Professional Documents
Culture Documents
Call A Case 5 PD
Uploaded by
api-383594492Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Call A Case 5 PD
Uploaded by
api-383594492Copyright:
Available Formats
Student
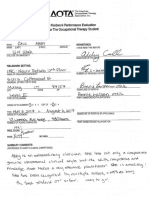
Name: Abby Call Case: Charlie Date: 3/27/2017
1. Diagnosis, Referral, Setting, Reimbursement, LOS
-DX: Parkinsons disease,
-Secondary DX: bilateral cataracts
-Referral: Physician
-Setting: Transitional rehab
-Reimbursement: Medicare
-LOS: 10 days
2. Pragmatic Factors to Consider
-Fractured left wrist; he will have cast on left UE for 6 weeks
-Lives alone
-Widower; wifes death 3 years ago
-LOS: Only 10 days are paid for by Medicare
-Relationship with daughter (& other family members), there is a disconnection between their stories.
Is he telling the truth? Is she telling the truth? Or does she just want money from his muscle car
-Secondary DX of bilateral cataracts
-Possibility of cognitive deficits
-PD symptoms; i.e. tremors, bradykinesia, depression
3. Context: Occupational Profile & Current Occupations
Cultural: Western culture of independent and individualism, his culture of friends meeting for
coffee and lunch every day, being capable to taking care of himself at home up until
this point both physically and financially, being a pet owner (beagle goes everywhere
with him)
Physical: Lives in a house, restored muscle car, garage, tools, driveway, the transitional rehab
room and bathroom, the rehabs dining area and hallways, the rehabs outside
grounds/gardens
Social: Widower, pet beagle named Boyd, the gang 4-6 buddies he meets for coffee and
lunch, daughter Lona, Charlies house cleaner; while at the rehab center-other patients,
staff, therapists, doctors
Personal: 72 year old male, retired electrician
Temporal: 10 days in transitional rehab, 6 weeks with cast on LUE, wifes death 3 years ago,
diagnosed and living with Parkinsons Disease, PD symptoms recently have increased
Virtual: Watches Wheel of Fortune and other TV, tinkers/fixes small appliances, interested in
computers but has no experience
Page 1 of 12 Revised 1/9/17
Prior Occupations: Independent in all ADL, financial management, simple meal prep and cooking,
driving, pet care. He has a house cleaner come in once a week to clean home and do laundry.
Independent with social interactions (meets friends for coffee and lunch). Restoring muscle car,
tinkers with things to try to get them working, fixes small appliances, reads newspaper
Current Occupations: Independent with grooming, Min A with bathing with use of shower chair
required assistance with transfer and LB washing, Mod A to cover cast prior to shower, Min A with
UB dressing and Mod A with LB dressing, Independent with self-feeding
4: Top Three Client/Family Goals and Priorities
1. Tool use to work on car/projects
2. Reading
3. Bathing
5. Diagnosis and Expected Course 6. Scientific Reasoning & Evidence
List the barriers to performance typical of this diagnosis:
DX: Parkinsons Disease
Barriers to performance: Tremors, bradykinesia, stiffness
PD is a chronic, idiopathic, progressive in joints and muscles, postural instability, weakness and
neurodegenerative disorder of the central fatigue, possible cognitive deficits, possible hallucination
nervous system characterized by damage to and delusions, depression, and flat affect
dopamine-producing brain cells. Primary
symptoms are: Treatment:
-Tremors at rest -Medication (used to increase dopamine levels in the
-Bradykinesia brain, influence neurotransmitters to ease symptoms of
-Stiffness/rigidity of arms, legs, or trunk PD such as tremor, also to treat non-motor symptoms
-Postural instability such as anxiety and depression).
