Professional Documents
Culture Documents
Gotlib. Neuroimaging and Depression
Uploaded by
mariobar17636Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Gotlib. Neuroimaging and Depression
Uploaded by
mariobar17636Copyright:
Available Formats
CU R RE N T D I R E CT I O NS IN P SYC H OL OG I C AL SC I EN C E
Neuroimaging and Depression
Current Status and Unresolved Issues
Ian H. Gotlib and J. Paul Hamilton
Stanford University
ABSTRACT—Major depression is among the most debilitat- Over the past 15 years, investigators have used neuroimaging
ing, prevalent, and recurrent of all psychiatric disorders. techniques to examine the neural substrates of depression. In
Over the past decade, investigators have examined the this review, we briefly summarize findings from this work, em-
neural mechanisms associated with this disorder. In this phasizing key regions of the brain that have been implicated
article we present an overview of neuroimaging research in MDD. We then discuss these findings in the context of an
that has assessed the structure and functioning of the integrative formulation of the neural substrates of depression.
amygdala, subgenual anterior cingulate cortex, and dorso- We conclude by highlighting important unresolved issues in this
lateral prefrontal cortex in major depression. We then field and by suggesting directions for future research that will
describe results of studies that have attempted to elucidate help to add specificity and breadth to neural models of depres-
the nature of the relations among these brain structures. sion.
The picture that emerges from these investigations is one
in which heightened activity in limbic structures that un- DEPRESSION AND THE BRAIN
derlie the experience and expression of emotion dampens
activation in dorsal cortical structures that are involved in Even before the advent of structural and functional neuro-
affect regulation, reducing their ability to influence limbic imaging research on MDD, there were strong indications that
activation. We conclude by highlighting unresolved issues neural abnormalities play a crucial role in depression. Foremost
concerning the roles of these structures in depression and among these is the fact that depressive disorders are responsive
their relation to specific symptoms of this disorder. to a diverse set of brain-based interventions. In addition to
KEYWORDS—depression; neuroimaging; fMRI; amygdala; showing positive outcome following drug treatment, for example,
ACC; DLPFC a significant subset of depressed individuals also respond
favorably to electroconvulsive therapy, in which seizure-in-
ducing current is applied to the temples, as well as to surgeries
Major Depressive Disorder (MDD) is among the most prevalent that sever neural fiber tracts or destroy brain regions that are
of all psychiatric disorders. MDD is characterized by sad mood postulated to be involved in the maintenance of depression.
and/or a loss of interest or pleasure in almost all daily activities, The specific symptoms that make up the syndrome of MDD
as well as by several associated symptoms such as weight loss also implicate the functioning of particular brain structures.
or gain, sleep disturbance, psychomotor agitation or retardation, Depression is primarily a disorder of emotion and its regulation;
fatigue, and concentration difficulties. Depression is both indeed, hallmark symptoms of depression are pervasive sad
widespread, with up to 20% of the general population experi- mood and an inability to inhibit the processing of negative in-
encing at least one episode of depression during their lifetime, formation, exacerbating the experience of negative affect. Over
and recurrent, with a relapse rate of over 80%. This high prev- the past decade, neuroscientists examining the ‘‘emotion cir-
alence and recurrence of depression, combined with its sig- cuitry’’ of the brain have documented the involvement of the
nificant personal and societal costs, makes it imperative that we limbic system, a complex of structures including the amygdala,
identify and elucidate factors that are involved in the onset and hippocampus, insula, and parts of the anterior cingulate cortex
maintenance of MDD and in recovery from this disorder. (ACC), in the experience and expression of emotional states (see
Davidson et al., 2002, for a review). Among these structures, the
amygdala and the ventral (i.e., bottom) aspect of the ACC, most
often referred to as the subgenual ACC, have received the most
Address correspondence to Ian H. Gotlib, Department of Psychology,
Bldg. 420, Jordan Hall, Stanford University, Stanford, CA 94305; attention from investigators interested in depression. Whereas
e-mail: ian.gotlib@stanford.edu. the amygdala has been shown to play a prominent role in
Volume 17—Number 2 Copyright r 2008 Association for Psychological Science 159
Neuroimaging and Depression
emotionally mediated attention, in assigning emotional signifi- finding of a decrease in subgenual ACC metabolism following
cance to stimuli, and in remembering emotionally significant the administration of fenfluramine—an agonist of serotonin with
events (see Phelps, 2008, this issue), the subgenual ACC ap- antidepressant effects—to depressed individuals. Kegeles et al.
pears to mediate subjective experience of emotion and emotional also found the magnitude of the metabolic subgenual ACC de-
reactions to stimuli, particularly stimuli associated with reward crease to be positively correlated with alleviation of depressive
seeking. These two structures are involved directly in the ex- symptoms. Consistent with the results of these studies, Gotlib
perience and processing of emotion, but investigators have also et al. (2005) found depressed individuals to exhibit greater
examined cortical structures, most notably the dorsolateral subgenual ACC activation than did controls in response to
prefrontal cortex (DLPFC), that appear to be involved in the emotional faces. Moreover, Siegle, Carter, and Thase (2006)
regulation of emotion in depression and in cognitive control. showed that those depressed persons who eventually improve
In the sections below, we briefly summarize empirical work with cognitive-behavior therapy have less subgenual ACC re-
examining the amygdala, subgenual ACC, and DLPFC in activity to affective words than do depressed individuals who do
depressed individuals. not improve.
