Professional Documents
Culture Documents
Main Presentations of Sexually Transmitted Infections in Men
Uploaded by
bbyesOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Main Presentations of Sexually Transmitted Infections in Men
Uploaded by
bbyesCopyright:
Available Formats
Clinical review
ABC of sexually transmitted infections
Main presentations of sexually transmitted infections in men
John Richens
Some sexually transmitted infections, such as gonorrhoea and
This article is adapted from the fifth edition of the ABC of
chlamydial infection, have different presentations in the two
Sexually Transmitted Diseases, which is published by BMJ
sexes because of differences in genital anatomy. This chapter Books (www.bmjbooks.com)
focuses on infections of the male urethra, epididymis, testis, and An overview of chlamydial infection and gonorrhoea is
prostate. Anal and oral symptoms are also covered because available on bmj.com
these are encountered more often among men, especially men
who have sex with men.
Causes of urethritis in men
Common diagnoses
Urethral discharge and dysuria x Gonorrhoea
x Chlamydial infection
Spontaneous discharge of fluid from the urethral meatus, x Non-specific urethritis
usually most noticeable after holding urine overnight and often Less common diagnoses
accompanied by burning discomfort during urination (dysuria), x Ureaplasma urealyticum infection
x Mycoplasma genitalium infection
strongly indicates a sexually acquired urethral infection.
x Trichomoniasis
Symptomatic gonorrhoea usually develops within a few days x Herpes simplex virus infection
of exposure. Chlamydial infections take slightly longer. Mild x Escherichia coli infection
infections may cause urethral discomfort and dysuria without x Bacteroides infection
discharge and may be confused with cystitis. x Cystitis
x Pyelonephritis
x Trauma
Management of urethritis x Foreign body
x Reactive arthritis, Reiter’s syndrome, and allied conditions
1 Take history, including sexual history
2 Examine, looking especially for evidence of discharge
3 Take samples from urethra
4 Treat for gonorrhoea and chlamydia if urethral Gram stain is
positive for Gram negative intracellular diplococci
5 Give treatment for chlamydia if the urethral smear shows five or
more polymorphs per high power field and the Gram stain does
not suggest gonorrhoea
6 Explain diagnosis, treatment, and methods of prevention
7 Advise to avoid sex until treatment and follow up are completed
8 Advise treatment of partners
9 Review patient after treatment for symptoms, adherence, treatment
of partners, and test of cure if gonorrhoea has been diagnosed
When laboratory investigation is not feasible, steps 3, 5, and the test of
cure can be omitted
In clinics with laboratory facilities, the usual approach is to
test for gonorrhoea and chlamydial infection. The first step is
microscopy of a urethral smear. Optimal results for this are Gonococcal urethral discharge
obtained from patients who have held their urine for four hours
or more.
Urethritis is confirmed if the urethral smear shows five or
more polymorphs per high power field. If the smear shows
Gram negative intracellular diplococci, the patient is treated for
gonorrhoea and chlamydia to cover the possibility of a mixed
infection. Meanwhile, confirmatory tests for gonorrhoea and
chlamydia are carried out (see bmj.com).
Patients without evidence of gonorrhoea receive doxycycline
(100 mg twice daily for one week), erythromycin (500 mg twice
daily for two weeks), or azithromycin (1 g single dose), which are
active against chlamydial infection and most other pathogens
associated with non-gonococcal urethritis. Doxycycline can
cause photosensitivity. Absorption is impaired by antacids, iron,
calcium, and magnesium salts. Gastrointestinal upset is
common with erythromycin and azithromycin.
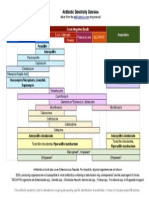
This approach will relieve symptoms in most patients, but World Health Organization flow chart for managing urethral
some will report persistent symptoms or show a persistently discharge
BMJ VOLUME 328 22 MAY 2004 bmj.com 1251
Clinical review
abnormal smear without symptoms. The options are then to
investigate for treatment failure or reinfection or for infection
by less common pathogens (for example, Trichomonas vaginalis)
and to repeat, continue, or change the antibiotic therapy or
await spontaneous resolution of symptoms.