-Gait changes (stride length, speed) often -Therapies (OT, PT, and ST)
characterized as shuffling gait -Surgery (PD that has progressed to the point wherein
-Masked face w/ decreased facial expression medications are no longer effective)
-Depression 50%
-Some individuals with PD can experience OT Interventions:
psychosis, such as hallucinations and delusions -Adaptive equipment to increase safety and
-Cognitive deficits: visual-spatial perception, independence with ADL, IADL, and leisure activities.
difficulty shifting attention among various -Compensatory strategies and techniques for medication
stimuli, processing simultaneous information. management, bathing, dressing, and meal prep, etc.
-Facilitate joint movement, maintain ROM, and prevent
Other symptoms possible with PD: autonomic contractures
dysfunction, dysphagia, dysarthria, bowel and -Improve motor planning and increase speed through
bladder problems such as constipation and adding cues; such as music with beats.
urgency of urination, orthostatic hypotension -Group interventions can improve the clients perception
(syncope is rare), some patients report abnormal of capacities and self-esteem.
tolerance of heat and cold, speech volume -Suggest home modification to increase safety
decreased and is monotone. -Suggest task modification to increase participation
Page 2 of 12 Revised 1/9/17
-Promote engagement in productive activities and leisure
A person diagnosed with PD may live an activities within the just right challenge.
additional 20 to 30 years, with a slow -Education client and family regarding support groups
progressive loss of motor function. and other community resources.
PD is categorized by the severity of the disease References:
based on Hoehn and Yahr staging system. -Pedrettis Occupational Therapy book
-Stage one: unilateral mild movement-related -Willard & Spackman Occupational Therapy book
symptoms. -Mayo Clinic; http://www.mayoclinic.org/diseases-
-Stage two: bilateral movement-related conditions/parkinsons-disease/basics/definition/con-
symptoms, balance intact 20028488)
-Stage three: mild imbalance during walking
and standing, moderately sever generalized
dysfunction but typically remains physically
independent.
-Stage four: motor symptoms are advanced and
severe, disabling instability while walking or
standing, the individual can no longer live
alone, changes in speech and swallowing are
apparent.
-Stage five: disease is severe and fully
developed; the individual is unable to stand or
walk and requires constant care.
7. Practice Models Guiding Rationale
Assessment and Treatment
1. PEO The PEO model postulates through improving the congruency
between the person, the environment, and the occupation, a persons
occupational performance is increased and improved. Using this
model I will focus on improving Charlies congruency though
activity and home modifications. Task modification can be achieved
through introducing adaptive equipment to reduce the task demands;
such as a button hook or sock aid. Environmental modifications to
Charlies home can be made to also reduce task demands; such as
shower chair, grab bars, and non-slip bath mats.
Page 3 of 12 Revised 1/9/17
2. Rehabilitation Model The rehabilitation model postulates with compensatory strategies
and techniques an individual can restore independence when the
underlying impairment cannot be remediated. Use of this model with
Charlie is appropriate because PD is a progressive neurodegenerative
disease. Some of the barriers Charlie experiences to his performance
cannot be remediated due to the nature of the disease. Therefore,
using this model I can focus on improving Charlies occupational
performance and increasing his participation and quality of life by
educated him on compensatory strategies and techniques that will
increase his independence. For example, energy saving techniques so
he can continue to participate in his occupations. Also,
compensatory strategies to help manage his medication and/or bills,
so he can continue being independent with those occupations.
3. Biomechanical Model This model postulates capacity for movement affects and is affected
by occupational performance. Therefore, to increase and maintain
Charlies occupational performance it is vital to increase his capacity
for movement; i.e. ROM, strength, and endurance. Furthermore, this
model states using whole tasks can positively affect and produce
change. Using the biomechanical model I can focus on increasing
Charlies muscle strength and endurance during meaningful
occupations; such as ADL, IADL, and leisure activities. We can
focus on strength and endurance for his morning routine, cooking
simple meals, caring for his pet, and tinkering with small appliances.
Also, focus on maintaining his ROM and facilitate joint mobility to
prevent contractures. Again, using a whole task that is meaningful to
Charlie; such as shoulder ROM during dressing and bathing, or wrist
ROM during tasks that require tools.