AMYGDALA DLPFC
Studies of amygdala volume in depression have yielded incon- Given the high levels of rumination in depression that may
sistent findings. We recently conducted a meta-analysis of these reflect difficulties in cognitive control, investigators have
studies and found no aggregate difference in amygdala volume hypothesized that depression is characterized by low levels of
between depressed and healthy individuals. We did find, how- activity in the DLPFC (e.g., Mayberg et al., 1999). Indeed,
ever, that amygdala volume decreases significantly with in- although there is little evidence of structural anomalies in the
creasing number of depressive episodes; depression history, DLPFC in depression, remarkably consistent findings regarding
therefore, may be an important variable to consider in future abnormalities of function in this region have been reported.
neuroimaging studies. Studies using positron emission tomog- Several investigators have reported lower resting-state DLPFC
raphy (PET) to examine neural activity have found elevated activity in depressed than in healthy individuals (e.g., Gonul,
baseline amygdala activity in depression that is positively cor- Kula, Bilgin, Tutus, & Oguz, 2004; Mayberg et al., 2005).
related with depressive severity (e.g., Drevets, Bogers, & Studies examining the neural bases of induced depressive re-
Raichle, 2002). In addition to being characterized by elevated lapse through depletion of tryptophan—an amino acid that is a
baseline amygdalar activity, depressed persons have also been necessary precursor to serotonin—have reported that individ-
found to exhibit greater amygdala reactivity to emotional stimuli, uals who relapse have lower DLPFC activity during relapse than
particularly negatively valenced stimuli, than do controls (e.g., do individuals who do not relapse (Bremner et al., 1997). Con-
Fales et al., in press; Sheline et al., 2001). Although some in- sistent with these findings, researchers have found depressed
vestigators have also found abnormal amygdala responsivity to individuals to exhibit less DLPFC reactivity to affective stimuli
positively valenced stimuli in depressed individuals, these ef- than do healthy controls. Hooley, Gruber, Scott, Hiller, and
fects are found infrequently and are less consistent in their di- Yurgelun-Todd (2005), for example, showed that, unlike their
rection, with one study showing increased amygdala response non-disordered counterparts, depressed individuals failed to
to happy faces (Sheline et al., 2001) and another reporting activate the DLPFC while listening to taped criticism from their
decreased amygdala reactivity to positive words (Canli et al., mothers. Schaefer, Putnam, Benca, and Davidson (2006) ex-
2004). tended these findings to positive affect, reporting diminished
reactivity of the DLPFC in depressed participants in response to
SUBGENUAL ACC both erotica and positive emotion faces.
A small number of studies have reported decreased volume in CONCLUSIONS, UNRESOLVED ISSUES, AND FUTURE
the subgenual ACC associated with depression (e.g., Drevets DIRECTIONS
et al., 1997). Investigators examining resting state activity in the
subgenual ACC of depressed individuals have found decreased This brief review has shown that, perhaps not surprisingly, there
activity in this region (e.g., Drevets et al., 2002; Drevets et al., are functional abnormalities of neural structures implicated in
1997). Interestingly, Drevets (1999) presented a simulation that the experience, expression, and regulation of emotion in de-
adjusted estimates of activity in the subgenual ACC to com- pression; most consistently, the amygdala and subgenual ACC
pensate for the volume loss in this structure associated with appear to be overactive in MDD, and the DLPFC underactive.
depression and found that the volume-adjusted activity esti- Given the patterns of anatomical connectivity among these
mates indicated increased subgenual ACC activity in this dis- structures, it is unlikely that they are expressing abnormality
order. This formulation is consistent with Kegeles et al.’s (2003) independently of one another. A challenge for future work,
160 Volume 17—Number 2
Ian H. Gotlib and J. Paul Hamilton
therefore, is to identify the patterns of functional connectivity cortical and subcortical structures that is proposed to mediate
that characterize the depressive neural network. Investigators internally generated thought processes, extends to include the
working from a neural systems perspective have begun to ex- subgenual ACC in depression. Moreover, in our laboratory we
amine functional connectivity in depression. Mayberg et al. are finding that when depressed individuals successfully encode
(2005), for example, assessed the neural consequences of negative information, there is increased correlation, relative to
modulating activity in the subgenual ACC by implanting and that found in never-depressed participants, between activity in
activating stimulating electrodes near this structure (deep brain the amygdala and activity in the hippocampus, a structure that
stimulation) in depressed patients who were unresponsive to is vital in the encoding of information. This amygdala–hippo-
conventional forms of therapy. They found, in addition to marked campus synchrony appears to facilitate memory for negative
clinical improvement in several patients, that stimulation near material; indeed, the degree of synchrony predicts individual
the subgenual ACC in such patients attenuated the pre-existing differences in subsequent memory for negative, but not positive
overactivity in this structure and resulted in increased activity or neutral, material in depressed individuals. Further research
in the previously underactive DLPFC. This reciprocal relation is needed both to continue to delineate patterns of functional
between dorsally situated cortical structures and limbic struc- connectivity among neural structures in depression and to begin
tures in depression has also been documented in functional to map the anatomical foundations of those patterns using
neuroimaging studies. Siegle, Steinhauer, Thase, Stenger, and techniques like diffusion tensor imaging that make it possible to
Carter (2002), for example, found an inverse relation between detect and assess the integrity of pathways connecting brain
amygdala and DLPFC activation in depressed individuals in structures.
