Professional Documents
Culture Documents
24hr Fluid Balance ADULT Chart - v3
Uploaded by
anggita diahOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
24hr Fluid Balance ADULT Chart - v3
Uploaded by
anggita diahCopyright:
Available Formats
Rotherham NHS Foundation Trust
24 Hour Adult Fluid Balance Chart Date:
Surname: Forenames (In full):
DOB: Sex:
Consultant: Ward:
Hospital No:
Patient assessment / goals
Weight: kg Target fluid input 24 hours: mls
PREVIOUS DAYS BALANCE mls
Input Output
NG/Vomitus Drain(s)
Time 1 2 3 Urine pH a b Faecal/ Initials
mls mls mls Aspirate mls mls Stoma
Type Volume mls Type Volume mls Type Volume mls
06:00
07:00
08:00
09:00
10:00
11:00
12:00
13:00
14:00
15:00
16:00
17:00
12 Hour Subtotal
12 Hour Input Total 12 Hour Output Total
Signature 12 Hour Balance
18:00
19:00
20:00
21:00
22:00
23:00
00:00
01:00
02:00
03:00
04:00
05:00
12 Hour Subtotal
12 Hour Input Total 12 Hour Output Total
24 Hour Input Total 24 Hour Output Total
Signature 24 Hour Balance
ALL FLUID BALANCE CHARTS MUST BE ACCURATE
WHEN YOUR PATIENT IS ON IV FLUIDS YOU MUST CHECK DAILY U&Es
The 5 Rs: (Intravenous Fluid Therapy NICE No174)
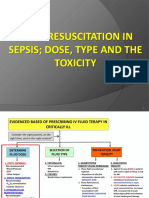
R Resuscitation
If a patient needs fluid resuscitation use crystalloids that contain sodium in the range of 130-154mmol/l with a bolus of 250-500ml
R
Routine Maintenance
Restrict initial IV prescription to 25-30 ml/kg per day e.g. 80kg patient requires 2000-2400 mls over a 24hr period. Sodium /
potassium (approx.) 1 mmol/kg/per day. Check DAILY U&Es.
R Replacement
Adjust the IV prescription to account for existing fluid and or electrolyte deficits or excesses, on-going losses, review Fluid
Balance chart, check for dehydration, fluid overload, hyperkalaemia / hypokalaemia.
R Redistribution
Check for oedema, sepsis 6, hypernatraemia, hyponatraemia, renal, liver or cardiac impairment, post op fluid retention,
malnourished and refeeding issues.
R Reassessment
Using the ABCDE approach, assess the patient’s likely fluid and electrolyte needs, clinical history, previous intake, thirst, abnormal
losses, comorbidities, PAR score, review fluid chart, weight and laboratory assessments.
Add 50-100grams/per day Glucose (eg Glucose 5% contains 5g/100mls) For special considerations refer to NICE guidelines 174
When to review the patient’s fluid status (Adapted from Central Manchester University Hospitals)
CAUSE FOR CONCERN Acute illness
Routinely PAR trigger
1. Low Urine Output
Action: Immediate review by Junior Clinical deterioration
Doctor if UOP <20mls
Doctor Nurse 2. High Urine Output Nurse Doctor
Action: Immediate review if UOP >
110mls/hr for 3 hrs in a row in the absence
Review during Review fluid balance Review fluid balance JUNIOR DRS
chart at start, middle of diuretics
routine ward chart as part of your MUST ESCALATE
round and end of shift, 3. No IV and patient NBM for 6 hrs. Nursing Assessment. CONCERNS TO A
ensuring accurate Ensure accurately SENIOR IF NOT
Action: Review by Junior Doctor <2 hrs
balanced chart balanced charts RESOLVED WITHIN
4. Actual or potential acutely ill patient 4 HOURS
JUNIOR DRS
MUST ESCALATE Action: Follow graded response on reverse
CONCERNS TO A Immediate referral to of observation charts.
SENIOR IF NOT Junior Doctor if Senior review Immediate referral
RESOLVED WITHIN To relevant medical
CAUSE FOR
4 HOURS CONCERN staff if any cause
for concern. Follow
GRADED RESPONSE
For PAR trigger score
HANDOVER
Nursing staff must indicate which patients are on a fluid balance chart.
When a patient is transferred verbal and written documentation must include fluid
If you are uncertain
balance and any concerns.
at any time seek
Medical staff documentation must include a clear fluid balance management plan. medical assistance
Any patient causing concern must be verbally handed over to next shift.
