Professional Documents
Culture Documents
Study and Evaluation of The Various Cutaneous Adverse Drug Reactions in Kasturba Hospital Manipal 2006
Uploaded by
David HCOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Study and Evaluation of The Various Cutaneous Adverse Drug Reactions in Kasturba Hospital Manipal 2006
Uploaded by
David HCCopyright:
Available Formats
www.ijpsonline.
com
Research Paper
Paper
Study and Evaluation of the Various Cutaneous
Various
Adverse Drug Reactions in Kasturba Hospital,
Manipal
S. GHOSH, LEELAVATHI D. ACHARYA 1 * AND PADMA G. M. RAO
1
Department of Pharmacy Practice, Manipal College of Pharmaceutical Sciences, MAHE, Manipal-576 104, India.
The present study emphasizes on implementation of the adverse drug reaction reporting and monitoring system,
in the Dermatology department of Kasturba Hospital, Manipal, by a clinical pharmacist, using different promotional
activities. Documented adverse drug reactions were assessed and analyzed for incidence, purpose of visit, types,
drug classes, individual drug causing adverse drug reactions, type of cutaneous reaction, and various predisposing
factors. Management and outcome of the adverse drug reactions were also studied. Adverse drug reactions were also
assessed for causality, using Naranjo’s scale, severity, and preventability, using Hartwig et al. scale. Adverse drug
reaction attributes to 77% of the hospital visit. Incidence of reported cutaneous adverse drug reactions, were
2.85%. Majority of the adverse drug reactions (96%) were of type B. Antibiotics (30%), were the common class of
drugs, causing a cutaneous adverse drug reactions. Maximum number of adverse drug reactions were due to
Acetaminophen, Amoxicillin, antitubercular drugs, and Phenytoin. Most of the adverse drug reactions were managed
by withdrawal of drug (81%), and 58% patients were recovered from the reaction. Naranjos scale classifies, 29 as
probable, 21 as possible, and 3 as definite adverse drug reactions. Most of the adverse drug reactions were of
moderate severity, however 13 adverse drug reactions were severe. All the adverse drug reactions were probably
preventable on extreme caution.
Adverse drug reactions (ADRs) are unwanted or can occur, which constitute from 2.6 to 7% of all drug
unintended effects of drugs, which occur during proper reactions7.
use of a drug. The safe use of medicines is an important
issue for prescribers, pharmacists, nurses, regulatory Drugs, no matter how safe and efficacious, are always
authorities, the pharmaceutical industry, and the public. coupled with inescapable risk of adverse reactions. ADRs
Healthcare professionals have a responsibility to their are a cause of significant morbidity and mortality in
patients, who themselves are increasingly aware of the patients of all areas of healthcare today. It has been
problems associated with drug therapy. It is essential that estimated, that from one third to as high as one half of
the practicing pharmacist should have a thorough ADRs, are believed to be preventable4. The incidence
knowledge about the various adverse effects of the and severity of ADRs can be influenced by patient
drugs, including its predictability and reversibility, related factors like age, sex, concurrent diseases, genetic
frequency and severity, predisposing factors and factors, and drug related factors like type of drug, route
recognition, relationship to dosage, and duration of of administration, duration of therapy, and dosage. The
treatment and prevention 1. Adverse reactions are other important risk factors associated with adverse drug
responsible for a significant number of hospital reactions are gender, increased number of drug
admissions, among these, cutaneous ADRs (2 to 3%) are exposures, advanced age, length of hospital stay,and
one of the frequent reason for patients to visit the function of excreting organs1,5. Cutaneous ADRs are the
physicians2. Although majority of ADRs are minor most common among the various adverse reactions
reactions and are self limiting, sometimes severe and attributed by the drugs. Any skin disorder can be imitated,
potentially life threatening situations3 like Steven Johnson induced, or aggravated by drugs. The incidence of
Syndrome (SJS) and Toxic epidermal necrolysis (TEN) cutaneous drug reactions vary from 15 to 30%6. Studies
on the epidemiology of common cutaneous ADRs have
*For correspondence rarely been reported, since such studies can only be
E-mail: leela.da@manipal.edu successfully conducted in clinics of internal medicine,
212 Indian Journal of Pharmaceutical Sciences March - April 2006
www.ijpsonline.com
who employ consultant dermatologists and where there is of reaction, or near fatal reaction with any component of
a comprehensive or intensive ADR monitoring system. the drug. Thank you cards were issued to those
Such evaluation of ADR in dermatology are yet to evolve dermatologists who reported ADR, so as to encourage
in India. further reporting. All the documented ADRs were
analyzed for incidence, purpose of visit to the hospital,
Kasturba Hospital (KH), Manipal, a 1400 bedded tertiary types of ADRs, drug classes, and individual drug causing
care hospital, has already an established ADR reporting cutaneous reaction, association of cutaneous reaction with
and monitoring system, in different medicine units. Since drugs, predisposing factors, management and outcome of
most of the drugs causes cutaneous ADRs, there is a ADRs. ADRs were also assessed for causality using
need for reporting these ADRs by department of Naranjo‘s scale, severity and preventability, using
Dermatology, where cutaneous ADRs are referred and Hartwig et al. scale. Severity of the reported ADRs were
treated. The present study focuses on extending the assessed at various levels, ranging between 1 and 7.
