Professional Documents
Culture Documents
Clinical Manifestations: Psammoma Bodies
Uploaded by
shinaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Clinical Manifestations: Psammoma Bodies
Uploaded by
shinaCopyright:
Available Formats
A 43-year-old woman comes to the office to discuss amenorrhea.
She began having irregular menses 2 years ago, and her last menstrual period was 9 months ago. Family history is unremarkable.
Laboratory studies show an increased serum prolactin level, a normal TSH level, and an undetectable β-hCG concentration. Serum calcium is normal. MRI reveals a 6-mm pituitary adenoma. The
patient refuses medical and surgical therapy as she is happy about not having menstrual periods. If left untreated, this patient is at greatest risk of developing which of the following?
This patient's small pituitary adenoma with an elevated prolactin level and secondary amenorrhea is consistent with a prolactin-secreting adenoma (prolactinoma). High levels of prolactin
suppress GnRH secretion from the hypothalamus, leading to reduced secretion of LH (and to a lesser extent FSH) and subsequent hypogonadism. Nonsecretory ("nonfunctioning") adenomas can
also cause mild hyperprolactinemia due to pressure on the stalk, but these tumors primarily cause mass-effect symptoms (eg, hypopituitarism, headache, bitemporal hemianopsia) due to pressure on
surrounding structures.
Estrogen maintains bone mass in premenopausal women. Low estrogen levels lead to increased production of inflammatory cytokines (especially IL-1 and tumor necrosis factor–alpha), increasing
expression of the receptor activator of nuclear factor kappa B ligand (RANKL) and resulting in increased osteoclast activity. Loss of estrogen, whether from menopause, ovulatory dysfunction, or
surgical removal of the ovaries, increases the risk of bone loss and osteoporosis.
Glucose is the major source of energy for all cells of the body. In the majority of tissues, glucose transport occurs along its concentration gradient, from higher concentrations outside the cell toward
lower concentrations inside the cell. However, glucose cannot passively diffuse across the cell membrane in any significant amount and requires carrier proteins to aid its crossing. Transport across
the cell membrane by carrier proteins (which undergo conformational changes as the substrate is transported, unlike channel proteins) is termed carrier-mediated transport. Transport that is facilitated
by transmembrane proteins without the expenditure of energy is called facilitated diffusion.
Transmembrane carrier proteins that belong to the GLUT family transport glucose by facilitated diffusion. These proteins are stereoselective and preferentially catalyze the entrance of D-glucose rather
than L-glucose into cells. GLUT4 is the insulin-sensitive transporter found in skeletal muscle cells and adipocytes. In these cells, the GLUT4 protein is stored in cytoplasmic vesicles. Under the
influence of insulin, the transporter protein is incorporated into the cell membrane. An increased number of transporters in the membrane leads to an increased rate of glucose uptake by the cells.
Another important glucose transporter is GLUT2. It facilitates export of glucose from the liver, small intestine, and kidneys into the circulation and also helps to control insulin secretion in the pancreas.
Incretins are gastrointestinal hormones produced by the gut mucosa that stimulate pancreatic insulin secretion in response to sugar-containing meals. This response is independent of blood glucose
levels, and typically occurs prior to any elevation in blood glucose level following a meal. Two hormones with incretin effects are glucagon-like peptide-1 (GLP-1) and gastric inhibitory peptide
(glucose-dependent insulinotropic peptide, GIP). Insulin levels will also increase following intravenous administration of glucose due to the sensitivity of the pancreatic beta-cells to increases in blood
glucose, but this increase will not be as marked as that seen following oral glucose administration because the effect of incretin is absent.