When access to laboratory testing is not available, the
simplest approach to managing urethritis is to administer blind
treatment for gonorrhoea and chlamydia.
Scrotal swelling and pain
Mild testicular discomfort in the absence of abnormal physical
signs is encountered commonly in young men attending STI
clinics. Many patients can be reassured if testicular examination Gram negative intracellular diplococci
and a screen for STIs give normal results. In some cases, anxiety
about infection, sexual function, or cancer is present. More
marked scrotal pain has various causes.
Acute inflammation of the scrotal contents (usually
unilateral) in young men is usually caused by gonorrhoea or Causes of scrotal swelling and pain
chlamydia. In older men, Escherichia coli, Klebsiella, Pseudomonas, x Infections of testis and epididymis: gonorrhoea, chlamydia,
and Proteus infections are found more often. The first tuberculosis, mumps, and Gram negative bacteria
consideration in diagnosis is to exclude acute torsion, which x Torsion of testis (mainly adolescents) or appendix testis (mainly 3-7
requires emergency surgery. Torsion predominates in the year olds)
teenage years, usually has an acute onset, and is often x Pain after vasectomy
x Fournier’s gangrene
accompanied by vomiting. An immediate surgical opinion x Vasculitis: Henoch-Schönlein purpura, Kawasaki disease, and
should be sought for any possible case. Doppler scanning is Buerger’s disease
useful to show impaired blood flow. x Amiodarone therapy
The distinguishing features of mumps orchitis (severe x Tumour
testicular pain and marked systemic symptoms) usually appear x Hernia
a few days after parotid swelling, although the parotitis may be x Trauma
absent. Useful tests for cases of suspected epididymo-orchitis
are a urethral smear, mid stream urine culture, and
investigations for gonorrhoea and chlamydia. Presumptive
treatment for gonorrhoea and chlamydia is appropriate in
younger men when investigation is not feasible. Severe cases
require treatment in hospital with parenteral antibiotics.
Analgesia, scrotal support, and elevation may reduce discomfort
and promote recovery.
Painless swellings in the scrotum are common. Most of these
are small, round, epididymal cysts or spermatoceles that require
no investigation or treatment. Lesions in the testis can be due to
tuberculosis, syphilis, or malignancy and require urgent
ultrasound examination. Varicoceles feel like a bag of worms in
the scrotum and can be associated with infertility. Therefore,
referral to a urologist is advised if pain, testicular atrophy,
infertility, or the threat of infertility are concerns.
Acute epididymo-orchitis due to STI
Pelvic pain
Differential diagnosis of prostatic pain
The prostate can be affected by a variety of infectious and NIH classification of prostatitis syndromes
poorly defined non-infectious conditions that present as acute I Acute bacterial prostatitis
or chronic pelvic pain with a range of accompanying urinary II Chronic bacterial prostatitis
and systemic symptoms. Gonorrhoea, chlamydial infections, and III Chronic pelvic pain syndrome (CPPS):
trichomoniasis can affect the prostate, but most acute infections IIIA Inflammatory (leucocytes in prostatic secretion, semen, or
are caused by other bacteria such as E coli, Proteus, Streptococcus urine after prostatic massage)
IIIB Non-inflammatory (as above without leucocytes)