response to affective words. Another critical task for future research is to elucidate the
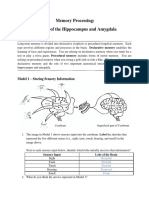
This pattern of activity is consistent with a neural model de- roles played by functional and structural anomalies in the onset
veloped by Helen Mayberg, who proposed that the normal re- and maintenance of depression and in recovery from this dis-
ciprocal relation between the limbic system and dorsal cortical order. Although the research we have described above indicates
structures is imbalanced, or skewed, in depression. Mayberg that the amygdala, subgenual ACC, and DLPFC are functionally
essentially describes a vicious circle in which hyperactivation in and, in some cases, structurally aberrant in depression, we know
limbic structures like the subgenual ACC and amygdala relatively little about how these anomalies are related to MDD.
dampens activation in dorsal structures, reducing the ability of In beginning to examine this question, researchers have
the latter to regulate limbic activation (see Fig. 1 for a simple assessed temporal relations between neural activity and symp-
schematic of this model). It is also important to note, however, toms of depression, examining whether neural abnormalities are
that recent work suggests that network abnormalities in de- present after symptomatic improvement, whether they precede
pression are not limited to interactions between the limbic the onset of depression, and whether they are associated with the
system and dorsal cortical structures. For example, Greicius subsequent course of depression. For example, the increased
et al. (2007) found that the ‘‘default mode network,’’ a complex of activity in the amygdala and subgenual ACC and the decreased
activity in the DLPFC that is present during the depressive
episode appears to normalize following successful treatment
(e.g., Drevets et al., 2002; Mayberg et al., 1999; Mayberg et al.,
2005; Schaefer et al., 2006); suggesting that functional distur-
bances in these structures are simply correlates of a depressive
episode. Two recent findings from our laboratory raise questions
Dorsal about this conclusion, however. First, studying a sample of re-
Cortex mitted depressed individuals in an induced sad mood, we found
that elevated amygdala activation during encoding predicts in-
creased recall of negative self-referent words (Ramel et al.,
2007). Second, young girls at elevated risk for depression
Limbic System because of a family history of the disorder but who have not
themselves had a depressive episode exhibit pronounced
amygdala activation when experiencing induced sadness and
when attempting to regulate that sadness (see Fig. 2). These
findings indicate that, in individuals who are vulnerable to de-
veloping depression, sad mood may provide the context for the
Fig. 1. Schematic of a neural model of depression emphasizing the dom- increased amygdala activation that has been found to charac-
inance of limbic activity in the reciprocal relation between the dorsal terize depressive episodes.
cortex, which includes the dorsolateral prefrontal cortex (DLPFC); and
the limbic system, which includes the amygdala, hippocampus, insula, and In interpreting the results of such studies, however, it is im-
parts of the anterior cingulate cortex (ACC). portant to recognize that elucidating the timing of neural
Volume 17—Number 2 161
Neuroimaging and Depression
Fig. 2. Amygdala activation during the experience of sad mood in young girls at high risk (left) and low risk
(right) of developing depression.
abnormalities in depression does not necessarily illuminate Recommended Reading
their role in the disorder. That is, anomalies can be present in a Davidson, R.J., Pizzagalli, D., Nitschke, J.B., & Putnam, K.M. (2002).
disordered state (and, indeed, may precede the onset of a dis- Depression: Perspectives from affective neuroscience. Annual
Review of Psychology, 53, 545–574. A review describing basic
order) without being involved in its development. Parsing this
research on the neural circuitry underlying affect and discussing
literature, therefore, is going to be a difficult endeavor. Adding to the dysfunction of this circuitry in depression.
this complexity are studies reporting seemingly contradictory Drevets, W.C., Price, J.L., Simpson, J.R., Todd, R.D., Reich, T., Vannier,
findings. For example whereas greater amygdala reactivity to M., et al. (1997). (See References). A seminal work on the affective
affective stimuli during a depressive episode has been found to neuroscience of depression, showing this disorder to be associated
predict a subsequent decrease in symptoms (e.g., Canli et al., with structural and functional abnormalities in the subgenual
ACC.
