Professional Documents
Culture Documents
CCB Od
Uploaded by
harasthaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
CCB Od
Uploaded by
harasthaCopyright:
Available Formats
CCB OD 1
Section I: Scenario Demographics
Scenario Title: CCB OD
Date of Development: 24/05/2015 (DD/MM/YYYY)
Target Learning Group: Juniors (PGY 1 2) Seniors (PGY 3) All Groups
Section II: Scenario Developers
Scenario Developer(s): Kyla Caners
Affiliations/Institution(s): McMaster University
Contact E-mail (optional): kcaners@gmail.com
Section III: Curriculum Integration
Learning Goals & Objectives
Educational Goal: To expose learners to a multi-drug overdose and the management of a severe CCB
OD.
CRM Objectives: 1) Maintain calm leadership throughout complex case.
2) Demonstrate situational awareness as patient status changes
Medical Objectives: 1) Recognize a possible CCB overdose
2) Administer appropriate early treatments for a CCB overdose
3) Recognize hypercapneic respiratory failure and manage appropriately.
4) Consider intralipid as treatment in an arrested CCB overdose
Case Summary: Brief Summary of Case Progression and Major Events
A 48-year-old female presents with a possible multi-drug overdose including glyburide, clonazepam and
nifedipine. She will remain hypotensive throughout the case, despite treatment with calcium, high dose
insulin, and other vasopressors. She will also have progressive respiratory depression and will eventually
require intubation. She will then proceed to arrest. The team will be expected to give intralipid once the
patient has arrested.
References
Marx, J. A., Hockberger, R. S., Walls, R. M., & Adams, J. (2013). Rosen's emergency medicine: Concepts and clinical practice. St. Louis: Mosby.
2015 EMSIMCASES.COM Page 1
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
CCB OD 2
Section IV: Scenario Script
A. Scenario Cast & Realism
Patient: Computerized Mannequin Realism: Conceptual
Mannequin Physical
Standardized Patient Select most Emotional/Experiential
Hybrid important Other:
Task Trainer dimension(s) N/A
Confederates Brief Description of Role
Family Brings list of medications, describes patients mood.
member
B. Required Monitors
EKG Leads/Wires Temperature Probe Central Venous Line
NIBP Cuff Defibrillator Pads Capnography
Pulse Oximeter Arterial Line Other:
C. Required Equipment
Gloves Nasal Prongs Scalpel
Stethoscope Venturi Mask Tube Thoracostomy Kit
Defibrillator Non-Rebreather Mask Cricothyroidotomy Kit
IV Bags/Lines Bag Valve Mask Thoracotomy Kit
IV Push Medications Laryngoscope Central Line Kit
PO Tabs Video Assisted Laryngoscope Arterial Line Kit
Blood Products ET Tubes Other: intralipid
Intraosseous Set-up LMA Other:
D. Moulage
None required. Could put emesis on shirt if desired.
E. Approximate Timing
Set-Up: 3 min Scenario: 12 min Debriefing: 15 min
2015 EMSIMCASES.COM Page 2
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
CCB OD 3
Section V: Patient Data and Baseline State
A. Clinical Vignette: To Read Aloud at Beginning of Case
A 48-year-old female presents to the ED with an unknown overdose. She was out drinking with friends
until an hour ago. Her daughter came home and found her with vomit around her, empty pill bottles, and
bits of pills in her vomit.
B. Patient Profile and History
Patient Name: Yvette Clark Age: 48 Weight: 100kg
Gender: M F Code Status: Full
Chief Complaint: ?OD
History of Presenting Illness: Out drinking last night. May have overdosed on meds when got home.
Past Medical History: HTN Medications: Nifedipine XR 60mg daily
DM Glyburide 5mg daily
Depression Lasix 40mg daily
HCTZ 25mg daily
Clonazepam 2mg qHS
Allergies: None
Social History: Single mother of two children, now grown. (Daughter here in ED.) Drinks heavily on
weekends.
Review of Systems: CNS: Nil
HEENT: Nil
CVS: Nil.