faecalis, Klebsiella, and Pseudomonas. IV Asymptomatic inflammatory prostatitis
STIs and non-sexually transmitted bacterial infections of the
Other causes of pain in region of prostate
prostate account for only a few painful prostatic syndromes. x Pudendal neuralgia (sometimes due to tumour)
Most patients with prostatic pain fall into a category recently x Bladder outlet obstruction
designated “chronic pelvic pain syndrome” by the newly x Bladder tumours
adopted National Institutes of Health classification of prostatitis x Urinary stone disease
syndromes. x Inguinal ligament enthesopathy
In patients who present with pelvic pain, the prostate should x Obstruction of ejaculatory duct
x Seminal vesicle calculi
be examined for enlargement and tenderness. Patients with
x Bowel disorders
prostatitis should be screened for STIs. The value of subjecting
1252 BMJ VOLUME 328 22 MAY 2004 bmj.com
Clinical review
patients to prostatic massage to examine prostatic secretions for
Measures occasionally found helpful in men with chronic
bacteria and inflammatory cells is now questioned by many
pelvic pain syndrome
experts. Transrectal ultrasonography and urodynamic studies
are helpful in some patients. Confirmed infections respond well x Simple analgesia
x Non-steroidal anti-inflammatory drugs
to antibiotics, the first choice often being a 28 day course of a
x 2-4 weeks of ciprofloxacin or doxycycline
quinolone or tetracycline, which have better prostatic x Alpha blocking drugs (alfuzosin, terazosin, tamsulosin)
penetration than other antibiotics. x Finasteride
Treating the more common causes of chronic pelvic pain is x Quercetin
difficult. None of the treatments is well validated, and response x Low dose amitriptyline
rates are often poor. A recently published NIH symptoms index x Repetitive prostatic massage (contraindicated in bacterial
prostatitis)
for chronic prostatitis is a useful way to record and monitor
x Regular ejaculation
symptoms.
Anal symptoms
Anorectal STIs
Sexually transmitted infections can be transmitted by
penile-anal contact, oroanal contact, or fingering, resulting in
asymptomatic infection, ulceration (for example, herpes and
syphilis) warts, or proctitis, the main manifestations of which are
pain, tenesmus, bleeding, and discharge. Ulceration is
investigated in the same way as genital ulceration. Discharges
require investigation by proctoscopy, during which samples can
be taken from the rectum to test for gonorrhoea and chlamydia.
The management of a sexually acquired rectal discharge
parallels that of urethritis. Anorectal infections are a potent
cofactor for HIV transmission.
Anal intercourse can lead to the transmission of a wide
variety of other organisms normally transmitted by the
faeco-oral route. These include hepatitis A virus, Shigella,
Salmonella, and Giardia. Anal intraepithelial neoplasia and
invasive carcinoma may follow infection with certain subtypes
of human papillomavirus.
Non-infectious anal conditions Rectal gonorrhoea
Patients who practise receptive anal sex often present to STI
services with anal fissure, haemorrhoids, perianal haematomas,
and pruritus ani. It is important to provide training and
guidelines for the management and referral of these common
conditions in clinics that see clients who practise anal sex.
Oral and perioral symptoms
Oral STIs usually are asymptomatic. Neisseria gonorrhoeae and
Chlamydia infect the pharyngeal mucosa readily but rarely cause
