Professional Documents
Culture Documents
Bacterial Infections: Understanding New Developments in the Diagnosis of Extrapulmonary Tuberculosis
Uploaded by
Retno ManggalihOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Bacterial Infections: Understanding New Developments in the Diagnosis of Extrapulmonary Tuberculosis
Uploaded by
Retno ManggalihCopyright:
Available Formats
BACTERIAL INFECTIONS
Extrapulmonary What’s new?
tuberculosis C The incidence of extrapulmonary TB (EPTB) in the UK is
Angela Houston increasing year-on-year
C Rising HIV prevalence and expanding use of immunomodula-
Derek Clive Macallan tory drugs such as anti-tumour necrosis factor have contributed
to the increase in EPTB
C Novel molecular diagnostics including nucleic acid amplification
tests (NAAT) and antigen detection assays have improved
Abstract
detection of TB and massively accelerated detection of drug
Extrapulmonary tuberculosis (EPTB) now represents about half of all diag-
resistance
nosed cases of TB in the UK and is seen increasingly in patients with
C Multi-drug resistant EPTB (as for pulmonary disease) is
immunosuppression or HIV. It is usually caused by reactivation of latent
increasing e highlighting the need for samples for NAAT/culture
infection and may cause disease at almost any site in the body. Most com-
mon sites include lymph nodes (19%), pleura (7%), gastrointestinal tract
(4%), bone (6%), CNS (3%) and genitourinary system (1%). Its manifesta-
tions depend on the site of disease, making diagnosis challenging as General principles of EPTB
EPTB may mimic many other diseases. Hence TB should be considered Epidemiology
in the differential diagnosis of any sick patient. A diagnosis of EPTB The incidence of TB in the UK has been increasing over the last
should trigger a search for concomitant pulmonary disease, which has im- decade and with it the incidence of EPTB, which represents about
plications for infectivity, and an HIV test (as with any TB diagnosis). half of all diagnosed TB cases.1 The most important risk factors
Obtaining appropriate samples for microbiological diagnosis is vital for for EPTB are shown in Table 1. Immunodeficiency increases both
effective management, especially as drug-resistance becomes more com- the risk of TB occurring (either primary or reactivation TB), and
mon. Treatment is generally with standard quadruple therapy for 6 the risk of extrapulmonary spread, if active disease does occur.
months (extended in TB meningitis); adjunctive steroid therapy is of In otherwise healthy people, most EPTB is presumed to arise
proven value in TB pericarditis and meningitis. from reactivation of latent infection, acquired during a primary
infection that could have occurred many years earlier.
Keywords tuberculosis; extrapulmonary tuberculosis; granuloma;
HIV; lymphadenitis; miliary TB; pericarditis; spondylodiscitis; Xpert Pathology
MTB/RIF As for pulmonary disease, the inflammatory response to myco-
bacterial invasion usually takes the form of granuloma forma-
tion. Although other diseases, such as sarcoid, can generate
granuloma, caseation is strongly indicative of TB. Pus formation
is characteristic and may cause extensive tissue damage; the
absence of an acute inflammatory infiltrate explains why such
Introduction abscesses may be ‘cold’. Disease may range from multi-bacillary,
as in miliary disease, to paucibacillary, where a very small
The most common site for infection with Mycobacterium tuber- number of bacteria generate a disproportionate destructive local
culosis (TB) is the lungs (representing about 51% of UK cases1), inflammatory response.
but dissemination may occur to any part of the body, resulting in
extrapulmonary tuberculosis (EPTB). Most common sites Diagnostics
include lymph nodes (19%), pleura (7%), the gastrointestinal As for TB in general, the importance of obtaining a positive culture
tract (4%), bone (6%), CNS (3%) and genitourinary system cannot be over-estimated, not least to exclude drug-resistant TB.
(1%) (Figure 1).1 Disseminated or miliary disease (w3% of UK EPTB is often hard to diagnose by microscopy because tissue may
cases) can also affect any organ. EPTB is under-recognized and be difficult to sample and tissue bacillary burden is often low.
diagnosis is often delayed, so it is important to appreciate the Characteristic histology (granuloma ! caseation) and imaging
variety of different organ-specific clinical scenarios with which it may be sufficient to mandate treatment whilst awaiting cultures.
may present, as well as the non-specific systemic symptoms of Novel molecular diagnostics have advanced our ability to detect
TB, such as fevers, night sweats and weight loss. and define TB (Table 2). Currently, the most promising of these is
the Xpert MTB/RIF,2,3 although the next few years will see more
diagnostic tests emerge from the development pipeline.4
Angela Houston BSc(Hons) MBchB DTM&H MRCP(UK) MSc FRCPath is an SpR in
Infectious Diseases and Medical Microbiology, Clinical Infection Unit, St Treatment
George’s Hospital, London, UK. Conflicts of interest: none declared. Treatment of EPTB is the same as for pulmonary TB, except that
the duration of treatment is extended for disease at some sites (12
Derek Clive Macallan MA PhD DTM&H FRCP is Professor of Infectious months for TB meningitis; some advocate extended treatment for
Diseases and Medicine, St George’s University of London, London, UK. TB of bone). Standard TB treatment comprises four drugs:
Conflicts of interest: none declared. isoniazid (H) rifampicin (R) pyrazinamide (Z) and ethambutol
MEDICINE 42:1 18 ! 2014 Elsevier Ltd. All rights reserved.
