Professional Documents
Culture Documents
Dental PPO20 - 2017
Uploaded by
SporkleCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Dental PPO20 - 2017
Uploaded by
SporkleCopyright:
Available Formats
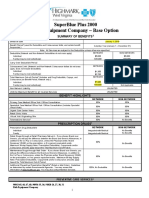
UnitedHealthcare® dental plan
Consumer MaxMultiplier In Network Only Options PPO 20 PIO40
NETWORK
Individual Annual Deductible $50
Family Annual Deductible $150
Annual Maximum Benefit* (The total benefit payable by the plan will not exceed the $1000 per person per calendar year
highest listed maximum amount for either Network or Non-Network services.)
Annual Deductible Applies to Preventive and Diagnostic Services No
Waiting Period 12 months for major services
NETWORK
COVERED SERVICES** BENEFIT GUIDELINES
PLAN PAYS***
DIAGNOSTIC SERVICES
Periodic Oral Evaluation 100% Limited to 2 times per consecutive 12 months.
Bitewing: Limited to 1 series of films per calendar year. Complete/Panorex: Limited to
Radiographs 100%
1 time per consecutive 36 months.
Lab and Other Diagnostic Tests 100%
PREVENTIVE SERVICES
Dental Prophylaxis (Cleanings) 100% Limited to 2 times per consecutive 12 months.
Limited to covered persons under the age of 16 years and limited to 2 times per
Fluoride Treatments 100%
consecutive 12 months.
Limited to covered persons under the age of 16 years and once per first or second
Sealants 100%
permanent molar every consecutive 36 months.
Space Maintainers 100% For covered persons under the age of 16 years, limit 1 per consecutive 60 months.
BASIC DENTAL SERVICES
Restorations (Amalgam or Anterior Composite)** 80% Multiple restorations on one surface will be treated as a single filling.
Covered as a separate benefit only if no other service was done during the visit other
Palliative Treatment 80% than X-rays.
General Anesthesia 80% When clinically necessary.
Covered only if prescribed to control habitual grinding, and limited to 1 guard every
Occlusal Guard 80% consecutive 36 months.
Simple Extractions 80% Limited to 1 time per tooth per lifetime.
MAJOR DENTAL SERVICES
Oral Surgery (includes surgical extractions) 50%
Perio Surgery: Limited to 1 quadrant or site per consecutive 36 months per surgical
area.
Periodontics 50% Scaling and Root Planing: Limited to 1 time per quadrant per consecutive 24 months.
Periodontal Maintenance: Limited to 2 times per consecutive 12 months following active
and adjunctive periodontal therapy, exclusive of gross debridement.
Endodontics 50% Root Canal Therapy: Limited to 1 time per tooth per lifetime.
Inlays/Onlays/Crowns** 50% Limited to 1 time per tooth per consecutive 60 months.
Full Denture/Partial Denture: Limited to 1 per consecutive 60 months. No additional
Dentures and other Removable Prosthetics 50%
allowances for precision or semi-precision attachments.
Fixed Partial Dentures (Bridges)** 50% Limited to 1 time per tooth per consecutive 60 months.
* This plan includes a maximum benefit award program. Some of the unused portion of your annual maximum benefit may be available in future benefit periods.
** Your dental plan provides that where two or more professionally acceptable dental treatments for a dental condition exist, your plan bases reimbursement on the least costly treatment alternative. If you
and your dentist have agreed on a treatment which is more costly than the treatment on which the plan benefit is based, you will be responsible for the difference between the fee for service rendered and
the fee covered by the plan. In addition, a pre-treatment estimate is recommended for any service estimated to cost over $500; please consult your dentist.
*** The network percentage of benefits is based on the discounted fee negotiated with the provider.
In accordance with the Illinois state requirement, a partner in a Civil Union is included in the definition of Dependent. For a complete description of Dependent Coverage, please refer to your Certificate of Coverage.