RESP: Nil
GI: Emesis prior to arrival
GU: Nil
MSK: Nil INT: Nil
C. Baseline Simulator State and Physical Exam
No Monitor Display Monitor On, no data displayed Monitor on Standard Display
HR: 50/min BP: 87/43 RR: 10/min O2SAT: 95% RA
Rhythm: junctional T: 36 C
o Glucose: 6.8 mmol/L GCS: 9 (E2 V2 M5)
General Status: Somnolent, looks unwell.
CNS: Somnolent. Grunts/moans only. Opens eyes to pain, localizes to pain.
HEENT: No signs HI. Pupils 3mm, reactive.
CVS: No murmur.
RESP: Slow resp rate. Slight work of breathing.
ABDO: Soft, NT.
GU: Nil.
MSK: No signs trauma. SKIN: Nil.
2015 EMSIMCASES.COM Page 3
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
CCB OD 4
Section VI: Scenario Progression
Scenario States, Modifiers and Triggers
Patient State Patient Status Learner Actions, Modifiers & Triggers to Move to Next State
1. Baseline State Somnolent, Learner Actions Modifiers
Rhythm: sinus brady responding to - IV, O2, monitors Changes to patient condition based on
with 1st degree block pain only. - IV NS 1L bolus learner action
HR: 50/min - Tox bloodwork, VBG - Narcan no effect
BP: 87/43 - ECG - 1L bolus BP 92/50
RR: 10/min - Go through med list transiently
O2SAT: 95% RA - More history/px exam - Glucagon given emesis
T: 36oC - Check glucose (6.8)
- Trial narcan Triggers
For progression to next state
- Call poison centre
- 3 min 2. Persistent
Hypotension
2. Persistent Patient status Learner Actions Modifiers
Hypotension unchanged - Ca gluconate 2g iv bolus, - Post calcium BP 83/46
consider Ca infusion 2-3g/hr
BP 75/45 - Insulin infusion (1u/kg/hr
with 0.5u/kg bolus) with Triggers
D10NS @ 150ml/hr - All 3 agents started 3. More
- Check glucose q15 min Somnolent
- Repeat NS bolus - 9 min 3. More Somnolent
- Add vasopressor infusion
3. More Somnolent Begin state Learner Actions Modifiers
with RN saying - Check glucose (7.1) - Narcan No effect
RR 6 she seems to - Trial narcan (if not before)
O2SAT 91% be making less - Assist breathing (bagging) Triggers
respiratory - Prepare for intubation - Intubation 4. Intubation
effort - If dont intubate give VBG. At
12 min 5. Arrest
4. Intubation Learner Actions Modifiers
With pre- - Appropriate RSI - Propofol for intubation BP
oxygenation: - Post-intubation CXR 50/22
O2SAT 95% - Sedation infusion
- Prepare for central line Triggers
Post paralytic: - OG placement - Intubated 5. Arrest
RR 0 - Call ICU
5. Arrest Patient Learner Actions Modifiers
Rhythm: asystole pulseless. - High quality CPR
No vitals - EtCO2 monitoring
- Epinephrine q3 min Triggers
- Calcium Chloride & HCO3 - Intralipid given END CASE
- Consider intralipid - 15 min END CASE
2015 EMSIMCASES.COM Page 4
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
CCB OD 5
Section VII: Supporting Documents, Laboratory Results, & Multimedia
Laboratory Results
VBG pH: 6.97 PCO2: 106 PO2: 50 HCO3: 7
Images (ECGs, CXRs, etc.)
Initial ECG: Sinus brady with 1st degree block
ECG source: http://lifeinthefastlane.com/ecg-library/beta-blocker-and-calcium-channel-blocker-
toxicity/sb-1hb/
Post-Intubation CXR:
CXR source: https://emcow.files.wordpress.com/2012/11/normal-intubation2.jpg
2015 EMSIMCASES.COM Page 5
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
CCB OD 6
Section VIII: Debriefing Guide
General Debriefing Plan
Individual Group With Video Without Video
Objectives
Educational Goal: To expose learners to a multi-drug overdose and the management of a
severe CCB OD.