BACTERIAL INFECTIONS
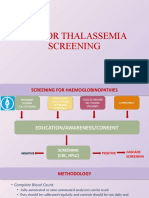
Proportion of TB reported to Public Health England New developments in the diagnosis of extrapulmonary
2000-2011 tuberculosis
miliary CNS
bone 3% 3% genitourinary C Automated DNA tests (e.g. Xpert MTB/RIF) are rapid tests
6% 1% (w2 hours) that detect the presence of MTB DNA and test for
gastrointestinal mutations in the rpoB gene
4% C In extrapulmonary samples, the overall sensitivity is 77.3e95%
and specificity 99e100%, equivalent to tuberculosis (TB) liquid
pleural culture3,5
7% C rpoB mutations identify 95% of resistance to rifampicin
(taken as an indicator of multi-drug resistant TB). This
other extra- represents a huge advance in TB diagnostics
pulmonary
pulmonary C Urine enzyme-linked immunosorbent assay (dipstick) tests
51%
6% extra thoracic (Determine TB-LAM ) detect the mycobacterial cell wall
lymphadenitis lipopolysaccharide antigen, lipoarabinomannan (LAM).
19%
Although still in development, they have potential as a low-cost,
point-of-care test to detect disseminated TB in highly
immunosuppressed patients (advanced HIV with CD4
count <200 cells/mm3 e also those most likely to benefit
Figure 1 from prompt treatment)6,7
(E): HRZE is given for a 2-month intensive phase, followed by HR Table 2
for 4 months (continuation phase).8
Specific extrapulmonary TB syndromes by disease site lymphadenitis may present with dysphagia or recurrent laryngeal
nerve involvement; abdominal/peritoneal disease, usually
Miliary TB affecting periportal, mesenteric or peri-pancreatic nodes, often
Miliary TB results from massive lympho-haematogeneous spread causes non-specific abdominal pain. Ultrasound or computerized
throughout the body. It accounts for 3% of EPTB cases and is tomographic (CT) imaging may show matted mesenteric lymph
associated with immunodeficiency. Infection is multi-bacillary, nodes with fat stranding and oedema. Rarely, enlarged lymph
with foci in many organs and mortality is high.9 The term nodes cause obstructive symptoms in the liver (presenting with
‘miliary’ (Manget, 1700) refers to the resemblance of pulmonary jaundice) or renal vasculature.
and hepatic nodules to millet seeds. Classically, these appear on Fine-needle aspiration (FNA) of the affected node is recom-
chest radiology as multiple small ("2 mm), discrete opacities. mended for mycobacterial molecular diagnostics and culture,
and to exclude differentials such as malignancy or other in-
TB lymphadenitis
fections (e.g. Bartonella, Toxoplasma) (Table 2).10 Excision bi-
Lymphadenitis is the most common presentation of EPTB in both
opsy may be considered if the diagnosis is in doubt. The yield of
children and adults (19% of UK TB cases). It usually represents
acid-fast bacilli (AFB) from a smear is poor but increases in pa-
reactivation from latent TB, although cervical disease may be
tients co-infected with HIV.10
caused by local spread from direct infection of tonsils or ade-
TB lymphadenitis often follows a waxing and waning course,
noids. The most common sites are the anterior or posterior cer-
even during treatment. Worsening on treatment may be attrib-
vical and submandibular nodes.
utable to paradoxical reactions (an enhanced immune response
TB lymphadenitis is usually painless. On palpation, nodes are
to dying mycobacteria). Aspiration of abscesses may relieve
firm but groups may become matted together with induration of
symptoms temporarily, although repeated aspiration carries a
overlying skin. Tissue necrosis with formation of fluctuant ab-
small risk of sinus or fistula formation. Treatment is with stan-
scesses is common and abscesses may discharge with sinus
dard quadruple therapy; the benefit of corticosteroids is debat-
formation. Symptoms depend upon site: mediastinal TB
able, although they do seem to expedite symptomatic
improvement.
Pleural TB
Risk factors for extrapulmonary tuberculosis Symptoms of pleural TB include pleuritic chest pain and breath-
C HIV infection lessness, associated with fevers and night sweats. Radiology may
C Tumour necrosis factor-a antagonists (e.g. Infliximab) show pleural effusions, even in the absence of lung parenchymal
C Corticosteroids changes. The pleural fluid is an exudate with high protein, low
C Malignancy glucose and often lymphocytosis. AFB are rarely visible but
C Female gender pleural fluid becomes culture positive in up to 75% of patients;
C Non-smoker adenosine deaminase analysis is useful, having an 88% sensi-
tivity for TB diagnosis.11 Diagnosis can also be aided by pleural
Table 1 biopsy (for histology and culture) and the use of video-assisted
MEDICINE 42:1 19 ! 2014 Elsevier Ltd. All rights reserved.