Page 4 of 12 Revised 1/9/17
8. Specific Areas of Occupation
What do you know? What do you need to know?
ADL: ADL:
-Grooming-Independent -Toileting. Level of dependence? Can he get on and off the toilet? He
-Bathing w/ AE-Min A for his safe when toileting? Does he use any adaptive equipment with
transfer and LB washing, Mod A toileting?
to cover cast prior to shower -Dressing, preferred clothing? State he usually wears slippers, but all
-UB Dressing-Min A (difficulty the time? Going out to meet friend?
with buttons) -Bathing, what AE does he have at home?
-LB Dressing-Mod A (donning -Feeding, what AE does he have for eating at home, if any?
socks) -Functional mobility, Is he safe to get around his home? Get around
-Feeding-Independent (frequently outside his home?
spilled food off silverware due to -Does he wear glasses? Can he care for them properly?
tremors)
IADL:
IADL: -Can he care for his pet beagle? Walk him? Bath him? Feed him?
-House cleaning-dependent (has -Can he use the telephone? Do his Parkinsons symptoms create any
house cleaner) barriers to dialing the phone? Do his cataracts create barriers to using
-Laundry-dependent (house the phone?
cleaner does laundry) -Is he safe to drive?
-Can he understand his bills? Pay them on time and correctly? Can he
manage is finances?
-Can he manage his medications? What medication is he taking? Does
he have any current strategies for medication management?
-Can he manage small cleaning around the house?
-Can he cook simple meals?
-Shopping, who does the grocery shopping?
Leisure:
-What are the barriers to using tools? Is it grip strength? ROM? Etc.
-Where does he tinker? In the garage? Is he sitting or standing? At a
work bench or table?
Social Participation:
-What kind of relationship does he have with daughter?
-Does he have any other close family members?
-How are his relationships with neighbors?
Page 5 of 12 Revised 1/9/17
9. Performance Skills
What do you know? What do you need to know?
-Has difficulty with transferring in and out or -How is his balance in sitting and in standing?
shower -Can he bend forward without losing balance?
-Difficulty with lower body washing -Can he reach his feet? Is it a flexibility issue?
-Difficulty with buttons -Can he grasp his socks? Can he grip the soap
-Difficulty with donning socks and/or washcloth?
-Frequently spilled food off silverware -Can Charlie manipulate buttons with fingers? Or
-At times drooled is it a visual issue?
-Requires extra time to complete ADL during to -How is Charlies endurance?
tremor and bradykinesia -Does he position his body safely when
-Difficulty covering cast prior to shower transferring?
-How is his cognition? Does he know the next
steps to take when performing an activity? Does
he gather the required items?
10. Performance Patterns-Habits, Routines, Rituals, Roles
What do you know? What do you need to know?
Routine/habits: awakes at 5am, in the morning he -How will his role as a pet owner affect
eats breakfast, gets dressed, retrieves the treatment?
newspaper and reads mostly the sports and -How will his family roles affect treatment?
weather sections, does projects around the house, -How long does it typically take for him to
sometimes naps, watches Wheel of Fortune. In complete morning routine?
the afternoon he drive into town for errand, meets
the gang for coffee and lunch at Daisys Cafe,
comes home for another nap. In the evening he
works on his car or thing around the house, eats
dinner, and then watches TV before bed.
Roles: father, friend, pet owners, retired
electrician, widow, patient in transitional rehab
Page 6 of 12 Revised 1/9/17
11. Activity Demands for the Client Goals and Priorities
What do you know? What do you need to know?
Heating up a bowl of soup in the microwave: -Does Charlie use a microwave at home? If yes,
-First step is to retrieve needed item; bowl, can of where is the microwave (on countertop, above
soup, can opener, spoon, and oven mitts countertop, etc.)?