2005), symptomatic improvement in depression has also been
Gotlib, I.H., & Hammen, C.L. (2002). Handbook of depression. New York:
found following deactivation of the subgenual ACC both with Guilford Press. A handbook presenting a comprehensive review of
deep brain stimulation (Mayberg et al., (2005) and, in our lab- research and theory in depression, including its characterization,
oratory, through neurofeedback (i.e., presenting real-time visual trajectory, biological and cognitive bases, and treatment.
feedback in the scanner to modulate ACC activity). It may be, Pizzagalli, D.A., Oakes, T.R., Fox, A.S., Chung, M.K., Larson, C.L.,
therefore, that although the amygdala and subgenual ACC have Abercrombie, H.C., et al. (2004). Functional but not structural
both been found to be more active in depressed than in nonde- subgenual prefrontal cortex abnormalities in melancholia. Mo-
lecular Psychiatry, 9, 393–405. An article describing a multimodal
pressed participants, they have different temporal relations with assessment of the role of subgenual ACC abnormality in melan-
the expression of depressive symptoms. cholic depression.
These results concerning the temporal relation between Sheline, Y.I. (2003). Neuroimaging studies of mood disorder effects on
neural activation and depression and the role of neural dys- the brain. Biological Psychiatry, 54, 338–352. A review presenting
function in depression are complex and do not cohere to tell as evidence from structural neuroimaging studies that abnormalities
clear a story as we would like. Above all, they underscore the fact in a neural circuit, the limbic-cortical-striatal-pallidal-thalamic
tract, is associated with depression.
that ‘‘depression’’ refers to a heterogeneous group of disorders
that are not carved at their neurobiological joints in the DSM-IV.
Perhaps the most pressing task for future research, therefore, is
to begin more explicitly to conceptualize depression subtypes Acknowledgments—Writing of this article was supported by
and symptom profiles that are related systematically to specific Grants MH59259 and MH074849 from the National Institute of
neural functional and structural abnormalities, and to explore Mental Health, awarded to Ian H. Gotlib.
more precisely how these neural abnormalities are related to the
behavioral, cognitive, and affective symptoms of depression. We REFERENCES
believe it is only through such an effort that significant progress
can be made in elucidating and understanding neural aspects of Bremner, J.D., Innis, R.B., Salomon, R.M., Staib, L.H., Ng, C.K., Miller,
depressive disorders. H.L., et al. (1997). Positron emission tomography measurement of
162 Volume 17—Number 2
Ian H. Gotlib and J. Paul Hamilton
cerebral metabolic correlates of tryptophan depletion-induced Hooley, J.M., Gruber, S.A., Scott, L.A., Hiller, J.B., & Yurgelun-Todd,
depressive relapse. Archives of General Psychiatry, 54, 364–374. D.A. (2005). Activation in dorsolateral prefrontal cortex in re-
Canli, T., Cooney, R.E., Goldin, P., Shah, M., Sivers, H., Thomason, sponse to maternal criticism and praise in recovered depressed
M.E., et al. (2005). Amygdala reactivity to emotional faces and healthy control participants. Biological Psychiatry, 57, 809–
predicts improvement in major depression. Neuroreport, 16, 1267– 812.
1270. Kegeles, L.S., Malone, K.M., Slifstein, M., Ellis, S.P., Xanthopoulos, E.,
Canli, T., Sivers, H., Thomason, M.E., Whitfield-Gabrieli, S., Gabrieli, Keilp, J.G., et al. (2003). Response of cortical metabolic deficits to
J.D.E., & Gotlib, I.H. (2004). Brain activation to emotional serotonergic challenge in familial mood disorders. American
words in depressed vs. healthy subjects. Neuroreport, 15, 2585– Journal of Psychiatry, 160, 76–82.
2588. Mayberg, H.S., Liotti, M., Brannan, S.K., McGinnis, S., Mahurin, R.K.,
Davidson, R.J., Lewis, D.A., Alloy, L.B., Amaral, D.G., Bush, G., Co- Jerabek, P.A., et al. (1999). Reciprocal limbic-cortical function
hen, J.D., et al. (2002). Neural and Behavioral substrates of mood and negative mood: Converging PET findings in depression and
and mood regulation. Biological Psychiatry, 52, 478–502. normal sadness. American Journal of Psychiatry, 156, 675–682.
Drevets, W.C. (1999). Prefrontal cortical-amygdalar metabolism in Mayberg, H.S., Lozano, A.M., Voon, V., McNeely, H.E., Seminowicz, D.,
major depression. Annals of the New York Academy of Sciences, Hamani, C., et al. (2005). Deep brain stimulation for treatment-
877, 614–637. resistant depression. Neuron, 45, 651–660.
