has been some epidemiological evidence
logical, musculoskeletal and facial, and urological and genital. for subclassifying MAC spectrum disorders according to the
Neurological abnormality was most common in the anophthal- presence or absence of a coloboma.9
mic subgroup (5 of 9) and least in the nonmicrophthalmic OFCD There have been recent advances in our understanding of
group (1 of 32) (P = .003). Urological and genital abnormality was the genetic etiology of microphthalmia and anophthalmia spec-
most common in the microphthalmic (5 of 34) and nonmicroph- trum disorders largely through family studies,25,26,32 and clini-
thalmic (7 of 32) OFCD groups and least common in the anoph- cal molecular testing for some candidate genes is now
thalmic group (0 of 9) (P = .009). Cardiac abnormality was not available.19,27,28,30,33,35,45 Because microphthalmia and anoph-
detected in the NOFCD group (0 of 61) and was present in all thalmia spectrum has a heterogenous genetic etiology with a
other groups in small numbers (P = .04). variety of phenotypic expressions, specific candidate genes for
1520 JAMA Ophthalmology December 2013 Volume 131, Number 12 jamaophthalmology.com
Copyright 2013 American Medical Association. All rights reserved.
Downloaded From: on 11/05/2017
Microphthalmia, Anophthalmia, and Coloboma Original Investigation Research
Table 3. Relative Prevalence of Associated Systemic Abnormalities Within MAC Subgroups
No. (%)
Microphthalmic Nonmicrophthalmic
Systemic Anophthalmia NOFCD OFCD Unclassified (OFCD) P
Abnormality (n = 9) (n = 61) (n = 34) (n = 5) (n = 32) Value
Neurological 5 (56): Hypoplastic optic 8 (13): Sensorineural hear- 7 (21): Sensorineural 1 (20): 1 (3): Absent cerebellar .003
nerves and tracts; ing loss and atrophic optic hearing loss; hydrocephalus; Cerebral vermis and expressive
septooptic chiasm; sensorineural basal encephalocele, corpus palsy dysphasia
dysplasia; occipital hearing loss; callosum agenesis; absent
encephalocele; bilateral sensorineural septum pellucidum with
frontal encephalocele; hearing impairment; dilated lateral ventricles,
bilateral sensorineural congential right cerebral hydrocephalus, and atrophic
hearing loss and hypoplasia, bifid corpus callosum; occult
absent septum pituitary, and small spina bifida; involuntary arm
pellucidum corpus callosum; severe movements; epilepsy
developmental delay;
hypotonia; hydrocephalus;
midline hypothalamus and
optic chiasm anomaly
Musculoskeletal 1 (11): Absent right ear, 5 (8): Short palpebral 8 (24): Facial 0 (0) 2 (6): Fused C2-3, .13
and facial cleft lip, and palate fissures, microcephalus, dysmorphology, down postaxial polydactyly
wide nasal bridge, small slating palpebral fissures, both upper limbs and left
posteriorly rotated ears and wide nasal bridge, short lower limb; cleft palate,
syndactyly of toes 2-3; nose, micrognathia, rotated hyperflexible thumb
limb overgrowth; ears, and nuchal thickening; joints, Klippel-Fiel
polydactyly; abnormal bilateral 5th finger anomaly C2-C4, high
dentition, right facial clinodactyly and override nasal bridge, protuberant
microsomia, malar toes 2-3; snub nose, low set lower lip, pectus
hypoplasia, small jaw, ears, cleft palate, redundant excavatum, malar
redundant upper eyelids, neck folds, micrognathia, hypoplasia and long feet
downsloping palpebral syndactyly of toes 2-3; right
fissures, fused C2-3, webbed toes, right
scoliosis, and nasal anomalous pinna;
deformity; 11 ribs hypoplastic left femur;
bilaterally, sacral bilateral limb anomalies,
hemivertebrae, exomphalos; bilateral
tracheo-esophageal inguinal hernias; cleft palate
fistula, low rotated ears,
flat facies, fused eyelids
Cardiac 1 (11): Hemitruncus 0 (0) 5 (15): Ventricular septal 1 (20): 2 (6): Subaortic stenosis; .04