-Next step is to open the can of soup using the -How is his kitchen set up? Is it a large area or
can opener. Skills required to open can of soup: small? How many steps does he need to take to
bilateral grasp (one hand holds can opener handle get the needed items to complete this activity?
and the other grasps and turns can opener knob), Does it have good lighting?
some UE strength, supination, pronation, wrist -What kind of can opener does he have at home?
extension, finger flexion and extension. Is it manual or electric? Does he find it difficult
-Once soup can is opened, next step is to pour to use?
soup into bowl. Skills required: grasping can, -What kind of bowls does he use at home?
shoulder and elbow flexion to lift can, pronation Plastic, porcelain, glass, etc.
to pour can into bowl. -Does Charlie like soup? Will he eat it at home?
-Next step is to carry bowl to microwave. Skills -Does he have the necessary strength in UE, LE,
required: grasping bowl, pushing microwave and trunk to care out activity
button to open door, placing bowl in microwave -Does he have the necessary endurance?
(could be on countertop requiring a slight bend or -Does he have the necessary ROM?
could be higher requiring a reach). -Does he have to needed cognitive skills to use
-Next step is to set microwave to proper time for microwave safely?
heating up soup. Skills required: vision, finger
dexterity, cognition
-This activity requires endurance, motor, sensory,
and cognition.
12. Client Factors- Values, Beliefs, Spirituality
What do you know? What do you need to know?
-Values his independence -Is he religious?
-Values his relationship with his pet beagle, Boyd -How does his believes influence his life?
-Charlie is eager to go home -How will his believes and values influence his
-Values his work as an electrician, although therapy?
retired he continues to work on small appliances -Does he value his relationship with daughter?
and tinker with things at home.
-Carlie values his ability to use tools and continue
working on his muscle car and things around
the house. One the COPM using tools was is
number one priority
Page 7 of 12 Revised 1/9/17
13. Client Factors- Body Functions & Structures
What do you know? What do you need to know?
-Right-side tremors -Strength in LEs, UEs and trunk
-Bradykinesia -ROM in LEs, UEs
-Bilateral cataracts -Severity of cataracts/ current visual abilities
-FX left wrist -Pain level
-Right hand dominant -Balance (sitting, standing, dynamic, etc.)
-Gait changes? If yes, how are they affecting
performance and safety?
-Cognitive deficits?
-Psychosis? Any hallucinations, delusions?
-He is experience depression and/or anxiety?
-How long has he been living with PD?
14. Evaluation: What Assessment tools and other means of assessment will you use?
Top Down Assessment: Prioritize one Occupation to observe the client perform
Observed Occupation Rationale/How will you use this information
Meal prep: heating up a bowl of canned soup During my observation of Charlie preparing a
bowl of canned soup I would be gathering
information regarding his balance, fine and gross
motor, and endurance. Also, this activity will
give me insight into his cognition. Can he follow
simple directions? Can he attend to a task? Can
he gather all the needed items to prepare the bowl
of canned soup; i.e. bowl, can of soup, can
opener, spoon, towel or oven mitten (if bowl is
hot). Furthermore, this task will give me insight
into Charlies safety in the kitchen. Whether we
are heating the soup over the stove or in the
microwave, is Charlie safely preforming this
task?
Method/Tool Rationale/What is being Assessed
1. SLUMS This assessment is a rapid cognitive screening
tool. It will provide insight into any cognitive
deficits Charlie might have. It assesses memory,
attention, conceptual thinking, executive
function, visuospatial, and orientation. This
assessment will give me indications into what
kind of cognitive deficits Charlie has, if any. If
necessary I can then further assess those
cognitive deficits to provide treatment.
Page 8 of 12 Revised 1/9/17
2. AROM This assessment will provide information about
Charlies range of motion against gravity in his
upper extremities. Also, this assessment will give
me information regarding any muscle rigidity.
3. Muscle Manual Testing This assessment will give me information
regarding Charlies muscle strength and
endurance in his upper extremities.
