Professional Documents
Culture Documents
Cervical Mucus Analysis: A Major Component in Evaluation of Infertility
Uploaded by
fifahcantikOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cervical Mucus Analysis: A Major Component in Evaluation of Infertility
Uploaded by
fifahcantikCopyright:
Available Formats
Cervical Mucus Analysis:
A Major Component in
Evaluation of Infertility
Tech Com:
Special Topics by Brooks A. Keel, B.S.
Male and female factors both con- been suggested as a causative fac- scanty amounts of thick, viscous
tribute to infertility. Cervical mucus- tor in 15% t o 50% of infertile mucus. The penetrability of sper-
sperm incompatibility can be a major couples. 1 Therefore, analysis of matozoa through the cervical m u -
factor in infertility, and the analysis of cervical mucus has become an im- cus is greatly inhibited during the
cervical mucus can be an important portant diagnostic tool in the eval- luteal phase. 2
tool in the evaluation of the infertile
uation of infertile couples, espe-
couple, especially when examination
cially when examination of the Specimen Collection
reveals that the male partner is ap-
parently normal. Several diagnostic male partner shows no abnormality.
Cervical mucus normally should
techniques used in the evaluation of be examined at the time of ovula-
This article describes the meth-
cervical mucus and of sperm-mucus
ods that we use for routine cervical t i o n , when one w o u l d ordinarily
interactions are described. These
mucus analysis. Along with a com- expect intercourse to result in
techniques, which can be performed
in any clinical laboratory, can greatly plete semen analysis, this evalua- pregnancy. Ovulation may be de-
assist the referring physician in mak- tion can provide the physician with tected in a variety of simple ways,
ing a proper diagnosis and prognosis valuable information concerning one of which is a shift in basal
when treating a couple for infertility. the possible cause and treatment body temperature. Most experts
(Key words: Cervical mucus; Infertil- of the infertile couple. agree that cervical mucus should
ity; Sperm-mucus interactions.) be collected 24 t o 48 hours before
Monthly Changes in Cervical the temperature shift. 1 3
Introduction Mucus
After the patient is prepared for
Before e n t e r i n g the h u m a n Cervical mucus undergoes dra- pelvic examination, cervical mucus
uterus, sperm must first pass matic changes during the men- can be aspirated directly from the
through the uterine cervix. The strual cycle. Hormones secreted endocervix using a tuberculin
cervical mucus plays an active role by the ovaries affect the structure syringe (without the needle). If the
in facilitating this passage. Nor- and secretory activity of the cervix, cervix cannot be reached with the
mally, both the cervix and the cer- resulting in both quantitative and syringe alone, a plastic tip may be
vical mucus undergo m o n t h l y qualitative changes in cervical m u - attached to the syringe. 3 Since the
changes that reflect the different cus. 2 D u r i n g the preovulatory characteristic ferning pattern of
phases of the hormonal cycle. The (follicular) phase of the normal the cervical mucus seen during
hormonal changes responsible for menstrual cycle, increasing levels ovulation (described below) is due
o v u l a t i o n normally cause the of estrogen influence the cervix to in part to an increase in salt ions,
mucus to become optionally re- produce copious amounts of t h i n , any apparatus used to collect the
ceptive to sperm penetration. watery mucus. By midcycle (around mucus should be free of saline to
Abnormal changes in mucus can the time of ovulation), the quality prevent false results. 4 After the mu-
adversely influence the passage of and quantity of cervical mucus is cus has been collected, it may be
sperm into the uterus. Cervical optimal for sperm penetration. sent to the laboratory immediately
m u c u s - s p e r m incompatibility has During the postovulatory (luteal) for analysis or it may be stored in
phase of the menstrual cycle, the an ordinary refrigerator freezer
levels of estrogen decrease and (-10C to -20C) for later analy-
progesterone begins to increase, sis. We have so stored mucus
From the Tissue Bank and Clinical Laboratory,
XYTEX Corporation, Augusta, Georgia. causing the cervix to produce specimens in the collection syringe
0007-5027/81/0300/161 $00.70 American Society of Clinical Pathologists 161
cm case, the cervical mucus). There-
fore, a complete cervical mucus
7
analysis must include analysis of
the interactions of sperm and
6
mucus. For the following proce-
I l l
5 dures, sperm should be collected
from the male partner after a three-
A
4 day sexual abstinence. The ejacu-
D late should then be evaluated as
3
described previously. 7 If the part-
ner's semen is unavailable, semen
2
from a donor of proven fertility
1 may be used. The diagnostic value
of donor semen is substantially
0 less than the value of partner
semen.
