Professional Documents
Culture Documents
Creatinine Revision
Uploaded by
monday125Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Creatinine Revision
Uploaded by
monday125Copyright:
Available Formats
2011 - Critically discuss the methods available for measuring serum creatinine (60%).
What are the advantages and disadvantages of routine reporting of estimated
glomerular filtration rate (eGFR)? (40%).
2009 - Critically evaluate the methods available for the measurement of serum
creatinine.
2007 - Critically evaluate methods for the measurement of serum creatinine
2006 - Critically discuss the methods available for estimating glomerular filtration rate
using serum creatinine as the only biochemical measurement. What are the
advantages and disadvantages of routine reporting of estimated glomerular filtration
rate?
Creatinine
Reference Range: 45 - 120 µmol/L (serum)
Creatinine is an amino acid derivative (113 Da). It is a waste product of creatine and
phosphocreatine and is found almost exclusively (90%) in skeletal muscle tissues. About 2%
of the body's creatine is converted to creatinine every day, resulting in a fairly constant rate
of creatinine production.
Serum creatinine varies with muscle mass and renal clearance.
A diet high in stewed meat will lead to an increase in creatinine, as will supplements (body
builders).
Creatinine is freely filtered through the glomerulus and is also secreted by the proximal
tubules (5% to 10% of the excreted creatinine).
As much as 50 percent of renal function may be lost before a significant rise in plasma
creatinine is seen.
Serum creatinine concentrations are affected by factors that influence the generation,
glomerular filtration, and tubular secretion of serum creatinine.
Creatinine methods
Chemical
Creatinine reacts with alkaline picrate to form an orange red complex (Jaffe reaction-first
described in 1886). The rate of absorbance change is measured at 505nm and compared to
a known calibrant.
Not specific for creatinine. Positive interference can occur with Jaffe-like chromogens eg.
Protein, ketones, pyruvate, glucose, ascorbic acid.
Haemolysed neonatal samples have shown a negative interference, leading to a negative
result.
The addition of ferricyanide (O’ Leary method) oxidises bilirubin to biliverdin, therefore
reducing interference. A blank reaction rate is performed using sodium hydroxide to minimise
the negative interference from bilirubin. Enzymatic can be used if high bilirubin.
To improve specificity – absorption of creatinine into llyods reagent, ion exchange resin or
solvent extraction or oxidation of interferents with cerium sulphate.
Greatest success with kinetic measurement, which measures the absorbance between 20-
80 seconds to avoid interference outside of these times.
Overestimates plasma creatinine by 20%.
Enzymatic – expensive reagents
1.Creatininase catalyses creatinine to creatine which is detected with a series of enzyme
reactions (creatine kinase, pyruvate kinase and lactate dehydrogenase) and the decrease in
absorbance is monitored.
30min incubation to reach equilibrium as poor reaction kinetics
2. creatininase and creatinase. Yields H2O2 which is detected with a variety of methods.
Interference from bilirubin.
3.creatinine deaminase catalyses creatinine to ammonia which can be detected using
glutamate dehydrogenase or bethelot reaction.
More specific than jaffe.
Dry chemistry methods: use enzymatic methods - low amount of reagent needed.
Although enzymatic expensive, used in dry chemistry systems (as lower reagent), including
some POC testing devices.
Isotope dilution-mass spectrometry (IDMS)-definitive method.
Candidate reference method - uses ion-exchange HPLC with UV detection.
Matrix problems when lyophilised preps used.
Imprecision at low creatinine concentrations and therefore greater error in GFR estimations.
Good correlation between Jaffe and enzymatic – differences due to calibration and
interference.
Calibration not standardised, therefore variation between labs which accounts for 85% of
differences.
Glomerular Filtration Rate
GFR can be measured directly by clearance studies of exogenous markers (inulin (gold
standard), iohexol, iothalamate and Cr51-EDTA). But these are costly and time consuming.
GFR can also be measured by clearance studies of endogenous markers such as urea and
creatinine. But these require a paired serum and an accurately timed urine collection. The
patient should be kept well hydrated and still.
Major use of MDRD eGFR is screening for CKD – more sensitive for the detection of CKD
than serum creatinine and more accurate than creatinine clearance. It is mainly used for the
systematic staging of kidney disease (CKD = eGFR < 60mL/min/1.73m2 for at least 3
months).
Several formulae derived from MDRD study.
In adults, eGFR should be calculated using the 4 variable IDMS traceable version of the
MDRD equation:
eGFR (ml/min/1.73m2) = 175 x (sCr x 0.011312 -1.154) x age-0.203 x 0.742 (if female) x
1.212 (if black)
sCr (µmol/L), age (years)
Formula was derived from studies on patients with chronic renal failure. Therefore values
greater than 60 should be reported as >60 (regarded normal if no clinical/lab evidence of
renal disease).