The Prenatal Dental Care (not available in WA) and Oral Cancer Screening programs are covered under this plan. The material contained in the above table is for informational purposes only and is not an offer of coverage. Please note
that the above provides only a brief, general description of coverage and does not constitute a contract. For a complete listing of your coverage, including exclusions and limitations relating to your coverage, please refer to your
Certificate of Coverage or contact your benefits administrator. If differences exist between this Summary Benefits and your Certificate of Coverage/benefits administrator, the Certificate/benefits administrator will govern. All terms and
conditions of coverage are subject to applicable state and federal laws. State mandates regarding benefit levels and age limitations may supersede plan design features.
UnitedHealthcare Dental® In Network Only (INO) Plan is either underwritten or provided by: UnitedHealthcare Insurance Company, Hartford, Connecticut; UnitedHealthcare Insurance Company of New York, Hauppage, New York;
Unimerica Insurance Company, Milwaukee, Wisconsin; Unimerica Life Insurance Company of New York, New York, New York; or United HealthCare Services, Inc.
100-10641 03/13 ©2013-2014 United HealthCare Services, Inc.
UnitedHealthcare/dental exclusions and limitations
Dental Services described in this section are covered when such services are:
A. Necessary;
B. Proviced by or under the direction of a Dentist or other appropriate provider as specifically described;
C. The least costly, clinically accepted treatment; and
D. Not excluded as described in the Section entitled, General Exclusions.
GENERAL LIMITATIONS GENERAL EXCLUSIONS
PERIODIC ORAL EVALUATION Limited to 2 times per consecutive 12 months. The following are not covered: 17. Attachments to conventional removable prostheses or
COMPLETE SERIES OR PANOREX RADIOGRAPHS Limited to 1 time per 1. Dental Services that are not necessary. fixed bridgework. This includes semi-precision or
consecutive 36 months. 2. Hospitalization or other facility charges. precision attachments associated with partial
3. Any dental procedure performed solely for dentures, crown or bridge abutments, full or partial
BITEWING RADIOGRAPHS Limited to 1 series of films per calendar year.
cosmetic/aesthetic reasons. (Cosmetic procedures are overdentures, any internal attachment associated
EXTRAORAL RADIOGRAPHS Limited to 2 films per calendar year.
those procedures that improve physical appearance.) with an implant prosthesis, and any elective
DENTAL PROPHYLAXIS Limited to 2 times per consecutive 12 months.
4. Reconstructive Surgery regardless of whether or not the
FLUORIDE TREATMENTS Limited to covered persons under the age of 16 endodontic procedure related to a tooth or root
surgery is incidental to a dental disease, injury, or
years, and limited to 2 times per consecutive 12 months. involved in the construction of a prosthesis of this
Congenital Anomaly when the primary purpose is to
nature.
SPACE MAINTAINERS Limited to covered persons under the age of 16 years, improve physiological functioning of the involved part of
limited to 1 per consecutive 60 months. Benefit includes all adjustments within 6 18. Procedures related to the reconstruction of a patient’s
the body.
months of installation. correct vertical dimension of occlusion (VDO).
5. Any dental procedure not directly associated with dental
SEALANTS Limited to covered persons under the age of 16 years, and once per disease. 19. Placement of dental implants, implant-supported
first or second permanent molar every consecutive 36 months. 6. Any dental procedure not performed in a dental setting. abutments and prostheses
7. Procedures that are considered to be Experimental, 20. Placement of fixed partial dentures solely for the
RESTORATIONS Multiple restorations on one surface will be treated as a
Investigational or Unproven. This includes purpose of achieving periodontal stability.
single filling.
pharmacological regimens not accepted by the American 21. Treatment of benign neoplasms, cysts, or other
PIN RETENTION Limited to 2 pins per tooth; not covered in addition to cast
Dental Association (ADA) Council on Dental pathology involving benign lesions, except
restoration.
Therapeutics. The fact that an Experimental, excisional removal. Treatment of malignant
INLAYS AND ONLAYS Limited to 1 time per tooth per consecutive 60 months.
Investigational or Unproven Service, treatment, device or neoplasms or Congenital Anomalies of hard or soft
Covered only when a filling cannot restore the tooth.
pharmacological regimen is the only available treatment tissue, including excision.
