Professional Documents
Culture Documents
74 79 Airway
Uploaded by
gusdinda27Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
74 79 Airway
Uploaded by
gusdinda27Copyright:
Available Formats
AIRWAY MANAGEMENT
Basic Airway Management
Dr. Madhurita Singh, Assoc. Professor, Dept. of Critical Care, CMC Vellore.
This is the first module in a series on management of airway and ventilation in critically ill patients.
Airway obstruction:
Introduction Airway obstruction results in hypoventilation,
In the initial assessment and management of any increased work of breathing and impaired gas ex-
critically ill patient the ABC's (Airway, Breathing change in the lungs. If this is not recognized in time
and Circulation) are the first priority. Hypoxia will and treated adequately, it can result in development
begin to cause irreversible brain injury within ap- of hypercarbia and ultimately hypoxaemia. Provision
proximately 5 minutes and so airway management of supplemental oxygen (using a mask or nasal
must precede any other treatment. canula) when there is an airway obstruction will not
The ability to establish and maintain an open air- resolve the problem of hypercapnia associated with
way in a patient, and the ability to ensure adequate hypoventilation and impaired alveolar ventilation.
ventilation and oxygenation of the patient, are there- Obstruction may be partial or complete, depend-
fore essential skills for physicians. For the purposes ing on the mechanism or cause. Complete airway
of this module "basic airway management" will refer obstruction will rapidly cause hypoxia and cardiac
to those basic interventions that maintain an open arrest, whereas partial obstruction may be more in-
airway and assist ventilation but do not include en- sidious in onset.
dotracheal intubation. Recognizing airway obstruction
Recognizing inadequate airway and venti- Some of the important signs of airway obstruction are:
lation 1. Noisy breathing: This is the hallmark of a com-
This is the first thing that doctors need to recog- promise in upper airway. It is indicative of partial
nize compromised airway and inadequate ventila- obstruction that can lead on to total obstruction.
tion. Noisy breathing may be in the form of snoring,
Adequate ventilation involves two factors gurgling (blood, vomit or secretions) or stridor.
1. Adequate intake as well as adequate exhalation of 2. Use of accessory muscles of respiration, agitation
air This indicates that there is enough tidal vol- 3. Expiratory wheeze (indicative of lower respira-
ume going into the patient as well as coming out. tory tract obstruction)
2. Adequate respiratory rate. Recognition of airway compromise, as seen from
The combination of these provides adequate oxygen the above description is primarily based on observa-
for gas exchange as well as allows removal of carbon tion and listening to the patient. A decrease in satura-
dioxide. Any problem with these two processes will tion is a late indication of ventilation and oxygena-
cause inadequate oxygenation and ventilation. tion. If one waits till the saturation decreases below
So what are the reasons of inadequate ventilation? 90%, significant damage due to hypoxia would have
The most common reasons are airway obstruction or already occurred. Dependence on the reading from
inadequate respiratory effort or a combination of the a saturation probe should never substitute for
two. looking and listening to the breathing of a patient.
CMI 13:2 74 April 2015
AIRWAY MANAGEMENT
Causes of airway obstruction: (1) struction will often be the result of the tongue falling
1. Obtundation of consciousness: In low level of con- back into the posterior pharynx due to loss of tone in
sciousness, the cause of the obstruction will often be the submandibular muscles. This problem can be
the result of the tongue falling back into the posterior quickly corrected using a simple maneuver such as a
pharynx due to loss of tone in the submandibular head tilt-chin lift or jaw thrust and this may be all
muscles. that is needed to open the airway and allow adequate
2. Intraluminal contents: Pooled secretions, blood, chest ventilation. If the physician encounters noisy or
vomitus and foreign bodies (Eg. Broken tooth in "gurgling" respirations at this point, the upper airway