arteriosum, defect; patent ductus Tetralogy ventricular septal defect
ventricular septal arteriosus; pulmonary of Fallot
defect, and pulmonary atresia, ventricular septal
hypertension defect, atrial septal defect;
ventricular septal defect,
atrial septal defect, patent
ductus arteriosus; atrial-
ventricular septal defect
Urological and 0 (0) 1 (2): Hydrocele 5 (15): Anterior anus and 1 (20): 7 (22): Undescended .009
genital hypoplastic labia majora; Congenital left testes; severe
vesicoureteric reflux; renal testicular vesicoureteric reflux;
pelvic dilatation; micropenis torsion medullary sponge
and absent scrotum; neuro- kidneys; single kidney;
genic bladder and renal cryptorchidism;
reflux dysplastic kidney;
bladder abnormalities,
dysplastic kidneys
Integumentary 1 (11): Linear 2 (3): Hypopigmented skin 1 (3): Caf au lait spot on 0 (0) 1 (3): Dry skin, sparse .56
scleroderma patches; hirsutism left shoulder hair
Other systemic 0 (0) 3 (5): Reduced growth 0 (0) 0 (0) 4 (12): Inguinal hernia; .60
abnormality hormone; congenital 2-vessel umbilicus with
cystic adenoid hernia; plagiocephaly;
malformation of lung type hepatosplenomegaly
II and duodenal atresia;
obstructive sleep apnea
Total 6 (67) 15 (25) 13 (38) 2 (40) 12 (38) .13
Abbreviations: MAC, microphthalmia, anophthalmia, and coloboma; NOFCD, nonoptic fissure closure defect; OFCD, optic fissure closure defect.
microphthalmia and anophthalmia can only be isolated in a The Australian prevalence of MAC is comparable with other
minority of cases.16,19 In the near future, whole-exome se- countries: 1 to 17 per 100 000 births for microphthalmia,4,9-18,47,48
quencing, with interpretation guided by an understanding of with variability largely based on different inclusion/exclusion
the overlapping roles of developmental genes in OFCD and criteria.4,9-11,13,14,16,17 The sex distribution of our cases was ap-
NOFCD, will lead to increased yield in diagnostic testing in proximately equal, in keeping with other studies.13-15 It is pos-
these conditions (Figure). This is likely to significantly en- sible that these were the more severe cases in this spectrum of
hance our understanding of the genetic etiology of these disorders or they may have had concomitant problems leading
disorders.46 to a referral for management.
jamaophthalmology.com JAMA Ophthalmology December 2013 Volume 131, Number 12 1521
Copyright 2013 American Medical Association. All rights reserved.
Downloaded From: on 11/05/2017
Research Original Investigation Microphthalmia, Anophthalmia, and Coloboma
possible nonsyndromic systemic associations, this cohort may
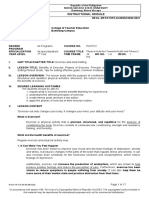
Figure. Disease Genes in Patients With Optic Fissure Closure Defect
(OFCD) and Nonoptic Fissure Closure Defect (NOFCD) Phenotypes
reflect a reduced incidence of systemic abnormalities associ-
ated with MAC.
In this series, most pedigrees had an autosomal domi-
nant inheritance pattern. However, most cases did not have a
Optic fissure Nonoptic fissure
closure defect closure defect known family history. Sibling recurrence is a significant risk
SOX2/SOX2 and must be explained to affected families. In this series, there
BMP4/BMP4
PAX6/PAX6 FOXE3 were familial cases in both the NOFCD (6 families) and OFCD
SHH/SHH OTX2 PITX3 (4 families) groups. There was marked variability within some
STRA6/STRA6 VSX2 NHS/NHS
GDF6/GDF6 ATOH7 GJA1 families. For example, there was 1 family where a father had
CHD7 RAX BCOR coloboma with normal size eyes, while his child had colo-
NDP HCCS
SMOC1 boma and microphthalmia. Three NOFCD families had indi-
viduals with microphthalmia and cataracts, whose relatives
(typically earlier generations) had pediatric cataract with nor-
mal globe size.