CROWNS Limited to 1 time per tooth per consecutive 60 months. Covered only for a particular condition will not result in coverage if the
22. Setting of facial bony fractures and any treatment
when a filling cannot restore the tooth. procedure is considered to be Experimental,
associated with the dislocation of facial skeletal hard
POST AND CORES Covered only for teeth that have had root canal therapy. Investigational or Unproven in the treatment of that
tissue.
SEDATIVE FILLINGS Covered as a separate benefit only if no other service, particular condition.
23. Services related to the temporomandibular joint
other than x-rays and exam, were performed on the same tooth during the visit. 8. Services for injuries or conditions covered by Worker’s (TMJ), either bilateral or unilateral. Upper and lower
SCALING AND ROOT PLANING Limited to 1 time per quadrant per Compensation or employer liability laws, and services jaw bone surgery (including that related to the
consecutive 24 months. that are provided without cost to the covered person temporomandibular joint). No coverage is provided
ROOT CANAL THERAPY Limited to 1 time per tooth per lifetime. by any municipality, county, or other political for orthognathic surgery, jaw alignment, or treatment
PERIODONTAL MAINTENANCE Limited to 2 times per consecutive 12 subdivision. This exclusion does not apply to any for the temporomandibular joint.
months following active or adjunctive periodontal therapy, exclusive of gross services covered by Medicaid or Medicare.
24. Acupuncture; acupressure and other forms of
debridement. 9. Expenses for dental procedures begun prior to the
alternative treatment, whether or not used as
FULL DENTURES Limited to 1 time every consecutive 60 months. No covered person becoming enrolled under the Policy.
anesthesia.
additional allowances for precision or semi-precision attachments. 10. Dental Services otherwise covered under the Policy,
25. Drugs/medications, obtainable with or without a
PARTIAL DENTURES Limited to 1 time every consecutive 60 months. No but rendered after the date individual coverage under
prescription, unless they are dispensed and utilized
additional allowances for precision or semi-precision attachments. the Policy terminates, including Dental Services for
in the dental office during the patient visit.
RELINING AND REBASING DENTURES Limited to relining/rebasing dental conditions arising prior to the date individual
26. Charges for failure to keep a scheduled appointment
performed more than 6 months after the initial insertion. Limited to 1 time per coverage under the Policy terminates.
without giving the dental office 24 hours notice.
consecutive 12 months. 11. Services rendered by a provider with the same legal
27. Occlusal guards used as safety items or to affect
REPAIRS TO FULL DENTURES, PARTIAL DENTURES, BRIDGES residence as a covered person or who is a member of
performance primarily in sports-related activities.
Limited to repairs or adjustments performed more than 12 months after the initial a covered person’s family, including spouse, brother,
28. Dental Services received as a result of war or any act
insertion. Limited to 1 per consecutive 6 months. sister, parent or child.
of war, whether declared or undeclared or caused
PALLIATIVE TREATMENT Covered as a separate benefit only if no other 12. Foreign Services are not covered unless required as
during service in the armed forces of any country.
service, other than the exam and radiographs, were performed on the same tooth an Emergency.
13. Replacement of crowns, bridges, and fixed or
during the visit.
removable prosthetic appliances inserted prior to plan
OCCLUSAL GUARDS Limited to 1 guard every consecutive 36 months and
coverage unless the patient has been covered under
only covered if prescribed to control habitual grinding.
the policy for 12 continuous months. If loss of a tooth
FULL MOUTH DEBRIDEMENT Limited to 1 time every consecutive 36 months.
requires the addition of a clasp, pontic, and/or
GENERAL ANESTHESIA Covered only when clinically necessary.
abutment(s) within this 12 month period, the plan is
OSSEOUS GRAFTS Limited to 1 per quadrant or site per consecutive 36 months.
responsible only for the procedures associated with
PERIODONTAL SURGERY Hard tissue and soft tissue periodontal surgery the addition.
are limited to 1 quadrant or site per consecutive 36 months per surgical area.