4. Jebsen Hand Function Test This assessment examines the fine motor skills,
in weighted and non-weighted hand function
activities during performance of ADL. The
assessment will provide information about
Charlies fine motor skills for writing, feeding,
handling small objects, and handling large light
and heavy objects. The Jebsen Hand Function
Test will give me information on how well
Charlie can performance ADL and some IADL
tasks; such as paying bills.
5. WHOQOL-BREF This assessment will provide information
World Health Organization Quality of Life regarding Charlies perceived quality of life. I
chose this assessment over the Geriatric
Depression Scale because it not only looks at
depression but also addresses personal goals,
standard, concerns, anxiety, cultural values, etc.
The WHOQOL-BREF will provide insight into
how Charlie feels about his personal abilities and
his social supports. Also, it might provide some
clues into how he feels about his relationship
with his daughter.
6. Cougar Home Safety Assessment The Cougar Home Safety Assessment examines
the safety of a clients home in the following
areas: fire hazards/carbon monoxide,
emergency/medical, electrical/water
temperatures, flooring/hallways, kitchen,
bedroom, bathroom(s), closets/storage areas,
parking, entrances, and disaster preparedness. It
would be good to evaluation Charlies home
environment before he is discharged to unsure he
is safe to return home and can continue to
participate in his ADL, IADL, and leisure
occupations.
Page 9 of 12 Revised 1/9/17
15. CPT Evaluation Code: Justification
97166 Charlies evaluation would be moderate complexity because he has
Moderate Complexity multiple diagnoses to consider during treatment; Parkinsons Disease,
FX of left wrist, and bilateral cataracts. Further, upon evaluation
Charlie has 3-5 performance deficits to consider; multiple physical
deficits, possible cognitive deficits. Lastly, when making clinical
decisions to treat Charlie I need to consider several treatment options to
address the different performance deficits, diagnoses, etc. Also, there is
a concern of his relationship with his family and if they are truly
supportive or have alternate agendas. This increases the complexity to
treat Charlie, because it is another angle to consider when making
clinical decisions.
16. Projected Outcomes Type of Outcome
I anticipate Charlie to increase his participation and improve his -Occupational Performance
performance in ADL, IADL, and leisure activities. Furthermore, I -Participation
anticipate him to increase is role competence as a friend, father, -Quality of Life
home owner, and pet owner. I expect Charlies quality of life to -Role competence
improve through increasing his participation and performance in
occupations; especially with self-care tasks, pet care tasks, and
leisure tasks. I also anticipate his quality of life to improve through
the improvements made in his role competence.
17. Resources and Team Members
Resources:
-Provide information about community support groups and therapy groups for people with PD.
-Provide Charlie with any adaptive equipment he might need for reducing task demands and/or
making his home a safer environment.
-Provide family with education material to take home regarding PD. Also, provide the follow website
for the Parkinsons Disease Foundation and Parkinsons Resource Organization to Charlie and his
family if theyd like to do further research on the disease (http://www/pdf.org, &
http://www.parkinsonsresouces.org).
Team Members: Physical therapy, Nursing, CNAs, Doctors, Rehab aides, Speech therapy, Charlies
family members (Daughter Lona)
18. Intervention Plan
Barriers Supports
-FX left wrist; with cast for 6 weeks -Friends
-Bilateral cataracts -Pet beagle, Boyd
-Tremor -His passion for tinkering and fixing
Page 10 of 12 Revised 1/9/17
-Bradykinesia things
-Short LOS (only 10 days) -Eager to return home
-Lives alone -Previous to transitional rehab was
-Family support? Agenda? (Daughter believes differently than living independent
Charlie about his capabilities, how much of this is the truth and -He has several hobbies and interest
how much is an agenda to get money from him?) Sounds like (reading, TV, working on his car,
she infrequently sees Charlie. fixing small appliances)
Goals Practice Model for each goal
1. LTG: At discharge, client will bath/shower independently PEO, Rehab model, Biomechanical
with use of adaptive equipment.