Persistent fetal vasculature, traditionally considered a sepa-
Mutations in some genes are specifically seen in patients with OFCD or NOFCD.
Some patients with OFCD can have associated NOFCD features, such as rate clinical entity,54,55 has been included as a subset of NOFCD
cataract and anterior or posterior segment abnormality, and at least 9 of the within this cohort. With increasing identification of causative
genes (eg, SOX2, BMP4, and PAX6) can be mutated in patients with OFCD, genes, there may be an etiological overlap between PFV and
NOFCD, or OFCD with associated ocular defects. For genes in bold, there may
other noncolobomatous cases of microphthalmia.56 When com-
be systemic features in patients with mutations in at least 13 genes, and a
mutation in these genes causes a syndromic ocular condition. For genes not in pared with non-PFV cases in the NOFCD group, those with PFV
bold, a mutation causes isolated ocular abnormality. For all genes, a mutation had similar frequencies of systemic and ocular abnormalities;
may cause isolated ocular abnormality or ocular and systemic abnormality. however, there was a higher prevalence of unilateral cases.
Five of the cases classified as microphthalmic on the basis
Epidemiological studies have suggested that cataract is of- of small corneal diameters were subsequently shown to have
ten found in association with microphthalmia.8,49 Our finding normal axial lengths when this was measured in later child-
that cataract was the most frequently associated eye abnormal- hood. Each of these cases had associated bilateral congenital
ity in the NOFCD cohort (Table 2) and can be found in relatives cataracts and had developed glaucoma or had an affected fam-
of patients with NOFCD is consistent with these reports. There ily member with congenital cataract and microphthalmia. These
have been previous instances of pedigrees with this pairing of cases represent a distinct clinical subset that requires recogni-
eye abnormalities.50 Anterior segment anomalies were more tion by the pediatric ophthalmologist and geneticist. Patients
common in the microphthalmic OFCD group than the nonmi- with the phenotype of cataract and microcornea, with or with-
crophthamic OFCD group. This may reflect an increased inci- out reduction in axial length, may have mutations in cataract-
dence of corneal abnormality and anterior segment disorgani- related genes such as GJA8, GJA3, CRYBA4, and CRYGC.57,58
zation in microphthalmic eyes. Glaucoma (an important This study provided useful clues for clinicians and geneti-
comorbidity) affected a small number of patients in all groups. cists involved in the management of these patients. First, the
Ocular motility abnormalities were present in all microphthal- phenotypic expression of MAC spectrum abnormalities is vari-
mic groups, consistent with a higher incidence of poor vision able (even within families) and a significant proportion of the
in microphthalmic eyes and subsequent sensory tropia. patient population has associated eye and systemic abnormali-
Similar to previous studies,9,16,49,51,52 a large proportion of ties and careful examination must be made for these. Some of
our cases (34%) had an associated systemic abnormality, most these, such as NOFCD with cataract and OFCD with urological
commonly neurological, musculoskeletal and facial, or uro- abnormalities, cluster together and this serves as an aid to the
logical and genital. Neurological abnormality was relatively clinician in recognizing these associations. While the inheri-
more common in the anophthalmic group followed by the mi- tance pattern is complex and incompletely understood, it is clear
crophthalmic OFCD and NOFCD groups (Table 3). This is in that cases of bilateral MAC abnormalities and those NOFCD cases
keeping with previous studies where neurological abnormal- with cataract may be particularly associated with a familial pat-
ity, especially midline anomalies, have been found, particu- tern of inheritance. Expression of MAC spectrum disorders is
larly when the eyes are more severely affected.33,53 Optic not uniform, so the clinical delineation of phenotypic features
fissure closure defect cases, both microphthalmic and non- is important to aid interpretation of exome and whole-
microphthalmic, showed an increased predisposition to uro- genome data in these patients as this becomes increasingly avail-
logical abnormalities compared with NOFCD cases. By exclud- able. This will lead to improved prospects for genetic diagno-
ing cases with known syndromic etiology to provide clues to sis and information for these patients and families.