All users of this fluid chart must enter their specimen signature and initials
Print name Signature Initials Print name Signature Initials
TRFT Graphic Design Service 01709 426352 / JS 04/14 CS Version 3 SF5002
You might also like
- Fetal Alcohol Syndrome Brochure For Nursing SchoolDocument2 pagesFetal Alcohol Syndrome Brochure For Nursing SchoolKrystal Cowley Miller100% (1)
- Group 5 13B: End Stage Renal Failure Secondary To Diabetes NephropathyDocument68 pagesGroup 5 13B: End Stage Renal Failure Secondary To Diabetes NephropathyJinski007100% (1)
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideFrom EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNo ratings yet
- Supraventricular TachycardiaDocument22 pagesSupraventricular TachycardiaFaza KahfiNo ratings yet
- The Battle Against Covid-19 Filipino American Healthcare Workers on the Frontlines of the Pandemic ResponseFrom EverandThe Battle Against Covid-19 Filipino American Healthcare Workers on the Frontlines of the Pandemic ResponseNo ratings yet
- Renal Replacement TherapyDocument50 pagesRenal Replacement TherapyMalueth Angui100% (1)
- Liverpool Care Pathway PDFDocument63 pagesLiverpool Care Pathway PDFBryan DorosanNo ratings yet
- Decent 17Document3 pagesDecent 17Han Joshua PacañaNo ratings yet
- Discharge Planning ChecklistDocument6 pagesDischarge Planning ChecklistcutevivesNo ratings yet
- Psychotherapeutic Management in The Continuum of CareDocument23 pagesPsychotherapeutic Management in The Continuum of CareJohn Mark ParacadNo ratings yet
- IVT Procedure IDocument47 pagesIVT Procedure Izhallene813No ratings yet
- 116 ExamDocument14 pages116 ExamZhailyn Joy DumlaoNo ratings yet
- Blood Transfusion ModuleDocument45 pagesBlood Transfusion ModuleElisse RamosNo ratings yet
- Discharge Plan: What You Need To Know: Discharge InstructionsDocument2 pagesDischarge Plan: What You Need To Know: Discharge Instructionscoral jade cuaNo ratings yet
- C C C M MMMM MM M MMM 3mm MMMMM MM M MMMMMDocument4 pagesC C C M MMMM MM M MMM 3mm MMMMM MM M MMMMMjohkieNo ratings yet
- Discharge PlanningDocument26 pagesDischarge PlanningEndah SetyawatiNo ratings yet
- Acute Kidney Injury (AKI) :: FeaturesDocument3 pagesAcute Kidney Injury (AKI) :: FeaturesDavid PerezNo ratings yet
- Dialysis ReviewerDocument16 pagesDialysis ReviewerlarraNo ratings yet
- Plan of Care For:: Nursing Diagnosis: Excess Fluid VolumeDocument3 pagesPlan of Care For:: Nursing Diagnosis: Excess Fluid VolumeKenji CadizNo ratings yet
- SBAR Report To Physician About A Critical SitutionDocument3 pagesSBAR Report To Physician About A Critical SitutionRandolph DjanieNo ratings yet
- HemodialysisDocument14 pagesHemodialysistri utamiNo ratings yet
- Self Directive LearningDocument18 pagesSelf Directive Learningcrystal fate valdezNo ratings yet
- Funda - Pretest 2Document10 pagesFunda - Pretest 2FreeNursingNotesNo ratings yet
- Peritoneal DialysisDocument5 pagesPeritoneal DialysisJulienne Sanchez-SalazarNo ratings yet
- Patient NursingDocument7 pagesPatient Nursingsahilchaudhary7No ratings yet
- Preliminary ExaminationDocument58 pagesPreliminary ExaminationKaycelyn JimenezNo ratings yet
- Nursing Management Pancreatic CancerDocument2 pagesNursing Management Pancreatic CancerKit NameKo100% (2)
- Study On Pressure UlcerDocument219 pagesStudy On Pressure UlcerThein Ko Oo100% (1)
- CHN RVW 2Document51 pagesCHN RVW 2Michael UrrutiaNo ratings yet
- MCN II AntepartumDocument28 pagesMCN II AntepartumJharaNo ratings yet
- Sbar Simulation ReflectionDocument3 pagesSbar Simulation Reflectionapi-314635911100% (2)
- Performance Evaluation Achieving Newborn Care CompetencyDocument2 pagesPerformance Evaluation Achieving Newborn Care CompetencyShekaina BartidoNo ratings yet