Drevets, W.C., Bogers, W., & Raichle, M.E. (2002). Functional ana- Phelps, E.A., & Sharot, T. (2008). How (and why) emotion enhances the
tomical correlates of antidepressant drug treatment assessed using subjective sense of recollection. Current Directions in Psycho-
PET measures of regional glucose metabolism. European Neuro- logical Science, 17, 147–152.
psychopharmacology, 12, 527–544. Ramel, W., Goldin, P.R., Eyler, L.T., Brown, G.G., Gotlib, I.H., &
Drevets, W.C., Price, J.L., Simpson, J.R., Todd, R.D., Reich, T., Vannier, McQuaid, J.R. (2007). Amygdala reactivity and mood-congruent
M., et al. (1997). Subgenual prefrontal cortex abnormalities in memory in individuals at risk for depressive relapse. Biological
mood disorders. Nature, 386, 824–827. Psychiatry, 61, 231–239.
Fales, C.L., Barch, D.M., Rundle, M.M., Mintun, M.A., Snyder, A.Z., Schaefer, H.S., Putnam, K.M., Benca, R.M., & Davidson, R.J. (2006).
Cohen, J.D., et al. (in press). Altered emotional interference pro- Event-related functional magnetic resonance imaging measures of
cessing in affective and cognitive-control brain circuitry in major neural activity to positive social stimuli in pre- and post-treatment
depression. Biological Psychiatry. depression. Biological Psychiatry, 60, 974–986.
Gonul, A.S., Kula, M., Bilgin, A.G., Tutus, A., & Oguz, A. (2004). The Sheline, Y.I., Barch, D.M., Donnelly, J.M., Ollinger, J.M., Snyder, A.Z.,
regional cerebral blood flow changes in major depressive disorder & Mintun, M.A. (2001). Increased amygdala response to masked
with and without psychotic features. Progress in Neuro-Psycho- emotional faces in depressed subjects resolves with antidepres-
pharmacology & Biological Psychiatry, 28, 1015–1021. sant treatment: An fMRI study. Biological Psychiatry, 50, 651–
Gotlib, I.H., Sivers, H., Gabrieli, J.D.E., Whitfield-Gabrieli, S., Goldin, 658.
P., Minor, K.L., et al. (2005). Subgenual anterior cingulate acti- Siegle, G.J., Carter, C.S., & Thase, M.E. (2006). Use of fMRI to predict
vation to valenced emotional stimuli in major depression. Neuro- recovery from unipolar depression with cognitive behavior thera-
report, 16, 1731–1734. py. American Journal of Psychiatry, 163, 735–738.
Greicius, M.D., Flores, B.H., Menon, V., Glover, G.H., Solvason, H.B., Siegle, G.J., Steinhauer, S.R., Thase, M.E., Stenger, V.A., & Carter, C.S.
Kenna, H., et al. (2007). Resting-state functional connectivity in (2002). Can’t shake that feeling: Assessment of sustained event-
major depression: Abnormally increased contributions from sub- related fMRI amygdala activity in response to emotional infor-
genual cingulate cortex and thalamus. Biological Psychiatry, 62, mation in depressed individuals. Biological Psychiatry, 51, 693–
429–437. 707.
Volume 17—Number 2 163
You might also like
- Alex Korb - Daniel J. Siegel - The Upward Spiral - Using Neuroscience To Reverse The Course of DepressionDocument241 pagesAlex Korb - Daniel J. Siegel - The Upward Spiral - Using Neuroscience To Reverse The Course of Depressionsiralk100% (14)
- Amygdala and HippocampusDocument8 pagesAmygdala and Hippocampusapi-400575655100% (1)
- Comfort - Nursing Test QuestionsDocument57 pagesComfort - Nursing Test QuestionsRNStudent1100% (1)
- Listening To Scent - An Olfactor - Jennifer Peace RhindDocument183 pagesListening To Scent - An Olfactor - Jennifer Peace RhindSamuche Huang100% (1)
- A Glossary: of Key Brain Science TermsDocument24 pagesA Glossary: of Key Brain Science TermscadulemosNo ratings yet
- 294 Lab ReportDocument10 pages294 Lab ReportDhanush Mahendran100% (1)
- Emotional Activation SystemDocument4 pagesEmotional Activation Systemwereck80100% (1)
- Abnormal Psychology Canadian 1st Edition Beidel Test BankDocument35 pagesAbnormal Psychology Canadian 1st Edition Beidel Test Bankdyestuffdynasticybwc89100% (16)
- Scopa Cog enDocument6 pagesScopa Cog endquebradasNo ratings yet
- Neural Circuits Underlying The Pathophysiology of Mood DisordersDocument11 pagesNeural Circuits Underlying The Pathophysiology of Mood Disordersrocambolescas perthNo ratings yet