ARTICLE INFORMATION Published Online: October 31, 2013. Eye and Developmental Genetics Research Group,
Submitted for Publication: February 28, 2013; doi:10.1001/jamaophthalmol.2013.5305. Western Sydney Genetics Program, The Childrens
final revision received May 9, 2013; accepted May Author Affiliations: Discipline of Ophthalmology, Hospital at Westmead, Sydney, New South Wales,
17, 2013. University of Sydney, New South Wales, Australia Australia (White, Grigg, Flaherty, Jamieson);
(Skalicky, White, Grigg, Martin, Jones, Jamieson); Department of Ophthalmology, The Childrens
1522 JAMA Ophthalmology December 2013 Volume 131, Number 12 jamaophthalmology.com
Copyright 2013 American Medical Association. All rights reserved.
Downloaded From: on 11/05/2017
Microphthalmia, Anophthalmia, and Coloboma Original Investigation Research
Hospital at Westmead, Sydney, New South Wales, epidemiologic study in about one million newborns 27. Fantes J, Ragge NK, Lynch S-A, et al. Mutations
Australia (Skalicky, White, Grigg, Martin, J. Smith, in Italy. Birth Defects Orig Artic Ser. in SOX2 cause anophthalmia. Nat Genet.
Jones, Donaldson, J.E. Smith, Flaherty); Childrens 1996;30(1):413-424. 2003;33(4):461-463.
Medical Research Institute, Westmead, Sydney, 11. Stoll C, Alembik Y, Dott B, Roth MP. Congenital 28. Ragge NK, Brown AG, Poloschek CM, et al.
New South Wales, Australia (Jamieson); Discipline eye malformations in 212,479 consecutive births. Heterozygous mutations of OTX2 cause severe
of Paediatrics and Child Health, University of Ann Genet. 1997;40(2):122-128. ocular malformations [erratum appears in Am J
Sydney, Sydney, New South Wales, Australia Hum Genet. 2005;77(2):334]. Am J Hum Genet.
(Jamieson). 12. Spagnolo A, Bianchi F, Calabro A, et al.
Anophthalmia and benomyl in Italy: a multicenter 2005;76(6):1008-1022.
Author Contributions: Dr Jamieson had full access study based on 940,615 newborns. Reprod Toxicol. 29. Schneider A, Bardakjian T, Reis LM, Tyler RC,
to all of the data in the study and takes 1994;8(5):397-403. Semina EV. Novel SOX2 mutations and
responsibility for the integrity of the data and the genotype-phenotype correlation in anophthalmia
accuracy of the data analysis. 13. Klln B, Tornqvist K. The epidemiology of
anophthalmia and microphthalmia in Sweden. Eur J and microphthalmia. Am J Med Genet A.
Study concept and design: Skalicky, White, Grigg, 2009;149A(12):2706-2715.
Jamieson. Epidemiol. 2005;20(4):345-350.
Acquisition of data: Skalicky, White, Martin, 14. Shaw GM, Carmichael SL, Yang W, Harris JA, 30. Schilter KF, Schneider A, Bardakjian T, et al.
Donaldson, J. E. H. Smith, Flaherty. Finnell RH, Lammer EJ. Epidemiologic OTX2 microphthalmia syndrome: four novel
Analysis and interpretation of data: Skalicky, White, characteristics of anophthalmia and bilateral mutations and delineation of a phenotype. Clin
J. Smith, Jones, Jamieson. microphthalmia among 2.5 million births in Genet. 2011;79(2):158-168.
Drafting of the manuscript: Skalicky, Grigg, California, 1989-1997. Am J Med Genet A. 31. Gonzalez-Rodriguez J, Pelcastre EL,
Jamieson. 2005;137(1):36-40. Tovilla-Canales JL, et al. Mutational screening of
Critical revision of the manuscript for important 15. Shah SP, Taylor AE, Sowden JC, et al; CHX10, GDF6, OTX2, RAX and SOX2 genes in 50
intellectual content: Skalicky, White, Martin, J. Surveillance of Eye Anomalies (SEA-UK) Special unrelated microphthalmia-anophthalmia-coloboma
Smith, Jones, Donaldson, J. E. H. Smith, Flaherty, Interest Group. Anophthalmos, microphthalmos, (MAC) spectrum cases. Br J Ophthalmol.