Thiazolidinediones (TZDs) exert their glucose-lowering effect by reducing insulin resistance. They do this by binding to peroxisome proliferator-activated receptor-γ (PPAR-γ), a transcriptional
regulator of genes involved in glucose and lipid metabolism. TZDs induce a conformational change in PPAR-γ, which subsequently binds additional cofactors. This complex then binds to the
transcriptional regulatory sequence of the target genes. Important genes that are upregulated by TZDs include:
Glucose transporter-4 (GLUT4), an insulin-responsive transmembrane glucose transporter expressed in adipocytes and skeletal myocytes that increases glucose uptake by target cells
Adiponectin, a cytokine secreted by fat tissue that increases the number of insulin-responsive adipocytes and regulates fatty acid oxidation
Because the glucose-lowering effect of TZDs requires alterations in gene transcription and protein synthesis, it takes several days to a few weeks after commencing TZD therapy to observe a
significant reduction in glucose levels.
The main side effect of TZDs is fluid retention due to increased sodium reabsorption in the renal collecting tubules. This can lead to water weight gain, peripheral edema, and decompensation of
underlying congestive heart failure. Fluid retention is often worse when TZDs are given in combination with insulin. TZDs also cause adipose weight gain, likely due to a combination of increased
fat storage in adipocytes and an increased number of adipocytes in subcutaneous tissue.
The brain relies heavily on glucose as an energy source, and the level of glucose uptake by the brain is not regulated by insulin. Prolonged central nervous system (CNS) hypoglycemia leads to
irreversible neurologic deficits and death. To prevent injury, multiple counter-regulatory systems are activated in response to hypoglycemia; these include glucagon, the sympathetic nervous system,
and to a lesser extent, growth hormone and cortisol. Glucagon increases blood glucose primarily by increasing glycogenolysis and gluconeogenesis. Epinephrine limits glucose use by insulin-
sensitive tissues and also stimulates hepatic glycogenolysis and gluconeogenesis. If hypoglycemia persists, the activity of higher brain centers diminishes to reduce glucose requirements.
Symptoms of hypoglycemia fall into 2 broad categories: neurogenic (autonomic) and neuroglycopenic.
1. Neurogenic symptoms are caused by sympathoadrenal activation and are mediated via norepinephrine/epinephrine and acetylcholine released by sympathetic postganglionic nerve fibers.
Symptoms of norepinephrine/epinephrine release include tremulousness, palpitations, and anxiety/arousal, whereas cholinergic symptoms include sweating, hunger, and paresthesias.
2. Neuroglycopenic symptoms include behavioral changes, confusion, visual disturbances, stupor, and seizures.
Non-selective β-blockers (eg, propranolol, timolol, nadolol) inhibit norepinephrine/epinephrine-mediated compensatory reactions to hypoglycemia (cholinergic symptoms are unaffected). In
addition, blockade of β2-adrenergic receptors inhibits hepatic gluconeogenesis and peripheral glycogenolysis and lipolysis. Non-selective β-blockers should be used with caution in diabetic
patients as these can increase the risk of hypoglycemia and reduce patient awareness of hypoglycemia. Selective β1 blockers and β-blockers with intrinsic sympathomimetic activity (eg,
pindolol, acebutolol) are preferred for diabetics as these have minimal effect on glucose metabolism and adrenergic symptoms.
A 4-year-old boy is brought to the physician after his mother noticed that he started developing pubic hair. She also says he had a recent growth spurt and is now taller than his 5-year-old brother. In
addition, his preschool teacher has noticed axillary odor after he runs or plays. On physical examination, his height corresponds to the 96th percentile and his weight corresponds to the 78th
percentile for his age. There is sparse growth of long, pigmented hair at the base of the penis and in both axilla. Laboratory assessment reveals high serum concentrations of 17-
hydroxyprogesterone and testosterone.
21-hydroxylase deficiency is a form of congenital adrenal hyperplasia caused by an autosomal recessive inherited defect in the 21-hydroxylase gene. It can present as 3 distinct syndromes
depending on the residual activity of the 21-hydroxylase enzyme. This patient is most likely suffering from the classic, non-salt-wasting form of the disease. Males with this variety typically present
during the first few years of life with early virilization and accelerated linear growth due to shunting of corticosteroid precursors toward androgen production in the adrenal cortex. Females with
this variety present with ambiguous genitalia at birth. As in all forms of 21-hydroxylase deficiency, patients will have increased serum concentrations of 17-hydroxyprogesterone and androgens.