acute inflammation. Primary syphilis may present on the
tongue or lips, and secondary syphilis can produce an oral
mucositis. HIV has an important array of oral manifestations
that include oral candidiasis (both erythematous and
pseudomembranous), angular cheilitis, gingivitis, oral hairy
leucoplakia, and Kaposi’s sarcoma. Warts may develop in and
around the mouth as a result of orogenital sexual activity. Perioral warts. Reproduced with permission of the Wellcome Trust
Further reading
x Galejs LE. Diagnosis and treatment of the acute scrotum. Am Fam
Physician 1999;59:817-24 John Richens is lecturer in sexually transmitted diseases, Royal Free
x Krieger JN, Ross SO, Deutsch L, Riley DE. The NIH consensus and University College Medical School, London
concept of chronic prostatitis/chronic pelvic pain syndrome (jrichens@gum.ucl.ac.uk)
compared with traditional concepts of nonbacterial prostatitis and The ABC of Sexually Transmitted Diseases is edited by Michael Adler,
prostatodynia. Curr Urol Rep 2002;3:301-6 professor of genitourinary medicine, Royal Free and University
x Holmes KK, Mårdh PA, Sparling PF, Lemon S, Stamm W, Piot P, et College Medical School, London
al. Sexually transmitted diseases. 3rd ed. New York: McGraw Hill, 1999
x Morton RS, ed. Gonorrhoea. 3rd ed. London: WB Saunders, 1977 Competing interests: None declared
x Ostrow DG, Sandholzer TA, Felman YM, eds. Sexually transmitted
BMJ 2004;328:1251–3
diseases in homosexual men: diagnosis, treatment, and research. New York:
Plenum, 1983
BMJ VOLUME 328 22 MAY 2004 bmj.com 1253
You might also like
- Urethral DischargeDocument26 pagesUrethral DischargeZahra ArainNo ratings yet
- Urethritis: Continuing Education ActivityDocument8 pagesUrethritis: Continuing Education ActivityMutiara AmaliaNo ratings yet
- UrethritisDocument11 pagesUrethritisgreggy_rebel17No ratings yet
- Includes: Urinary Tract Infections Genital Tract Infections Viral Sexually Transmitted Diseases Bacterial Sexual Transmitted DiseasesDocument37 pagesIncludes: Urinary Tract Infections Genital Tract Infections Viral Sexually Transmitted Diseases Bacterial Sexual Transmitted DiseasesDon Pelicio NgohoNo ratings yet
- Infectious Causes of Dysuria in Adult MenDocument5 pagesInfectious Causes of Dysuria in Adult MenFrancisco Javier Contreras MoralesNo ratings yet
- Gonorrhea - Practice Essentials, Background, Pathophysiology Sumber 13Document15 pagesGonorrhea - Practice Essentials, Background, Pathophysiology Sumber 13Anizha AdriyaniNo ratings yet
- By: Jennifer Vu, Teresa Kodi, Emily Dang, James Baawuo and Yesenia AlmanzaDocument19 pagesBy: Jennifer Vu, Teresa Kodi, Emily Dang, James Baawuo and Yesenia AlmanzajbaawuoNo ratings yet
- Sexually Transmitted DiseasesDocument71 pagesSexually Transmitted DiseasesAkwu AkwuNo ratings yet
- Urinary System and Its PathologiesDocument23 pagesUrinary System and Its Pathologiesngachangong victorineNo ratings yet
- Sexually Transmitted InfectionsDocument48 pagesSexually Transmitted InfectionsYsabella LlanetaNo ratings yet
- UrethritisDocument11 pagesUrethritismarej143No ratings yet
- Sexually Transmitted Infections (Sti) Ii: Return To SyllabusDocument15 pagesSexually Transmitted Infections (Sti) Ii: Return To SyllabusANGGITA LARASATI PURBANINGRUMNo ratings yet
- Genitourinary SystemDocument7 pagesGenitourinary SystemMary Angel VelascoNo ratings yet
- GonorrheaDocument53 pagesGonorrheaapi-1991639975% (4)