Jamieson. and typical coloboma in the United Kingdom: a 2010;94(8):1100-1104.
Statistical analysis: Skalicky, Grigg. prospective study of incidence and risk. Invest 32. Ferda Percin E, Ploder LA, Yu JJ, et al. Human
Obtained funding: Grigg. Ophthalmol Vis Sci. 2011;52(1):558-564. microphthalmia associated with mutations in the
Administrative, technical, or material support: retinal homeobox gene CHX10. Nat Genet.
Skalicky, Grigg, Donaldson. 16. Morrison D, FitzPatrick D, Hanson I, et al.
National study of microphthalmia, anophthalmia, 2000;25(4):397-401.
Study supervision: Grigg, Martin, Jones, Donaldson,
J. E. H. Smith, Jamieson. and coloboma (MAC) in Scotland: investigation of 33. Glaser T, Jepeal L, Edwards JG, Young SR, Favor
genetic aetiology. J Med Genet. 2002;39(1):16-22. J, Maas RL. PAX6 gene dosage effect in a family
Conflict of Interest Disclosures: None reported. with congenital cataracts, aniridia, anophthalmia
17. Vogt G, Szunyogh M, Czeizel AE. Birth
Additional Contributions: We acknowledge the characteristics of different ocular congenital and central nervous system defects. Nat Genet.
contribution of Stephen Hing, FRANZCO, and Neil abnormalities in hungary. Ophthalmic Epidemiol. 1994;7(4):463-471.
Rowe, FRANZCO, in the management of many 2006;13(3):159-166. 34. Voronina VA, Kozhemyakina EA, OKernick CM,
patients in this series. et al. Mutations in the human RAX homeobox gene
18. Australian Institute of Health and Welfare. Eye
Health Among Australian Children. Canberra, in a patient with anophthalmia and sclerocornea.
REFERENCES Hum Mol Genet. 2004;13(3):315-322.
Australia: Australian Institute of Health and Welfare;
1. Verma AS, Fitzpatrick DR. Anophthalmia and 2008. 35. Jimenez NL, Flannick J, Yahyavi M, et al.
microphthalmia. Orphanet J Rare Dis. 2007;2:47. Targeted next-generation sequencing in
19. Bardakjian TM, Schneider A. The genetics of
2. Ragge NK, Subak-Sharpe ID, Collin JRO. A anophthalmia and microphthalmia. Curr Opin anophthalmia and microphthalmia patients
practical guide to the management of anophthalmia Ophthalmol. 2011;22(5):309-313. confirms SOX2, OTX2 and FOXE3 mutations. BMC
and microphthalmia. Eye (Lond). 2007;21(10):1290- Med Genet. 2011;12:172.
1300. 20. Gregory-Evans CY, Williams MJ, Halford S,
Gregory-Evans K. Ocular coloboma: a reassessment 36. Bakrania P, Efthymiou M, Klein JC, et al.
3. Fitzpatrick DR, van Heyningen V. Developmental in the age of molecular neuroscience. J Med Genet. Mutations in BMP4 cause eye, brain, and digit
eye disorders. Curr Opin Genet Dev. 2004;41(12):881-891. developmental anomalies: overlap between the
2005;15(3):348-353. BMP4 and hedgehog signaling pathways. Am J Hum
21. Fuhrmann S. Eye morphogenesis and Genet. 2008;82(2):304-319.
4. Hornby SJ, Gilbert CE, Rahi JK, et al. Regional patterning of the optic vesicle. Curr Top Dev Biol.
variation in blindness in children due to 2010;93:61-84. 37. Bessant DA, Khaliq S, Hameed A, et al. A locus
microphthalmos, anophthalmos and coloboma. for autosomal recessive congenital microphthalmia
Ophthalmic Epidemiol. 2000;7(2):127-138. 22. Yun S, Saijoh Y, Hirokawa KE, et al. Lhx2 links maps to chromosome 14q32. Am J Hum Genet.
the intrinsic and extrinsic factors that control optic 1998;62(5):1113-1116.