trauma) should be suctioned for vomitus and excess secre-
3. External compression: Haematoma, tumour, goitre tions.
4. Direct trauma: Blunt trauma to maxilla, larynx, In patients with a low level of consciousness (Eg.
mandible, burns, smoke inhalation Head injury), the airway may be maintained by
5. Artificial airways: Blockage or displacement of proper positioning (semi-prone position) to prevent
tracheostomy, displacement of tracheal stent the tongue from falling back and obstructing the air-
6. Excessive granulation tissue: Prolonged mechani- way in the supine position.
cal ventilation, tracheal stenosis, supraglottic steno- Endotracheal intubation is the definitive interven-
sis tion in the management of an obstructed airway as it
7. Neuromuscular disorders: myasthenia gravis not only provides passage for air, but also protects
the trachea from further obstruction due to pooling of
secretions etc. Endotracheal intubation will be dis-
Management of obstructed airway
cussed in the next module.
Once obstruction of the airway is detected, imme-
Some of the simple interventions to maintain air-
diate measures have to be taken to discover the cause
way in a critically ill patient are described below.
and to maintain the airway. Delay can lead to danger-
Simple airway manoeuvres
ous hypoxemia and cardiac arrest.
Head Tilt-Chin-Lift:
Opening up and maintaining an obstructed airway
This manoeuvre should only be used if the physi-
may require one or more of the following measures:
cian is confident there is no risk of injury to the cer-
1. Physical manoeuvres like head tilt-chin lift or
vical spine. Standing on the patient's right hand side,
jaw thrust
2. Suctioning to remove debris and foreign bodies
3. Positioning
4. Airway adjuncts
5. Endotracheal intubation
If the patient is making respiratory effort but is
not adequately ventilating his/her chest because of
airway obstruction the doctor must determine the
cause and take immediate measures to alleviate the
obstruction.
In an unconscious patient, the cause of the ob- Fig.1: Chin-lift and jaw thrust manoeuvres
CMI 13:2 75 April 2015
AIRWAY MANAGEMENT
the doctors left hand is used to apply pressure to the inserted as soon as possible by someone with training
forehead to extend the neck. The volar surfaces of the and expertise in that skill.
tips of the index and middle finger are used to elevate 1. Oropharyngeal airway
the mandible, which will lift the tongue from the pos- The oropharyngeal airway is essentially a curved
terior pharynx. (Fig.1) hollow tube that is used to create an open conduit
Jaw-Thrust: through the mouth and posterior pharynx. A rough
Where there is risk of cervical spine injury, such guide for choosing the correct size is to hold the air-
as a patient who is unconscious as a result of a head way beside the patient's mandible, orienting it with
injury, the airway should be opened using a manoeu- the flange at the
vre that does not require neck movement. The jaw patient's mouth
thrust is performed by having the physician stand at and the tip at the
the head of the patient looking down at the patient. angle of jaw. The
The middle finger of the each hand is placed at the tip should just
angle of the patient's jaw on both sides. An upward reach the angle of
pressure is applied to elevate the mandible, which the jaw. While
will lift the tongue from the posterior pharynx. inserting the air-
(Fig.1) way avoid push-
Positioning ing the tongue
In patients with a poor level of consciousness due Fig.2: Oropharyngeal airway -
into the posterior Assessing size (2)
to any cause, airway obstruction is usually because pharynx. This can
the tongue falls back in the supine position and partly be accomplished by starting with the curve of the
obstructs the upper airway. If endotracheal intubation airway inverted, and then rotate the airway as the tip
is not being considered, (Eg. mild to moderate head reaches the posterior pharynx. Alternatively a tongue
injury), the airway in these patients can be main- depressor can be used to move the tongue out of the
tained by semi-prone positioning. The patient lies on way as the airway is passed. Whichever technique is
the side with the chest supported by pillows and head chosen the physician must be certain that the airway
facing down. Instability of the cervical spine will is indeed in the right position. If there are problems
have to be ruled out before positioning. ventilating the patient after insertion of the airway
Airway adjuncts then it should be removed and reinserted.