BACTERIAL INFECTIONS
thoracic surgery (VATS). The differential diagnosis for pleural symptoms. Plain X-rays may be deceptively normal and CT or
effusion is obviously wide, notably including para-pneumonic magnetic resonance (MR) imaging is often needed for diagnosis.
effusions, adenocarcinoma and malignant mesothelioma. Aspiration of collections and/or biopsy of the affected bone may
aid diagnosis and drainage may expedite recovery. TB treatment
Spinal and bone TB should be started immediately with standard quadruple therapy
TB affecting bones accounts for 12% of EPTB cases and 6% of all for 6e9 months. Adjuvant corticosteroids are recommended if
TB notifications in the UK.1 The most common site of infection is there is evidence of CNS or dural involvement. Joint manage-
the spine (9% of EPTB), followed by other large joints such as ment with orthopaedic or neurosurgeons experienced in the
the hip, knee and shoulder. Spinal TB comprises several patho- management of TB spine is essential to assess spinal stability and
logical entities including vertebral osteomyelitis, spondylitis and the need for external support or operative stabilization.
discitis (or spondylodiscitis, “Pott’s disease”) (Figure 2). The TB affecting other bones and joints is less common. Most
infection usually begins in the anterior aspect of the vertebral cases present with bone or soft tissue swelling, often with sinus
body adjacent to the subchondral plate, spreading to the adjacent formation. There is no clear evidence to support the role of
disc, although in children the sequence may be reversed, pro- surgery and drainage or sinus repair. Sinus formation can be
gressing from vascularized disc to bone. Progressive bone particularly troublesome and can take months if not years to
destruction may lead to vertebral collapse and kyphosis with heal, even with fully drug-sensitive organisms.
spinal gibbus formation (anterior angulation). Destructive cold
abscesses may form and commonly extend into adjacent liga- Abdominal TB
ments and soft tissues, especially the psoas muscle (psoas Gastrointestinal TB has a predilection for the terminal ileum;
abscess). Narrowing of the spinal canal by deformity, abscess- thickening or ulceration in this area may easily be mistaken for
formation, granulation tissue or direct dural invasion may result Crohn’s disease. Conversely, large bowel disease may be diag-
in spinal cord compression, a neurosurgical emergency.12,13 nosed radiologically as cancer. Complications include perforation
Typically there is a long history (#6 months) of fluctuating and TB peritonitis. Diagnosis is difficult as symptoms (abdominal
non-specific back pain, accompanied by constitutional pain, fevers, weight loss) are non-specific. Radiological findings
may include bowel thickening, lymphadenopathy, ascites, free
gas suggestive of perforation, and abscess-formation, but the
most important diagnostic aspect is a high index of suspicion in
patients with risk factors for TB.14 Laparoscopic or colonoscopic
biopsies are useful for histology and culture.
Urogenital TB
Urogenital TB comprises renal disease, ureteric disease and gen-
ital infection. The diagnosis of renal disease is easily missed, as
back or flank pain, dysuria or constitutional symptoms occur in
only 30% of patients.15 Renal TB is usually unilateral and rarely
causes renal failure; the exception is tuberculous interstitial
nephritis, which may affect both kidneys. Renal abscesses
(Figure 3) may destroy the entire renal parenchyma. Pelvo-
calyceal involvement may result in thickening of the collecting
system; more distally, ureteric fibrosis and stricture formation
may cause hydronephrosis,16 whereas TB of the bladder wall may
lead to fibrosis. Genital tract infection is unusual but most
commonly affects the prostate of men or endometrium of women.
Ovarian, tubal and testicular disease may result in infertility.
Depending on site, diagnosis depends on a combination of
early-morning urine samples (EMUs) (when the concentration of
AFBs in the urine is highest), biopsies and radiology. EMUs are
insensitive but molecular tests may improve diagnostic yield
(Table 2).6 Renal biopsy may show granulomatous interstitial
nephritis, often with multifocal caseous necrosis. Cystoscopy
with biopsies of bladder or ureteric/prostate tissue may also be
helpful. Imaging or the renal tract may show a characteristically
‘beaded’ ureter (ureteritis cystica).17
Pericardial TB
Although rare (accounting for <1% of EPTB), pericardial TB
Figure 2 MR imaging in TB spondylodiscitis. The lumbar spine is most
commonly affected, but involvement can occur at multiple sites, as seen merits consideration because it is potentially life-threatening. TB
here (arrows). Importantly, look for evidence of spinal cord compression, pericarditis can present either acutely, with massive pericardial
which is a neurosurgical emergency. fluid accumulation causing cardiac tamponade, or sub-acutely
MEDICINE 42:1 20 ! 2014 Elsevier Ltd. All rights reserved.