5. Nakamura KM, Diehl NN, Mohney BG. Incidence, cup formation. Development. 2009;136(23):3895-
ocular findings, and systemic associations of ocular 3906. 38. Morl L, Bozon M, Zech J-C, et al. A locus for
coloboma: a population-based study. Arch autosomal dominant colobomatous
Ophthalmol. 2011;129(1):69-74. 23. Eiraku M, Takata N, Ishibashi H, et al. microphthalmia maps to chromosome 15q12-q15.
Self-organizing optic-cup morphogenesis in Am J Hum Genet. 2000;67(6):1592-1597.
6. Chang L, Blain D, Bertuzzi S, Brooks BP. Uveal three-dimensional culture. Nature.
coloboma: clinical and basic science update. Curr 2011;472(7341):51-56. 39. Ng D, Hadley DW, Tifft CJ, Biesecker LG.
Opin Ophthalmol. 2006;17(5):447-470. Genetic heterogeneity of syndromic X-linked
24. Vissers LELM, van Ravenswaaij CMA, Admiraal recessive microphthalmia-anophthalmia: is Lenz
7. Weiss AH, Kousseff BG, Ross EA, Longbottom J. R, et al. Mutations in a new member of the
Complex microphthalmos. Arch Ophthalmol. microphthalmia a single disorder? Am J Med Genet.
chromodomain gene family cause CHARGE 2002;110(4):308-314.
1989;107(11):1619-1624. syndrome. Nat Genet. 2004;36(9):955-957.
8. Nishina S, Kurosaka D, Nishida Y, Kondo H, 40. Happle R, Danils O, Koopman RJ. MIDAS
25. Ng WY, Pasutto F, Bardakjian TM, et al. A puzzle syndrome (microphthalmia, dermal aplasia, and
Kobayashi Y, Azuma N. Survey of microphthalmia in over several decades: eye anomalies with FRAS1
Japan. Jpn J Ophthalmol. 2012;56(3):198-202. sclerocornea): an X-linked phenotype distinct from
and STRA6 mutations in the same family. Clin Genet. Goltz syndrome. Am J Med Genet.
9. Bermejo E, Martnez-Fras M-L. Congenital eye 2013;83(2):162-168. 1993;47(5):710-713.
malformations: clinical-epidemiological analysis of 26. Mihelec M, Abraham P, Gibson K, et al. Novel
1,124,654 consecutive births in Spain. Am J Med 41. Tsurusaki YKY, Kobayashi Y, Hisano M, et al. The
SOX2 partner-factor domain mutation in a diagnostic utility of exome sequencing in Joubert
Genet. 1998;75(5):497-504. four-generation family. Eur J Hum Genet. syndrome and related disorders. J Hum Genet.
10. Clementi M, Tenconi R, Bianchi F, et al. 2009;17(11):1417-1422. 2013;58(2):113-115.
Congenital eye malformations: a descriptive
jamaophthalmology.com JAMA Ophthalmology December 2013 Volume 131, Number 12 1523
Copyright 2013 American Medical Association. All rights reserved.
Downloaded From: on 11/05/2017
Research Original Investigation Microphthalmia, Anophthalmia, and Coloboma
42. Neveling KCR, Collin RW, Gilissen C, et al. Congenital Anomalies Surveillance System [erratum comprising anophthalmia, pituitary hypoplasia, and
Next-generation genetic testing for retinitis appears in Can J Ophthalmol. 2006;41(2):232]. Can ear anomalies. Am J Med Genet A.
pigmentosa. Hum Mutat. 2012;33(6):963-972. J Ophthalmol. 2005;40(1):38-44. 2006;140(16):1711-1718.
43. Hornby SJ, Adolph S, Gilbert CE, Dandona L, 49. Shah SP, Taylor AE, Sowden JC, et al; 54. Shastry BS. Persistent hyperplastic primary
Foster A. Visual acuity in children with coloboma: Surveillance of Eye Anomalies Special Interest vitreous: congenital malformation of the eye. Clin
clinical features and a new phenotypic classification Group. Anophthalmos, microphthalmos, and Experiment Ophthalmol. 2009;37(9):884-890.
system. Ophthalmology. 2000;107(3):511-520. Coloboma in the United kingdom: clinical features, 55. Anteby I, Cohen E, Karshai I, BenEzra D.