- Sexually Transmitted Infections - Hatem Sadek PresentationDocument36 pagesSexually Transmitted Infections - Hatem Sadek PresentationHatem SadekNo ratings yet
- Sti 2018 LseDocument67 pagesSti 2018 LsespinosumNo ratings yet
- Urinary Tract Infections DR Moses KazevuDocument23 pagesUrinary Tract Infections DR Moses KazevuMoses Jr KazevuNo ratings yet
- Epididymitis and OrchitisDocument11 pagesEpididymitis and Orchitiscitra08No ratings yet
- URETHRITIS - Yulia W 026Document20 pagesURETHRITIS - Yulia W 026Yulia WidiastutiNo ratings yet
- Tubo Ovarian Abcess (Abses Tuba-Ovari)Document4 pagesTubo Ovarian Abcess (Abses Tuba-Ovari)Muhammad Naqiuddin JalaluddinNo ratings yet
- Wikipedia - Epididymitis (CHECKED)Document6 pagesWikipedia - Epididymitis (CHECKED)pixoguiasNo ratings yet
- OrchitisDocument5 pagesOrchitisNader SmadiNo ratings yet
- TrichomoniasisDocument23 pagesTrichomoniasisSaba Siva50% (2)
- Sexually Transmitted Infections GuideDocument89 pagesSexually Transmitted Infections GuidegibreilNo ratings yet
- Sindrome Duh Genital GODocument9 pagesSindrome Duh Genital GOIntan PermataNo ratings yet
- STI Clinical GuideDocument83 pagesSTI Clinical Guidebekbekk cabahugNo ratings yet
- 7 PyuriaDocument19 pages7 PyuriaFarihatun NisaNo ratings yet
- Urinary Tract InfectionDocument46 pagesUrinary Tract Infectionbest batiNo ratings yet
- Reproductive Tract InformationDocument14 pagesReproductive Tract InformationGonçalo BaptistaNo ratings yet
- Urinary Tract Infection: By: Yoavita Moderator: Dr. Ati Rastini Ri, SPPK (K)Document40 pagesUrinary Tract Infection: By: Yoavita Moderator: Dr. Ati Rastini Ri, SPPK (K)ChristinaNo ratings yet
- Sexually Transmitted InfectionsDocument10 pagesSexually Transmitted InfectionsStar CruiseNo ratings yet
- Acute CervicitisDocument9 pagesAcute CervicitisVicobeingoNo ratings yet
- Causes and management of common vaginal dischargesDocument8 pagesCauses and management of common vaginal dischargesMELVYN HAROLD CHAVEZ MAURICIONo ratings yet
- Chapter 53: Nursing Management: Sexually Transmitted DiseasesDocument4 pagesChapter 53: Nursing Management: Sexually Transmitted DiseasesjefrocNo ratings yet
- Daring Aidil Akbar Internal Genital InfectionDocument29 pagesDaring Aidil Akbar Internal Genital InfectionrakaNo ratings yet
- Genitourinary Chlamydial Infection GuideDocument18 pagesGenitourinary Chlamydial Infection GuideNatalie AlcântaraNo ratings yet
- Pelvic Inflammatory DiseaseDocument15 pagesPelvic Inflammatory Diseaseashleenriya832No ratings yet
- Trusted Medical Answers-In Seconds.: GonorrheaDocument7 pagesTrusted Medical Answers-In Seconds.: GonorrheantnquynhproNo ratings yet
- By: Shazleen Farhana Anggun Lestary Advisor: Dr. Diana Muchsin Supervisor: Dr. Asnawi Madjid, SP - KK, MARSDocument25 pagesBy: Shazleen Farhana Anggun Lestary Advisor: Dr. Diana Muchsin Supervisor: Dr. Asnawi Madjid, SP - KK, MARSShazleen FarhanaNo ratings yet
- STD 1Document56 pagesSTD 1PrakritiNo ratings yet
- Non Gonococcal UrethritisDocument4 pagesNon Gonococcal UrethritisEunice TrongcoNo ratings yet
- Homeopathic Treatment of Urethritis Thomas A. Kruzel, N. DDocument6 pagesHomeopathic Treatment of Urethritis Thomas A. Kruzel, N. DAtmayadi GunawanNo ratings yet
- RPS Penyakit KelaminDocument133 pagesRPS Penyakit KelaminArdana WindriyaNo ratings yet
- Urethral Discharge in Male, 1987Document6 pagesUrethral Discharge in Male, 1987ElisabethJaniceRusliNo ratings yet
