Professional Documents
Culture Documents
Simulation of Growth Trajectories of Childhood Obesity Into Adulthood
Uploaded by
Juan Camilo LandazuriOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Simulation of Growth Trajectories of Childhood Obesity Into Adulthood
Uploaded by
Juan Camilo LandazuriCopyright:
Available Formats
The n e w e ng l a n d j o u r na l of m e dic i n e
Original Article
Simulation of Growth Trajectories
of Childhood Obesity into Adulthood
ZacharyJ. Ward, M.P.H., MichaelW. Long, Sc.D., StephenC. Resch, Ph.D.,
CatherineM. Giles, M.P.H., AngieL. Cradock, Sc.D.,
and StevenL. Gortmaker, Ph.D.
A BS T R AC T
BACKGROUND
Although the current obesity epidemic has been well documented in children and From the Center for Health Decision Sci-
adults, less is known about long-term risks of adult obesity for a given child at his ence (Z.J.W., S.C.R.) and the Department
of Social and Behavioral Sciences (C.M.G.,
or her present age and weight. We developed a simulation model to estimate the A.L.C., S.L.G.), Harvard T.H. Chan School
risk of adult obesity at the age of 35 years for the current population of children of Public Health, Boston; and the Depart-
in the United States. ment of Prevention and Community
Health, Milken Institute School of Public
Health, George Washington University,
METHODS Washington, DC (M.W.L.). Address re-
We pooled height and weight data from five nationally representative longitudinal print requests to Mr. Ward at the Center
studies totaling 176,720 observations from 41,567 children and adults. We simu- for Health Decision Science, Harvard
T.H. Chan School of Public Health, 718
lated growth trajectories across the life course and adjusted for secular trends. We Huntington Ave., Boston, MA 02115, or
created 1000 virtual populations of 1 million children through the age of 19 years at z ward@hsph.harvard.edu.
that were representative of the 2016 population of the United States and projected N Engl J Med 2017;377:2145-53.
their trajectories in height and weight up to the age of 35 years. Severe obesity was DOI: 10.1056/NEJMoa1703860
defined as a body-mass index (BMI, the weight in kilograms divided by the square Copyright 2017 Massachusetts Medical Society.
of the height in meters) of 35 or higher in adults and 120% or more of the 95th
percentile in children.
RESULTS
Given the current level of childhood obesity, the models predicted that a majority
of todays children (57.3%; 95% uncertainly interval [UI], 55.2 to 60.0) will be obese
at the age of 35 years, and roughly half of the projected prevalence will occur dur-
ing childhood. Our simulations indicated that the relative risk of adult obesity
increased with age and BMI, from 1.17 (95% UI, 1.09 to 1.29) for overweight
2-year-olds to 3.10 (95% UI, 2.43 to 3.65) for 19-year-olds with severe obesity. For
children with severe obesity, the chance they will no longer be obese at the age of
35 years fell from 21.0% (95% UI, 7.3 to 47.3) at the age of 2 years to 6.1% (95% UI,
2.1 to 9.9) at the age of 19 years.
CONCLUSIONS
On the basis of our simulation models, childhood obesity and overweight will
continue to be a major health problem in the United States. Early development of
obesity predicted obesity in adulthood, especially for children who were severely
obese. (Funded by the JPB Foundation and others.)
n engl j med 377;22nejm.org November 30, 2017 2145
The New England Journal of Medicine
Downloaded from nejm.org on November 29, 2017. For personal use only. No other uses without permission.
Copyright 2017 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
I
n the United States, the prevalence risks of obesity are well established, in order to
of obesity has declined recently among chil- analyze the effect of a childs current weight on
dren between the ages of 2 and 5 years and the risk of adult obesity.
has stabilized among those between the ages
of 6 and 11 years of age but continues to rise Me thods
among adolescents and adults.1,2 Although the
obesity epidemic has been well characterized Data Sources
ata population level, less is known about the We pooled five nationally representative U.S. data
individual-level risk of adult obesity for a given sets that contain repeated measures of individual-
child on the basis of current weight and age. level height and weight: the National Longitudi-
Cohort studies indicate that excess weight dur- nal Survey of Youth, the National Longitudinal
ing childhood is a predictor of future obesity,3-13 Study of Adolescent to Adult Health, the Early
with high correlations with body-mass index Childhood Longitudinal StudyKindergarten, the
(BMI, the weight in kilograms divided by the Panel Study of Income Dynamics, and the Epide-
square of the height in meters) over time.14-16 miologic Follow-up Study of the National Health
A number of epidemiologic cohort studies and Nutrition Examination Survey (NHANES).
provide insight into growth trajectories, but they After removing participants who had fewer than
often do not follow children into adulthood. For 2 recorded observations, the pooled data set con-
example, the sample-weighted average follow-up tained 176,720 observations from 41,567 children
period among 16 international cohorts was 12 and adults, a mean (SD) of 4.31.6 observations
years3-13,15-18 and was only 7 years among U.S. per person. Participants with 2 or more observa-
studies.3-10 Although obesity has health effects in tions were on average younger and more likely
children,19-22 obesity-related death and complica- to be female and white. (Details regarding data
tions generally affect adults who are 35 years of sources and exclusion criteria are provided in Sec-
age or older.23,24 Longitudinal data linking trajec- tion 1.1 in the Supplementary Appendix, available
tories of childhood BMI with health risks in with the full text of this article at NEJM.org.)