BACTERIAL INFECTIONS
Medical emergencies in extrapulmonary TB e the
‘alarm bells’
Syndromes or complications that need urgent intervention include:
C Miliary disease may paradoxically worsen on treatment initia-
tion e consider corticosteroids
C TB meningitis e beware of increased intracranial pressure (see
MEDICINE 41(12): 683-685)
C Check for spinal cord compression in spinal TB e consider
surgical decompression and add corticosteroids
C Look for cardiac tamponade in pericardial TB e give cortico-
steroids and consider drainage/pericardiectomy
C Hydronephrosis in renal/urogenital TB may need stenting
C Adrenal disease may precipitate an addisonian crisis, which is
easy to overlook e corticosteroid replacement may be required
C Beware of vascular obstruction due to mass lesions (cold ab-
scesses) or lymphadenopathy
Table 3
Other forms of extrapulmonary TB
Tuberculous meningitis is not discussed here as it is covered in
MEDICINE 41(12): 683-685. Other EPTB sites that merit consid-
eration include TB of the larynx because of its very high infec-
tivity; cutaneous TB, either as primary disease, ‘scrofuloderma’,
Figure 3 Urogenital TB. Histological section through a kidney containing a or local spread from adjacent affected organs; and adrenal
tuberculous abscess. Reproduced with kind permission of the Department involvement which, although rare, can result in acute adrenal
of Pathology, University of Cambridge.
insufficiency or the syndrome of inappropriate anti-diuretic
hormone (SIADH) secretion.19 Non-specific syndromes such as
with constrictive pericarditis. In acute disease, the chest X-ray haemophagocytic syndrome have also been described in EPTB.
shows cardiomegaly (Figure 4) and echocardiography reveals a
large pericardial effusion. Aspiration/drainage may control the Conclusion
acute situation but surgical intervention (forming an open peri-
TB can affect any part of the body, hence this review cannot be
cardial window to prevent fluid reaccumulation) may also be
exhaustive. EPTB is a great imitator and can easily be mis-
required (and also provides tissue for histology/culture). Corti-
diagnosed. Key aspects of management include a high index of
costeroids expedite clinical recovery and reduce mortality.18
suspicion for the disease, particularly in those with epidemio-
logical risk factors or who are immunosuppressed, and taking
appropriate specimens for histology and culture. Therapeutic
outcomes are generally good, provided diagnosis is prompt and
complications can be avoided (Table 3). A
REFERENCES
1 PHE. Tuberculosis in the UK: 2012 report. Public Health England,
2012 (accessed 5 November 2013). http://www.hpa.org.uk/webw/
HPAweb&HPAwebStandard/HPAweb_C/1317134916916.
2 Hillemann D, Ru €sch-Gerdes S, Boehme C, Richter E. Rapid molecular
detection of extrapulmonary tuberculosis by the automated Gen-
eXpert MTB/RIF system. J Clin Microbiol 2011; 49: 1202e5.
3 Boehme CC, Nabeta P, Hillemann D, et al. Rapid molecular detection of
tuberculosis and rifampin resistance. N Engl J Med 2010; 363: 1005e15.
4 Lawn SD, Mwaba P, Bates M, et al. Advances in tuberculosis di-
agnostics: the Xpert MTB/RIF assay and future prospects for a point-
of-care test. Lancet Infect Dis 2013; 13: 349e61.
5 Causse M, Ruiz P, Guti"errez-Aroca JB, Casal M. Comparison of two
Figure 4 TB pericarditis. Chest radiograph showing cardiomegaly and molecular methods for rapid diagnosis of extrapulmonary tubercu-
pleural effusion. losis. J Clin Microbiol 2011; 49: 3065e7.
MEDICINE 42:1 21 ! 2014 Elsevier Ltd. All rights reserved.
BACTERIAL INFECTIONS
6 Peter J, Green C, Hoelscher M, Mwaba P, Zumla A, Dheda K. Urine 15 Eastwood JB, Corbishley CM, Grange JM. Tuberculosis and the kidney.
for the diagnosis of tuberculosis: current approaches, clinical J Am Soc Nephrol 2001; 12: 1307e14.
applicability, and new developments. Curr Opin Pulm Med 2010; 16 Figueiredo AA, Lucon AM, Arvellos AN, et al. A better understanding
16: 262e70. http://dx.doi.org/10.1097/MCP.0b013e328337f23a. of urogenital tuberculosis pathophysiology based on radiological
7 Lawn S. Point-of-care detection of lipoarabinomannan (LAM) in urine findings. Eur J Radiol 2010; 76: 246e57.
for diagnosis of HIV-associated tuberculosis: a state of the art review. 17 Matos MJ, Bacelar MT, Pinto P, Ramos I. Genitourinary tuberculosis.
BMC Infect Dis 2012; 12: 103. Eur J Radiol 2005; 55: 181e7.
8 WHO. Guidelines for treatment of tuberculosis. 4th edn. Geneva: 18 Trautner BW, Darouiche RO. Tuberculous pericarditis: optimal diag-
World Health Organisation, 2010. http://www.who.int/tb/publications/ nosis and management. Clin Infect Dis 2001; 33: 954e61.
2010/9789241547833/en/index.html. 19 Kinjo T, Higuchi D, Oshiro Y, et al. Addison’s disease due to tuber-
9 Sharma SK, Mohan A, Sharma A, Mitra DK. Miliary tuberculosis: new culosis that required differentiation from SIADH. J Infect Chemother
insights into an old disease. Lancet Infect Dis 2005; 5: 415e30. 2009; 15: 239e42.