Adrenal medullary hyperplasia would result in increased production and release of catecholamines. This would have no effect on virilization or linear growth and would not produce the laboratory
abnormalities noted.
Leydig cell hyperplasia would result in masculinization due to excessive production of testosterone, androstenedione, and dehydroepiandrosterone. However, there would be no excess of the adrenal
hormone 17-hydroxyprogesterone.
Pituitary adenomas producing excessive luteinizing hormone and follicle-stimulating hormone can result in increased testosterone levels but would not increase 17-hydroxyprogesterone levels.
Pituitary adenomas producing excess adrenocorticotropic hormone (ACTH) can lead to excessive adrenal androgen production. However, the symptoms of excess cortisol production (Cushing's
syndrome) would dominate.
A seminoma is a testicular tumor most commonly seen in adults. These tumors are derived from the seminiferous tubules and do not present with virilization or hormonal abnormalities.
Patients with congenital adrenal hyperplasia due to 21-hydroxylase deficiency have defective conversion of 17-hydroxyprogesterone to 11-deoxycortisol, which impairs cortisol synthesis. Decreased
cortisol levels are sensed by the hypothalamus and cause a consequential increase in adrenocorticotropic hormone (ACTH) secretion by the anterior pituitary. This results in stimulation of the adrenal
cortex and androgen overproduction.
Treatment of congenital adrenal hyperplasia involves administering low (ie, physiologic) doses of exogenous corticosteroids to suppress ACTH secretion. By removing excessive ACTH stimulation,
exogenous corticosteroids can decrease androgen production by the adrenal cortex.
Testosterone is a gonadal androgen that is synthesized only in minimal quantities by the adrenal gland. The virilizing effects seen in this patient are the result of excessive adrenal androgen production
(eg, dehydroepiandrosterone and androstenedione). These adrenal androgens undergo peripheral conversion to testosterone, thus explaining the high levels of testosterone found in this patient.
A 51-year-old woman comes to the physician for a routine follow-up appointment. She appears in good health and has no complaints. Physical examination shows a nodule in the left lobe of the
thyroid. She has no family history of thyroid cancer and has had no prior radiation exposure. Thyrotropin-stimulating hormone level is normal. Thyroid ultrasound shows a hypo-echoic nodule in
the left lobe of the thyroid with increased central blood flow. Fine-needle aspiration of the nodule is performed, and cytology shows clusters of overlapping cells with large nuclei containing
sparse, finely dispersed chromatin. Numerous intranuclear inclusion bodies and grooves are also seen. Which of the following is the most likely diagnosis?
Thyroid nodules are seen often in clinical practice. The prevalence increases with age and most are benign. Approximately 5%-10% of thyroid nodules are cancerous. Malignant causes of thyroid
nodules, in order of decreasing frequency, are papillary (>70% of cases), follicular, medullary, and anaplastic carcinoma. Factors that increase the risk of thyroid malignancy are a positive family history
of thyroid cancer and a history of neck irradiation in childhood. Fine-needle aspiration has a high sensitivity and specificity in differentiating benign nodules from thyroid cancers, particularly papillary
thyroid cancers. Papillary carcinoma cells are characteristically large with overlapping nuclei containing finely dispersed chromatin, giving them a ground-glass appearance (Orphan Annie eye
[arrow]). Numerous intranuclear inclusions and grooves can be seen due to invagination of the nuclear membrane. Psammoma bodies (laminated calcium deposits) are also found within the
tumor.
Anaplastic cancer is an aggressive tumor with a very poor prognosis. Cytologic features of anaplastic cancer are markedly pleomorphic cells, including irregular giant cells and biphasic spindle
cells.
Most benign thyroid nodules are colloid nodules formed from focal hyperplasia of normal thyroid follicular cells. On cytopathology, a colloid nodule consists of variable-sized thyroid follicles,
colloid, and macrophages.
Distinguishing a benign follicular adenoma from a well-differentiated follicular cancer depends on the presence of vascular and capsular invasion, which cannot be determined on a fine-needle
aspiration specimen. Gene expression analysis is also useful for differentiating malignant from benign follicular lesions.