1a.STG: In 8 days, client will demonstrate increased endurance PEO, Biomechanical
and balance by transferring into shower with standby assist for
safety
1b.STG: In 6 days, client will demonstrate increased range of PEO, Biomechanical, Rehab model
motion by washing his lower body with setup assist and use of
adaptive equipment.
2. LTG: At discharge, client will dress lower body in preferred PEO, Rehab model
clothing independently using compensatory strategies.
2a. STG: In 7 days, client will don preferred pants PEO, Rehab model
independently using adaptive equipment and compensatory
strategies.
2b. STG: In 3 days, client will don socks using adaptive PEO, Rehab model
equipment with min assist.
3. LTG: At discharge, client will independently prepare simple PEO, Biomechanical
hot meal using microwave.
3a.STG: In 8 days, client will demonstrate increased endurance PEO, Biomechanical
when standing and walking by completing countertop task in
kitchen for 10 minutes without rest break.
3b. STG: In 5 days, client will demonstrate improved strength PEO, Biomechanical
in hand by opening jar independently.
Page 11 of 12 Revised 1/9/17
19. Treatment Sessions: Plan for first two 45 minute treatment sessions:
1. What will you do? Identify Based on which
Approaches goal(s)?
-For this first treatment session I want to focus on
Charlies trunk stability, ROM, strength and endurance. -Establish 1&2
-First, I would have him sitting at edge of bed. I would -Restore
have 10-15 different size and weight dog toys in a basket -Modify
placed 5-10 inches off the floor on Charlies right side.
He will reach down with his RUE, grasp a dog toy with
right hand, sit up straight, twist trunk and place toy into a
basket sitting on a chair to his left.
-Next, the exercise will be reversed. The toys will be
placed in a basket placed 5-10 inches off the floor to his
left side. He will reach down with LUE, grasp toy, sit up
straight, twist trunk and place toy into a basket placed on
a chair to his right.
-This activity will target Charlie trunk control, sitting
balance, ROM, UB strength, and endurance. It facilitates
reaching down toward LE, rotating and balancing his
trunk; which are needed skills for LB dressing and
bathing.
2. What will you do? Identify Based on which
Approaches goal(s)?
-For this next treatment session I want to focus on
Charlies endurance, ROM, strength and core stability. -Establish 3
This activity also works his cognition. -Restore
-First, because Charlie enjoys working with tools I would -Maintain
use a wood board with various items on it to practice
different hand tool use (bolt, screws, etc.); the board
would have 5-6 different items. I would give a picture of
how I wanted the items arranged on the board to Charlie
and ask him to make his board look like mine. He would
need to decide on the appropriate tool to use to take off
the item and then place it back on the board in the proper
location; i.e. Phillips screwdriver, socket wrench, etc.
-Ideally this activity will be done in standing; however
depending on how Charlie is doing it may need to be
done while seated. This is one way I could grade the
activity to fit the just right challenge for Charlie.
-This activity will target Charlies UB strength and
ROM. It also works on his fine motor coordination and
manipulation. Furthermore, it targets his cognition
through having to look at the picture, decide where the
objects need to be placed, decide which hand tool is
appropriate, etc.