10 Nayak S, Puranik SC, Deshmukh SD, Mani R, Bhore AV, Bollinger RC.
Fine-needle aspiration cytology in tuberculous lymphadenitis of pa-
tients with and without HIV infection. Diagn Cytopathol 2004; 31:
204e6. Practice points
11 Villegas MV, Labrada LA, Saravia NG. Evaluation of polymerase chain
reaction, adenosine deaminase, and interferon-g in pleural fluid for C Always try to get samples for microbiology in patients with
the differential diagnosis of pleural tuberculosis. Chest J 2000; 118: suspected TB; discuss appropriate sampling with a microbi-
1355e64. ology doctor first
12 Pertuiset E, Beaudreuil J, Liot"e F, et al. Spinal tuberculosis in adults: a C Always look for pulmonary TB in patients with extrapulmonary
study of 103 cases in a developed country, 1980e1994. Medicine TB as concurrent pulmonary TB has implications for infectivity,
1999; 78: 309e20. isolation and contact tracing
13 Cormican L, Hammal R, Messenger J, Milburn HJ. Current difficulties in C Always perform an HIV test in anyone with TB
the diagnosis and management of spinal tuberculosis. Postgrad Med C early-morning urine samples should be taken in patients with
J 2006; 82: 46e51. suspected renal TB
14 Tan K-K, Chen K, Sim R. The spectrum of abdominal tuberculosis in a C Be aware of increasing incidence of multi-drug resistant TB
developed country: a single institution’s experience over 7 years. C Check and replace vitamin D, if low, in patients with TB
J Gastrointest Surg 2009; 13: 142e7.
MEDICINE 42:1 22 ! 2014 Elsevier Ltd. All rights reserved.
You might also like
- Infections in Cancer Chemotherapy: A Symposium Held at the Institute Jules Bordet, Brussels, BelgiumFrom EverandInfections in Cancer Chemotherapy: A Symposium Held at the Institute Jules Bordet, Brussels, BelgiumNo ratings yet
- Viral Hepatitis: Acute HepatitisFrom EverandViral Hepatitis: Acute HepatitisResat OzarasNo ratings yet
- Bacterial Infections: Key Points on Diagnosing and Treating Extrapulmonary TuberculosisDocument6 pagesBacterial Infections: Key Points on Diagnosing and Treating Extrapulmonary TuberculosisRetno ManggalihNo ratings yet
- Tuberculous pleural effusionDocument14 pagesTuberculous pleural effusionstephanie bojorquezNo ratings yet
- Extrapulmonary TuberculosisDocument19 pagesExtrapulmonary Tuberculosisanitaabreu123No ratings yet
- Current Medical Management of Pulmonary TuberculosisDocument9 pagesCurrent Medical Management of Pulmonary TuberculosisFaradilla FirdausaNo ratings yet
- Tuberculous Meningitis: Challenges in Diagnosis and ManagementDocument7 pagesTuberculous Meningitis: Challenges in Diagnosis and ManagementNursyahidah IdrisNo ratings yet
- JCTH 7 140Document9 pagesJCTH 7 140evanNo ratings yet
- Non-Cystic Fibrosis Bronchiectasis: Diagnosis and Management in 21st CenturyDocument10 pagesNon-Cystic Fibrosis Bronchiectasis: Diagnosis and Management in 21st CenturyIvan VeriswanNo ratings yet
- CTB Metastatic AbscessDocument3 pagesCTB Metastatic Abscessjhon_4548No ratings yet
- Tuberculosis or TBDocument8 pagesTuberculosis or TBJ Russel DichosoNo ratings yet
- 6.2. NeumoníaDocument5 pages6.2. NeumoníaErmilo José Echeverría OrtegónNo ratings yet
- RESPI (PBL2) - Mohamad Arbian Karim - FMUI20Document8 pagesRESPI (PBL2) - Mohamad Arbian Karim - FMUI20Mohamad Arbian KarimNo ratings yet
- Extrapulmonary Tuberculosis: Are Statistical Reports Accurate?Document10 pagesExtrapulmonary Tuberculosis: Are Statistical Reports Accurate?Utari UbNo ratings yet
- Tuberculous Meningitis: Neurological Aspects of Tropical DiseaseDocument11 pagesTuberculous Meningitis: Neurological Aspects of Tropical DiseaseullyfatmalaNo ratings yet
- J Neurol 2019 07 007Document7 pagesJ Neurol 2019 07 007ONENG IFAYANINo ratings yet
- 24-Article Text-240-1-10-20211029Document10 pages24-Article Text-240-1-10-20211029fitrianiNo ratings yet
- Book 2Document9 pagesBook 2AbdouldjalilNo ratings yet
- Hepatic Tuberculosis (New)Document23 pagesHepatic Tuberculosis (New)khunleangchhun0% (1)
- TuberculosisDocument9 pagesTuberculosisDana Abdallah Jalal AlnimriNo ratings yet