- Female Genital Inflammatory DiseasesDocument39 pagesFemale Genital Inflammatory DiseaseseveeNo ratings yet
- GonorrheaDocument3 pagesGonorrheaRe-ann Mae F. MendozaNo ratings yet
- Evaluation of Dysuria in AdultsDocument8 pagesEvaluation of Dysuria in AdultspapermintNo ratings yet
- The Pathophysiology of Urinary Tract Infections: Practical Interpretations of Commonly Used TermsDocument6 pagesThe Pathophysiology of Urinary Tract Infections: Practical Interpretations of Commonly Used TermsPaullette SanjuanNo ratings yet
- Tai Lieu Tieng Anh Cho Sinh Vien Bai Nhiem Khuan Duong Tiet NieuDocument3 pagesTai Lieu Tieng Anh Cho Sinh Vien Bai Nhiem Khuan Duong Tiet NieuLê Mỹ Khánh LyNo ratings yet
- Orchits ManagementDocument9 pagesOrchits ManagementMarshall ThompsonNo ratings yet
- Trichomoniasis: Causes, Symptoms and Treatment of Trichomonas vaginalis InfectionDocument17 pagesTrichomoniasis: Causes, Symptoms and Treatment of Trichomonas vaginalis InfectionAndi MuhammadNo ratings yet
- Upper Genital Tract Infection (PID)Document24 pagesUpper Genital Tract Infection (PID)Tofitofi TofiNo ratings yet
- MICROBIOLOGY OF GENITOURINARY TRACT-2 (Julia Hartati, DR.)Document24 pagesMICROBIOLOGY OF GENITOURINARY TRACT-2 (Julia Hartati, DR.)Ayi Abdul BasithNo ratings yet
- Gonorrhea: Neisseria GonorrhoeaeDocument60 pagesGonorrhea: Neisseria GonorrhoeaeRikki OkNo ratings yet
- Review of Aetiology and Management of Testicular Abscess and Case Reports On Testicle Sparing Management of Testicular AbscessDocument5 pagesReview of Aetiology and Management of Testicular Abscess and Case Reports On Testicle Sparing Management of Testicular AbscessBodat BodatsNo ratings yet
- 2028-Article Text-6551-1-10-20230128Document5 pages2028-Article Text-6551-1-10-20230128hellowqueenyNo ratings yet
- Urinary Tract InfectionDocument50 pagesUrinary Tract Infectionpokhara gharipatanNo ratings yet
- Medical Microbiology: Sti (STD)Document90 pagesMedical Microbiology: Sti (STD)Brother GeorgeNo ratings yet
- Reproductive System DiseasesDocument5 pagesReproductive System DiseasesMichael Vincent P.No ratings yet
- Pead 3 - Abdominal Pain and VommitingDocument22 pagesPead 3 - Abdominal Pain and Vommitingbbyes100% (1)
- Pead 1 - NeonatologyDocument21 pagesPead 1 - NeonatologybbyesNo ratings yet
- Advanced Life Support AssessmentDocument1 pageAdvanced Life Support AssessmentbbyesNo ratings yet
- SSIC Program of Delivery: Should Be Completed (Week) Date Orientation Evening and Entrance ExamDocument4 pagesSSIC Program of Delivery: Should Be Completed (Week) Date Orientation Evening and Entrance ExambbyesNo ratings yet
- Tocolytics in PretermDocument13 pagesTocolytics in PretermbbyesNo ratings yet
- HMO Surgical PositionDocument4 pagesHMO Surgical PositionbbyesNo ratings yet
- Prenatal ScreeningDocument26 pagesPrenatal ScreeningbbyesNo ratings yet
- Early Pregnancy ComplciationsDocument43 pagesEarly Pregnancy ComplciationsbbyesNo ratings yet
- Substance Abuse in PregnancyDocument151 pagesSubstance Abuse in PregnancybbyesNo ratings yet
- Guideline: Maternity - Maternal Group B Streptococcus (GBS) and Minimisation of Neonatal Early-Onset GBS SepsisDocument18 pagesGuideline: Maternity - Maternal Group B Streptococcus (GBS) and Minimisation of Neonatal Early-Onset GBS SepsisbbyesNo ratings yet
- Position Description ENTDocument3 pagesPosition Description ENTbbyesNo ratings yet
- BASIC Course Gosford June 2021Document3 pagesBASIC Course Gosford June 2021bbyesNo ratings yet