Medullary thyroid cancer arises from parafollicular c-cells and appears histologically as polygonal to spindle-shaped cells with a slightly granular cytoplasm that stains for calcitonin. Adjacent
amyloid deposits are typically seen. Medullary thyroid cancer is a component of multiple endocrine neoplasia 2A and 2B.
The superior thyroid artery (a branch of the external carotid artery) and the inferior thyroid artery (a branch of the thyrocervical trunk) provide the blood supply to the thyroid and parathyroid glands.
The superior thyroid artery and vein and external branch of the superior laryngeal nerve course together in a neurovascular triad that originates superior to the thyroid gland and lateral to the
thyroid cartilage. The external branch is at risk of injury during thyroidectomy as it courses just deep to the superior thyroid artery. The cricothyroid muscle is the only muscle innervated by this
nerve. It originates on the cricoid cartilage and inserts on the lower border of the thyroid cartilage. The cricothyroid muscle acts to tense the vocal cords, and denervation injury may cause a low,
hoarse voice with limited range of pitch.
The internal branch of the superior laryngeal nerve does not innervate any muscles but provides sensory innervation to the laryngeal mucosa above the vocal folds.
The remaining laryngeal muscles are innervated by the recurrent laryngeal nerves, which also provide sensory innervation to the larynx below the vocal folds.
A 25-year-old man comes to the office for evaluation of facial acne. He has no significant past medical history and does not use tobacco or alcohol. The patient works as a personal trainer. His
family history is significant for diabetes mellitus in his mother and leukemia in his father. His blood pressure is 134/82 mm Hg and pulse is 58/min. On physical examination, there is mild facial acne.
The patient's lungs are clear to auscultation. The liver span is 8 cm, and the spleen is not palpable. His testes are soft, and testicular volume is decreased. Laboratory results are as follows:
Hematocrit 60%
White blood cells 7,500/mm3
Platelets 225,000/mm3
Erythrocyte sedimentation rate 15 mm/hr
Serum creatinine 1.2 mg/dL
Blood urea nitrogen 18 mg/dL
Which of the following is the most likely explanation for this patient's abnormal laboratory findings?
This patient has acne, testicular atrophy, and erythrocytosis, findings concerning for androgenic steroid abuse. Abuse of androgens, androgen precursors, and agents that increase endogenous
androgen production is most common in young adults who engage in competitive athletic activities or for cosmetic purposes.
Chronic androgen use may increase muscle mass but has multiple associated risks. Testosterone stimulates red blood cell production, which accounts for the higher hematocrit in normal
males compared to normal females. This effect is exaggerated in exogenous androgen abuse, which increases hematocrit in a dose-dependent manner. Androgens decrease gonadotropin
secretion, which results in testicular atrophy and decreased sperm production. Other common findings include virilization in women (eg, clitoromegaly, hirsutism) and acne.
A 42-year-old woman with Graves disease is hospitalized for elective total thyroidectomy. Her hyperthyroid symptoms have been controlled with methimazole and propranolol, but she still has a
goiter. The patient has no other medical problems. She undergoes total thyroidectomy without any immediate operative complications and feels well the next day. Laboratory results are as follows:
Serum chemistry
Sodium 141 mEq/L
Potassium 4.4 mEq/L
Creatinine 0.8 mg/dL
Calcium 7.5 mg/dL
Preoperative electrolyte values were within normal limits. Which of the following medications should be started in this patient?
The parathyroid glands are relatively small and indistinct and can be injured during thyroid surgery due to direct trauma, devascularization, or inadvertent removal. Transient or permanent
postoperative hypoparathyroidism can occur following thyroidectomy and cause clinically significant hypocalcemia. Patients may be asymptomatic initially but can develop paresthesias (of the
lips, mouth, hands, and feet), muscle twitching, or cramps. Worsening hypocalcemia can lead to trismus or tetany with changes in mental status and generalized seizures.