14. Replacement of missing natural teeth lost prior to the
REPLACEMENT OF COMPLETE DENTURES, FIXED OR REMOVABLE onset of plan coverage until the patient has been
PARTIAL DENTURES, CROWNS, INLAYS OR ONLAYS Replacement of covered under the Policy for 12 continuous months.
complete dentures, fixed or removable partial dentures, crowns, inlays or onlays 15. Replacement of complete dentures, fixed and removable
previously submitted for payment under the plan is limited to 1 time per partial dentures, or crowns, if damage or breakage was
consecutive 60 months from initial or supplemental placement. This includes directly related to provider error. This type of
retainers, habit appliances, and any fixed or removable interceptive orthodontic replacement is the responsibility of the Dentist. If
appliances. replacement is necessary because of patient
non-compliance, the patient is liable for the cost of
replacement.
16. Fixed or removable prosthodontic restoration
procedures for complete oral rehabilitation or
Plans sold in Texas use associated COC form number: DCOC.CER.06 reconstruction.
You might also like
- Animal Management in Disasters, Volume 2, Animals and CommunitiesFrom EverandAnimal Management in Disasters, Volume 2, Animals and CommunitiesNo ratings yet
- Dental PPO30 - 2017Document2 pagesDental PPO30 - 2017SporkleNo ratings yet
- Covered Services Network Plan Pays Benefit Guidelines Non-Network Plan PaysDocument2 pagesCovered Services Network Plan Pays Benefit Guidelines Non-Network Plan PaysJohnny CallananNo ratings yet
- Dental Plans and Rates: Bay AreaDocument6 pagesDental Plans and Rates: Bay AreaJDanaNo ratings yet
- TeamCare DentalDocument8 pagesTeamCare DentalHector FloydNo ratings yet
- Snap Guardian Dental Plan Summary 2022Document4 pagesSnap Guardian Dental Plan Summary 2022Samson FungNo ratings yet
- 2011 Delta Dental General MarketingDocument1 page2011 Delta Dental General MarketingKristieNo ratings yet
- Disclaimer: Trinet Is The Single-Employer Sponsor of All Its Benefit Plans. This Communication Is For Informational PurposesDocument26 pagesDisclaimer: Trinet Is The Single-Employer Sponsor of All Its Benefit Plans. This Communication Is For Informational PurposesJosh JasperNo ratings yet
- 2017 DgldmetDocument5 pages2017 DgldmetLucas FrançaNo ratings yet
- Everyday Extras: Get The Same Amount Back Each Time You VisitDocument2 pagesEveryday Extras: Get The Same Amount Back Each Time You Visitfrank.wangNo ratings yet
- Generic Open Enrollment KitDocument22 pagesGeneric Open Enrollment KitSteve BarrowsNo ratings yet
- Oak Mountain Dental BrochureDocument2 pagesOak Mountain Dental BrochureErdeli StefaniaNo ratings yet
- Dental BS Delta 1500 PPO Benefit Summary 2018Document4 pagesDental BS Delta 1500 PPO Benefit Summary 2018deepchaitanyaNo ratings yet
- Snic - Payless Tob 2021Document6 pagesSnic - Payless Tob 2021DIVYAS11No ratings yet
- SuperBlue Plus 2000 Plan SummaryDocument4 pagesSuperBlue Plus 2000 Plan Summarymichala anthonyNo ratings yet
- Materials Testing and Consulting Inc 2024 Classic 1000 BsDocument5 pagesMaterials Testing and Consulting Inc 2024 Classic 1000 Bsapi-307235383No ratings yet
- SABH D - BBB Value - Table of BenefitsDocument2 pagesSABH D - BBB Value - Table of BenefitsAkhil VijaiNo ratings yet
- Benefit at A GlanceDocument2 pagesBenefit at A GlanceShiv ChauhanNo ratings yet
- Special Care and Adultbasic: Comparison ChartDocument1 pageSpecial Care and Adultbasic: Comparison ChartjhsmalankaNo ratings yet