3
Slide Test
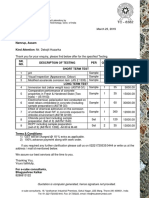
Fig. 1. Measurement of cervical mucus spinnbarkeit: (A) centimeter ruler;
The slide test 1 8 is a simple quali-
(B) microscope slide; (C) cervical mucus extruded from (D) tuberculin
tative evaluation of the ability of
syringe.
sperm to penetrate cervical mucus.
A drop of semen and a drop of
cervical mucus are placed on a
for several weeks w i t h o u t any Ferning
clean, dry glass slide and then care-
noticeable detrimental effects.
When a drop of cervical mucus fully brought together by placing
obtained at midcycle from a nor- a coverslip on t o p , thus f o r m i n g
Gross Examination mal patient is spread on a clean, an interface between the sperm
dry glass slide and allowed to dry, and mucus. In a normal interface,
Spinnbarkeit a characteristic palm-leaf or fern- one is able to observe under the
ing effect (Fig. 2) can be seen un- microscope sperm migration
Spinnbarkeit, an index to the d e r t h e microscope. 6 Although the across the interface from the
viscoelasticity or "threading capac- criteria for quantifying the degree seminal plasma into the mucus.
ity" of cervical mucus, can be eval- of ferning are subjective, 3 ferning Results should be reported as pen-
uated easily by extruding a small is usually graded on a scale of 1 + etrable or nonpenetrable mucus.
portion of the mucus from the to 4 + ; the number rating repre-
syringe onto a clean, dry glass slide sents the number of right angles CapiJJary-Tube Test
(Fig. 1). The extruding portion of in the f e r n , with 4 + representing
the mucus is held on the slide w i t h maximum branching with four The quantitative capillary-tube
a coverslip, and the syringe is raised right angles (Fig. 3). method of measuring the ability of
to measure the maximum thread- sperm to penetrate cervical mucus,
Normal midcycle cervical mucus
ing capacity of the mucus. This first described by Kremer, 9 utilizes
height is measured with a centi- should display good ferning with
an easily constructed sperm pene-
meter ruler which is held vertically 3+ to 4 + branching. A low degree
tration meter (Fig. 4). A sperm
behind the slide. 1 A spinnbarkeit of ferning or an irregular or " p u f f y "
reservoir is made from a glass or
of 5 - 6 cm or more has been ac- appearance may indicate abnor-
plastic test tube 7 cm long and 7
cepted as normal for ovulatory mal cervical mucus and should be
mm wide by longitudinally bisect-
mucus. 1 ' 5 reported.
ing the test tube using a diamond-
point pencil and retaining a 1-cm
Analysis of Sperm-Mucus " h e m i c u p " from the bottom of the
Because variability in the ex-
Interactions bisected tube. This hemicup is
truded volume of cervical mucus
can affect accurate measurement Because infertility can be caused glued to a clean glass slide to make
of spinnbarkeit, it is important to by either sexual partner, an ac- the reservoir. A glass capillary tube
standardize the volumes by ex- curate evaluation of the problem 2 cm long is then glued onto the
truding the same volume of mucus can be accomplished only by eval- slide 1 cm from the aperture of
from the syringe each time spinn- uating both the male factor (se- the reservoir and parallel to the
barkeit is measured. men) and female factors (in this short side of the slide. The slide
162 LABORATORY MEDICINE VOL 12, NO. 3, MARCH 1981
can then be calibrated with a centi-
meter scale using ink.