adulthood are needed to characterize the long-
term consequences of childhood obesity more Trajectory Simulation
precisely.25-27 Using these data, we developed a simulation
Although a few studies do follow children model to predict growth trajectories on the basis
into midadulthood, such studies are necessarily of individual-level weight and height informa-
based on cohorts that were initiated decades tion. We interpolated childhood trajectories on
earlier.5,16,18 Given the changes in obesity preva- the basis of growth curves developed by the
lence and environmental influences,28,29 it is not Centers for Disease Control and Prevention
clear how applicable the results of these studies (CDC) after adjustment for secular trends in
are for todays children. For example, a compari- weight using NHANES data from 1976 through
son of two British cohorts born 12 years apart 2014. We obtained the parameters that were
showed significant differences in BMI trajecto- used to adjust for these trends by means of a
ries,18 which raises questions about the use of model-fitting procedure that aligned trends in
past cohort studies to predict risks for todays our simulated BMI categories with recently ob-
youth. Although previous studies have used sta- served trends, using data from the Census, the
tistical methods to forecast the population-level American Community Survey, the Behavioral Risk
prevalence of obesity in the United States,30-34 Factor Surveillance System, the National Survey
they have not incorporated individual-level longi- of Childrens Health, and NHANES. We estimated
tudinal data. trends for four BMI categories: underweight or
To address such concerns, we developed a normal weight, overweight, moderate obesity,
method to simulate individual-level height and and severe obesity. Once these steps were com-
weight trajectories over the life course while ac- pleted, we used the simulation model to predict
counting for secular trends. For this study, we the risk of obesity. (Details regarding these steps
simulated such trajectories from childhood until are provided in Sections 1 through 3 in the
the age of 35 years, at which point the health Supplementary Appendix.)
2146 n engl j med 377;22nejm.org November 30, 2017
The New England Journal of Medicine
Downloaded from nejm.org on November 29, 2017. For personal use only. No other uses without permission.
Copyright 2017 Massachusetts Medical Society. All rights reserved.
Simulation of Growth Tr ajectories of Childhood Obesity
Simulation Predictions dicted his or her height and weight over the
To predict the risk of obesity at the age of 35 length of the observed trajectory. We then com-
years, we created virtual populations of 1 million pared our predictions with the actual values to
children who were 19 years of age or younger evaluate the accuracy of our algorithm. We con-
using statistical matching techniques to produce ducted cross-validation analyses for participants
nationally representative, open populations be- whose last age was between 34 and 36 years and
ginning in 2016, as described previously.35,36 (In calculated the coverage probability of our esti-
an open population, new participants are being mates that is, we calculated the probability
born into the simulation model, so the popula- that the actual values for this cohort fell within
tion structure changes over time, whereas in a our predicted uncertainty intervals. In addition,
closed population, no new participants are en- we ran prospective cross-validation analyses for
tering the model.) We estimated the conditional younger cohorts starting from the age of 2 years
probability of obesity at the age of 35 years given to 29 years and calculated the number of times
BMI status at each age in childhood and then that our predictions fell within the bootstrapped
calculated the associated relative risks. We also 95% confidence intervals (Section 4 in the Sup-
calculated the risks of future obesity at 5-year plementary Appendix).
intervals for each BMI group, according to age Our model was coded in Java as part of the
and sex. We repeated this process with 1000 Childhood Obesity Intervention Cost-Effective-
independently generated populations, each time ness Study (CHOICES).40,41 Statistical analyses were
randomly sampling a set of good-fitting parame- performed with the use of R software. BMI cat-
ters for secular trends. egories were calculated on the basis of CDC
This approach allowed us to incorporate the standards, with severe obesity defined as a BMI
individual-level (first-order) uncertainty that arises of 35 or higher for adults42 and 120% or more of
from the simulation of trajectories and also to the 95th percentile for children.43 Data and R code
incorporate uncertainty about the parameters are available from the authors on request.
(second-order) that we used to adjust for secular
trends.37 Because the effect of first-order uncer-
R e sult s
tainty on aggregate estimates decreases as the
sample size increases, most of the uncertainty in Accuracy of the Simulation Model
our estimates reflects the previously described Our simulated projections of BMI categories from
second-order issues. We report means and 95% 2010 to 2030 corresponded well to trends observed
uncertainty intervals (i.e., the 2.5 and 97.5 percen- in NHANES and captured differences according
tiles). We also performed sensitivity analyses for to age, sex, and race or ethnic group (Fig.1, and
secular trends by performing 100 iterations of the Section 3.4 in the Supplementary Appendix). Our
model, assuming there were actually no secular simulated trajectories also showed correlations
trends. By not incorporating uncertainty about between BMI during childhood and BMI at the
the various parameters into our sensitivity analysis, age of 35 years that were similar to correlations
we could estimate the relative contribution of indi- that have been shown in previous studies. Such
vidual-level uncertainty to our prediction intervals. correlations range from approximately 0.2 at
To evaluate the convergent validity (the extent the age of 2 years to 0.5 by 10 years and to more
to which different models that address the same than 0.6 by 15 years. BMI correlations for periods
problem calculate similar results) of our ap- of 5 years and 10 years ranged from approxi-
proach,38 we compared the simulated prevalence mately 0.4 at the age of 2 years to more than
of obesity at the age of 35 years with logistic- 0.8 by 15 years (Section 3.5 in the Supplemen-
regression predictions on the basis of NHANES tary Appendix). Our cross-validation analyses
data from 1999 through 2014 for persons be- showed coverage estimates of 100% for predict-
tween the ages of 34 and 36 years. ed obesity prevalence and mean BMI values be-
We also performed extensive cross-validation tween the ages of 34 and 36 years; 94% of our
analyses in which we predicted values for partici- obesity predictions for younger ages fell within
pants in our data set.39 We removed a participant the 95% confidence intervals of the actual val-
from our data set one at a time and then pre- ues (Section 4 in the Supplementary Appendix).
n engl j med 377;22nejm.org November 30, 2017 2147
The New England Journal of Medicine
Downloaded from nejm.org on November 29, 2017. For personal use only. No other uses without permission.