- Orient - Table of BenefitsDocument3 pagesOrient - Table of Benefitsd.deustacchioNo ratings yet
- MCI One Pager Version 1.0 Oct 2020Document1 pageMCI One Pager Version 1.0 Oct 2020naval730107No ratings yet
- RES000988105Document10 pagesRES000988105Leonardo MbangataNo ratings yet
- Medgulf Nextcare Rn2 TobDocument4 pagesMedgulf Nextcare Rn2 Tobkcatolico00No ratings yet
- HCF Starter Extras With OpticalDocument3 pagesHCF Starter Extras With OpticalMike LatterNo ratings yet
- QInsurance Factsheet Basic ExtrasDocument1 pageQInsurance Factsheet Basic Extrasjonathan gohNo ratings yet
- 2021 - Life, Dental, Vision PacketDocument12 pages2021 - Life, Dental, Vision PacketEberNo ratings yet
- SuperBlue Plus 2000 Plan Summary Highlights Benefits Deductibles CopaysDocument4 pagesSuperBlue Plus 2000 Plan Summary Highlights Benefits Deductibles CopaysSean MurrayNo ratings yet
- Benefits DetailDocument2 pagesBenefits DetailMJ SkyNo ratings yet
- HCF Mid ExtrasDocument3 pagesHCF Mid Extrasnoneother2No ratings yet
- Gyll Aaron Insurance Verification 1654900113Document2 pagesGyll Aaron Insurance Verification 1654900113Jean Alyssa Mae CalingacionNo ratings yet
- Premier 2000 NWDocument2 pagesPremier 2000 NWacolyteNo ratings yet
- Barclays Dental Plan BenefitsDocument6 pagesBarclays Dental Plan Benefitssaksham23No ratings yet
- Arogya Sanjeevani - One PagerDocument1 pageArogya Sanjeevani - One Pagernaval7301070% (1)
- Arogya Sanjeevani - One PagerDocument1 pageArogya Sanjeevani - One Pagernaval730107No ratings yet
- 2021 GemPlan Summary of BenefitsDocument53 pages2021 GemPlan Summary of BenefitsRaja Churchill DassNo ratings yet
- HCF Lifestyle ExtrasDocument3 pagesHCF Lifestyle ExtrasMintNo ratings yet
- Health QuotationDocument4 pagesHealth QuotationKasturi SankarNo ratings yet
- Vanderbilt phf-21-22Document2 pagesVanderbilt phf-21-22api-458468763No ratings yet
- Regional Victoria's RoadmapDocument12 pagesRegional Victoria's RoadmapTara CosoletoNo ratings yet
- Arogya Sanjeevani Policy ParametersDocument1 pageArogya Sanjeevani Policy Parametersstar health Vadavalli0% (1)
- Arogya - One Pager - Version 1.0 April 2020Document1 pageArogya - One Pager - Version 1.0 April 2020Ari BanerjeeNo ratings yet
- MCS Classicare (MA) Dental Coverage SummaryDocument4 pagesMCS Classicare (MA) Dental Coverage SummaryJessicaNo ratings yet
- Arogya Sanjeevani - One Pager PDFDocument1 pageArogya Sanjeevani - One Pager PDFstar health Vadavalli50% (2)
- Health & Dental Handout JUN17Document2 pagesHealth & Dental Handout JUN17Darius YangNo ratings yet
- Stonewall 0.43% Plus Fertilizer: CautionDocument4 pagesStonewall 0.43% Plus Fertilizer: CautiondthibodeNo ratings yet
- 2020 Schedule of Benefits (SOB) - PPODocument26 pages2020 Schedule of Benefits (SOB) - PPOMonica LeeNo ratings yet
- Kaiser Permanente California Dental Insurance Plan Brochure KPIF 2011Document2 pagesKaiser Permanente California Dental Insurance Plan Brochure KPIF 2011Dennis100% (1)
- Focus On The Extender Option 2017Document9 pagesFocus On The Extender Option 2017mozartatplayNo ratings yet
- Makoti 1 Pager 2021Document2 pagesMakoti 1 Pager 2021TylorNo ratings yet
- US Apple Vision Plan Overview JAN152021 enDocument1 pageUS Apple Vision Plan Overview JAN152021 enCT NguonNo ratings yet
- Anthem Gold Pathway X HMO 1400 SBC SummaryDocument12 pagesAnthem Gold Pathway X HMO 1400 SBC SummaryscheriNo ratings yet