- 1 s2.0 S128645792030099X MainDocument7 pages1 s2.0 S128645792030099X MainNia KurniawanNo ratings yet
- Assignment: - TuberculosisDocument9 pagesAssignment: - TuberculosisAakash SahaNo ratings yet
- Active Pulmonary Tuberculosis - Something Old, Something New, Something Borrowed, Something BlueDocument13 pagesActive Pulmonary Tuberculosis - Something Old, Something New, Something Borrowed, Something Blueoralposter PIPKRA2023No ratings yet
- Tuberculous Meningitis: Neurological Aspects of Tropical DiseaseDocument12 pagesTuberculous Meningitis: Neurological Aspects of Tropical DiseaseBayuHernawanRahmatMuhariaNo ratings yet
- TuberculosisDocument76 pagesTuberculosissashmita rautNo ratings yet
- Review Article: Challenges in Endobronchial Tuberculosis: From Diagnosis To ManagementDocument9 pagesReview Article: Challenges in Endobronchial Tuberculosis: From Diagnosis To ManagementInsinyur_077No ratings yet
- Meningitis TBCDocument12 pagesMeningitis TBCJessica L. AlbornozNo ratings yet
- 1-S2.0-S1726490112000895-Main Baru - En.idDocument5 pages1-S2.0-S1726490112000895-Main Baru - En.idHenandwita Fadilla PravitasariNo ratings yet
- Tuberculosis: Therapeutics IIDocument54 pagesTuberculosis: Therapeutics IIdstu20No ratings yet
- Pulmonary Tuberculosis: Up-to-Date Imaging and Management: Yeon Joo Jeong Kyung Soo LeeDocument11 pagesPulmonary Tuberculosis: Up-to-Date Imaging and Management: Yeon Joo Jeong Kyung Soo LeeElza Astri SafitriNo ratings yet
- TUBERCULOSISDocument16 pagesTUBERCULOSISMehveen KashifNo ratings yet
- Global Epidemiology of Tuberculosis: Philippe Glaziou, MD Katherine Floyd, PHD Mario C. Raviglione, MDDocument15 pagesGlobal Epidemiology of Tuberculosis: Philippe Glaziou, MD Katherine Floyd, PHD Mario C. Raviglione, MDbrachiuroNo ratings yet
- Tuberculosis Unit 1 Lecture - 1Document39 pagesTuberculosis Unit 1 Lecture - 1Kubra Rasool100% (1)
- Kansasiiand M. Avium), May Be Positive For AFB Stain. Thus, A PositiveDocument8 pagesKansasiiand M. Avium), May Be Positive For AFB Stain. Thus, A PositiveMarisa PetersonNo ratings yet
- Pneumonia Caused by M. TBDocument8 pagesPneumonia Caused by M. TBerniherawatia658No ratings yet
- A Presentation On-: Dr. Nikhil Oza Intern BvdumcDocument43 pagesA Presentation On-: Dr. Nikhil Oza Intern BvdumcMaheboob GanjalNo ratings yet
- Diagnostic Challenges in CervicalDocument6 pagesDiagnostic Challenges in CervicalOgi Y. Casesarando PurbaNo ratings yet
- Pulmonary Tuberclosis: Presented By:Dr Sobia Mangi Houseofficer at Medical Unit 3Document41 pagesPulmonary Tuberclosis: Presented By:Dr Sobia Mangi Houseofficer at Medical Unit 3Feroz RaZa SoomrOoNo ratings yet
- Gastrointestinal Tuberculosis: Singapore Medical Journal July 2009Document10 pagesGastrointestinal Tuberculosis: Singapore Medical Journal July 2009carmenNo ratings yet
- Central Nervous System Tuberculosis: John M. LeonardDocument10 pagesCentral Nervous System Tuberculosis: John M. LeonardMarcela Catalina Fandiño VargasNo ratings yet
- FullDocument17 pagesFullambiebieNo ratings yet
- Review: Atypical Pathogen Infection in Community-Acquired PneumoniaDocument7 pagesReview: Atypical Pathogen Infection in Community-Acquired PneumoniaDebi SusantiNo ratings yet
- Contents XTSCDocument3 pagesContents XTSCWulandari WulandariNo ratings yet
- TB KuyuxDocument5 pagesTB KuyuxzzulmanafNo ratings yet
- Jasim2018 PDFDocument8 pagesJasim2018 PDFCorona FingerNo ratings yet
- Pancreatic Tuberculosis Diagnosis UpdateDocument24 pagesPancreatic Tuberculosis Diagnosis UpdatesamudraandiNo ratings yet
- Bourgi 2017Document9 pagesBourgi 2017winter wineNo ratings yet
- Non-Tuberculous Mycobacterial Pulmonary Infections: ReviewDocument12 pagesNon-Tuberculous Mycobacterial Pulmonary Infections: Reviewmgoez077No ratings yet
- Bronchiectasis - Diagnosis and TreatmentDocument9 pagesBronchiectasis - Diagnosis and Treatmentalfred1294No ratings yet
- International Journal of Infectious Diseases: Evangelia Skoura, Alimuddin Zumla, Jamshed BomanjiDocument7 pagesInternational Journal of Infectious Diseases: Evangelia Skoura, Alimuddin Zumla, Jamshed BomanjiIndah Putri UtamiNo ratings yet