Copyright 2017 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
Population: NHANES CHOICES model
BMI Category: Underweight or normal weight Overweight Moderate obesity Severe obesity
A Children 219 Yr of Age
100
80
Prevalence (%)
60
40
20
0
2000 2004 2008 2012 2016 2020 2024 2028
B Adults 20 Yr of Age
100
80
Prevalence (%)
60
40
20
0
2000 2004 2008 2012 2016 2020 2024 2028
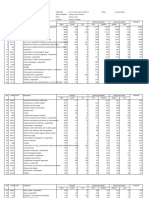
Figure 1. Predicted Prevalence of BMI Categories through 2030 for Children and Adults.
Shown is a comparison of the predicted prevalence of categories of body-mass index (BMI) from the Childhood
Obesity Intervention Cost-Effectiveness Study (CHOICES) model and logistic-regression predictions that are based
on data from the National Health and Nutrition Examination Survey (NHANES) from 1999 through 2014 for children
between the ages of 2 and 19 years (Panel A) and adults 20 years of age or older (Panel B). The shaded areas indi-
cate 95% uncertainty intervals for the logistic-regression predictions, and the dashed lines, ranges for simulated
prevalence. BMI categories were calculated on the basis of standards of the Centers for Disease Control and Preven-
tion (CDC), with severe obesity defined as a BMI of 35 or higher for adults and 120% or more of the 95th percentile
for children.
Projections for All Children jected prevalence reached by this point (Fig. 2B,
On the basis of current trends for BMI and obe- and Section 5.2 in the Supplementary Appendix).
sity, our projections for children between the ages The prevalence then continued to increase after
of 2 years and 19 years showed that the majority adolescence. Similar patterns were observed ac-
of todays youth (57.3%; 95% uncertainty inter- cording to race or ethnic group but with sig-
val [UI], 55.2 to 60.0) will be obese at the age of nificant disparities in obesity prevalence already
35 years (Fig. 2A, and Section 5.1 in the Supple- present by the age of 2 years (Fig. 3).
mentary Appendix). For a cohort of current
2-year-olds, we found that the prevalence of Projections According to Obesity Status
obesity increased until adolescence, at which Among obese children, we found that the prob-
point it stabilized, with about half of the pro- ability that they will still be obese at the age of
2148 n engl j med 377;22 nejm.org November 30, 2017
The New England Journal of Medicine
Downloaded from nejm.org on November 29, 2017. For personal use only. No other uses without permission.
Copyright 2017 Massachusetts Medical Society. All rights reserved.
Simulation of Growth Tr ajectories of Childhood Obesity
A Predicted Prevalence of Obesity at 35 Years of Age, According to Calendar Year
100 NHANES CHOICES model
Observed
Regression model
80
Obesity Prevalence (%)
60
40
20
0
2000 2004 2008 2012 2016 2020 2024 2028 2032 2036 2040 2044 2048
B Predicted Prevalence of Obesity among 2-Year-Olds at Future Ages
60
50
Obesity Prevalence (%)
40
30
20
10
0
5 10 15 20 25 30 35
Age (yr)
Figure 2. Predicted Prevalence of Obesity at the Age of 35 Years.
Panel A shows the predicted prevalence of obesity at the age of 35 years among todays children from the CHOICES
simulation model as compared with logistic-regression predictions on the basis of NHANES data for adults between
the ages of 34 and 36 years from 1999 through 2014. The 95% uncertainty intervals are indicated by a shaded area
for the NHANES data and by dashed lines for the CHOICES model. Panel B shows the projected prevalence of obe-
sity at future ages among 2-year-olds in 2016. The shaded areas indicate 95% uncertainty intervals.
35 years increased with age, from 74.9% (95% 1.80 to 2.17) at 19 years. We found a consistent
UI, 67.3 to 81.5) at 2 years of age to 88.2% (95% risk gradient according to BMI category at all
UI, 84.6 to 92.3) at 19 years (Fig. 4A). Among ages (Fig. 4B); the relative risk ranged from 1.17
children who were not obese, the probability of (95% UI, 1.09 to 1.29) for overweight 2-year-olds
obesity at the age of 35 years decreased with age, to 3.10 (95% UI, 2.43 to 3.65) for severely obese
from 57.8% (95% UI, 54.5 to 62.1) at 2 years of 19-year-olds (Section 5.3 in the Supplementary
age to 44.4% (95% UI, 40.4 to 49.7) at 19 years. Appendix).