CRM Objectives: 1) Maintain calm leadership throughout complex case.
2) Demonstrate situational awareness as patient status changes
Medical Objectives: 1) Recognize a possible CCB overdose
2) Administer appropriate early treatments for a CCB overdose
3) Recognize hypercapneic respiratory failure and manage
appropriately.
4) Consider intralipid as treatment in an arrested CCB overdose
Sample Questions for Debriefing
1) When did you first consider nifedipine to be a possible cause of hypotension?
2) When did you first consider intubation?
3) What are the first line treatments for a CCB overdose?
4) When is intralipid indicated in a CCB overdose?
5) Why do you think the patient became somnolent?
Key Moments
Recognition of hypotension as possibly due to CCB
Recognition of respiratory depression and need for intubation
Recognition of need for intralipid in context of cardiac arrest
2015 EMSIMCASES.COM Page 6
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
You might also like
- No.6 Tzellos2008Document8 pagesNo.6 Tzellos2008harasthaNo ratings yet
- Opioid-Induced Tolerance and HyperalgesiaDocument70 pagesOpioid-Induced Tolerance and HyperalgesiaharasthaNo ratings yet
- Regional Anaesthesia To Prevent Chronic Pain After Surgery: A Cochrane Systematic Review and Meta-AnalysisDocument10 pagesRegional Anaesthesia To Prevent Chronic Pain After Surgery: A Cochrane Systematic Review and Meta-AnalysisharasthaNo ratings yet
- HOW TO Assess For Pain Sensitisation in The Clinic HANDOUTDocument12 pagesHOW TO Assess For Pain Sensitisation in The Clinic HANDOUTharasthaNo ratings yet
- Postmastectomy and Postthoracotomy Pain: Anne M. Wallace, MD, and Mark S. Wallace, MDDocument18 pagesPostmastectomy and Postthoracotomy Pain: Anne M. Wallace, MD, and Mark S. Wallace, MDharasthaNo ratings yet
- Endothelial Glycocalyx: Role in Body Fluid Homeostasis and Fluid ManagementDocument9 pagesEndothelial Glycocalyx: Role in Body Fluid Homeostasis and Fluid ManagementharasthaNo ratings yet
- Peripheral Chemical Mediators of Pain and HyperalgesiaDocument1 pagePeripheral Chemical Mediators of Pain and HyperalgesiaharasthaNo ratings yet
- Caesarean Section1846Document12 pagesCaesarean Section1846harasthaNo ratings yet
- Managing Advanced PD PDFDocument29 pagesManaging Advanced PD PDFharasthaNo ratings yet
- Craniocervical Dystonia Blepharospasm. Spasmodic Contraction of TheDocument3 pagesCraniocervical Dystonia Blepharospasm. Spasmodic Contraction of TheharasthaNo ratings yet
- Aortic Dissection: Section I: Scenario DemographicsDocument6 pagesAortic Dissection: Section I: Scenario DemographicsharasthaNo ratings yet
- Anaphylaxis With Angioedema: Section I: Scenario DemographicsDocument7 pagesAnaphylaxis With Angioedema: Section I: Scenario DemographicsharasthaNo ratings yet
- Laporan Kasus KADDocument43 pagesLaporan Kasus KADharasthaNo ratings yet
- Data Collection Is Done by Collecting Questioners and Processed Using SPSS ProgramDocument1 pageData Collection Is Done by Collecting Questioners and Processed Using SPSS ProgramharasthaNo ratings yet
- Acute Respiratory Distress: Section I: Scenario DemographicsDocument6 pagesAcute Respiratory Distress: Section I: Scenario DemographicsharasthaNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Acute Otitis Media: Jama Patient PageDocument1 pageAcute Otitis Media: Jama Patient PageS. JohnNo ratings yet