- Training Manual 2020Document53 pagesTraining Manual 2020bbyesNo ratings yet
- Surgical - Information GuideDocument2 pagesSurgical - Information GuidebbyesNo ratings yet
- C SpineDocument44 pagesC SpinebbyesNo ratings yet
- Organisation Chart - TraineeDocument1 pageOrganisation Chart - TraineebbyesNo ratings yet
- Right VATS Pleural BiopsyDocument4 pagesRight VATS Pleural BiopsybbyesNo ratings yet
- Ischkwa DiagramDocument1 pageIschkwa DiagrambbyesNo ratings yet
- Atrial Fibrillation Managing Acute Atrial FibrillationDocument8 pagesAtrial Fibrillation Managing Acute Atrial FibrillationbbyesNo ratings yet
- Upper GI BleedDocument8 pagesUpper GI BleedbbyesNo ratings yet
- Varicose VeinDocument6 pagesVaricose VeinbbyesNo ratings yet
- RHDDocument130 pagesRHDDeepu RajendranNo ratings yet
- ECGs - UpdatedDocument26 pagesECGs - UpdatedbbyesNo ratings yet
- Antibiotic Sensitivity Overview for Gram Positive Cocci, Gram Negative Bacilli and AnaerobesDocument1 pageAntibiotic Sensitivity Overview for Gram Positive Cocci, Gram Negative Bacilli and AnaerobesGuillermo Damian RodriguezNo ratings yet
- Infections in PregnancyDocument11 pagesInfections in PregnancybbyesNo ratings yet
- Prof PracDocument3 pagesProf PracbbyesNo ratings yet
- Shoulder PainDocument5 pagesShoulder PainbbyesNo ratings yet
- Pump Manual TextDocument17 pagesPump Manual TextbbyesNo ratings yet
- Weekly SDS Topics: Week 3Document1 pageWeekly SDS Topics: Week 3bbyesNo ratings yet
- Curriculum Vitae: Shaikh Rukshana SalimDocument2 pagesCurriculum Vitae: Shaikh Rukshana SalimMithlesh SinghNo ratings yet
- CandidiasisDocument27 pagesCandidiasisWr Newgate50% (2)
- CCG Elderholme Responses To Final ReportDocument24 pagesCCG Elderholme Responses To Final ReportLeonard BeddowsNo ratings yet
- Shallo El Hard I90 BDocument2 pagesShallo El Hard I90 Belhard shalloNo ratings yet
- Course Task Unit 3Document2 pagesCourse Task Unit 3BSN 1-YA-22 ELITIONG, MARY JEAN A.No ratings yet
- The Health Bank (THB) Connected Care Program A Pilot Study of Remote Monitoring For The Management of Chronic Conditions Focusing On DiabetesDocument5 pagesThe Health Bank (THB) Connected Care Program A Pilot Study of Remote Monitoring For The Management of Chronic Conditions Focusing On DiabetesInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Role of Ayurveda in Treating Cervical ErosionDocument9 pagesRole of Ayurveda in Treating Cervical Erosionrazvan rotaruNo ratings yet
- Evidence 1.15.9-Change Log To Demonstrate The Differences Between 2017 and 2021 Edition PDFDocument13 pagesEvidence 1.15.9-Change Log To Demonstrate The Differences Between 2017 and 2021 Edition PDFKhalid ElwakilNo ratings yet
- Hypertension: Facts, Causes, Prevention and TreatmentDocument18 pagesHypertension: Facts, Causes, Prevention and TreatmentasepNo ratings yet
- Pulsed Dye Laser Therapy For Cutaneous Vascular LesionsDocument3 pagesPulsed Dye Laser Therapy For Cutaneous Vascular LesionsOogway MasterNo ratings yet
- Helping Babies Breathe™ 06.27.2014Document18 pagesHelping Babies Breathe™ 06.27.2014Emily EresumaNo ratings yet
- Additional File 3 - JBI ChecklistsDocument10 pagesAdditional File 3 - JBI Checklistsbella friscaamaliaNo ratings yet
- EthambutolDocument1 pageEthambutolSibel ErtuğrulNo ratings yet
- Pediatric Ophthalmology DR - JusufDocument25 pagesPediatric Ophthalmology DR - JusufAmira AlhaddarNo ratings yet