The relative risks of adult obesity in obese chil- Although these projections indicated that
dren, as compared with children who were not obese children are likely to be obese as adults,
obese, increased with age, from 1.30 (95% UI, we also found that the majority of obese 35-year-
1.17 to 1.45) at 2 years of age to 1.99 (95% UI, olds were not obese as children (Section 5.4 in
n engl j med 377;22 nejm.org November 30, 2017 2149
The New England Journal of Medicine
Downloaded from nejm.org on November 29, 2017. For personal use only. No other uses without permission.
Copyright 2017 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
80
Race or Ethnic Group
Hispanic
Black
60 White
Obesity Prevalence (%) Other
40
20
0
5 10 15 20 25 30 35
Age (yr)
Figure 3. Predicted Prevalence of Obesity, According to Race or Ethnic Group.
Shown is the projected prevalence of obesity at future ages among 2-year-olds in 2016 from the CHOICES simulation
model, according to race or ethnic group. The model shows that significant disparities are already established at
very young ages. The shaded areas indicate 95% uncertainty intervals.
the Supplementary Appendix). As an indicator (57.3%), with similar age-related trends and
of adult obesity, childhood obesity had a high BMI risk gradients. Details regarding the sen-
specificity (93.1%) but a low sensitivity (29.3%) sitivity analyses are provided in Section 7 in the
on average (Section 5.5 in the Supplementary Supplementary Appendix.
Appendix). However, the high prevalence of obe-
sity in the population resulted in a higher posi- Discussion
tive predictive value (85.1%) and a lower negative
predictive value (49.5%). Although a broad range of public health and
Severely obese children are at especially high clinical efforts appear to have stabilized early
risk for adult obesity, with the chance of not be- childhood obesity rates,1 in this study we esti-
ing obese at the age of 35 years ranging from mated that among children between the ages of
21.0% (95% UI, 7.3 to 47.3) at 2 years of age to 2 and 19 years in 2016, more than half (57.3%)
6.1% (95% UI, 2.1 to 9.9) at 19 years (Section 5.6 will be obese by the age of 35 years. However,
in the Supplementary Appendix); at the age of the majority of these children were not currently
19 years, the chance drops to 3.5% (95% UI, 0.9 obese; about half of the total prevalence of obe-
to 8.5) among boys and to 8.2% (95% UI, 2.4 to sity began in childhood, and adult-onset obesity
14.5) among girls. Obesity risk tables at 5-year by 35 years of age accounted for the rest.
intervals are provided for each age, sex, and BMI Given the increased risk of adult obesity, it
group in Section 6 in the Supplementary Appendix. seems clear that children who are obese are
prime candidates for early intervention. Children
Sensitivity Analyses with severe obesity, a condition that now affects
In sensitivity analyses in which we assumed 4.5 million children (6%) in the United States,1
that there were no secular trends in weight are at particularly high risk. At 2 years of age,
gain, the predicted prevalence of obesity at the severely obese children have only a 1-in-5 chance
age of 35 years for todays children was 48.9% of not being obese by the age of 35 years; by
(95% UI, 48.8 to 49.1), a prevalence that was 5 years, that chance is halved, to 1 in 10. The
slightly lower than that in our main results persistence of elevated risk is striking: a 2-year-
2150 n engl j med 377;22 nejm.org November 30, 2017
The New England Journal of Medicine
Downloaded from nejm.org on November 29, 2017. For personal use only. No other uses without permission.
Copyright 2017 Massachusetts Medical Society. All rights reserved.
Simulation of Growth Tr ajectories of Childhood Obesity
A Probability According to Current Obesity Status and Age B Probability According to Current BMI Category and Age
Probability of Obesity at 35 Yr of Age 1.0 1.0
Probability of Obesity at 35 Yr of Age
0.8 0.8
0.6 0.6
0.4 0.4
Current Status Current Status
Obesity Severe obesity
0.2 No obesity 0.2 Moderate obesity
Overweight
Normal weight or underweight
0.0 0.0
5 10 15 5 10 15
Current Age (Yr) Current Age (Yr)
Figure 4. Predicted Probability of Obesity at the Age of 35 Years, According to Current Age, Obesity Status, and BMI
Category.
Shown is the probability of obesity at the age of 35 years, according to current age and obesity status (Panel A) and
BMI category (Panel B). The shaded areas indicate 95% uncertainty intervals.
old who is obese is more likely to be obese at of obesity at various ages with a high degree of
35 years of age than an overweight 19-year-old. accuracy.
Thus, our findings highlight the importance of Although our approach may facilitate more
promoting a healthy weight throughout child- accurate predictions of future obesity risk for a
hood and adulthood. A narrow focus solely on given child than were possible in previous stud-
preventing childhood obesity will not avert poten- ies, our results generally yielded insights that
tial future health damage that may be induced were consistent with those of previous studies,
by the ongoing obesity epidemic.27 In our sensi- such as the persistence of childhood obesity over
tivity analyses, even when we assumed no continu- time,3,5-7,9 especially among severely obese chil-
ing secular trends in weight gain, we predicted dren.44 Our simulated trajectories also showed
that almost half of children will be obese when age-related correlations with respect to BMI and
they are 35 years of age. There is evidence that test characteristics (sensitivity and specificity) that
cost-effective approaches with broad population were similar to those in previous studies.3,11,14-16,26
reach could have substantial effects for the pres- However, our calculated relative risks of obesity
ent generation of children.40,41 were smaller than those in past studies, since we
A strength of our study is that we used a rigor- accounted for secular trends of an increasing
ous approach to simulate demographic and public risk of obesity in the reference group of children
health surveillance data together with nationally who were underweight or of normal weight. We
representative growth trajectories over the life also found significant disparities in the preva-
course while simultaneously adjusting for secu- lence of obesity according to race or ethnic group
lar trends. Our approach provides estimates that that were already present by 2 years of age, an in-
were not possible with simpler methods, since it sight that was consistent with previous findings.45
generated projections of population-level obesity Our study has certain limitations. The main
consistent with current trends while maintain- assumption and potential limitation underlying
ing individual-level heterogeneity in growth. Our our method of predicting growth patterns is that
cross-validation analyses have shown that our on average, persons with similar trajectories in
algorithm could be used to predict the prevalence height and weight for a given period of their
n engl j med 377;22 nejm.org November 30, 2017 2151
The New England Journal of Medicine
Downloaded from nejm.org on November 29, 2017. For personal use only. No other uses without permission.