44. Warburg M. Classification of microphthalmos results of investigations, and early management. Unilateral persistent hyperplastic primary vitreous:
and coloboma. J Med Genet. 1993;30(8):664-669. Ophthalmology. 2012;119(2):362-368. course and outcome. J AAPOS. 2002;6(2):92-99.
45. Casey J, Kawaguchi R, Morrissey M, et al. First 50. Billingsley G, Santhiya ST, Paterson AD, et al. 56. Pelcastre EL, Villanueva-Mendoza C, Zenteno
implication of STRA6 mutations in isolated CRYBA4, a novel human cataract gene, is also JC. Novel and recurrent NDP gene mutations in
anophthalmia, microphthalmia, and coloboma: involved in microphthalmia. Am J Hum Genet. familial cases of Norrie disease and X-linked
a new dimension to the STRA6 phenotype. Hum 2006;79(4):702-709. exudative vitreoretinopathy. Clin Experiment
Mutat. 2011;32(12):1417-1426. 51. Stoll C, Alembik Y, Dott B, Roth MP. Ophthalmol. 2010;38(4):367-374.
46. Priya RR, Rajasimha HK, Brooks MJ, Swaroop Epidemiology of congenital eye malformations in 57. Guo Y, Su D, Li Q, et al. A nonsense mutation of
A. Exome sequencing: capture and sequencing of 131,760 consecutive births. Ophthalmic Paediatr CRYGC associated with autosomal dominant
all human coding regions for disease gene Genet. 1992;13(3):179-186. congenital nuclear cataracts and microcornea in a
discovery. Methods Mol Biol. 2012;884:335-351. 52. Forrester MB, Merz RD. Descriptive Chinese pedigree. Mol Vis. 2012;18:1874-1880.
47. Dolk H, Busby A, Armstrong BG, Walls PH. epidemiology of anophthalmia and 58. Zhou G, Zhou N, Hu S, Zhao L, Zhang C, Qi Y. A
Geographical variation in anophthalmia and microphthalmia, Hawaii, 1986-2001. Birth Defects missense mutation in CRYBA4 associated with
microphthalmia in England, 1988-94. BMJ. Res A Clin Mol Teratol. 2006;76(3):187-192. congenital cataract and microcornea. Mol Vis.
1998;317(7163):905-909; discussion 910. 53. Nolen LD, Amor D, Haywood A, et al. Deletion 2010;16:1019-1024.
48. Lowry RB, Kohut R, Sibbald B, Rouleau J. at 14q22-23 indicates a contiguous gene syndrome
Anophthalmia and microphthalmia in the Alberta
1524 JAMA Ophthalmology December 2013 Volume 131, Number 12 jamaophthalmology.com
Copyright 2013 American Medical Association. All rights reserved.
Downloaded From: on 11/05/2017
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- 2020 HivDocument1 page2020 HivhenkNo ratings yet
- Subacute and Chronic MeningitisDocument8 pagesSubacute and Chronic MeningitisLucky PuspitasariNo ratings yet
- English For Academic and Professional Purposes (EAPP) : Quarter 1 - Module 3: SummarizingDocument31 pagesEnglish For Academic and Professional Purposes (EAPP) : Quarter 1 - Module 3: SummarizingJay L. Espino85% (85)
- DR Antonious CV N & AEDocument27 pagesDR Antonious CV N & AEdoctorantoniNo ratings yet
- Caring For Injured Reptiles2004Document40 pagesCaring For Injured Reptiles2004SujayJainNo ratings yet
- GI Bleeding in Patients Receiving Antiplatelets and Anticoagulant TherapyDocument11 pagesGI Bleeding in Patients Receiving Antiplatelets and Anticoagulant TherapyTony LeeNo ratings yet
- Campbell Chapter 43 NotesDocument13 pagesCampbell Chapter 43 NotesRyan LiuNo ratings yet
- MRCPCH q15Document30 pagesMRCPCH q15Galaleldin AliNo ratings yet