Once the airway is open, an oropharyngeal or na- 2. Nasopharyngeal airway
sopharyngeal airway may need to be inserted to make The nasopharyngeal airway is a soft rubber or
it easier to maintain an open airway. Both of these plastic hollow tube that is passed through the nose
devices prevent the tongue from occluding the airway into the posterior pharynx. To measure the length of
and thereby provide an open conduit for air to pass. It the airway, measure the distance from the tip of the
is important to note that these two airway devices, nose to the tip of the tragus. The diameter of the air-
unlike a cuffed endotracheal tube, will not protect way should also be measured and it should be little
the trachea from aspiration of secretions or stom- less that the diameter of the patient nares. The naso-
ach contents. If a patient is unable to protect their pharyngeal airway is generally better tolerated than
own airway, they should have an endotracheal tube the oropharyngeal airway in a semiconscious patient.
CMI 13:2 76 April 2015
AIRWAY MANAGEMENT
The nasal airway is well lubricated with lignocaine
jelly and inserted with the bevel toward the septum.
While a nasopharyngeal airway may be left in
place, an oropharyngeal airway should only
be used as a temporary measure to keep the
airway open before definitive management
like endotracheal intubation. This is because
the oropharyngeal airway does not protect the
trachea and also prevents the patient from swal-
Fig. 5: Bag-mask ventilation (two-person
Fig.3: technique) (5)
Assessing The first step in bag-mask ventilation is to select a
size of naso-
pharyngeal mask that will cover the mouth and nose of the pa-
tube (3) tient and create a tight seal. The mask is then at-
tached to the bag device, which should be attached to
high flow oxygen (15L/min.) such that the reservoir
of the bag is fully inflated.
Two-person technique
The biggest challenge in bag-mask ventilation is
maintaining an open airway and a tight seal using one
hand. If a second person is available, it is recom-
mended that one person manages the mask and the
Fig.4: Insertion of nasopharyngeal airway
airway, while the second person squeezes the bag to
lowing and if left in place for long periods ventilate the chest. The person responsible for the
(especially in a patient who is able to swallow), mask stands at the head of the bed and places his
it only quickens the process of pooling of secre- thumbs on the top surface of the mask. The remain-
tions and aspiration ing fingers are then used to grip the mandible on ei-
Bag-mask ventilation ther side. The mask is squeezed between the thumbs
A patient who is not able to breathe adequately on and the fingers to create a seal and at the same time
their own will require support of their breathing the mandible is elevated to open the airway. This
through artificial means. In order to push oxygen rich technique is considerably easier, but again, the doctor
air into the patient's chest, some form of positive must be constantly checking that air is flowing easily
pressure ventilatory assistance is required. The tech- into the patient and that the chest is rising and falling.
nique of bag-mask ventilation is difficult even in the The rate of ventilation should be about 12 15
best of hands and will require considerable practice breaths per minute. In a cardiac arrest, the rate of res-
before it can be done effectively on a patient. How- pirations is 1 breath every 6-8 seconds. In a respira-
ever, if mastered, this can be lifesaving in an emer- tory arrest, the rate of respirations is 1 breath every 5-
gency. 6 seconds.
CMI 13:2 77 April 2015
AIRWAY MANAGEMENT
If there is obstruction to air flow or the chest does should immediately ventilate the chest and watch for
not rise, recheck to make sure that there is a tight seal adequate chest rise using the two-person technique.
to the face, that the mandible is being elevated to Remember, adequate chest ventilation is the single
open the airway and, if an artificial airway is being most important determinant of patient outcome in an
used, that it is in place. Readjust the mask and try apneic patient. Continue ventilating till help arrives
again. and definitive care with endotracheal intubation can
Steps toward assessing the airway (Basic be performed. If you are the only one at the scene,
Life Support protocol): ask a nurse to gather the equipment for endotracheal
Step 1: Assess responsiveness intubation and perform it, while continuing mask
Use the "shake and shout" technique to assess re- ventilation.
sponsiveness. At the same time scan the chest for Sources:
breathing. If the patient is unresponsive and not 1.Managing airway obstruction. British Journal of Hospi-
breathing, proceed to the next step. If the patient is tal Medicine, October 2012, Vol 73, No 10
2.Image from http://www.haworth21.karoo.net
breathing proceed to step 4.