To perform the capillary-tube
test, mucus is drawn into a capil-
lary tube. A drop of mucus is al-
lowed to f o r m at one end of the
capillary tube and the other end is
sealed with clay. The capillary tube
is then placed onto the penetra-
tion meter (Fig. 4) so that the mucus
drop comes into contact with the
semen that has been placed in the
reservoir. The capillary is then se-
cured to the meter with clay. The
meter is placed horizontally in an
incubator at 37C for three hours.
After the incubation p e r i o d , the
meter is placed under a microscope
and examined using low power. ' ! 3^>v
The distance that the sperm travels
Fig. 2. Photomicrograph demonstrating a typical 3-4+ cervical mucus
up the tube of mucus in three
ferning pattern.
hours is then recorded. It has been
suggested that the lower limit of
normal for this test is 20 mm/3 h,
and the lower limit for fertility is
6 mm/3 h. 5 1 0
Sperm-Mucus Immobilization
Test
The s p e r m - m u c u s immobiliza-
tion test is performed to determine
if any factors (e.g., chemical or
immunologic) are present in the
cervical mucus that may cause im-
mobilization of the sperm. To per-
form this test, a drop of semen
and a drop of mucus are mixed on
one end of a glass slide and cov-
ered with a coverslip. Another
drop of semen is placed at the op-
posite end of the slide and also
covered with a coverslip to serve
as a test control. Both drops of
semen are then evaluated micro-
scopically for percent motility by
examining ten high-power fields
(hpf) and estimating the percent-
age of motile sperm. The slide is
then placed in an incubator at 37C
for 30 minutes, and reexamined
after incubation for percent mo-
tility. The motility of the control
drop of semen is compared with the
s p e r m - m u c u s mixture, and any Fig. 3. Simplified diagram demonstrating the rating system used to grade
decrease in motility is recorded. cervical mucus ferning. The grade number (1 + to4 +) represents the num-
Chemical factors in the mucus or ber of right angles on the fern.
LABORATORY MEDICINE VOL. 12, NO. 3, MARCH 1981 1 6 3
in the seminal plasma may cause a preferably obtained from donors
simple decrease in motility. How- of proven fertility.
ever, if a decrease in motility is
accompanied by sperm aggrega- After an initial analysis of the
t i o n , one must consider i m m u n o - semen and the mucus has been
logic factors. evaluated, crossmatch testing is
performed as follows: 1) the hus-
Sims-Huhner Postcoital TestfPCTJ band's sperm is tested w i t h the
wife's mucus; 2) the husband's
The Sims-Huhner postcoital test sperm is tested w i t h the donor's
(PCT), a classical procedure in the mucus; 3) the donor's sperm is
testing of the infertile couple, is tested with the wife's mucus; and
currently subject to widespread 4) the donor's sperm is tested with
debate. The method of performing the donor's mucus. If the hus-
and interpreting this test has not band's sperm will penetrate the
yet been standardized. 1 The re- donor's mucus but not the wife's
sults of the test are affected by mucus, a cervical mucus abnor-
timing, coital technique and semen
quality as well as cervical mucus
physiology. 3 However, this simple
test can be performed in the physi-
mality is indicated. However, if
the husband's sperm will not pen-
etrate either the wife's or the
donor's mucus, a semen abnor-
Fig. 4. Kremer sperm penetration
cian's office during a routine pelvic mality is indicated. The interpre-
meter: left, front view; right, side
examination. tation of the crossmatch results
view (see text).
will be reflected in the outcome
Basically, the test involves sam-
of interaction of the d o n o r ' s
pling the cervical mucus after inter-
sperm and the wife's mucus.