- Your Gsa Student Health & Dental PlanDocument2 pagesYour Gsa Student Health & Dental Planvictor8790No ratings yet
- CisplatinDocument3 pagesCisplatinRicey MelegritoNo ratings yet
- Regence Bronze HSA 5000 Plan DetailsDocument4 pagesRegence Bronze HSA 5000 Plan DetailsVasikaran PrabaharanNo ratings yet
- Tiger Brands Medical Scheme Mzansi Brochure 2020Document16 pagesTiger Brands Medical Scheme Mzansi Brochure 2020ASIVE MLONDLENINo ratings yet
- Asma 101Document43 pagesAsma 101Asfiksia NeonatorumNo ratings yet
- Pesticide Labeling: Ensuring Safe UseDocument24 pagesPesticide Labeling: Ensuring Safe UseJevelyn Mendoza FarroNo ratings yet
- Care Freedom For DiabtiesDocument25 pagesCare Freedom For DiabtiesAgile ServicesNo ratings yet
- Annexure A1-LH23 Malawi ClassicDocument1 pageAnnexure A1-LH23 Malawi Classiccorridor.insuranceNo ratings yet
- Shri Ganesh Insurance Mechanism: Recovery Benefit On Single Hospitalisation More Than 10 DaysDocument4 pagesShri Ganesh Insurance Mechanism: Recovery Benefit On Single Hospitalisation More Than 10 Dayspattani_viral04No ratings yet
- The Changeling: A Monster of the Week PlaybookDocument7 pagesThe Changeling: A Monster of the Week PlaybookSporkle100% (3)
- Curse of Strahd Deathhouse Player MapDocument3 pagesCurse of Strahd Deathhouse Player MapRobert100% (6)
- Janet Female Human BodyguardDocument1 pageJanet Female Human BodyguardSporkleNo ratings yet
- Read Me FirstDocument1 pageRead Me FirstSporkleNo ratings yet
- MA - Notary Public Application 2018Document6 pagesMA - Notary Public Application 2018SporkleNo ratings yet
- Dental PPO20 - 2017Document2 pagesDental PPO20 - 2017SporkleNo ratings yet
- Vision Benefits Summary - 2017Document2 pagesVision Benefits Summary - 2017SporkleNo ratings yet
- Assumption College (CC) Spring 2018 ScheduleDocument3 pagesAssumption College (CC) Spring 2018 ScheduleSporkleNo ratings yet
- Enrollment Application/Change/Cancellation Request For Medical CoverageDocument4 pagesEnrollment Application/Change/Cancellation Request For Medical CoverageSporkleNo ratings yet
- PSP Game File Structure and Audio FilesDocument5 pagesPSP Game File Structure and Audio FilesSporkleNo ratings yet
- READMEDocument3 pagesREADMESporkleNo ratings yet
- Enrollment Application/Change/Cancellation Request For Medical CoverageDocument4 pagesEnrollment Application/Change/Cancellation Request For Medical CoverageSporkleNo ratings yet
- Presentation OutlineDocument1 pagePresentation OutlineSporkleNo ratings yet
- Pet AgreementDocument2 pagesPet AgreementSporkleNo ratings yet
- Death by DesignDocument56 pagesDeath by DesignSporkle100% (3)
- Neha 2020 TendinteDocument16 pagesNeha 2020 TendinteIrina BesliuNo ratings yet
- NobelReplace Tapered Sales Brochure GB Tcm61-19282Document28 pagesNobelReplace Tapered Sales Brochure GB Tcm61-19282Ana Sofia RodriguezNo ratings yet
- 2017 Laleman - Guided Implant Surgery in The Edentulous Maxilla - A Systematic ReviewDocument15 pages2017 Laleman - Guided Implant Surgery in The Edentulous Maxilla - A Systematic ReviewFabio FabrettiNo ratings yet
- Implant Prosthetics: With Bionic High-Performance PolymersDocument12 pagesImplant Prosthetics: With Bionic High-Performance PolymersLucian Catalin CalinNo ratings yet
- Periodontal Prosthesis in Contemporary Dentistry: SciencedirectDocument8 pagesPeriodontal Prosthesis in Contemporary Dentistry: SciencedirectJuan Carlos Montañez BenavidesNo ratings yet