Equations tend to underestimate normal GFR function and slightly low values should not be
over-interpreted.
The patients creatinine level must also be stable
Not applicable in acute renal failure, pregnancy, severe muscle wasting, oedematous
conditions, amputees, malnourished people and in children - Schwartz or Cockcroft-Gault
equations are used for children.
The more a method overestimates true creatinine, the greater the underestimation of GFR.
The precision and accuracy of eGFR decreases as GFR increases.
Declines with age.
If ethnic origin unknown, assume Caucasian ethnicity.
CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration) equation – performs better
than the MDRD equation, especially at higher GFRs with less bias, improved precision and
better accuracy. Could possibly replace the MDRD equation for routine clinical use.
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Creativity Triggers 2017Document43 pagesCreativity Triggers 2017Seth Sulman77% (13)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Clock of Destiny Book-1Document46 pagesClock of Destiny Book-1Bass Mcm87% (15)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Pleasing Her Husband's Boss (Hot Wife and Her Cuckold 2) by Michaels DeanaDocument29 pagesPleasing Her Husband's Boss (Hot Wife and Her Cuckold 2) by Michaels Deanamonday12560% (10)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
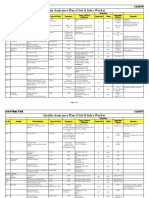
- Quality Assurance Plan - CivilDocument11 pagesQuality Assurance Plan - CivilDeviPrasadNathNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- JonathanLandsman VitaminToKillVirusesDocument18 pagesJonathanLandsman VitaminToKillVirusesPortugal ForenseNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Top Survival Tips - Kevin Reeve - OnPoint Tactical PDFDocument8 pagesTop Survival Tips - Kevin Reeve - OnPoint Tactical PDFBillLudley5100% (1)
- An Analysis of The Cloud Computing Security ProblemDocument6 pagesAn Analysis of The Cloud Computing Security Problemrmsaqib1No ratings yet
- Market Structure and TrendDocument10 pagesMarket Structure and TrendbillNo ratings yet
- Define Variable and ConstantDocument17 pagesDefine Variable and ConstantSenthil MuruganNo ratings yet
- Acupuncture in Modern MedicineDocument400 pagesAcupuncture in Modern Medicinepranav100% (2)
- Robert Egby - DecreesDocument9 pagesRobert Egby - DecreesmuzickaueNo ratings yet
- Karen Smith Duty Biochemist ScenariosDocument43 pagesKaren Smith Duty Biochemist Scenariosmonday125100% (2)
- HAI ROBOTICS Introduction ENV2022.0829 MarketingDocument40 pagesHAI ROBOTICS Introduction ENV2022.0829 MarketingKit WooNo ratings yet
- OspeDocument29 pagesOspemonday125No ratings yet
- Project Report On HeritageDocument39 pagesProject Report On HeritageBALA YOGESH YANDAMURINo ratings yet
- FRCPath OSPE 25042014Document11 pagesFRCPath OSPE 25042014monday125No ratings yet
- SchedulingDocument47 pagesSchedulingKonark PatelNo ratings yet
- Become Healthy or Extinct Darryl DsouzaDocument180 pagesBecome Healthy or Extinct Darryl Dsouzacontactsm100% (1)
- ADMA 2010 BlackboardDocument41 pagesADMA 2010 Blackboardmonday125No ratings yet
- Annals 1368 001Document9 pagesAnnals 1368 001monday125No ratings yet
- 2020 Review PIC - Uniform PolicyDocument2 pages2020 Review PIC - Uniform Policymonday125No ratings yet
- Clinical Guideline For Anticoagulant Use in AdultsDocument108 pagesClinical Guideline For Anticoagulant Use in Adultsmonday125No ratings yet
- Caffeine BronchodilatorDocument30 pagesCaffeine Bronchodilatormonday125No ratings yet
- Les Perry How Do We Define An Adequate Response To SynacthenDocument66 pagesLes Perry How Do We Define An Adequate Response To Synacthenmonday125No ratings yet
- ICP-MS Talk ACBDocument31 pagesICP-MS Talk ACBmonday125No ratings yet
- Acupuncture PDFDocument14 pagesAcupuncture PDFmonday125No ratings yet
- 2010 - Zhang - EAP For AR Review PDFDocument8 pages2010 - Zhang - EAP For AR Review PDFmonday125No ratings yet