- Care of Adults 26 Endocrine ManagementDocument26 pagesCare of Adults 26 Endocrine ManagementGaras AnnaBerniceNo ratings yet
- Peritoneal DialysisDocument5 pagesPeritoneal DialysisLisette TupasNo ratings yet
- Drug CalculationDocument7 pagesDrug CalculationYashly VargheseNo ratings yet
- Admission and DischargeDocument3 pagesAdmission and DischargePhilip Jay Braga100% (1)
- 100 Items Comprehensive Exam2Document17 pages100 Items Comprehensive Exam2miranda3163100% (1)
- Handouts-Standards of Professional Care in Intravenous TherapyDocument13 pagesHandouts-Standards of Professional Care in Intravenous TherapyTony DemaguilNo ratings yet
- 1 FluidsDocument17 pages1 FluidsMae CalunsagNo ratings yet
- Parenteral Nutrition Basic IVT Nov 2008Document53 pagesParenteral Nutrition Basic IVT Nov 2008Crystal Mae Castrodes DaquipilNo ratings yet
- Teamworks! Game: Summary ReportDocument2 pagesTeamworks! Game: Summary ReportAngela May Pustasa AllamNo ratings yet
- Nclex Cardio QuestionsDocument4 pagesNclex Cardio QuestionsMichelleNo ratings yet
- CNN Practice QuestionsDocument5 pagesCNN Practice QuestionsUri Perez MontedeRamosNo ratings yet
- Comprehensive Geriatric Assessment ToolDocument10 pagesComprehensive Geriatric Assessment ToolAmeraidah Patorai100% (2)
- Adams4e Tif Ch04Document26 pagesAdams4e Tif Ch04fbernis1480_11022046No ratings yet
- Medical Surgical Nursing IIDocument52 pagesMedical Surgical Nursing IItwinkle143No ratings yet
- Post Test - CHNDocument13 pagesPost Test - CHNNaomi VirtudazoNo ratings yet
- HD Nurse Job Description HD NurseDocument6 pagesHD Nurse Job Description HD NurseFathima Nasrin0% (1)
- Sinus Rhythms: Dysrhythmia Recognition & ManagementDocument29 pagesSinus Rhythms: Dysrhythmia Recognition & Managementkamel6No ratings yet
- FAQ About IVT TrainingDocument12 pagesFAQ About IVT TrainingJohanna ChavezNo ratings yet
- Anticoagulation in Hemodialysis: Arlene S. Munoz MD, FPCP, FPSNDocument51 pagesAnticoagulation in Hemodialysis: Arlene S. Munoz MD, FPCP, FPSNBryant MunozNo ratings yet
- Carl Rogers Erik Erikson Ivan Pavlov Albert Ellis B.F SkinnerDocument3 pagesCarl Rogers Erik Erikson Ivan Pavlov Albert Ellis B.F Skinnermark OrpillaNo ratings yet
- Status Epilepticus Case Study Kristopher Kirby.Document4 pagesStatus Epilepticus Case Study Kristopher Kirby.KrisNo ratings yet
- ABDOMINAL ObjectiveDocument9 pagesABDOMINAL ObjectiveXing-Jin RomeroNo ratings yet
- DARDocument4 pagesDARfritzroseNo ratings yet
- 2020 Gaumard CatalogDocument252 pages2020 Gaumard Catalogjuan javier apazaNo ratings yet
- Fluid Resuscitation - The Evidence PDFDocument54 pagesFluid Resuscitation - The Evidence PDFrsia fatimahNo ratings yet
- Patient Blood Management Equals Patient SafetyDocument19 pagesPatient Blood Management Equals Patient SafetyMuhammadBudiman RbcNo ratings yet
- Ketoconazole PDFDocument7 pagesKetoconazole PDFparand2003No ratings yet
- Renal Cell Carcinoma: DR Kalyan K Sarkar Ms FrcsedDocument38 pagesRenal Cell Carcinoma: DR Kalyan K Sarkar Ms FrcsedMichael ParkNo ratings yet
- (Protocolo) ACT For Psychosis. An 18 Session Group Therapy Protocol - Pearson & TingeyDocument82 pages(Protocolo) ACT For Psychosis. An 18 Session Group Therapy Protocol - Pearson & TingeyDavid Espinola100% (1)
- 04 GTTDocument15 pages04 GTTAshish TuraleNo ratings yet
- What Is Alzheimer's - Alzheimer's AssociationDocument6 pagesWhat Is Alzheimer's - Alzheimer's AssociationRatnaPrasadNalamNo ratings yet
- Truncated Middle Turbinnate SNPDocument4 pagesTruncated Middle Turbinnate SNPSriram RajanNo ratings yet
- Bioremediation of Environmental PollutantsDocument21 pagesBioremediation of Environmental PollutantsaziskfNo ratings yet
- Therapeutic Interventions Part I Rubberbands NowDocument8 pagesTherapeutic Interventions Part I Rubberbands NowAnna Purna100% (1)