- Jörg A. Auer Craniomaxillofacial Disorders (Equine Surgery (Fourth Edition) )Document27 pagesJörg A. Auer Craniomaxillofacial Disorders (Equine Surgery (Fourth Edition) )Ana Carolina MartinsNo ratings yet
- Precision AttachmentsDocument10 pagesPrecision Attachmentsdentist40No ratings yet
- Basic Implant Surgery: Dental ImplantsDocument7 pagesBasic Implant Surgery: Dental ImplantsHau TranNo ratings yet
- Retention of Locator and Resilient Telescopic Attachment For Implant Retenied Mandibular Overdentures. An Invitro StudyDocument8 pagesRetention of Locator and Resilient Telescopic Attachment For Implant Retenied Mandibular Overdentures. An Invitro StudyDr FarhatNo ratings yet
- Advanced AM HandbookDocument290 pagesAdvanced AM HandbookBikash ChoudhuriNo ratings yet
- Review Cirugía Preprotésica. ArtículoDocument9 pagesReview Cirugía Preprotésica. ArtículoAnita Estela Batz MatulNo ratings yet
- BPS+ +the+Biofunctional+Prosthetic+SystemDocument20 pagesBPS+ +the+Biofunctional+Prosthetic+SystemPravin Prathip JNo ratings yet
- Burkhardt 2015Document12 pagesBurkhardt 2015Posgrado Periodoncia2017No ratings yet
- Use of Polyethylene Ribbon To Create A Provisional Fixed Partial DentureDocument4 pagesUse of Polyethylene Ribbon To Create A Provisional Fixed Partial DentureAhmed AbdulazeezNo ratings yet
- Prama implant system catalogueDocument104 pagesPrama implant system catalogueGheorgheNo ratings yet
- How To Read CBCTDocument17 pagesHow To Read CBCTRazvan UngureanuNo ratings yet
- "Sticky Bone" Use in Implant Dentistry: Zirconia Full Arch Implant RestorationDocument64 pages"Sticky Bone" Use in Implant Dentistry: Zirconia Full Arch Implant RestorationJuan David Torres CanoNo ratings yet
- Risks and Complications of Orthodontic MiniscrewsDocument51 pagesRisks and Complications of Orthodontic MiniscrewsutokaNo ratings yet
- Terraform Delta: A Novel by W C Vetsch All Rights ReservedDocument25 pagesTerraform Delta: A Novel by W C Vetsch All Rights ReservedW C VETSCH100% (2)
- Seminar 13Document60 pagesSeminar 13radhikamiNo ratings yet
- Diagnosis and Treatment Planning in ImplantsDocument26 pagesDiagnosis and Treatment Planning in ImplantsGayathri Gangadharan100% (3)
- Digital Wax Up in DentistryDocument14 pagesDigital Wax Up in Dentistrybanea costin100% (1)
- فحص جراحة 11Document144 pagesفحص جراحة 11Ola AlaaNo ratings yet
- Prof. Dr. David Buntoro Drg. MDS. SP-BMKDocument30 pagesProf. Dr. David Buntoro Drg. MDS. SP-BMKDipdha Arum SangoraNo ratings yet
- The Vertical Dimension in Prosthesis and Orthognathodontics PDFDocument380 pagesThe Vertical Dimension in Prosthesis and Orthognathodontics PDFPatri Meisaros100% (1)
- Rehabilitation of Hemimandibulectomy PatientDocument3 pagesRehabilitation of Hemimandibulectomy PatientAB MISHRANo ratings yet
- The Trimeric Model: A New Model of Periodontal Treatment PlanningDocument5 pagesThe Trimeric Model: A New Model of Periodontal Treatment PlanningNz BebekNo ratings yet
- Artículo Alloys For Prosthodontic RestorationsDocument13 pagesArtículo Alloys For Prosthodontic RestorationsCelia LizarazoNo ratings yet
- Clinical Oral Implants Res - 2023 - Schwarz - Effectiveness of Modified and Control Protocols For The Surgical Therapy ofDocument27 pagesClinical Oral Implants Res - 2023 - Schwarz - Effectiveness of Modified and Control Protocols For The Surgical Therapy ofIsaac MoNo ratings yet
- Unit 1 - Dental SpecialtiesDocument36 pagesUnit 1 - Dental SpecialtiesCapalb AlbertNo ratings yet