Postoperative supplementation with oral calcium and vitamin D can be used to treat and prevent postoperative hypocalcemia. Calcitriol, the active form of vitamin D, should be chosen over calcidiol
as the conversion of calcidiol to calcitriol is dependent on parathyroid hormone, and patients with hypoparathyroidism can have inadequate production of calcitriol.
A 63-year-old man comes to the office for a follow-up visit. Two months ago, he was hospitalized for chest pain and was found to have a blockage in the left anterior descending artery. He had
percutaneous coronary intervention with placement of a drug-eluting stent, and was discharged on appropriate medical therapy. His other medical problems include hypertension, type 2 diabetes
mellitus, and degenerative joint disease. The patient has been taking all his medications as prescribed. He has no chest pain but does have diffuse muscle aches and cramps, especially after
exercise. Physical examination is unremarkable. Laboratory testing reveals elevated serum creatine kinase. The medication most likely responsible for this patient's current findings also causes
which of the following effects?
This patient's symptoms are most likely due to statin-induced myopathy. Statins are an effective treatment for hypercholesteremia and are now routinely prescribed for all patients with symptomatic
coronary artery disease, regardless of baseline cholesterol levels. Myopathy is the most common complication of statin use, and symptoms can range from myalgia or myopathy, with or without
myonecrosis (elevated serum creatine kinase), to frank rhabdomyolysis.
Statins act through competitive inhibition of HMG-CoA reductase, preventing conversion of HMG-CoA to mevalonic acid (the rate-limiting step in cholesterol biosynthesis). Decreased liver
cholesterol synthesis leads to increased hepatic clearance of LDL from the circulation by LDL receptors. After mediating endocytosis of LDL particles, the LDL receptors are returned to the cell
surface for reuse (receptor recycling); LDL is digested and used for metabolic purposes. This increase in LDL receptor recycling allows intrahepatic cholesterol levels to remain at normal levels while
blood levels are kept low.
A 43-year-old woman comes to the office due to increasing fatigue and weight gain despite decreased food intake. She states, "I have not been feeling like myself lately." The patient asks to be
referred to a dermatologist as she has always had "nice" skin that has now become dry. Her hair has been thinning and she hopes that a dermatologist can help with that too. Laboratory
evaluation shows high serum TSH, low triiodothyronine (T3), and low thyroxine (T4) levels. The patient has a family member with fatigue whose energy level increased after liothyronine (T3)
supplementation, and she asks to try this medication. Administering this therapy would most likely result in which of the following hormone level changes in this patient?
Circulating thyroid hormone exists in 3 primary forms:
1. T4 (thyroxine) is the major secretory product of the thyroid gland.
2. T3 (triiodothyronine) is the most active form of thyroid hormone; a small amount is released by the thyroid gland, but the majority arises from peripheral deiodination of T4.
3. Reverse T3 (rT3) is an inactive form that is generated almost entirely from the peripheral conversion of T4.
The hypothalamus-pituitary-thyroid axis is regulated via negative feedback by thyroid hormone on thyrotropin-releasing hormone–secreting neurons in the hypothalamus and thyrotrophs of the
anterior pituitary. In the normal state, most of the circulating thyroid hormone is in the form of T4, which provides most of the feedback suppression of TSH release. However, T3 also suppresses TSH.
This patient has primary hypothyroidism, with low thyroid hormone (T3 and T4) and elevated TSH levels. Exogenous T3 supplementation rapidly suppresses TSH levels by increasing negative
feedback, which in turn decreases T4 secretion from the thyroid gland. Furthermore, rT3 also decreases because less T4 is available for conversion (T3 cannot be converted into rT3).
However, synthetic T3 (liothyronine) is not recommended for the routine treatment of hypothyroidism, as it has a short half-life and patients can experience wide fluctuations in plasma T3 levels. T4
(levothyroxine) supplementation provides a more physiologic effect and is preferred.