ADR reporting and monitoring program to the Level 1 and 2 indicates mild, 3 and 4 as moderate, and
dermatology department, with the objective to implement level 5 and above, as severe ADRs.
ADR reporting and monitoring system in the department
of dermatology of Kasturba Hospital, Manipal; to RESULTS AND DISCUSSION
categorize and analyze the reported cutaneous ADRs,
which were reported during the study period; to evaluate Implementation of ADR reporting and monitoring system
the management and outcome of ADRs; and to assess the in the Dermatology department was successfully done by
causality, severity and preventability of the reported displaying the posters, through oral campaign, and formal
cutaneous ADRs, using different scales. speeches related to importance of reporting ADRs,by the
clinical pharmacist. There were 53 ADRs reported,
MATERIALS AND METHODS during study period of six months.
The present study was a prospective one, conducted in A total number of 1859 patients visited the dermatology
the dermatology department of KH Manipal, for a period department, during the study period. Among these,
of six months, between November 2002 and April 2003. 53(2.85%) patients, either visited the hospital with already
All the inpatients and the outpatients who visited the developed ADRs, or developed ADR during their stay in
department during the study period, were monitored for the hospital. This shows a similar pattern of results, as
ADRs. Patient case notes/files and suspected ADR reported by Michael Bigby8. Out of the total ADRs
notification forms were used as main sources of data reported, 53% involved outpatients, and the remaining
collection. For the study purpose, the following 47% were inpatients. Significant differences were
documents were used. Suspected ADR notification form, observed in the reaction pattern, drugs involved, and
ADR reporting and documentation form, ADR alert card, severity between these two group of patients. The
Thank you card, Causality assessment scale (Naranjo’s reason for admission in most of the in-patients, were
scale)15, Severity assessment and Preventability assessment found to be ADRs, and they were of severe category.
scale (Hartwig et al. scale)14.
It was observed that 41 (77%) patients visited the hospital
The clinical pharmacist who was posted in the due to ADRs. The other reasons, were due to various
dermatology department, used to take part in the ward diseases like epilepsy in 4 (8%) cases, 1 (2%) each of
rounds along with other dermatologists, and actively breast cancer, end-stage renal disease (ESRD), renal cell
monitor for any ADRs. To strengthen the awareness of calculi, squamous cell carcinoma, and tuberculosis. Three
the ADR reporting system posters were displayed, oral cases could not be evaluated.
campaign, and formal speeches about the importance of
reporting ADRs, were done. On intimation of suspected According to Rawlins and Thompson’s classification,1
ADRs by the dermatologist, the notification form was filled ADRs were grouped into 2 types. The majority of the
up by the pharmacist, and the case was followed up for ADRs 51 (96%), were of Type B, since these reactions
further details, and were documented in the ADR were totally aberrant effects that are not to be expected
reporting and documentation forms. ‘ADR alert card ‘ was from the known pharmacological actions of a drug, when
given to the patients who exhibited hypersensitivity type given in the usual therapeutic doses to a patient, whose
March - April 2006 Indian Journal of Pharmaceutical Sciences 213
www.ijpsonline.com
body handles the drug in the normal way. The remaining carbamazepine (1). The other most common skin reactions
2 (4%) ADRs belonged to Type A, since these reactions were fixed drug eruption (5), urticaria (5), SJS (4),
were the result of an exaggerated, but otherwise normal, hyperpigmentation (3), pruritis (2), angioedema (2), and
pharmacological action, of a drug given in usual acne (2).
therapeutic doses.