Copyright 2017 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
lives will also grow similarly in future periods. could not examine the effect of excess weight in
The assumption that secular trends will continue, infancy on adult obesity.
and the assumptions underlying our estimation In conclusion, using simulated growth trajec-
of these trends, may also have influenced our tories across the life course and adjusting for
results. However, in our analyses, the age-related secular trends, we found that only those children
trends in relative risk were robust to sensitivity with a current healthy weight have less than a
analyses in which no secular trends were applied. 50% chance of becoming obese by the age of 35
Our reference group also included children years. For children with severe obesity, the risk
who were underweight, which is known to be of adult obesity is particularly high.
problematic in the estimation of the risk of death The views expressed in this article are those of authors and do
or complications because of confounding associ- not represent the official views of the Centers for Disease Con-
trol and Prevention or any of the other funders.
ated with low weight.24 However, it is unlikely No potential conflict of interest relevant to this article was
that the inclusion of underweight children in our reported.
study presents similar issues for comparisons of Disclosure forms provided by the authors are available with
the full text of this article at NEJM.org.
future obesity risks, although it may underesti- Supported in part by grants from the JPB Foundation, the
mate the risks in our combined group of chil- Robert Wood Johnson Foundation (grant no. 66284), the Donald
dren who are underweight or of normal weight. and Sue Pritzker Nutrition and Fitness Initiative, and the Centers
for Disease Control and Prevention (grant no. U48/DP001946),
Finally, because overweight and obesity are de- including the Nutrition and Obesity Policy Research and Evalua-
fined by the CDC starting at 2 years of age, we tion Network.
References
1. Ogden CL, Carroll MD, Lawman HG, tions through childhood and early adoles- Risk in Young Finns Study. J Pediatr 2011;
et al. Trends in obesity prevalence among cence: a multistate life table approach. 159:584-90.
children and adolescents in the United Am J Epidemiol 2016;183:643-9. 17. Ekelund U, Ong K, Linn Y, et al. Up-
States, 1988-1994 through 2013-2014. 10. Wang LY, Chyen D, Lee S, Lowry R. ward weight percentile crossing in infancy
JAMA 2016;315:2292-9. The association between body mass index and early childhood independently predicts
2. Flegal KM, Kruszon-Moran D, Carroll in adolescence and obesity in adulthood. fat mass in young adults: the Stockholm
MD, Fryar CD, Ogden CL. Trends in obe- J Adolesc Health 2008;42:512-8. Weight Development Study (SWEDES).
sity among adults in the United States, 11. Evensen E, Wilsgaard T, Furberg AS, Am J Clin Nutr 2006;83:324-30.
2005 to 2014. JAMA 2016;315:2284-91. Skeie G. Tracking of overweight and obe- 18. Li L, Hardy R, Kuh D, Lo Conte R,
3. Cunningham SA, Kramer MR, Naray- sity from early childhood to adolescence Power C. Child-to-adult body mass index
an KM. Incidence of childhood obesity in in a population-based cohort the Troms and height trajectories: a comparison of
the United States. N Engl J Med 2014;370: Study, Fit Futures. BMC Pediatr 2016;16:64. 2 British birth cohorts. Am J Epidemiol
403-11. 12. Kim KR, Kim MK, Shin YJ, Choi BY. 2008;168:1008-15.
4. Gordon-Larsen P, Adair LS, Nelson Relationship between the change in over- 19. Dietz WH. Health consequences of
MC, Popkin BM. Five-year obesity inci- weight status from childhood to adoles- obesity in youth: childhood predictors of
dence in the transition period between cence and metabolic syndrome pheno- adult disease. Pediatrics 1998;101:518-25.
adolescence and adulthood: the National types: a 9-year retrospective study. Eur J 20. Rao G. Diagnosis, epidemiology, and
Longitudinal Study of Adolescent Health. Clin Nutr 2008;62:748-53. management of hypertension in children.
Am J Clin Nutr 2004;80:569-75. 13. Venn AJ, Thomson RJ, Schmidt MD, Pediatrics 2016;138(2):e20153616.