course and examining the mucus after coitus. 1 A normal PCT will
for the presence of motile sperm. demonstrate more than ten sperm
A great deal of controversy exists per hpf w i t h 50% motility, and an References
concerning the timing of the test. abnormal PCT will show less than
Most experts agree that the PCT five sperm per hpf with less than 1. Davajan, V., and Nakamura, R.M., 1975. The
should be performed during mid- cervical factor. In Progress of Infertility. 2nd
50% motility. edition. Edited by Behrman, S.J., and Kistner,
cycle or ovulation. However, the R.W. Boston, LittleBrown and Company, p. 17.
recommended time interval from 2. Hafez, E.S.E., 1976. Sperm transport in the
coitus to analysis ranges f r o m 90 Sperm-Mucus Crossmatch human and mammalian cervix. In The Cervix.
Edited by Jordan, J.A., and Singer, A. Phila-
seconds 11 to eight days. 12 We rec-
If cervical mucus is found to be delphia, W.B. Saunders Company, p. 164.
o m m e n d that the physician use 3. Blasco, L, 1977. Clinical approach to the
nonpenetrable to spermatozoa, or
the PCT as an office technique evaluation of sperm-cervical mucus inter-
if the results of a PCT are below actions. Fertil. Steril. 28:1133.
to determine if further laboratory
the normal range, a s p e r m - m u c u s 4. Grant, A., 1958. Cervical hostility. Fertil.
studies are warranted. Steril. 9:321.
crossmatch is indicated. This test
5. Ulstein, M., 1972. Evaluation of a capillary
After the cervical mucus speci- compares the s p e r m - m u c u s in- tube sperm penetration method for fertility in-
men has been obtained, a d r o p is teractions of the infertile couple vestigations. Acta Obstet. Gynecol. Scand.
with that of fertile donors. The re- 51:287.
placed on a slide, covered with a 6. Campos, duPaz, A., 1953. Crystallization
coverslip and examined micro- sults of this test can yield valuable phenomenon of cervical mucus in the human
scopically under high power. Five information in determining if the being and in animals. Proc. Internat. Fertil.
nonpenetrability is due to a factor Assoc. 1:595.
hpf are examined, and the num- 7. Keel, B.A., 1979. The semen analysis: An
ber and percent motility of sperm in the husband's semen, the wife's important diagnostic evaluation. Lab. Med.
in each field are recorded. The mucus, or both. 10:686.
8. Perloff, W.H., and Steinberger, E., 1963. In
mean number of sperm per hpf vivo penetration of cervical mucus by
The s p e r m - m u c u s crossmatch
and the mean percent motility are spermatozoa. Fertil. Steril. 14:231.
can be performed by using either
then calculated. 9. Kremer, J., 1965. A simple sperm penetration
the slide test or the Kremer capil- test. Int. J. Fertil. 10:201.
Although the interpretation of lary test m e t h o d . Cervical mucus 10. Ulstein, M., 1972. Sperm penetration of
cervical mucus as a criterion of male fertility.
the results requires a great deal of and semen are obtained both f r o m Acta Obstet. Gynecol. Scand. 51:335.
clinical j u d g m e n t , the normal the infertile couple being evalu- 11. Noyes, R.W., Adams, C.E., and Walton, A.,
range for a PCT may be considered ated and from suitable donors. 1958. Transport of spermatozoa into the
uterus of the rabbit. Fertil. Steril. 9:288.
to be the presence of 10-20 motile Donor semen and donor mucus
12. Fraenkel, L, 1930. Sterilisierung and Kozep-
sperm per hpf within 8-10 hours should be of good quality and tionsverhutung. Arch. Gynakol. 144:86.