Out of 53 ADRs, 20 reported cases had predisposing
Most frequently reported cutaneous drug reactions were factors. Among these, the most common was history of
for antibiotics in 16 (30%) cases, followed by allergy of the patient (7). Other risk factors involved,
antiepileptics in 13 (25%) cases, antitubercular drugs in 6 were inconcurrent disease (3), pharmacokinetic variables
(11%) cases, and antipyretics in 5 (9%) cases. Some of (3), multiple drug therapy (4), and pharmaceutical factors
the other drug classes involved, were steroids and (1). Whenever the patient had severe ADR to the
ayurvedic medicines, with 2 (4%) cases each, etc. Studies particular drug, ‘ADR alert card ‘ was given to the
conducted by Bern et al., Faich et al. and Bigby et al. patient, and they were asked to produce the same, while
shows similar results, antibiotics as the most frequent cause visiting the physician or pharmacist in the future.
of adverse skin reactions reported in their spontaneous
surveillance 9,10 , or hospital incidence system 2 . Most of the ADRs were managed by the withdrawal of
Antiepileptics have also been well known as a causative the drug in 43 (81%) cases. The remaining 10 patients
agent for a wide spectrum of dermatological ADRs11. continued on the same drug, without any major changes.
However, in these cases, reaction may or may not be
It was observed, that the drugs which caused maximal continuing. It was the dermatologist’s discretion, whether
undesired effects were acetaminophen, amoxicillin, anti the benefit of the drug overweighed the existing ADR.
tubercular drugs [ATT (isoniazid, rifampicin, The final outcome of the dermatological ADRs were that,
pyrazinamide, ethambutol)] (6 each), and phenytoin (5). 58% of patients recovered from the reaction, and 17%
Studies conducted by Bigby et al. showed that penicillins had it continuing on them. The fate of 23% of patient
and aminopenicillins were involved with the highest were not known, while there was one death reported,
incidence of cutaneous ADRs.2 In the study conducted either due to the direct or indirect effect of the
by Naldi et al. acetaminophen was ranked 8 among drug,during the study.
common analgesics, to cause cutaneous reactions11. But,
the present study showed more number of dermatological To strengthen and further emphasize the validity of the
ADRs with acetaminophen. This may be related to the findings of the study, causality assessment was done by
common prescribing pattern and self-medication habits using Naranjo’s scale. Out of the 53 ADRs reported, 29
among the local population. Few of the adverse reactions ADR’s were probable, 21 ADR’s were possible, and 3
observed by our surveillance system, were not reported ADR’s were definite. It was emphasized that most of the
earlier in medical literature, like SJS (1), and erythematous reported ADRs were caused by the accused drug, and
lesion (1), induced by an ayurvedic drug (1), erythema not otherwise. Results are tabulated in Table 1.
elevatum diutinum (EED) to gatifloxacin (1), and
hyperpigmentation associated with moxifloxacin (1). On evaluation of the severity of ADRs by Hartwig et
al.,14 it was evident that most of the dermatological ADRs
The most common reaction observed, was maculopapular reported in the study, were of moderate severity. A total
rashes with an incidence of 11 (21%) cases. These of 13 ADRs came under the level 3, while 7 ADRs came
findings were similar to studies carried out by Kushwaha under level 4 (a), and 8 ADRs under level 4 (b). These
et al. and Naina et al., to evaluate the incidence of results demonstrate that most of the ADRs were moderate
dermatological ADRs12,13. In this study, the drug which in terms of severity. The dermatological patients were
was attributed to cause maximal number of maculopapular also exposed to higher rates of severity, with 13 ADRs
rashes, was amoxicillin (6). amoxicillin, which induced
maculopapular rash, is well documented in medical TABLE 1: CAUSALITY ASSESSMENT
literature, and there were very high reported incidences Probability scale Definite Probable Possible Unlikely
(5%)2. The second most common ADR, was erythematous Naranjo’s scale 3 29 21 0
skin lesion (8). This was more among patients treated with As per the Naranjo’s scale of causality assessment, ADRs were classified as
roxithromycin (2), and antiepileptics like phenytoin (1) and definite, probable, possible and unlikely.