5. Janssen I, Katzmarzyk PT, Srinivasan et al. Overweight and obesity from child- 21. Temple JL, Cordero P, Li J, Nguyen V,
SR, et al. Utility of childhood BMI in the hood to adulthood: a follow-up of partici- Oben JA. A guide to non-alcoholic fatty
prediction of adulthood disease: compari- pants in the 1985 Australian Schools liver disease in childhood and adoles-
son of national and international refer- Health and Fitness Survey. Med J Aust cence. Int J Mol Sci 2016;17:E947.
ences. Obes Res 2005;13:1106-15. 2007;186:458-60. 22. Thompson N, Mansfield B, Stringer
6. Nader PR, OBrien M, Houts R, et al. 14. Deshmukh-Taskar P, Nicklas TA, Mo- M, Stewart B, Potter J, Fernengel K. An
Identifying risk for obesity in early child- rales M, Yang SJ, Zakeri I, Berenson GS. evidence-based resource for the manage-
hood. Pediatrics 2006;118(3):e594-e601. Tracking of overweight status from child- ment of comorbidities associated with
7. Stovitz SD, Hannan PJ, Lytle LA, De- hood to young adulthood: the Bogalusa childhood overweight and obesity. J Am
merath EW, Pereira MA, Himes JH. Child Heart Study. Eur J Clin Nutr 2006;60:48- Assoc Nurse Pract 2016;28:559-70.
height and the risk of young-adult obesity. 57. 23. GBD 2013 Risk Factors Collaborators,
Am J Prev Med 2010;38:74-7. 15. Magarey AM, Daniels LA, Boulton TJ, Forouzanfar MH, Alexander L, et al. Global,
8. Thompson DR, Obarzanek E, Franko Cockington RA. Predicting obesity in early regional, and national comparative risk
DL, et al. Childhood overweight and car- adulthood from childhood and parental assessment of 79 behavioural, environ-
diovascular disease risk factors: the Na- obesity. Int J Obes Relat Metab Disord mental and occupational, and metabolic
tional Heart, Lung, and Blood Institute 2003;27:505-13. risks or clusters of risks in 188 countries,
Growth and Health Study. J Pediatr 2007; 16. Juhola J, Magnussen CG, Viikari JSA, 1990-2013: a systematic analysis for the
150:18-25. et al. Tracking of serum lipid levels, blood Global Burden of Disease Study 2013.
9. Tran MK, Krueger PM, McCormick E, pressure, and body mass index from child- Lancet 2015;386:2287-323.
Davidson A, Main DS. Body mass transi- hood to adulthood: the Cardiovascular 24. Global BMI Mortality Collaboration,
2152 n engl j med 377;22nejm.org November 30, 2017
The New England Journal of Medicine
Downloaded from nejm.org on November 29, 2017. For personal use only. No other uses without permission.
Copyright 2017 Massachusetts Medical Society. All rights reserved.
Simulation of Growth Tr ajectories of Childhood Obesity
Di Angelantonio E, Bhupathiraju SN, et al. Gortmaker SL, Brown M. Health and eco- 39. Efron B, Gong G. A leisurely look at
Body-mass index and all-cause mortality: nomic burden of the projected obesity the Bootstrap, the Jackknife, and cross-
individual-participant-data meta-analysis trends in the USA and the UK. Lancet validation. Am Stat 1983;37:36-48.
of 239 prospective studies in four conti- 2011;378:815-25. 40. Gortmaker SL, Wang YC, Long MW,
nents. Lancet 2016;388:776-86. 33. Finkelstein EA, Khavjou OA, Thomp- et al. Three interventions that reduce child-
25. Cheung PC, Cunningham SA, Narayan son H, et al. Obesity and severe obesity hood obesity are projected to save more
KM, Kramer MR. Childhood obesity inci- forecasts through 2030. Am J Prev Med than they cost to implement. Health Aff
dence in the United States: a systematic 2012;42:563-70. (Millwood) 2015;34:1932-9.
review. Child Obes 2016;12:1-11. 34. Wang YC, Orleans CT, Gortmaker SL. 41. Cradock AL, Barrett JL, Kenney EL,
26. Goldhaber-Fiebert JD, Rubinfeld RE, Reaching the Healthy People goals for et al. Using cost-effectiveness analysis to
Bhattacharya J, Robinson TN, Wise PH. reducing childhood obesity: closing the prioritize policy and programmatic ap-
The utility of childhood and adolescent energy gap. Am J Prev Med 2012;42:437- proaches to physical activity promotion
obesity assessment in relation to adult 44. and obesity prevention in childhood. Prev
health. Med Decis Making 2013;33:163-75. 35. Ward ZJ, Long MW, Resch SC, et al. Med 2017;95:Suppl:S17-S27.
27. Trasande L. How much should we in- Redrawing the US obesity landscape: bias- 42. Wang YC, Pamplin J, Long MW, Ward
vest in preventing childhood obesity? corrected estimates of state-specific adult ZJ, Gortmaker SL, Andreyeva T. Severe
Health Aff (Millwood) 2010;29:372-8. obesity prevalence. PLoS One 2016;11(3): obesity in adults cost state Medicaid pro-
28. Swinburn BA, Sacks G, Hall KD, et al. e0150735. grams nearly $8 billion in 2013. Health
The global obesity pandemic: shaped by 36. Long MW, Ward ZJ, Resch SC, et al. Aff (Millwood) 2015;34:1923-31.
global drivers and local environments. State-level estimates of childhood obesity 43. Claire Wang Y, Gortmaker SL, Taveras
Lancet 2011;378:804-14. prevalence in the United States corrected EM. Trends and racial/ethnic disparities
29. Institute of Medicine. Accelerating for report bias. Int J Obes (Lond) 2016;40: in severe obesity among US children and
progress in obesity prevention:solving 1523-8. adolescents, 1976-2006. Int J Pediatr Obes
the weight of the nation. Washington, DC: 37. Briggs AH, Weinstein MC, Fenwick 2011;6:12-20.