164 LABORATORY M E D I C I N E VOL. 12, NO. 3, MARCH 1981
You might also like
- Sperm Recovery and SurvivalDocument6 pagesSperm Recovery and SurvivalArturo IturraldeNo ratings yet
- 2004 Article 461193Document3 pages2004 Article 461193Arturo AndNo ratings yet
- Cervical MucusDocument24 pagesCervical MucusRgn McklNo ratings yet
- 62 IhuDocument4 pages62 IhuAnonymous YyLSRdNo ratings yet
- Laboratory Assessment of Male Infertility - A Guide For The UrologistDocument4 pagesLaboratory Assessment of Male Infertility - A Guide For The UrologistMehmet Ali KaragözNo ratings yet
- Nursing Care Plan Cues Diagnosis Planning Implementation Rationale EvaluationDocument4 pagesNursing Care Plan Cues Diagnosis Planning Implementation Rationale EvaluationChrizley Shawn DeroniaNo ratings yet
- Cole & Hart 1930Document12 pagesCole & Hart 1930Nicolas Cabrera GimenaNo ratings yet
- Lesson 29 PDFDocument6 pagesLesson 29 PDFLaura B.No ratings yet
- 6.3 Deteccion de La OvulacionDocument9 pages6.3 Deteccion de La OvulacionLuis CarrascoNo ratings yet
- Male RSDocument7 pagesMale RSpravina praviNo ratings yet
- Other Body FluidsDocument10 pagesOther Body FluidsHiraya ManawariNo ratings yet
- Determination of Ovulation Time in Bitches Based On Teasing, Vaginal Cytology, and Elisa For ProgesteroneDocument9 pagesDetermination of Ovulation Time in Bitches Based On Teasing, Vaginal Cytology, and Elisa For ProgesteroneAna Luísa SampaioNo ratings yet
- Fertility and SubfertilityDocument95 pagesFertility and SubfertilitydidiNo ratings yet
- Bovine Reproduction Booklet UK A5 16pp Text 10Document20 pagesBovine Reproduction Booklet UK A5 16pp Text 10lenn chandNo ratings yet
- SimsDocument4 pagesSimsMariel AbatayoNo ratings yet
- Human ReproductionDocument2 pagesHuman Reproductionfaizan123khanNo ratings yet
- Evaluation of The Infertility CoupleDocument19 pagesEvaluation of The Infertility Coupleapi-3705046No ratings yet
- Silva2017-Flujo Vascular en Utero AlpacaDocument6 pagesSilva2017-Flujo Vascular en Utero AlpacaEnzo German ZampiniNo ratings yet
- ROLE OF FNAC TESTIS IN MALE INFERTILITY by SpandanaDocument61 pagesROLE OF FNAC TESTIS IN MALE INFERTILITY by SpandanaDineshprakash GovindhrajNo ratings yet
- Allen and Doisy 1923Document3 pagesAllen and Doisy 1923izaquenNo ratings yet
- Detection of Reproductive Status in Ongole Crossbred (PO) Cow Based On Vaginal Epithel Morphology and Profile Hormone - 2020Document5 pagesDetection of Reproductive Status in Ongole Crossbred (PO) Cow Based On Vaginal Epithel Morphology and Profile Hormone - 2020Isnin RamadhaniNo ratings yet
- Lecture Notes AnatomyDocument18 pagesLecture Notes AnatomyFau Fau DheoboNo ratings yet
- Undescended Testes: What General Practitioners Need To KnowDocument4 pagesUndescended Testes: What General Practitioners Need To KnowRizka Desti AyuniNo ratings yet
- Determining Canine Estrus Stage Via Vaginal Cytology: TheriogenologyDocument3 pagesDetermining Canine Estrus Stage Via Vaginal Cytology: TheriogenologyGissele ParaisoNo ratings yet
- T.G.Cooper, C.Keck, U.Oberdieck and E.Nieschlag: Human Reproduction Vol.8 No.8 Pp. 1251-1258, 1993Document8 pagesT.G.Cooper, C.Keck, U.Oberdieck and E.Nieschlag: Human Reproduction Vol.8 No.8 Pp. 1251-1258, 1993Reski AdeliaNo ratings yet