- 4 MMMMMMMDocument5 pages4 MMMMMMMSatriaAuliansyahNo ratings yet
- Fimmu 11 02161Document15 pagesFimmu 11 02161tatiana.balanici13No ratings yet
- Necrotizing Pneumonia (Aetiology, Clinical Features and Management)Document8 pagesNecrotizing Pneumonia (Aetiology, Clinical Features and Management)pachomdNo ratings yet
- Tuberculosis Diagnosis & TreatmentDocument7 pagesTuberculosis Diagnosis & TreatmentYashaswi ANo ratings yet
- Severe TuberculosisDocument4 pagesSevere TuberculosisAdelia GhosaliNo ratings yet
- Respiratory Medicine CME: Lancelot Mark Pinto, Arpan Chandrakant Shah, Kushal Dipakkumar Shah, Zarir Farokh UdwadiaDocument3 pagesRespiratory Medicine CME: Lancelot Mark Pinto, Arpan Chandrakant Shah, Kushal Dipakkumar Shah, Zarir Farokh UdwadiaLintang SuroyaNo ratings yet
- International Journal of Infectious Diseases: Evangelia Skoura, Alimuddin Zumla, Jamshed BomanjiDocument7 pagesInternational Journal of Infectious Diseases: Evangelia Skoura, Alimuddin Zumla, Jamshed BomanjiNita Julita CindayaNo ratings yet
- Accepted Manuscript: Clinics in DermatologyDocument30 pagesAccepted Manuscript: Clinics in DermatologyM AbhiNo ratings yet
- Miliary Tuberculosis: Surendra K. Sharma and Alladi MohanDocument22 pagesMiliary Tuberculosis: Surendra K. Sharma and Alladi MohanNidya PutriNo ratings yet
- TB Ped 2019Document14 pagesTB Ped 2019Edgar ronán Cabrera moralesNo ratings yet
- Fahy 2017Document7 pagesFahy 2017Retno ManggalihNo ratings yet
- Out 14Document11 pagesOut 14Retno ManggalihNo ratings yet
- Migraine and Body Mass Index Categories: A Systematic Review and Meta-Analysis of Observational StudiesDocument14 pagesMigraine and Body Mass Index Categories: A Systematic Review and Meta-Analysis of Observational StudiesRetno ManggalihNo ratings yet
- Jurnal 2Document7 pagesJurnal 2Retno ManggalihNo ratings yet
- Out 18Document8 pagesOut 18Retno ManggalihNo ratings yet
- Jurnal TB 1Document11 pagesJurnal TB 1Retno ManggalihNo ratings yet
- Chung 2014Document6 pagesChung 2014Retno ManggalihNo ratings yet
- Efficacy of Steroidal Vs Non-Steroidal Agents in Oral Lichen Planus: A Randomised, Open-Label StudyDocument9 pagesEfficacy of Steroidal Vs Non-Steroidal Agents in Oral Lichen Planus: A Randomised, Open-Label StudyRetno ManggalihNo ratings yet
- P 53Document8 pagesP 53Retno ManggalihNo ratings yet
- 679 1364 1 SMDocument5 pages679 1364 1 SMRetno ManggalihNo ratings yet
- Childhood Nephrotic Syndrome Management and Outcome - A Single Center Retrospective AnalysisDocument8 pagesChildhood Nephrotic Syndrome Management and Outcome - A Single Center Retrospective AnalysisRosi IndahNo ratings yet
- KepustakaanDocument1 pageKepustakaanRetno ManggalihNo ratings yet
- Surgical Aseptic Technique Sterile FieldDocument18 pagesSurgical Aseptic Technique Sterile FieldAsiah IsmailNo ratings yet
- Decision Making GuideDocument1 pageDecision Making GuideRetno ManggalihNo ratings yet
- Repro Duks IDocument7 pagesRepro Duks IRetno ManggalihNo ratings yet
- Who Guidelines For Safe SurgeryDocument173 pagesWho Guidelines For Safe SurgeryAhmed M Frieg100% (1)
- 440 664 1 SMDocument6 pages440 664 1 SMAdi Look-us KurniawanNo ratings yet
- Ann Rheum Dis 2015 Dejaco 1799 807Document11 pagesAnn Rheum Dis 2015 Dejaco 1799 807Retno ManggalihNo ratings yet
- BMJ I2610 Full-2Document6 pagesBMJ I2610 Full-2Retno ManggalihNo ratings yet
- Seminars in Arthritis and Rheumatism: Contents Lists Available atDocument11 pagesSeminars in Arthritis and Rheumatism: Contents Lists Available atRetno ManggalihNo ratings yet
- Whoqol BrefDocument5 pagesWhoqol BrefLynn Morrison WilliamsNo ratings yet
- J Gerontol A Biol Sci Med Sci-1997-Vitiello-M189-91Document3 pagesJ Gerontol A Biol Sci Med Sci-1997-Vitiello-M189-91Retno ManggalihNo ratings yet
- EAT 26test 3 20 10Document1 pageEAT 26test 3 20 10Retno ManggalihNo ratings yet
- Body Shape QuestionnaireDocument2 pagesBody Shape QuestionnaireCaleb Sylvester100% (2)
- Bipolar DisorderDocument9 pagesBipolar DisorderAnqelicus AsacinevaNo ratings yet
- Dass (Depresion Anxiety Stress Scale)Document5 pagesDass (Depresion Anxiety Stress Scale)Trian SatrioNo ratings yet