National Academies Press, 2012. EA, Karnon J, Sculpher MJ, Paltiel AD. 44. Freedman DS, Mei Z, Srinivasan SR,
30. Wang YC, Colditz GA, Kuntz KM. Model parameter estimation and uncertain- Berenson GS, Dietz WH. Cardiovascular
Forecasting the obesity epidemic in the ty analysis: a report of the ISPOR-SMDM risk factors and excess adiposity among
aging U.S. population. Obesity (Silver Modeling Good Research Practices Task overweight children and adolescents: the
Spring) 2007;15:2855-65. Force Working Group-6. Med Decis Mak- Bogalusa Heart Study. J Pediatr 2007;
31. Wang Y, Beydoun MA, Liang L, Cabal- ing 2012;32:722-32. 150(1):12-17.e2.
lero B, Kumanyika SK. Will all Americans 38. Eddy DM, Hollingworth W, Caro JJ, 45. Taveras EM, Gillman MW, Kleinman
become overweight or obese? Estimating Tsevat J, McDonald KM, Wong JB. Model KP, Rich-Edwards JW, Rifas-Shiman SL.
the progression and cost of the US obesity transparency and validation: a report of Reducing racial/ethnic disparities in child-
epidemic. Obesity (Silver Spring) 2008;16: the ISPOR-SMDM Modeling Good Re- hood obesity: the role of early life risk fac-
2323-30. search Practices Task Force-7. Med Decis tors. JAMA Pediatr 2013;167:731-8.
32. Wang YC, McPherson K, Marsh T, Making 2012;32:733-43. Copyright 2017 Massachusetts Medical Society.
clinical trial registration
The Journal requires investigators to register their clinical trials
in a public trials registry. The members of the International Committee
of Medical Journal Editors (ICMJE) will consider most reports of clinical
trials for publication only if the trials have been registered.
Current information on requirements and appropriate registries
is available at www.icmje.org/faq_clinical.html.
n engl j med 377;22nejm.org November 30, 2017 2153
The New England Journal of Medicine
Downloaded from nejm.org on November 29, 2017. For personal use only. No other uses without permission.
Copyright 2017 Massachusetts Medical Society. All rights reserved.
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Drug Study ICUDocument14 pagesDrug Study ICUAndrea Isabel U. O'Dell100% (1)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Aromatherapy Permacharts PDFDocument4 pagesAromatherapy Permacharts PDFLeo AdamsNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Wisdom Chi KungDocument0 pagesWisdom Chi KungDevlinPyxNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Colour Atlas of Mouth, Throat and Ear Disorders in Children 1985Document84 pagesColour Atlas of Mouth, Throat and Ear Disorders in Children 1985Vitaliy ZhevachevskyyNo ratings yet
- Essential Neurology 4Th Ed PDFDocument290 pagesEssential Neurology 4Th Ed PDFPutu 'yayuk' Widyani WiradiraniNo ratings yet
- Cva Case StudyDocument20 pagesCva Case StudyEricson Somera100% (1)
- Model of Human Ocupattion Screening Tool MOHOSTDocument30 pagesModel of Human Ocupattion Screening Tool MOHOSTLuis Luna Hernandez100% (3)
- Sce Gastro Sample QsDocument36 pagesSce Gastro Sample QsZoya Annam100% (8)
- Plantar Fascitis 2 PDFDocument18 pagesPlantar Fascitis 2 PDFDSouza Dominic RoyNo ratings yet
- Terminologia Dolor Plantar o Fascitis PlantarDocument3 pagesTerminologia Dolor Plantar o Fascitis PlantarJuan Camilo LandazuriNo ratings yet
- Neuropatia Por Atrapamiento Revision Actualizada de SchonDocument9 pagesNeuropatia Por Atrapamiento Revision Actualizada de SchonJuan Camilo LandazuriNo ratings yet
- Baxter y Los Bailarines 2008 PDFDocument6 pagesBaxter y Los Bailarines 2008 PDFJuan Camilo LandazuriNo ratings yet
- Plantar Fascitis JaaosDocument9 pagesPlantar Fascitis JaaosCatherine JonesNo ratings yet
- Revision Mas Completa Fascitis PlantarDocument10 pagesRevision Mas Completa Fascitis PlantarJuan Camilo LandazuriNo ratings yet
- Practice: Klinefelter's SyndromeDocument4 pagesPractice: Klinefelter's SyndromeJuan Camilo LandazuriNo ratings yet
- Baxter y Su Neuropatia en El Año 1994Document6 pagesBaxter y Su Neuropatia en El Año 1994Juan Camilo LandazuriNo ratings yet
- Heel Pain Syndrome: Electrodiagnostic Support For Nerve EntrapmentDocument7 pagesHeel Pain Syndrome: Electrodiagnostic Support For Nerve EntrapmentJuan Camilo LandazuriNo ratings yet
- Alshami2008 PDFDocument9 pagesAlshami2008 PDFJuan Camilo LandazuriNo ratings yet
- Baxter y Los Bailarines 2008 PDFDocument6 pagesBaxter y Los Bailarines 2008 PDFJuan Camilo LandazuriNo ratings yet