214 Indian Journal of Pharmaceutical Sciences March - April 2006
www.ijpsonline.com
TABLE 2: SEVERITY ASSESSMENT
Severity levels Level 1 Level 2 Level 3 Level 4 (a) Level 4 (b) Level 5 Level 6 Level 7
No. of ADRs 3 8 13 7 8 13 0 1
Percentage of ADRs 6 15 24 13 15 25 0 2
As per the Hartwig et al. ADR severity assessment scale, level of severity of ADRs classified as level 1 to 7. Level 1 and 2 indicates mild, level 3, 4 (a) and 4
(b) as moderate, level 5, 6 and 7 as severe.
coming under level 5 category. The ADR, which came the department and Prof. C. Balachandran, unit head of
under this category, were mostly skin reactions like SJS, dermatology department, Kasturba Hospital, Manipal for
EM, and urticaria. The study also reported one death, their constant support and help during this study.
which was probably caused by ATT-induced erythma
multiforme (Major). Even though various incidences REFERENCES
support the finding that the most common ADRs are skin
reactions, there has been very less effort to curtail its 1. Beard, K., In: Lee, A., Eds., Adverse Drug Reactions, 1st Edn.,
severity. Reactions like SJS have a very high incidence Pharmaceutical Press, London, 2001, 1.
2. Bigby, M., Jick, S., Jick, H. and Arndt, K.A., J. Amer. Med.
of occurrence, and pose a significant risk to patient’s life. Assoc., 1986, 256, 3358.
It further emphasizes the importance of monitoring ADRs. 3. Lee, A. and Thomson, J., In: Lee, A., Eds., Adverse Drug Reactions,
Results are tabulated in Table 2. 1st Edn., Pharmaceutical Press, London, 2001, 19.
4. Barbara, S.M., In: Shargel, L., Eds., Comprehensive Pharmacy
Review, 4th Edn., Lippincott Williams & Wilkins, London, 2001, 416.
On evaluation of the chances of preventability (Hartwig 5. Edwards, I.R., In: Speight, T.M. and Nicholas, H.G., Eds., Avery’s
et al.) of the ADRs, it was evident that all the ADRs may Drug Treatment, 4th Edn., Adis International, 1997, 261.
6. Boston collaborative Drug Surveillance Program, Int. J.
have probably been preventable, if proper precautions Epidemiol., 1973, 2, 167.
were taken. 7. Roujeau, J.C., Kelly, J.P. and Naldi, L., N. Engl. J. Med., 1995,
333, 1600.
8. Bigby, M., Arch. Dermatol., 2001, 137, 765.
This study shows that ADRs attribute to a significant 9. Bern, J.I., Mann, R.D. and Rawlins, M.D., Brit. Med. J., 1998, 296,
percentage of hospital visits, in the dermatological 1319.
population. The mechanism behind most of the 10. Faich, G.A., Knapp, D., Dreis, M. and Turner, W., J. Amer. Med.
Assoc., 1987, 257, 2068.
dermatological ADRs was hypersensitivity reaction, and 11. Naldi, L., Conforti, A. and Venegoni, M., Brit. J. Clin.
was most commonly associated with antibiotics, analgesics, Pharmacol., 1999, 48, 839.
and antiepileptics. Maculopapular rash was the most 12. Kushwaha, K.P., Verma, R.B., Singh, Y.D. and Rathi, A.K., Indian
J. Pediatr., 1994, 61, 357.
common type of ADRs. Most of the reactions were of 13. Naina, H.H., Philip, A.N. and Dennis, P.W., In: Dipiro, T.J., Eds.,
moderate severity, and could be managed by the Pharmacotherapy; A Pathophysiologic Approach, 4th Edn., Appleton
withdrawal of the drug. and Lange, Stamford, Cannecticut, 1999, 1505.
14. Hartwig, S.C., Siege, l.J. and Schneider, P. J., Amer. J. Hosp.
Pharm., 1992, 49, 2229.
By implementing the ADR reporting and monitoring 15. Naranjo, C. A., Busto, U., Sellers, E. M., Clin. Pharmacol. Ther.,
system, the pharmacist can promote drug safety and better 1981, 30, 239.
patient care, among health care professionals.