- Azoospermia Guidelines PDFDocument7 pagesAzoospermia Guidelines PDFafifberlianNo ratings yet
- The Effect of Intrauterine Insemination Time On Semen ParametersDocument4 pagesThe Effect of Intrauterine Insemination Time On Semen ParametersRamadhan AkmalNo ratings yet
- Undescended Testes (Orchidopexy)Document9 pagesUndescended Testes (Orchidopexy)nuranysha havizNo ratings yet
- 7.6 Undescended Testis Inguinal HerniaDocument7 pages7.6 Undescended Testis Inguinal HerniaΜατθαίος ΠαππάςNo ratings yet
- Pediatric Urology PDFDocument14 pagesPediatric Urology PDFekalospratamaNo ratings yet
- Difficulty of Conceiving-McnDocument4 pagesDifficulty of Conceiving-McnMary Leshiel TamayoNo ratings yet
- Proceedings of The 16th Italian Association of Equine Veterinarians CongressDocument14 pagesProceedings of The 16th Italian Association of Equine Veterinarians CongressCabinet VeterinarNo ratings yet
- Diagnostic Methods For Evaluation of Stallion Subfertility - A Review PDFDocument16 pagesDiagnostic Methods For Evaluation of Stallion Subfertility - A Review PDFalejandro sotoNo ratings yet
- Infertility IIDocument58 pagesInfertility IIdr_asalehNo ratings yet
- NCM 109 SKILLS LAB DAY 1 Laboratory and Diagnostics22Document55 pagesNCM 109 SKILLS LAB DAY 1 Laboratory and Diagnostics22Joseph DusichNo ratings yet
- Natural Family Planning: An Update: Canadian Family Physician Médecin de Famille Canadien September 1986Document8 pagesNatural Family Planning: An Update: Canadian Family Physician Médecin de Famille Canadien September 1986Analie GuirhemNo ratings yet
- Semen TransesDocument4 pagesSemen TransesElijah Mae MundocNo ratings yet
- Jurnal Internasional - ServiksDocument9 pagesJurnal Internasional - ServiksAnggita MelaniNo ratings yet
- Semen AnalysisDocument9 pagesSemen AnalysisGlydenne Glaire Poncardas GayamNo ratings yet
- Nerves DistributionDocument9 pagesNerves Distributiondeargrace2512No ratings yet
- Keys2012 6Document5 pagesKeys2012 6TRIANDINI TRIANDININo ratings yet
- The Undescended Testis: A.E. MackinnonDocument4 pagesThe Undescended Testis: A.E. MackinnonAin GhazaliNo ratings yet
- Ovarian Ultrasonography and Follow of Estrus in The Bitch and QueenDocument8 pagesOvarian Ultrasonography and Follow of Estrus in The Bitch and QueenTere GarzónNo ratings yet
- Exfoliative Vaginal Cytology and Vaginal Acidity Profile in Ettawa-Saanen Grade DoesDocument16 pagesExfoliative Vaginal Cytology and Vaginal Acidity Profile in Ettawa-Saanen Grade DoesAndi Khuswatul Khazanah RNo ratings yet
- Alakeshbarman Zoology PG 2nd FertilizationDocument28 pagesAlakeshbarman Zoology PG 2nd Fertilizationouafia liiamaniNo ratings yet
- Seminal Fluid AnalysisDocument11 pagesSeminal Fluid AnalysisKenneth Jake BatiduanNo ratings yet
- Implantación Endometrial - GenéticaDocument9 pagesImplantación Endometrial - GenéticaMaríaJoséPinedaNo ratings yet
- Macleod 1Document8 pagesMacleod 1rakibhossainNo ratings yet
- Sperm Test and Semen Analysis Semen AnalysisDocument2 pagesSperm Test and Semen Analysis Semen Analysismahendra_choudhary07No ratings yet