- Practice: Klinefelter's SyndromeDocument4 pagesPractice: Klinefelter's SyndromeJuan Camilo LandazuriNo ratings yet
- Fig. 13.49 Hypertensive Retinopathy. (A) Focal ArteriolarDocument3 pagesFig. 13.49 Hypertensive Retinopathy. (A) Focal ArteriolarJuan Camilo LandazuriNo ratings yet
- Neonatal MRI To Predict Neurodevelopmental Outcomes in Preterm InfantsDocument10 pagesNeonatal MRI To Predict Neurodevelopmental Outcomes in Preterm InfantsJuan Camilo LandazuriNo ratings yet
- Cannabis Use and Disorder - Epidemiology, Comorbidity, Health Consequences, and Medico-Legal Status - UpToDateDocument19 pagesCannabis Use and Disorder - Epidemiology, Comorbidity, Health Consequences, and Medico-Legal Status - UpToDateJuan Camilo Landazuri100% (1)
- Nejmp1513708 PDFDocument2 pagesNejmp1513708 PDFJuan Camilo LandazuriNo ratings yet
- Neonatal MRI To Predict Neurodevelopmental Outcomes in Preterm InfantsDocument10 pagesNeonatal MRI To Predict Neurodevelopmental Outcomes in Preterm InfantsJuan Camilo LandazuriNo ratings yet
- New England Journal Medicine: The ofDocument11 pagesNew England Journal Medicine: The ofGonzalo LealNo ratings yet
- Heart AttackDocument13 pagesHeart AttackJuan Camilo LandazuriNo ratings yet
- Doctors NDocument2 pagesDoctors NJuan Camilo LandazuriNo ratings yet
- The Effect of Doxycycline On Serum Levels Of.18Document5 pagesThe Effect of Doxycycline On Serum Levels Of.18Juan Camilo LandazuriNo ratings yet
- Nejmoa 060467Document11 pagesNejmoa 060467Juan Camilo LandazuriNo ratings yet
- Respiratory Tract InfectionsDocument31 pagesRespiratory Tract InfectionsPritha BhuwapaksophonNo ratings yet
- FLM-porto Systemic AnastomosisDocument10 pagesFLM-porto Systemic AnastomosisYusuf Bin ZaidiNo ratings yet
- MCH MCQSDocument10 pagesMCH MCQSPabitra ThapaNo ratings yet
- Edible Vaccines: Promises and Challenges: Vrinda M Kurup Jaya ThomasDocument12 pagesEdible Vaccines: Promises and Challenges: Vrinda M Kurup Jaya ThomasBelaNo ratings yet
- Ocular ManifestationDocument10 pagesOcular ManifestationPrincess Cate MercadoNo ratings yet
- Clinical Evaluation of Paneeya Kshara (Oral Administration of Alkaline Medicine) in The Management of PittashayaDocument7 pagesClinical Evaluation of Paneeya Kshara (Oral Administration of Alkaline Medicine) in The Management of PittashayagingerthealienNo ratings yet
- Drug Study - VancomycinDocument2 pagesDrug Study - VancomycinKhatlen BagaresNo ratings yet
- AfflictionsDocument12 pagesAfflictionsshiraaazNo ratings yet
- Ebook PDF Churchills Pocketbook of Surgery e Book 5th Edition PDFDocument30 pagesEbook PDF Churchills Pocketbook of Surgery e Book 5th Edition PDFelizabeth.mcmillion447100% (31)
- Syok NeurogenikDocument14 pagesSyok NeurogenikFerrany ThiflaNo ratings yet
- Cipro: (Ciprofloxacin Hydrochloride) TabletsDocument34 pagesCipro: (Ciprofloxacin Hydrochloride) TabletsgammasharkNo ratings yet
- Differential Diagnosis of Stuttering For Forensic Purposes/journal Club Presentation/ Kunnampallil GejoDocument58 pagesDifferential Diagnosis of Stuttering For Forensic Purposes/journal Club Presentation/ Kunnampallil GejoKUNNAMPALLIL GEJO JOHNNo ratings yet
- Collateral History For Delirium/ DementiaDocument2 pagesCollateral History For Delirium/ DementiaPetros Akin-NibosunNo ratings yet
- MTRH I.Med ProtocolsDocument42 pagesMTRH I.Med ProtocolsRoberto Maina100% (3)
- SIP 2016 Abstract & Background Booklet V.6 PDFDocument187 pagesSIP 2016 Abstract & Background Booklet V.6 PDFJimboreanu György PaulaNo ratings yet
- Quizlet Renal QsDocument5 pagesQuizlet Renal QsElizabeth McKeeNo ratings yet
- DX TerseringDocument51 pagesDX TerseringShinta DeviantiNo ratings yet
- Health Declaration FormDocument1 pageHealth Declaration FormCalleja Jemimah Rose AristokiNo ratings yet
- Case Studies Therapy 1Document9 pagesCase Studies Therapy 1WONDWOSSEN ALEMUNo ratings yet
- Heat Stress Plan Revision 002Document33 pagesHeat Stress Plan Revision 00201095902062ahmedNo ratings yet
- Neonatal Sepsis CPGDocument115 pagesNeonatal Sepsis CPGFrances Jean T. DoblasNo ratings yet
- Blindness Control ProgramsDocument66 pagesBlindness Control ProgramsAravind KumarNo ratings yet
- Nosa Hse Qualifying Criteria and Classification of IncidentsDocument25 pagesNosa Hse Qualifying Criteria and Classification of IncidentsOvais FarooqNo ratings yet