3.Image from http://little-medic.blogspot.in
Step 2: Call for help 4.Essentials of Critical Care 8th Ed. Division of critical
In all resuscitation situations, the first one on the care, CMC Vellore.
scene will require assistance and hence the impor- 5.Image from http://www.cuhk.edu.hk/
6.Image from http://emedicine.medscape.com/
tance of this step. At this point you must ask for a
article/80184-overview#a15
monitor with facility for SpO2, non-invasive blood
pressure and ECG monitoring, a defibrillator and per-
Suggested material for the
sonnel to come and assist with resuscitation.
Step 3: Check pulse
Equipment Tray
If there is no pulse, start chest compressions im- 1. Gloves
The rescuer should at all times avoid direct con-
mediately and follow the basic life support protocol.
tact with the blood and other body fluids of the
If pulse is present and the patient is not breathing
patient. If available, gloves should be worn dur-
proceed to the next step.
ing all airway management procedures.
Step 4: Open the airway
2. Suction apparatus
Noisy breathing is indicative of an obstructed air-
In most resuscitation situations, the patient will
way. Ensure an open airway using the techniques
either vomit, or at the very least, have an excess
described ear-
of secretion in their oropharynx. If available, a
lier.
suction catheter should be included as part of
Step 5: Venti- your basic airway equipment.
late chest
In the ab-
sence of spon-
taneous respira-
tion, the rescuer Fig. 6: Holding mask in two-
person technique (6)
CMI 13:2 78 April 2015
AIRWAY MANAGEMENT
3. Lubricant
If a nasopharyngeal airway is used, it will require lubrication of
its outer surface prior to insertion. Xylocaine Jelly is used be-
cause it is a good lubricant and it reduces irritation through its
local anaesthetic effect.
4. Nasopharyngeal Airway
The nasopharyngeal airway is made of soft, pliable plastic,
and is inserted through the nares and into the nasopharynx,
thus providing a patent airway to facilitate chest ventilation. It
has the advantage of being better tolerated in the conscious
or semi-conscious patient than the oropharyngeal airway. It is
also easier to insert in a patient who has his/her teeth
clenched. It is important to note that the NP airway does not
protect the airway from aspiration of vomitus.
5. Oropharyngeal Airway
The oropharyngeal airway is a rigid plastic device, which is
inserted through the mouth into the oropharynx. This provides
a patent airway to facilitate chest ventilation. It is important to
note that the oropharyngeal airway does not protect the air-
way from aspiration of vomitus.
6. Bag-Valve Ventilator
The bag-valve ventilator is a device designed to ventilate the
chest. By attaching an oxygen supply, it can be used to venti-
late the chest with a high concentration of oxygen. The bag-
valve ventilator can be used with a mask, as in basic airway
management, or it can be attached to an endotracheal tube as
part of advanced airway management.
7. Mask
Masks are used to provide a tight seal between the patient's
face and the bag-valve ventilator. Masks come in various
sizes. The correct size of the mask for a particular patient
should provide a tight seal around the nose and mouth. The
pointed end of the mask creates a seal over the bridge of the
patient's nose, while the round end creates a seal between the
lower lip and chin.