- Morton's NeuromaDocument8 pagesMorton's Neuromagreencrystal81No ratings yet
- CHFDocument35 pagesCHFNurayunie Abd HalimNo ratings yet
- Curative and Rehabilitative Nursing Care Management of Clients in Acute Biologic CrisisDocument44 pagesCurative and Rehabilitative Nursing Care Management of Clients in Acute Biologic CrisisArgee AlonsabeNo ratings yet
- Region 2 - Community-Based Services - September 2017Document12 pagesRegion 2 - Community-Based Services - September 2017Jennifer BankerNo ratings yet
- ICD 10overviewDocument4 pagesICD 10overviewObat Dot In100% (1)
- G10-Basic Principles and Techniques of Internal Fixation of FracturesDocument57 pagesG10-Basic Principles and Techniques of Internal Fixation of FracturesSumantNo ratings yet
- Scaling Teeth TechniquesDocument12 pagesScaling Teeth TechniqueshanyNo ratings yet
- Adamantinoma: Sebok Daniel Sucher ErwinDocument34 pagesAdamantinoma: Sebok Daniel Sucher ErwinGheorghe SebokNo ratings yet
- Assessing Nutrition in Patients With Chronic Kidney Disease by Kimberly Thompson, MS, RD, LDNDocument23 pagesAssessing Nutrition in Patients With Chronic Kidney Disease by Kimberly Thompson, MS, RD, LDNCarlos RaiolNo ratings yet
- Perineal RuptureDocument24 pagesPerineal RuptureIzz ShuhaimiNo ratings yet
- Rogelio P. Nogales Et Al vs. CMC, Dr. Oscar Estrada Et Al - gr142625Document5 pagesRogelio P. Nogales Et Al vs. CMC, Dr. Oscar Estrada Et Al - gr142625Dani EsequeNo ratings yet
- Child Psychopathology: Child Psychopathology Is The Manifestation of Psychological Disorders in Children andDocument7 pagesChild Psychopathology: Child Psychopathology Is The Manifestation of Psychological Disorders in Children andMarvellous MunhuwaNo ratings yet
- Skin Diseases in Pregnancy: by by Ahmed Elbohoty MD, MRCOG Lecturer of Obstetrics and Gynecology Ain Shams UniversityDocument63 pagesSkin Diseases in Pregnancy: by by Ahmed Elbohoty MD, MRCOG Lecturer of Obstetrics and Gynecology Ain Shams UniversityAhmed Bassett100% (1)
- Intraoral Gothic Arch Tracing PDFDocument5 pagesIntraoral Gothic Arch Tracing PDFSamuel Flores CalderonNo ratings yet
- Therapy - Case Study 2Document7 pagesTherapy - Case Study 2api-239581082100% (1)
- Obstetric Analgesia PDFDocument45 pagesObstetric Analgesia PDFBoneyJalgar100% (1)
- Why Are Black Women Rated Less Physically Attractive Than Other Women, But Black Men Are Rated Better Looking Than Other Men?Document6 pagesWhy Are Black Women Rated Less Physically Attractive Than Other Women, But Black Men Are Rated Better Looking Than Other Men?koa_x100% (2)
- Immunological Basis of Infertility in AnimalsDocument13 pagesImmunological Basis of Infertility in AnimalsRamachandran Ram100% (3)
- Nursereview Org Therapeutic Communication TechniquesDocument6 pagesNursereview Org Therapeutic Communication TechniquesPatricia VasquezNo ratings yet
- Types of Diagnosis:: Problem-Focused Nursing Diagnoses Have Three Components: (1) Nursing DiagnosisDocument4 pagesTypes of Diagnosis:: Problem-Focused Nursing Diagnoses Have Three Components: (1) Nursing DiagnosisDaisy MellaNo ratings yet
- Anaphylactic ShockDocument29 pagesAnaphylactic ShockHIND100% (7)
- How to Talk to Anyone: Learn the Secrets of Good Communication and the Little Tricks for Big Success in RelationshipFrom EverandHow to Talk to Anyone: Learn the Secrets of Good Communication and the Little Tricks for Big Success in RelationshipRating: 4.5 out of 5 stars4.5/5 (1135)
- Deep Sleep Hypnosis: Guided Meditation For Sleep & HealingFrom EverandDeep Sleep Hypnosis: Guided Meditation For Sleep & HealingRating: 4.5 out of 5 stars4.5/5 (104)
- Breaking the Habit of Being YourselfFrom EverandBreaking the Habit of Being YourselfRating: 4.5 out of 5 stars4.5/5 (1460)