Page 12 of 12 Revised 1/9/17
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Textbook of Personality DisordersDocument618 pagesTextbook of Personality DisordersCátia Ramos100% (10)
- Call A PDTDocument2 pagesCall A PDTapi-383594492No ratings yet
- Call A Soap Note 5Document2 pagesCall A Soap Note 5api-383594492No ratings yet
- Discharge SummaryDocument2 pagesDischarge Summaryapi-338566712No ratings yet
- Call A Obpp CompleteDocument35 pagesCall A Obpp Completeapi-383594492No ratings yet
- Fieldwork Level IIDocument7 pagesFieldwork Level IIapi-383594492No ratings yet
- Evidencebasedpaper HandwritingDocument12 pagesEvidencebasedpaper Handwritingapi-383594492No ratings yet
- Achieving Sustainability in Reducing Unplanned Extubations in PICUDocument7 pagesAchieving Sustainability in Reducing Unplanned Extubations in PICUKevin Bazán TorrealvaNo ratings yet
- Stewardship White PaperDocument21 pagesStewardship White PaperHosam GomaaNo ratings yet
- MPDS Codes PDFDocument19 pagesMPDS Codes PDFjared999No ratings yet
- Waksman 2018Document7 pagesWaksman 2018harry pribadiNo ratings yet
- H1N1 Swine FlupptDocument28 pagesH1N1 Swine FlupptDr. Hesham Zaatar100% (1)
- Löfgren's SyndromeDocument1 pageLöfgren's SyndromeLakshya J BasumataryNo ratings yet
- Pathophys CH 9Document48 pagesPathophys CH 9ErnestNo ratings yet
- Teaching Students With Autism Spectrum DisordersDocument155 pagesTeaching Students With Autism Spectrum DisordersAnonymous Pj6Odj0% (1)
- Discharge PlanDocument1 pageDischarge PlanGail GenturalezNo ratings yet
- Medico Graph I A 123Document124 pagesMedico Graph I A 123Rafael CastilloNo ratings yet
- Delusional Jealusy - FullDocument17 pagesDelusional Jealusy - FullnicolasNo ratings yet
- MidazolamDocument2 pagesMidazolamDesireemae Riosa-Candaroma100% (6)
- 1cardiovascular and Pulmonary Physical TherapyDocument347 pages1cardiovascular and Pulmonary Physical TherapyLiviu CuvoiNo ratings yet
- Health Hazards of Chemicals Commonly Used On Military BasesDocument35 pagesHealth Hazards of Chemicals Commonly Used On Military Basesmale nurseNo ratings yet
- Chagrin Factor - Feinstein1985Document3 pagesChagrin Factor - Feinstein1985Rafael MartinsNo ratings yet
- Medical Emergencies in OSDocument62 pagesMedical Emergencies in OSAditi RapriyaNo ratings yet
- Health PromotionDocument10 pagesHealth PromotionReyta NoorNo ratings yet
- Neurology Board Review MsDocument17 pagesNeurology Board Review Mssucca07No ratings yet
- Head TraumaDocument22 pagesHead TraumaSana RaniNo ratings yet
- Malaria: Definition: Infection Due To PlasmodiumDocument17 pagesMalaria: Definition: Infection Due To PlasmodiumCLEMENTNo ratings yet
- 2014 Final With Answers: 10000 SeriesDocument36 pages2014 Final With Answers: 10000 SeriesMareeswaranNo ratings yet
- Indonesia Health SectorDocument84 pagesIndonesia Health SectorBung RandiNo ratings yet
- Thrombosis Research: Letter To The Editors-in-ChiefDocument3 pagesThrombosis Research: Letter To The Editors-in-ChiefRia GandaNo ratings yet
- Cesarean Delivery: Postoperative Issues - UpToDateDocument12 pagesCesarean Delivery: Postoperative Issues - UpToDateZurya UdayanaNo ratings yet
- The Poppelreuter Figure Visual PerceptualDocument4 pagesThe Poppelreuter Figure Visual PerceptualIcaroNo ratings yet
- Knee Osteoarthritis: Steriods Verus Platelets Rich Plasma EffectivenessDocument5 pagesKnee Osteoarthritis: Steriods Verus Platelets Rich Plasma EffectivenessInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Report 8b3a3101Document11 pagesReport 8b3a3101Pooja AgarwalNo ratings yet
- Guideline of Record-KeepingDocument9 pagesGuideline of Record-KeepingGen LCNo ratings yet
- Respiratory DiseasesDocument2 pagesRespiratory Diseasessarguss14No ratings yet