Involvement of a pharmacist in patient care, can help in
prevention and early detection of ADRs.
Accepted 4 March 2006
ACKOWLEDGEMENTS Revised 18 July 2005
Received 22 July 2004
Indian J. Pharm. Sci., 2006, 68 (2): 212-215
The authors wish to thank Prof. S. D. Shenoy, Head of
March - April 2006 Indian Journal of Pharmaceutical Sciences 215
You might also like
- Dosage Form-Related Food Interaction Observed in A Marketed Once-Daily Nifedipine Formulation After A High-Fat American Breakfast - 2002Document2 pagesDosage Form-Related Food Interaction Observed in A Marketed Once-Daily Nifedipine Formulation After A High-Fat American Breakfast - 2002David HCNo ratings yet
- Amlodipine - C20H25ClN2O5 - PubChem PDFDocument72 pagesAmlodipine - C20H25ClN2O5 - PubChem PDFDavid HCNo ratings yet
- Timeline of History of Hypertension Treatment - 2016 PDFDocument14 pagesTimeline of History of Hypertension Treatment - 2016 PDFDavid HCNo ratings yet
- Drug Induced Muscle Disorders - 2009 PDFDocument7 pagesDrug Induced Muscle Disorders - 2009 PDFDavid HCNo ratings yet
- Cutaneous Adverse Drug Reactions - 2014 PDFDocument11 pagesCutaneous Adverse Drug Reactions - 2014 PDFDavid HCNo ratings yet
- Clinically Significant Pharmacokinetic Drug Interactions With Carbamazepine - SpringerLinkDocument42 pagesClinically Significant Pharmacokinetic Drug Interactions With Carbamazepine - SpringerLinkDavid HCNo ratings yet
- Efficacy and Safety of Alternate-Day Versus Daily Dosing of Statins - A Systematic Review and Meta-Analysis - SpringerLinkDocument23 pagesEfficacy and Safety of Alternate-Day Versus Daily Dosing of Statins - A Systematic Review and Meta-Analysis - SpringerLinkDavid HCNo ratings yet
- Herbal Medicines - Adverse Effects and Drug-Herb Interactionssarah Spiteri Staines B.Pharm PDFDocument5 pagesHerbal Medicines - Adverse Effects and Drug-Herb Interactionssarah Spiteri Staines B.Pharm PDFDavid HCNo ratings yet
- Pharmacist's Interventions in Reducing The Incidences of Drug Relatedproblems in Any Practice Setting - 2015Document8 pagesPharmacist's Interventions in Reducing The Incidences of Drug Relatedproblems in Any Practice Setting - 2015David HCNo ratings yet
- J. Biol. Chem. 1986Document6 pagesJ. Biol. Chem. 1986David HCNo ratings yet
- Medical BiochemistryDocument264 pagesMedical BiochemistryKarren Taquiqui PleteNo ratings yet
- Clinical Cases in CardiologyDocument343 pagesClinical Cases in CardiologyDavid HC50% (2)
- Mosby's Drug Reference For Health Professions, 4E (PDF) (Tahir99) VRG PDFDocument2,401 pagesMosby's Drug Reference For Health Professions, 4E (PDF) (Tahir99) VRG PDFDavid HC50% (2)
- Clinical Cases in CardiologyDocument343 pagesClinical Cases in CardiologyDavid HC50% (2)
- 1Document4 pages1David HCNo ratings yet
- A Handbook of Applied Statistics in Pharmacology - 2013Document226 pagesA Handbook of Applied Statistics in Pharmacology - 2013David HCNo ratings yet
- Mosby's Drug Reference For Health Professions, 4E (PDF) (Tahir99) VRG PDFDocument2,401 pagesMosby's Drug Reference For Health Professions, 4E (PDF) (Tahir99) VRG PDFDavid HC50% (2)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- CKD (F&e)Document110 pagesCKD (F&e)Al-nazer Azer Al100% (1)
- Torts Cases: I. Fe Cayao vs. Ramolete FactsDocument16 pagesTorts Cases: I. Fe Cayao vs. Ramolete FactsJana GonzalezNo ratings yet