- Critical Reasoning Questions for Schizoaffective DisorderDocument2 pagesCritical Reasoning Questions for Schizoaffective DisorderjessyNo ratings yet
- NCP DrainageDocument3 pagesNCP DrainageRuby GuarinNo ratings yet
- Den 437Document6 pagesDen 437Prince AhmedNo ratings yet
- BBBFDocument3 pagesBBBFSkAliHassanNo ratings yet
- Student Response Sheet: PurposeDocument4 pagesStudent Response Sheet: PurposeYoshi NNo ratings yet
- MalariaDocument38 pagesMalariaMehroze FatimaNo ratings yet
- Pathology Situational EthicsDocument28 pagesPathology Situational Ethicsmohitsingla_86No ratings yet
- Guidelines For 1st Quarter AY 2022-2023Document12 pagesGuidelines For 1st Quarter AY 2022-2023Zhen ChiNo ratings yet
- Healthcare Stats - Assignment #2Document6 pagesHealthcare Stats - Assignment #2erickgregs0% (1)
- Hepatic Dysfunction in Dengue Fever - A ProspectiveDocument20 pagesHepatic Dysfunction in Dengue Fever - A ProspectiveSanjay RaoNo ratings yet
- Epidemiology & Health Information: NU1103 Tara Brookes @tarapb8Document40 pagesEpidemiology & Health Information: NU1103 Tara Brookes @tarapb8smartisaacNo ratings yet
- Endometritis Unrelated To Pregnancy - UpToDateDocument9 pagesEndometritis Unrelated To Pregnancy - UpToDateLeoberto Batista Pereira SobrinhoNo ratings yet
- Helicopter interventions for polytraumatized patients in North-East RomaniaDocument2 pagesHelicopter interventions for polytraumatized patients in North-East RomaniaN.DanielaNo ratings yet
- How To Setup Biotrans ?Document21 pagesHow To Setup Biotrans ?Agoes TreeyantNo ratings yet
- Medication Safety UnitDocument58 pagesMedication Safety Unitfarmasi_hmNo ratings yet
- NEET MDS 2021 Recall 151-200 Questions PDFDocument183 pagesNEET MDS 2021 Recall 151-200 Questions PDFMahima Mishra100% (1)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (402)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 3.5 out of 5 stars3.5/5 (2)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (78)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (13)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- Techniques Exercises And Tricks For Memory ImprovementFrom EverandTechniques Exercises And Tricks For Memory ImprovementRating: 4.5 out of 5 stars4.5/5 (40)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 5 out of 5 stars5/5 (4)
- The Ultimate Guide To Memory Improvement TechniquesFrom EverandThe Ultimate Guide To Memory Improvement TechniquesRating: 5 out of 5 stars5/5 (34)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 5 out of 5 stars5/5 (4)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisFrom EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisRating: 5 out of 5 stars5/5 (8)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 3.5 out of 5 stars3.5/5 (33)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Summary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisFrom EverandSummary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisRating: 5 out of 5 stars5/5 (3)
- The Happiness Trap: How to Stop Struggling and Start LivingFrom EverandThe Happiness Trap: How to Stop Struggling and Start LivingRating: 4 out of 5 stars4/5 (1)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsFrom EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsNo ratings yet
- The Tennis Partner: A Doctor's Story of Friendship and LossFrom EverandThe Tennis Partner: A Doctor's Story of Friendship and LossRating: 4.5 out of 5 stars4.5/5 (4)