- A Fertility PlanningDocument7 pagesA Fertility PlanningSHAHADANo ratings yet
- A Practical Approach To Testicular BiopsyDocument8 pagesA Practical Approach To Testicular BiopsyNazaqat FarooqNo ratings yet
- Pregnancy TestDocument10 pagesPregnancy TestquerokeropiNo ratings yet
- Segmental Cervical Aplasia in A Colombian Creole Mare X Chromosome Aneuploidy 2021Document7 pagesSegmental Cervical Aplasia in A Colombian Creole Mare X Chromosome Aneuploidy 2021Laura VillotaNo ratings yet
- 0091-2182 2885 2990126-0 PDFDocument1 page0091-2182 2885 2990126-0 PDFParahmitaNo ratings yet
- Bovine Reproductive Ultrasound GuideDocument16 pagesBovine Reproductive Ultrasound GuideRuben Gutierrez-ArizacaNo ratings yet
- Canine ReproductionDocument30 pagesCanine Reproductionwindi nurhidayahNo ratings yet
- Ajacm 2009 4 (1) Acup Improve EndometrDocument7 pagesAjacm 2009 4 (1) Acup Improve EndometrdirkvandeweyerNo ratings yet
- Sperm PreparationDocument10 pagesSperm Preparationcarlosdanielrc1983No ratings yet
- Experiment No. 8Document2 pagesExperiment No. 8Jenny Acosta CatacutanNo ratings yet
- Inverted Nipples PDFDocument2 pagesInverted Nipples PDFfifahcantikNo ratings yet
- Nipple Pain in Breastfeeding Mothers Incidence, Causes and TreatmentsDocument17 pagesNipple Pain in Breastfeeding Mothers Incidence, Causes and TreatmentsDianVitasariNo ratings yet
- Anorectal Manometry Patient Information 8-5-2005Document2 pagesAnorectal Manometry Patient Information 8-5-2005fifahcantikNo ratings yet
- JDS 392Document10 pagesJDS 392fifahcantikNo ratings yet
- Surgical Management For Hirschsprung Disease A.4Document6 pagesSurgical Management For Hirschsprung Disease A.4fifahcantikNo ratings yet
- Inverted Nipples PDFDocument2 pagesInverted Nipples PDFfifahcantikNo ratings yet
- Nephroblastoma: Radiological and Pathological Diagnosis of A Case With Liver MetastasesDocument5 pagesNephroblastoma: Radiological and Pathological Diagnosis of A Case With Liver MetastasesfifahcantikNo ratings yet
- Wilms TumourDocument3 pagesWilms TumourfifahcantikNo ratings yet
- 560 FACTORS AFFECTING THE CERVICAL MUCUS CRYSTALLIZATION THE SPERM SURVIVAL IN CERVICAL MUCUS AND PREGNANCY RATES OF HOLSTEIN COWS en PDFDocument8 pages560 FACTORS AFFECTING THE CERVICAL MUCUS CRYSTALLIZATION THE SPERM SURVIVAL IN CERVICAL MUCUS AND PREGNANCY RATES OF HOLSTEIN COWS en PDFfifahcantikNo ratings yet
- ErgonomicDocument23 pagesErgonomicAmalia PutriNo ratings yet
- Rabu, 20 Jul 2016Document32 pagesRabu, 20 Jul 2016nur_betaNo ratings yet
- Visite BesarDocument3 pagesVisite BesarfifahcantikNo ratings yet
- Cornea/External Disease Summary Benchmarks For Preferred Practice Pattern® GuidelinesDocument12 pagesCornea/External Disease Summary Benchmarks For Preferred Practice Pattern® GuidelinesfifahcantikNo ratings yet
- Layers of HeartDocument4 pagesLayers of HeartfifahcantikNo ratings yet
- The Effects of Violent Video Games Research Paper English Comp2Document11 pagesThe Effects of Violent Video Games Research Paper English Comp2api-451442670No ratings yet