CMI 13:2 79 April 2015
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Empirical First Line AntibioticsDocument1 pageEmpirical First Line Antibioticsdiati zahrainiNo ratings yet
- Scrotal HerniaDocument9 pagesScrotal HerniaReymart BolagaoNo ratings yet
- Big Book Sponsorship - The Twelve Step Program - Big Book Guide - 4-Hour-12-StepsDocument30 pagesBig Book Sponsorship - The Twelve Step Program - Big Book Guide - 4-Hour-12-StepscafegrNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Saudi Commission Manual Classifies Health PractitionersDocument38 pagesSaudi Commission Manual Classifies Health Practitionerstoplexil100% (1)
- Yvonne Farrell Psycho Emotional NotesDocument10 pagesYvonne Farrell Psycho Emotional Notesபாலஹரிப்ரீதா முத்து100% (2)
- Motorcycle DiariesDocument9 pagesMotorcycle DiariesGelo De Guzman100% (1)
- Respiratory System Notes - KEYDocument3 pagesRespiratory System Notes - KEYjoy100% (1)
- Cephalometric Evaluation and Measurement of The Upper Airway PDFDocument13 pagesCephalometric Evaluation and Measurement of The Upper Airway PDFSoe San KyawNo ratings yet
- Ifu Somatom DriveDocument600 pagesIfu Somatom DriveImc Muati100% (1)
- Analytical Method Validation of Clopidogrel Tablets BR HPLCDocument48 pagesAnalytical Method Validation of Clopidogrel Tablets BR HPLCAman ThakurNo ratings yet
- Jurnal InvaginasiDocument3 pagesJurnal InvaginasiAbdurrohman IzzuddinNo ratings yet
- Depression in Today - BioDocument5 pagesDepression in Today - Bioapi-272648963No ratings yet
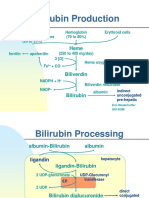
- Bilirubin Production: Hemoglobin (70 To 80%) Erythroid Cells Heme Proteins Myoglobin, Cytochromes (20 To 25%)Document5 pagesBilirubin Production: Hemoglobin (70 To 80%) Erythroid Cells Heme Proteins Myoglobin, Cytochromes (20 To 25%)Daffa Samudera Nakz DoeratipNo ratings yet
- C.V AfayoDocument4 pagesC.V AfayoAfayo RobertNo ratings yet
- Lactose intolerance diagnosis and treatmentDocument12 pagesLactose intolerance diagnosis and treatmentNico BatallaNo ratings yet
- Diatermo MB 122 and MB 160 Mono-Bipolar: Cautery & ElectrosurgeryDocument13 pagesDiatermo MB 122 and MB 160 Mono-Bipolar: Cautery & ElectrosurgeryDani Daniela100% (1)
- PRC FormDocument5 pagesPRC FormPamela DomingoNo ratings yet
- Forearm Fracture in ChildrenDocument45 pagesForearm Fracture in ChildrenMagnusNo ratings yet
- Masterlist SummaryDocument6 pagesMasterlist Summarykentclark03No ratings yet
- Lawsuit Against Small Smiles Dental Center Aka Alabany Access Dental Center Et. Al.Document52 pagesLawsuit Against Small Smiles Dental Center Aka Alabany Access Dental Center Et. Al.DebHgnNo ratings yet
- Chapter 3 PsychDocument12 pagesChapter 3 Psychred_gyrl9282No ratings yet
- Nursing Comps Study GuideDocument15 pagesNursing Comps Study GuideforminskoNo ratings yet
- Large Volume Parenterals: Guidelines and Quality Control TestsDocument36 pagesLarge Volume Parenterals: Guidelines and Quality Control TestsRákêsh MãttàNo ratings yet
- Pre Conference Final ProgDocument2 pagesPre Conference Final ProgkeithlyndNo ratings yet
- Spring 2011 21st AnniversaryDocument56 pagesSpring 2011 21st AnniversaryRajesh SekhriNo ratings yet
- Hybrid Hyrax Distalizer JO PDFDocument7 pagesHybrid Hyrax Distalizer JO PDFCaTy ZamNo ratings yet
- Adult Diarrhea GuideDocument15 pagesAdult Diarrhea GuideM.Reza ErlanggaNo ratings yet
- Medicine in Situ Panchen TraditionDocument28 pagesMedicine in Situ Panchen TraditionJigdrel77No ratings yet
- PG Physician Guide 03 Eng1Document88 pagesPG Physician Guide 03 Eng1hüseyin vururNo ratings yet
- ق 4Document36 pagesق 4Zainab HasanNo ratings yet