- Kuesioner Kualitas HidupDocument9 pagesKuesioner Kualitas HidupRetno ManggalihNo ratings yet
- !the H Book For 5th Year OSCE - Part 1Document147 pages!the H Book For 5th Year OSCE - Part 1farzzana100% (1)
- Chronology of Human Dentition & Tooth Numbering SystemDocument54 pagesChronology of Human Dentition & Tooth Numbering Systemdr parveen bathla100% (4)
- Chapter 27 - Anxiety-Related, Obsessive-Compulsive, Trauma and Stressor-Related, Somatic, and Dissociative DisordersDocument10 pagesChapter 27 - Anxiety-Related, Obsessive-Compulsive, Trauma and Stressor-Related, Somatic, and Dissociative DisordersKTNo ratings yet
- 1-Equine Digestion PowerPointDocument15 pages1-Equine Digestion PowerPointMazhar FaridNo ratings yet
- Bachelor of Medical Lab. Technology-BmltDocument33 pagesBachelor of Medical Lab. Technology-BmltSantosh KanelNo ratings yet
- Vital Signs ChecklistDocument21 pagesVital Signs ChecklistJapsay Francisco GranadaNo ratings yet
- Risk Prediction Model for Heart Failure in DiabetesDocument20 pagesRisk Prediction Model for Heart Failure in DiabetesjamesboendNo ratings yet
- Voice and Speech DisordersDocument2 pagesVoice and Speech DisordersVishal Gaurav100% (1)
- Sop For Thalassemia Screening Wwith NbsDocument11 pagesSop For Thalassemia Screening Wwith NbsUMMID WashimNo ratings yet
- Temu Ilmiah Reumatologi (TIR) 2023 - Perhimpunan Reumatologi IndonesiaDocument1 pageTemu Ilmiah Reumatologi (TIR) 2023 - Perhimpunan Reumatologi IndonesiabelanjayukdiNo ratings yet
- Ebp Picc Line - RevisedDocument6 pagesEbp Picc Line - Revisedapi-234544335No ratings yet
- 1 - Indocyanine Green-Enhanced Fluorescence To Assess BowelDocument7 pages1 - Indocyanine Green-Enhanced Fluorescence To Assess BowelIcaro DanielNo ratings yet
- Upper Airway Obstruction: Croup and Its DifferentialDocument36 pagesUpper Airway Obstruction: Croup and Its DifferentialJoseph Stans KasiryeNo ratings yet
- HYDRONEPHROSISDocument43 pagesHYDRONEPHROSISEureka RathinamNo ratings yet
- Type III Radix Entomolaris in Permanent Mandibular Second MolarDocument3 pagesType III Radix Entomolaris in Permanent Mandibular Second MolarGJR PUBLICATIONNo ratings yet
- HONRADO-Group 3 - Pedia NCPDocument7 pagesHONRADO-Group 3 - Pedia NCP2A - Nicole Marrie HonradoNo ratings yet
- Food Classes: FAT Water Vitamins, Minerals, & Roughage ProteinDocument25 pagesFood Classes: FAT Water Vitamins, Minerals, & Roughage Proteinuminoriah80% (5)
- Ascitis Quilosa Post Cirugía Abdominal: Caso Clínico y Revisión de La LiteraturaDocument7 pagesAscitis Quilosa Post Cirugía Abdominal: Caso Clínico y Revisión de La LiteraturaJuliet castilloNo ratings yet
- Denial Codes 05aug2020Document9 pagesDenial Codes 05aug2020naharmampillyNo ratings yet
- The Paleopathology of Specific Infectious Diseases From Southeastern Hungary: A Brief OverviewDocument6 pagesThe Paleopathology of Specific Infectious Diseases From Southeastern Hungary: A Brief OverviewLucía Chavarría RíosNo ratings yet
- Autophagy and CancerDocument349 pagesAutophagy and CancerSohibun21No ratings yet
- Heritage Health - Pre Auth FormDocument6 pagesHeritage Health - Pre Auth FormBOOKREADER_NOWNo ratings yet
- Vaccination Records - AdultsDocument2 pagesVaccination Records - AdultsverumluxNo ratings yet
- Apl 1Document45 pagesApl 1api-243480627No ratings yet
- Researchers and by Clinicians For Use With Their PatientsDocument3 pagesResearchers and by Clinicians For Use With Their PatientsAnton Henry MiagaNo ratings yet
- Medicine English Fun Activities Games Grammar Drills Grammar Guides 17199Document20 pagesMedicine English Fun Activities Games Grammar Drills Grammar Guides 17199LisleNo ratings yet
- Pharmacology and The Older AdultDocument26 pagesPharmacology and The Older AdultJether Joy Hyacinth VelardeNo ratings yet
- E383 Full PDFDocument11 pagesE383 Full PDFBarryNo ratings yet
- College of Nursing: Pharmacology Drug StudyDocument2 pagesCollege of Nursing: Pharmacology Drug StudyChristine Pialan SalimbagatNo ratings yet
- Expanding Consensus in Portal HypertensionDocument29 pagesExpanding Consensus in Portal HypertensionJosé Pepo Apey Reinoso100% (1)