- Mindfulness y Sintomatologia DepresivaDocument26 pagesMindfulness y Sintomatologia DepresivaOlivia EmporioNo ratings yet
- Is Major Depression A Cognitive Disorder?: SciencedirectDocument4 pagesIs Major Depression A Cognitive Disorder?: Sciencedirectmahmoud fuqahaNo ratings yet
- 2005 Eriv J. Nestler The Mesolimbic Dopamine Reward Circuit in DepressionDocument9 pages2005 Eriv J. Nestler The Mesolimbic Dopamine Reward Circuit in Depressionadni halianieNo ratings yet
- Amygdala Volume DepressionDocument13 pagesAmygdala Volume DepressionEllenaNo ratings yet
- Inhibicion Cognitiva en Depresion 2007Document12 pagesInhibicion Cognitiva en Depresion 2007Rene GallardoNo ratings yet
- The Significance of Artistic Creativity On Treatment of DepressionDocument5 pagesThe Significance of Artistic Creativity On Treatment of Depressionchristian-arcayos-2035No ratings yet
- Biology 12 01399Document20 pagesBiology 12 01399fathul muinNo ratings yet
- Functional Neuroanatomy of Bipolar Disorder: Structure, Function, and Connectivity in An Amygdala-Anterior Paralimbic Neural SystemDocument16 pagesFunctional Neuroanatomy of Bipolar Disorder: Structure, Function, and Connectivity in An Amygdala-Anterior Paralimbic Neural SystemLin FernándezNo ratings yet
- He Cholinergic System and Depression: Dagytė G, Den Boer JA, Trentani ADocument16 pagesHe Cholinergic System and Depression: Dagytė G, Den Boer JA, Trentani AMaharaniDewiNo ratings yet
- Executive Dysfunction in Geriatric DepressionDocument8 pagesExecutive Dysfunction in Geriatric DepressiondiegomaximilianoherreraNo ratings yet
- Research PaperDocument11 pagesResearch PaperRamjan KhandelwalNo ratings yet
- Depression: Brigitta BondyDocument8 pagesDepression: Brigitta BondyLiaNo ratings yet
- DepressionDocument26 pagesDepressionkanwalsweetNo ratings yet
- Depression, Hippocampal Volume Changes, and Cognitive Decline in A Clinical Sample of Older Depressed Outpatients and Non-Depressed ControlsDocument11 pagesDepression, Hippocampal Volume Changes, and Cognitive Decline in A Clinical Sample of Older Depressed Outpatients and Non-Depressed ControlsMiguelySusy Ramos-RojasNo ratings yet
- Literature Review 1Document7 pagesLiterature Review 1api-549444062No ratings yet
- Emotional Dysfunction As A Marker of Bipolar DisordersDocument8 pagesEmotional Dysfunction As A Marker of Bipolar DisordersFrancisca VargasNo ratings yet
- NST 151Document13 pagesNST 151JoeNo ratings yet
- TMP E2 FBDocument9 pagesTMP E2 FBFrontiersNo ratings yet
- 1 s2.0 S0278584623000027 Main PDFDocument10 pages1 s2.0 S0278584623000027 Main PDFPeng WangNo ratings yet
- McTeague, Et Al - Common Neural Circuit Disruptions in Emotional Processing Disorders (2019)Document11 pagesMcTeague, Et Al - Common Neural Circuit Disruptions in Emotional Processing Disorders (2019)Ricardo EscNo ratings yet
- Eurobiology of Depression: 01.11.13 Laura BohleberDocument58 pagesEurobiology of Depression: 01.11.13 Laura BohlebernerissaNo ratings yet
- Implicación Del Lóbulo Frontal en La Depresión Mayor Senil: M.J. Portella, T. MarcosDocument4 pagesImplicación Del Lóbulo Frontal en La Depresión Mayor Senil: M.J. Portella, T. MarcosAlexis ChaflaNo ratings yet
- NIH Public AccessDocument14 pagesNIH Public AccessjuanNo ratings yet
- Hayley Frontiers NeuroDocument18 pagesHayley Frontiers NeuroShawn HayleyNo ratings yet
- 1 s2.0 S0022395622000309 MainDocument10 pages1 s2.0 S0022395622000309 MainRaquel PintoNo ratings yet
- LeMoult & Gotlib - 2019 - Depression A Cognitive PerspectiveDocument16 pagesLeMoult & Gotlib - 2019 - Depression A Cognitive PerspectivePaloma GonzálezNo ratings yet
- Beblo, Sinnamon & Baune - Specifying The Neuropsychology of Affective Disorders - Neuropsychology Reviews - 2011Document23 pagesBeblo, Sinnamon & Baune - Specifying The Neuropsychology of Affective Disorders - Neuropsychology Reviews - 2011Roberta Finamore de AraujoNo ratings yet
- Appi Focus 20160036Document7 pagesAppi Focus 20160036Dewi NofiantiNo ratings yet
- Psychopathology Notes 5Document4 pagesPsychopathology Notes 5Holly Hu JenkinsonNo ratings yet