- Business Case For A New Consultant Chemical Pathology Final VersionDocument11 pagesBusiness Case For A New Consultant Chemical Pathology Final Versionmonday125No ratings yet
- Les Perry How Do We Define An Adequate Response To SynacthenDocument66 pagesLes Perry How Do We Define An Adequate Response To Synacthenmonday125No ratings yet
- Uric AcidDocument6 pagesUric Acidmonday125100% (1)
- Bible 2018Document183 pagesBible 2018monday125No ratings yet
- 1 s2.0 S0753332218345657 MainDocument11 pages1 s2.0 S0753332218345657 Mainmonday125No ratings yet
- Trisomy ScreeningDocument55 pagesTrisomy Screeningmonday125No ratings yet
- Oil Pulling A Traditional Method On The Edge of EvDocument4 pagesOil Pulling A Traditional Method On The Edge of Evmonday125No ratings yet
- ST Agnes Catholic Primary SchoolDocument12 pagesST Agnes Catholic Primary Schoolmonday125No ratings yet
- Critical Appraisal: DR A C J Hutchesson Chair of Examiners' Panel, Frcpath (Clinical Biochemistry)Document10 pagesCritical Appraisal: DR A C J Hutchesson Chair of Examiners' Panel, Frcpath (Clinical Biochemistry)monday125No ratings yet
- Writing An Abstract: Sally - Benton@bartshealth - Nhs.ukDocument7 pagesWriting An Abstract: Sally - Benton@bartshealth - Nhs.ukmonday125No ratings yet
- SasDocument8 pagesSasmonday125No ratings yet
- FOCUS SAS Training Day Leeds Dr. Joanna Sheldon Protein Reference Unit, St. George'sDocument19 pagesFOCUS SAS Training Day Leeds Dr. Joanna Sheldon Protein Reference Unit, St. George'smonday125No ratings yet
- DRDocument17 pagesDRmonday125No ratings yet
- DRDocument17 pagesDRmonday125No ratings yet
- Comparison of Multi-Coil and Diaphragm Spring ClutchesDocument3 pagesComparison of Multi-Coil and Diaphragm Spring Clutchesmasb_994077No ratings yet
- A Mini-Review On New Developments in Nanocarriers and Polymers For Ophthalmic Drug Delivery StrategiesDocument21 pagesA Mini-Review On New Developments in Nanocarriers and Polymers For Ophthalmic Drug Delivery StrategiestrongndNo ratings yet
- LNWH Alcohol GUIDELINE SUMMARY 2018Document1 pageLNWH Alcohol GUIDELINE SUMMARY 2018Ai Hwa LimNo ratings yet
- Enzymatic Hydrolysis, Analysis of Mucic Acid Crystals and Osazones, and Thin - Layer Chromatography of Carbohydrates From CassavaDocument8 pagesEnzymatic Hydrolysis, Analysis of Mucic Acid Crystals and Osazones, and Thin - Layer Chromatography of Carbohydrates From CassavaKimberly Mae MesinaNo ratings yet
- Finance 2021 23Document16 pagesFinance 2021 23GAURAV UPADHYAYNo ratings yet
- Unix SapDocument4 pagesUnix SapsatyavaninaiduNo ratings yet
- Security Policy 6 E CommerceDocument6 pagesSecurity Policy 6 E CommerceShikha MehtaNo ratings yet
- Solitax SCDocument8 pagesSolitax SCprannoyNo ratings yet
- Annotated Bibliography 2Document3 pagesAnnotated Bibliography 2api-458997989No ratings yet
- Communication MethodDocument30 pagesCommunication MethodMisganaw GishenNo ratings yet
- Turbine Flowmeters-Commonly Asked Questions and Answers: For Chemical Composition Information.)Document8 pagesTurbine Flowmeters-Commonly Asked Questions and Answers: For Chemical Composition Information.)Alexander KlmNo ratings yet
- MGT403 Slide All ChaptersDocument511 pagesMGT403 Slide All Chaptersfarah aqeelNo ratings yet
- - Анализ текста The happy man для ФЛиС ЮФУ, Аракин, 3 курсDocument2 pages- Анализ текста The happy man для ФЛиС ЮФУ, Аракин, 3 курсJimmy KarashNo ratings yet
- Skills Check Extra 2ADocument1 pageSkills Check Extra 2AVishmi JayawardeneNo ratings yet
- Mars Atlas MOM 8 13Document6 pagesMars Atlas MOM 8 13aldert_pathNo ratings yet
- (LaSalle Initiative) 0Document4 pages(LaSalle Initiative) 0Ann DwyerNo ratings yet
- Enzymes WorksheetDocument5 pagesEnzymes WorksheetgyunimNo ratings yet
- Unit 2 Module 2 Combined-1Document14 pagesUnit 2 Module 2 Combined-1api-2930012170% (2)
- ETSI EG 202 057-4 Speech Processing - Transmission and Quality Aspects (STQ) - Umbrales de CalidaDocument34 pagesETSI EG 202 057-4 Speech Processing - Transmission and Quality Aspects (STQ) - Umbrales de Calidat3rdacNo ratings yet