- Village Survey Form For Project Gaon-Setu (Village Questionnaire)Document4 pagesVillage Survey Form For Project Gaon-Setu (Village Questionnaire)Yash Kotadiya100% (2)
- Rooftop Rain Water Harvesting in An Educational CampusDocument9 pagesRooftop Rain Water Harvesting in An Educational CampusAkshay BoratiNo ratings yet
- Basics of Fire SprinklerDocument21 pagesBasics of Fire SprinklerLeo_1982No ratings yet
- Ds0h Ufaa68 ProposalDocument11 pagesDs0h Ufaa68 Proposaledward baskaraNo ratings yet
- Oil ShaleDocument13 pagesOil Shalergopi_83No ratings yet
- Fast FashionDocument9 pagesFast FashionTeresa GonzalezNo ratings yet
- Comparison and Contrast Essay FormatDocument5 pagesComparison and Contrast Essay Formattxmvblaeg100% (2)
- Employee Final SettlementDocument1 pageEmployee Final SettlementZeeshan Mirza0% (1)
- Heteropolyacids FurfuralacetoneDocument12 pagesHeteropolyacids FurfuralacetonecligcodiNo ratings yet
- J130KDocument6 pagesJ130KBelkisa ŠaćiriNo ratings yet
- Contractor: Item No. MRS-1st 2021 Ref. Description Unit Quantity Rate of Contractor Unit Rate in Words AmountDocument1 pageContractor: Item No. MRS-1st 2021 Ref. Description Unit Quantity Rate of Contractor Unit Rate in Words AmountusmanaliNo ratings yet
- QA-QC TPL of Ecube LabDocument1 pageQA-QC TPL of Ecube LabManash Protim GogoiNo ratings yet
- Turning Risk Into ResultsDocument14 pagesTurning Risk Into Resultsririschristin_171952No ratings yet
- Chemical Quick Guide PDFDocument1 pageChemical Quick Guide PDFAndrejs ZundaNo ratings yet
- Flame Retardant and Fire Resistant Cable - NexansDocument2 pagesFlame Retardant and Fire Resistant Cable - NexansprseNo ratings yet
- Method StatementDocument29 pagesMethod StatementZakwan Hisyam100% (1)
- Dr. Nastiti K - Manajemen Asma Pada Anak 2018 PDFDocument72 pagesDr. Nastiti K - Manajemen Asma Pada Anak 2018 PDFagnesspratiwiNo ratings yet
- Parche CRP 65 - Ficha Técnica - en InglesDocument2 pagesParche CRP 65 - Ficha Técnica - en IngleserwinvillarNo ratings yet
- Thesis ProposalDocument19 pagesThesis Proposaldharmi subedi75% (4)
- 7 UpDocument3 pages7 UpRajeev TripathiNo ratings yet
- 6 Kuliah Liver CirrhosisDocument55 pages6 Kuliah Liver CirrhosisAnonymous vUEDx8100% (1)
- 6Document2 pages6Min Hsuan HsianNo ratings yet
- Riber 6-s1 SP s17-097 336-344Document9 pagesRiber 6-s1 SP s17-097 336-344ᎷᏒ'ᏴᎬᎪᏚᎢ ᎷᏒ'ᏴᎬᎪᏚᎢNo ratings yet
- Lesson 1 - Intro To Highway EngineeringDocument15 pagesLesson 1 - Intro To Highway EngineeringSaoirseNo ratings yet
- Psychoanalysis AND History: Freud: Dreaming, Creativity and TherapyDocument2 pagesPsychoanalysis AND History: Freud: Dreaming, Creativity and TherapyJuan David Millán MendozaNo ratings yet
- Mainstreaming Gad Budget in The SDPDocument14 pagesMainstreaming Gad Budget in The SDPprecillaugartehalagoNo ratings yet
- Task 5 Banksia-SD-SE-T1-Hazard-Report-Form-Template-V1.0-ID-200278Document5 pagesTask 5 Banksia-SD-SE-T1-Hazard-Report-Form-Template-V1.0-ID-200278Samir Mosquera-PalominoNo ratings yet
- Procedure FireDocument28 pagesProcedure FireRichard D DuNo ratings yet
- Chemical Engineering Projects List For Final YearDocument2 pagesChemical Engineering Projects List For Final YearRajnikant Tiwari67% (6)