- Stress, Depression and Neuroplasticity: Shatrunjai P. Singh and Swagata KarkareDocument6 pagesStress, Depression and Neuroplasticity: Shatrunjai P. Singh and Swagata KarkareJoeNo ratings yet
- tmp656D TMPDocument40 pagestmp656D TMPFrontiersNo ratings yet
- Mejora de La Función Ejecutiva Tras Remisión de La Depresión Unipolar Recurrente.Document8 pagesMejora de La Función Ejecutiva Tras Remisión de La Depresión Unipolar Recurrente.Miguel Ángel DominguezNo ratings yet
- 2010 Goh Vulnera - EngDocument5 pages2010 Goh Vulnera - EngFernandoCedroNo ratings yet
- DNB 22 2 J PDFDocument5 pagesDNB 22 2 J PDFFlorinaNo ratings yet
- Mather2012 - ParadoxDocument17 pagesMather2012 - ParadoxMariana PestanaNo ratings yet
- Buhle Et Al 2014 CerebCortex Cognitive ReappraDocument10 pagesBuhle Et Al 2014 CerebCortex Cognitive Reappra童帅No ratings yet
- Pittenger 2007Document22 pagesPittenger 2007rocambolescas perthNo ratings yet
- Neuroimage: Clinical: SciencedirectDocument9 pagesNeuroimage: Clinical: SciencedirectMostafa FakhriNo ratings yet
- Beauregard Paquette2006Document4 pagesBeauregard Paquette2006felix pastorNo ratings yet
- Experience Effects On Brain Development Possible Contributions To PsychopathologyDocument31 pagesExperience Effects On Brain Development Possible Contributions To PsychopathologyShirleuy GonçalvesNo ratings yet
- Pharmacology, Biochemistry and BehaviorDocument11 pagesPharmacology, Biochemistry and BehaviorRevis BlackNo ratings yet
- Zilver Stand 2016Document38 pagesZilver Stand 2016童帅No ratings yet
- Emotional Processing in Functional Neurological Disorder: A Review, Biopsychosocial Model and Research AgendaDocument8 pagesEmotional Processing in Functional Neurological Disorder: A Review, Biopsychosocial Model and Research AgendaManuel Guerrero GómezNo ratings yet
- Brain and Cognition: Anna Weinberg, E. David Klonsky, Greg HajcakDocument8 pagesBrain and Cognition: Anna Weinberg, E. David Klonsky, Greg HajcakGheorghe SecuNo ratings yet
- Brain and Cognition: Anna Weinberg, E. David Klonsky, Greg HajcakDocument8 pagesBrain and Cognition: Anna Weinberg, E. David Klonsky, Greg HajcakGheorghe SecuNo ratings yet
- Schaefer, S., Jackson, D., Davidson, R. Et Al. (2002) - Modulation of Amygdalar Activity by The Conscious Regulation of Negative Emotion PDFDocument9 pagesSchaefer, S., Jackson, D., Davidson, R. Et Al. (2002) - Modulation of Amygdalar Activity by The Conscious Regulation of Negative Emotion PDFJuan Camilo SotoNo ratings yet
- Mcrae 2010Document15 pagesMcrae 2010童帅No ratings yet
- ProjectDocument16 pagesProjectshahriar firouzabadiNo ratings yet
- Emotion Perception 2Document14 pagesEmotion Perception 2Juan Camilo Sánchez AriasNo ratings yet
- A Complex Relation Between Depression and Multiple Sclerosis: A Descriptive ReviewDocument8 pagesA Complex Relation Between Depression and Multiple Sclerosis: A Descriptive ReviewGilvan ValdevinoNo ratings yet
- Cognitive Functions in Depressive Disorders Evidence From A Population-Based StudyDocument10 pagesCognitive Functions in Depressive Disorders Evidence From A Population-Based StudyNathaly BerríoNo ratings yet
- Neuroimagen y EmocionDocument10 pagesNeuroimagen y Emocionnatsumi18No ratings yet
- Kanske 2010Document10 pagesKanske 2010童帅No ratings yet
- Epigenetic Signaling in Psychiatric Disorders - 2014Document39 pagesEpigenetic Signaling in Psychiatric Disorders - 2014Margarida SolizNo ratings yet
- Fnbeh 12 00326Document2 pagesFnbeh 12 00326Tania SilverioNo ratings yet
- Etiologies of Depressive Disorders BiologicalDocument27 pagesEtiologies of Depressive Disorders Biologicalcinnabon9.75No ratings yet
- Fpsyt 12 804269Document10 pagesFpsyt 12 804269Sahadevan NairNo ratings yet
- 2007 - BiolPsychiatry - Wang Mood Alters Amygdala Activation To Sad DistractorsDocument8 pages2007 - BiolPsychiatry - Wang Mood Alters Amygdala Activation To Sad DistractorsDimitra KlouvatouNo ratings yet
- Baxter, 1987. Local Cerebral Glucose Metabolic Rates in OCDDocument8 pagesBaxter, 1987. Local Cerebral Glucose Metabolic Rates in OCDmariobar17636No ratings yet