- Chair Yoga: Sit, Stretch, and Strengthen Your Way to a Happier, Healthier YouFrom EverandChair Yoga: Sit, Stretch, and Strengthen Your Way to a Happier, Healthier YouRating: 3.5 out of 5 stars3.5/5 (5)
- Peaceful Sleep Hypnosis: Meditate & RelaxFrom EverandPeaceful Sleep Hypnosis: Meditate & RelaxRating: 4.5 out of 5 stars4.5/5 (144)
- Summary of The 4-Hour Body: An Uncommon Guide to Rapid Fat-Loss, Incredible Sex, and Becoming Superhuman by Timothy FerrissFrom EverandSummary of The 4-Hour Body: An Uncommon Guide to Rapid Fat-Loss, Incredible Sex, and Becoming Superhuman by Timothy FerrissRating: 4.5 out of 5 stars4.5/5 (82)
- The Happiest Baby on the Block: The New Way to Calm Crying and Help Your Newborn Baby Sleep LongerFrom EverandThe Happiest Baby on the Block: The New Way to Calm Crying and Help Your Newborn Baby Sleep LongerRating: 4.5 out of 5 stars4.5/5 (58)
- Forever Strong: A New, Science-Based Strategy for Aging WellFrom EverandForever Strong: A New, Science-Based Strategy for Aging WellNo ratings yet
- Love Yourself, Heal Your Life Workbook (Insight Guide)From EverandLove Yourself, Heal Your Life Workbook (Insight Guide)Rating: 5 out of 5 stars5/5 (40)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Really Very Crunchy: A Beginner's Guide to Removing Toxins from Your Life without Adding Them to Your PersonalityFrom EverandReally Very Crunchy: A Beginner's Guide to Removing Toxins from Your Life without Adding Them to Your PersonalityRating: 5 out of 5 stars5/5 (30)
- 369: Manifesting Through 369 and the Law of Attraction - METHODS, TECHNIQUES AND EXERCISESFrom Everand369: Manifesting Through 369 and the Law of Attraction - METHODS, TECHNIQUES AND EXERCISESRating: 5 out of 5 stars5/5 (50)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningFrom EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningRating: 4 out of 5 stars4/5 (3)
- Instant Loss On a Budget: Super-Affordable Recipes for the Health-Conscious CookFrom EverandInstant Loss On a Budget: Super-Affordable Recipes for the Health-Conscious CookRating: 3.5 out of 5 stars3.5/5 (2)
- What to Expect When You’re Expecting (5th Edition)From EverandWhat to Expect When You’re Expecting (5th Edition)Rating: 5 out of 5 stars5/5 (1)
- Aging Backwards: Reverse the Aging Process and Look 10 Years Younger in 30 Minutes a DayFrom EverandAging Backwards: Reverse the Aging Process and Look 10 Years Younger in 30 Minutes a DayNo ratings yet
- The Longevity Book: The Science of Aging, the Biology of Strength, and the Privilege of TimeFrom EverandThe Longevity Book: The Science of Aging, the Biology of Strength, and the Privilege of TimeRating: 3.5 out of 5 stars3.5/5 (13)
- Allen Carr's Easy Way to Quit Vaping: Get Free from JUUL, IQOS, Disposables, Tanks or any other Nicotine ProductFrom EverandAllen Carr's Easy Way to Quit Vaping: Get Free from JUUL, IQOS, Disposables, Tanks or any other Nicotine ProductRating: 5 out of 5 stars5/5 (31)
- The Beck Diet Solution Weight Loss Workbook: The 6-Week Plan to Train Your Brain to Think Like a Thin PersonFrom EverandThe Beck Diet Solution Weight Loss Workbook: The 6-Week Plan to Train Your Brain to Think Like a Thin PersonRating: 3.5 out of 5 stars3.5/5 (33)
- Grit & Grace: Train the Mind, Train the Body, Own Your LifeFrom EverandGrit & Grace: Train the Mind, Train the Body, Own Your LifeRating: 4 out of 5 stars4/5 (3)
- Find Your Path: Honor Your Body, Fuel Your Soul, and Get Strong with the Fit52 LifeFrom EverandFind Your Path: Honor Your Body, Fuel Your Soul, and Get Strong with the Fit52 LifeRating: 4 out of 5 stars4/5 (3)
- Summary of The Body Keeps the ScoreFrom EverandSummary of The Body Keeps the ScoreRating: 4.5 out of 5 stars4.5/5 (18)