- Instructional Module: Republic of The Philippines Nueva Vizcaya State University Bambang, Nueva VizcayaDocument19 pagesInstructional Module: Republic of The Philippines Nueva Vizcaya State University Bambang, Nueva VizcayaCJ M. Pablo100% (1)
- CHAPTER 2 - Textbook ExerciseDocument8 pagesCHAPTER 2 - Textbook ExercisenoorNo ratings yet
- AP Bio Lab 3Document18 pagesAP Bio Lab 3zzmasterNo ratings yet
- Inferior Vena Cava and Its TributariesDocument12 pagesInferior Vena Cava and Its TributariesRahaf MajadlyNo ratings yet
- Spirituality, Spiritual Well-Being, and Spiritual Coping in Advanced Heart FailureDocument18 pagesSpirituality, Spiritual Well-Being, and Spiritual Coping in Advanced Heart FailurezakiaNo ratings yet
- Scheduling: IndiaDocument5 pagesScheduling: IndiaCristinaNo ratings yet
- OCTA InflammatoryEyediseaseSrivastavaDocument24 pagesOCTA InflammatoryEyediseaseSrivastavaPriyanka DocNo ratings yet
- GUMAMELA Nutritional Status Baseline 2018 2019Document1 pageGUMAMELA Nutritional Status Baseline 2018 2019Sheryll PortuguesNo ratings yet
- (Dental Discussion 1) - Hesy ReDocument32 pages(Dental Discussion 1) - Hesy ReethanNo ratings yet
- Anchor Speech On WorkshopDocument6 pagesAnchor Speech On WorkshopPabhat Kumar100% (2)
- Farmakologi Geriatri: Oleh: P. Santoso, S.Si.,M.Biomed, AptDocument40 pagesFarmakologi Geriatri: Oleh: P. Santoso, S.Si.,M.Biomed, AptEva Dharma WahyuniNo ratings yet
- Central Council of Indian Medicine New Delhi: Syllabus of Ayurvedacharya (Bams) CourseDocument22 pagesCentral Council of Indian Medicine New Delhi: Syllabus of Ayurvedacharya (Bams) CourseAnanya MenonNo ratings yet
- Feeding A Dairy CowDocument31 pagesFeeding A Dairy CowFrancis Onyango OduorNo ratings yet
- Domiciliary Midwifery RDocument16 pagesDomiciliary Midwifery Rswillymadhu83% (6)
- DS - Aseptoman® Plus - Pif - en - 1711Document2 pagesDS - Aseptoman® Plus - Pif - en - 1711Serbanica RazvanNo ratings yet
- CREW: Department of Veterans Affairs: Regarding PTSD Diagnosis: Quick Referenec To Laws and Regulatinos Relating To Psychiactric DisordersDocument30 pagesCREW: Department of Veterans Affairs: Regarding PTSD Diagnosis: Quick Referenec To Laws and Regulatinos Relating To Psychiactric DisordersCREWNo ratings yet
- Maintenance Fluid Therapy in ChildrenDocument4 pagesMaintenance Fluid Therapy in ChildrenNicole_0No ratings yet
- Systematic Review Pelaksanaan Programmatic Management of Drug-Resistant Tuberculosis Pada Pasien Tuberkulosis Resistan ObatDocument8 pagesSystematic Review Pelaksanaan Programmatic Management of Drug-Resistant Tuberculosis Pada Pasien Tuberkulosis Resistan ObatAdinda Pramesthi RiadyaniNo ratings yet
- 2 - Megaloblastic Anaemia EssayDocument2 pages2 - Megaloblastic Anaemia EssayLefteris ChatzidoukasNo ratings yet
- Scientific Book Jicccim 2018Document171 pagesScientific Book Jicccim 2018ngwinda90No ratings yet
- Postanesthetic Aldrete Recovery Score: Original Criteria Modified Criteria Point ValueDocument3 pagesPostanesthetic Aldrete Recovery Score: Original Criteria Modified Criteria Point ValueBonny ChristianNo ratings yet
- IAPHD Hand Book On Palliative Care PDFDocument37 pagesIAPHD Hand Book On Palliative Care PDFMohammed ArshadNo ratings yet