- CONN FMRI Functional Connectivity Toolbox Manual v17Document38 pagesCONN FMRI Functional Connectivity Toolbox Manual v17mariobar17636No ratings yet
- Ain Stimulation in The Study and Treatment of AddictionDocument16 pagesAin Stimulation in The Study and Treatment of Addictionmariobar17636No ratings yet
- Jhung, 2014. Distinct Functinal Connectivity of Limbic Network in The Washing Type OCDDocument7 pagesJhung, 2014. Distinct Functinal Connectivity of Limbic Network in The Washing Type OCDmariobar17636No ratings yet
- Default Network Connectivity As A Vulnerability Marker For OCD (Peng, 2014)Document10 pagesDefault Network Connectivity As A Vulnerability Marker For OCD (Peng, 2014)mariobar17636No ratings yet
- Manual SPM12Document508 pagesManual SPM12mariobar17636No ratings yet
- Tutorial FSLDocument23 pagesTutorial FSLmariobar17636No ratings yet
- Brain Activation of Patients With OCD During Neuropsychological and Symptom Provocation Task Before and After Symptom Improvement (Nakao Et Al, 2005, Revisado)Document10 pagesBrain Activation of Patients With OCD During Neuropsychological and Symptom Provocation Task Before and After Symptom Improvement (Nakao Et Al, 2005, Revisado)mariobar17636No ratings yet
- Introduction To Psychology ModuleDocument100 pagesIntroduction To Psychology Moduleconsela MeNo ratings yet
- Schaefer 2010Document21 pagesSchaefer 2010Andrea OrtizNo ratings yet
- MindfulnessDocument11 pagesMindfulnessapi-461329485No ratings yet
- Principles of Animal Physiology 3Rd Edition Moyes Test Bank Full Chapter PDFDocument35 pagesPrinciples of Animal Physiology 3Rd Edition Moyes Test Bank Full Chapter PDFAndrewRobinsonixez100% (7)
- Psychological Science: Facial Expressions of Emotion: New Findings, New QuestionsDocument6 pagesPsychological Science: Facial Expressions of Emotion: New Findings, New QuestionsIoana PascalNo ratings yet
- 10-1 TestDocument4 pages10-1 Testapi-301592360No ratings yet
- What Is Highly GiftedDocument8 pagesWhat Is Highly GiftedRisa SuryantiNo ratings yet
- Outline and Evaluate Research Into Effects of Age On The Accuracy of EWTDocument2 pagesOutline and Evaluate Research Into Effects of Age On The Accuracy of EWTGladei Carmelita100% (1)
- Deep Feeling Therapy: From Emotional Pain To Whole AgainDocument3 pagesDeep Feeling Therapy: From Emotional Pain To Whole AgainPaul J. Hannig, Ph.D. MFTNo ratings yet
- Your Breath Shall Set You FreeDocument58 pagesYour Breath Shall Set You FreeVenus RobertsonNo ratings yet
- Sensory Gating Deficits Pattern Completion and Disturbed Fronto Limbic Balance A Model For Description of Hallucinations and Delusions in SchizophreniaDocument12 pagesSensory Gating Deficits Pattern Completion and Disturbed Fronto Limbic Balance A Model For Description of Hallucinations and Delusions in SchizophreniaAna Maria RomeroNo ratings yet
- Psychology Recitation - 13Document2 pagesPsychology Recitation - 13shamim3261No ratings yet
- Depth of Processing and The Retention of Words in Episodic MemoryDocument27 pagesDepth of Processing and The Retention of Words in Episodic Memoryaint4everybodyNo ratings yet
- Memory TechniquesDocument5 pagesMemory TechniquesJeyakumar RajaNo ratings yet
- WMSDocument5 pagesWMSAnaaaerobiosNo ratings yet
- Acta Psychologica: Sylvie Droit-Volet, Panos Trahanias, Michail ManiadakisDocument6 pagesActa Psychologica: Sylvie Droit-Volet, Panos Trahanias, Michail ManiadakisSergioNo ratings yet
- Smell and Memory: Smells LikeDocument5 pagesSmell and Memory: Smells LikeLime LuminousNo ratings yet
- Behavioral and Neural Effects of Compassion Medita9onDocument37 pagesBehavioral and Neural Effects of Compassion Medita9onccareemailNo ratings yet
- Chapter 2 Cognitive Psychology NotesDocument8 pagesChapter 2 Cognitive Psychology NotesShekinah Pearl Niog100% (1)
- Diagnostic DiferentialDocument19 pagesDiagnostic DiferentialdouramaterNo ratings yet
- Human Development Across The Lifespan: Chapter 5 (2008)Document36 pagesHuman Development Across The Lifespan: Chapter 5 (2008)Jordan100% (3)