- Opinion WritingDocument20 pagesOpinion WritingnirmalaNo ratings yet
- Wound MGMT Guidelines SEPTDocument93 pagesWound MGMT Guidelines SEPTYuda ArifkaNo ratings yet
- HSB Pneumonia Antibiotic AlgorithmDocument4 pagesHSB Pneumonia Antibiotic AlgorithmDr.Senthil KumarNo ratings yet
- Periodic Safety Update Reports: Adel Alrwisan B.SC, M.SC, PPCDocument16 pagesPeriodic Safety Update Reports: Adel Alrwisan B.SC, M.SC, PPCHala MohamedNo ratings yet
- OncologyDocument7 pagesOncologyaleks100% (1)
- Overview and Treatment Option: SkizofreniaDocument8 pagesOverview and Treatment Option: SkizofreniaEvi LoNo ratings yet
- PETUNJUK KHUSUS PILIHAN GANDADocument12 pagesPETUNJUK KHUSUS PILIHAN GANDARindah Tiara SariNo ratings yet
- Recording Neutral Zone.Document3 pagesRecording Neutral Zone.rekabiNo ratings yet
- Perioperative Management of AdrenalectomyDocument13 pagesPerioperative Management of AdrenalectomyTJ LapuzNo ratings yet
- Economics of Patient Safety - Acute Care - Final ReportDocument72 pagesEconomics of Patient Safety - Acute Care - Final ReportHanan AhmedNo ratings yet
- Memorandum of UnderstandingDocument3 pagesMemorandum of UnderstandingLionel MsuNo ratings yet
- Bronchiolitis Diagnosis Management and Prevention Pediatric Inpatient Emergency Department Guideline 20200810Document8 pagesBronchiolitis Diagnosis Management and Prevention Pediatric Inpatient Emergency Department Guideline 20200810Eduardo Rios DuboisNo ratings yet
- BGD Tutorial 2015 - Applied Embryology and TeratologyDocument10 pagesBGD Tutorial 2015 - Applied Embryology and TeratologyRendy YogaNo ratings yet
- Cdbb-Guide Vocal-Techniques EN PDFDocument17 pagesCdbb-Guide Vocal-Techniques EN PDFrox100% (1)
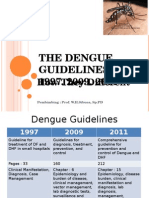
- Guideline Evolution for Diagnosis and Management of DengueDocument35 pagesGuideline Evolution for Diagnosis and Management of DengueFrinciaNo ratings yet
- Soyabean Milk Project Class 12Document18 pagesSoyabean Milk Project Class 12Sanjay Khandelwal0% (1)
- Thames Valley Y-Site Intravenous Drugs Compatibility ChartDocument2 pagesThames Valley Y-Site Intravenous Drugs Compatibility ChartА. СосорбарамNo ratings yet
- KaoshikiiDocument24 pagesKaoshikiiapi-238078813No ratings yet
- Shave 10 Hours Off Your WorkweekDocument50 pagesShave 10 Hours Off Your WorkweekDimitri PetrovNo ratings yet
- Mobile Games Addiction Corrupts OneDocument1 pageMobile Games Addiction Corrupts OnenanthiniNo ratings yet
- Ventilater CareDocument6 pagesVentilater CarehelenfreedaeqdNo ratings yet
- Y3TEBOOKDocument40 pagesY3TEBOOKayecim100% (14)
- Omega 85Document11 pagesOmega 85soorajssNo ratings yet
- Mystic Magazine August 1955 Issue 11Document70 pagesMystic Magazine August 1955 Issue 11Nikša StanojevićNo ratings yet
- Dr. Daniel Mok, Dr. Sibao Chen and Dr. Charmaine Tsang: Dept. of Applied Biology and Chemical TechnologyDocument43 pagesDr. Daniel Mok, Dr. Sibao Chen and Dr. Charmaine Tsang: Dept. of Applied Biology and Chemical TechnologyBrian LiNo ratings yet
- Renal impairment and dexketoprofen pharmacokineticsDocument2 pagesRenal impairment and dexketoprofen pharmacokineticsMaria UlfaNo ratings yet
- Carbofil 07 2019 e PDFDocument4 pagesCarbofil 07 2019 e PDFjpsingh75No ratings yet
- DAFTAR PUSTAKA AnestesiDocument2 pagesDAFTAR PUSTAKA AnestesiauliyaanandaNo ratings yet