- Algorithm For Perioperative Management of Anticoagulation1Document8 pagesAlgorithm For Perioperative Management of Anticoagulation1andi namirah100% (1)
- Topic 5. MEDICAL TECHNOLOGY EDUCATIONDocument7 pagesTopic 5. MEDICAL TECHNOLOGY EDUCATIONSophia GarciaNo ratings yet
- Artículo de Trabeculectomía.Document13 pagesArtículo de Trabeculectomía.Dore OrtizNo ratings yet
- Myasthenia GravisDocument11 pagesMyasthenia GravisParvathy RNo ratings yet
- Med Surg (Oncology)Document169 pagesMed Surg (Oncology)DardarConstantinoNo ratings yet
- Giotto Image3D BrochureDocument16 pagesGiotto Image3D BrochureGriselda Maria Pinto SanchezNo ratings yet
- Mia SmsDocument8 pagesMia SmsGlasiNo ratings yet
- Pfizer Vaccine Explainer Version 2Document9 pagesPfizer Vaccine Explainer Version 2nqosa neidscqNo ratings yet
- Pelvic FracturesDocument17 pagesPelvic FracturesDiane IsmaelNo ratings yet
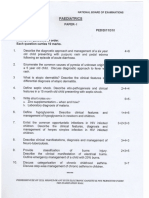
- Paediatrics: Final Exam National Board of Examinations December 2011Document4 pagesPaediatrics: Final Exam National Board of Examinations December 2011AlolikaNo ratings yet
- Form 5 Chemistry Folio - MedicineDocument37 pagesForm 5 Chemistry Folio - MedicineHeon50% (2)
- Amnesia ExplanationDocument2 pagesAmnesia ExplanationMuslim NugrahaNo ratings yet
- Dengue OutlineDocument6 pagesDengue OutlineLouie George NeriNo ratings yet
- Nitrous Oxide Sedation DentistryDocument16 pagesNitrous Oxide Sedation DentistryAnonymous k8rDEsJsU1100% (1)
- Medrobotics Receives FDA Clearance For ColorectalDocument2 pagesMedrobotics Receives FDA Clearance For ColorectalmedtechyNo ratings yet
- Common Dermatology Multiple Choice Questions and Answers - 6Document3 pagesCommon Dermatology Multiple Choice Questions and Answers - 6Atul Kumar Mishra100% (1)
- Family Therapy and Systemic PracticeDocument4 pagesFamily Therapy and Systemic PracticeUyên TrươngNo ratings yet
- Neuropathology: Stroke With Kartik Rangaraj MDDocument37 pagesNeuropathology: Stroke With Kartik Rangaraj MDAbdi fatah ali1No ratings yet
- Navle NotesDocument32 pagesNavle NotesRyan Fortier94% (18)
- MagnecalmfactsheetDocument5 pagesMagnecalmfactsheetKeith TippeyNo ratings yet
- Peripheral NeuropathyDocument30 pagesPeripheral NeuropathyLyn LynNo ratings yet
- Rabbit Analgesia: Standard Operating Procedure #102Document5 pagesRabbit Analgesia: Standard Operating Procedure #102Malu Verruck TortolaNo ratings yet
- Euros Core OrgDocument6 pagesEuros Core OrgClaudio Walter VidelaNo ratings yet
- Oral Biopsy: Oral Pathologist's Perspective: Review ArticleDocument7 pagesOral Biopsy: Oral Pathologist's Perspective: Review ArticleRafa LopezNo ratings yet
- Dialysis SkillsDocument2 pagesDialysis Skillssheelaaku100% (1)
- Maternal and Early-Life Nutrition and HealthDocument4 pagesMaternal and Early-Life Nutrition and HealthTiffani_Vanessa01No ratings yet
- 10 - Neonaticide, Infanticide and Child HomicideDocument45 pages10 - Neonaticide, Infanticide and Child HomicideWala AbdeljawadNo ratings yet
- Retinal Drawing: A Lost Art of MedicineDocument2 pagesRetinal Drawing: A Lost Art of MedicineManuel GallegosNo ratings yet
- Tension Pneumothorax: Modifiable FactorsDocument3 pagesTension Pneumothorax: Modifiable FactorsJustin MaverickNo ratings yet