A 56-year-old woman comes to the physician complaining of recent weight gain and easy fatigability. Her blood pressure is 160/90 mm Hg and heart rate is 80/min. Her fasting plasma glucose level is
135 mg/dL and she has increased 24-hour urinary cortisol excretion. Further evaluation shows that her serum cortisol is suppressed by high-dose, but not low-dose, dexamethasone. Her serum
adrenocorticotropic hormone (ACTH) levels are borderline elevated. Which of the following is the most likely cause of this patient's problems?
Features of Cushing syndrome
Central obesity (eg, fat accumulation in the cheeks & dorsocervical & supraclavicular fat pads)
Clinical
Skin atrophy & wide, purplish striae
manifestations
Proximal muscle weakness
Hypertension
Glucose intolerance
Skin hyperpigmentation (if ACTH excess)
24-hour urinary cortisol excretion
Diagnosis
Late-night salivary cortisol assay
Low-dose dexamethasone suppression test
This patient's clinical presentation is consistent with Cushing syndrome, the syndrome of glucocorticoid excess. Causes of Cushing syndrome include:
1. Treatment with pharmacological doses of exogenous glucocorticoids (most common)
2. ACTH-secreting pituitary adenomas
3. Ectopic production of ACTH (ie, paraneoplastic)
4. Primary adrenocortical hyperplasia (eg, adrenocortical tumors)
Of these, only pituitary adenomas and ectopic ACTH production present with elevated ACTH levels.
Screening tests for endogenous Cushing syndrome include low-dose dexamethasone suppression testing and measurement of late-night salivary cortisol levels or 24-hour urinary cortisol excretion.
Administration of dexamethasone, a potent glucocorticoid, will suppress ACTH and cortisol levels in normal individuals. However, ACTH and cortisol levels will not be suppressed in patients with
Cushing syndrome.
When Cushing syndrome is caused by pituitary ACTH overproduction (Cushing disease), cortisol levels do not suppress with low-dosedexamethasone but do suppress with high-dose
dexamethasone. This test is useful in differentiating Cushing disease from Cushing syndrome caused by ectopic ACTH production. Ectopic ACTH production (eg, from malignant tumors such as
small cell lung cancer) is typically associated with markedly elevated ACTH levels that do not suppress even after high-dose dexamethasone administration.
A 25-year-old woman is brought to the emergency department due to progressive lethargy. For the last 3 weeks, she has also had loss of appetite, constipation, muscle weakness, and increased
thirst and urination. The patient's medical history is unremarkable, but she has been taking large doses of vitamin D supplements in the belief that they are beneficial for her health. On examination,
she is stuporous and has dry mucous membranes. The metabolic abnormality most likely causing this patient's clinical findings can also occur in which of the following conditions?
This patient has clinical features consistent with hypercalcemia. Moderate doses of vitamin D are recommended for patients at risk for osteoporosis to increase intestinal absorption of calcium and
phosphate, leading to improved mineralization of bone. However, excessive vitamin D supplementation can lead to symptomatic hypercalcemia, with impaired depolarization of neuromuscular
membranes (leading to muscle weakness, constipation, confusion) and impaired concentration of urine in the distal tubule (leading to polyuria/polydipsia). Chronic intoxication can lead to renal
stone formation and bone demineralization with associated bone pain. Hypervitaminosis D is most often seen in food faddists, patients with mental illness, and patients treated with prescription
calcitriol for an excessive period.
Normally, 25-hydroxyvitamin D is converted to 1,25-dihydroxyvitamin D (calcitriol, the active form) by 1-α-hydroxylase in the kidneys, a process regulated by parathyroid hormone (PTH). However,
patients with granulomatous diseases (eg, sarcoidosis, tuberculosis) can have PTH-independent conversion due to expression of 1-α-hydroxylase in activated macrophages. This leads to
increased intestinal calcium absorption with subsequent hypercalcemia and hypercalciuria. A similar process is also frequently seen in Hodgkin disease and some non-Hodgkin lymphomas.
A 34-year-old woman experiences nausea, abdominal pain, and dizziness after undergoing open reduction and internal fixation of a femur fracture. One year ago, she was diagnosed with systemic
lupus erythematosus with significant renal involvement, and she has since been on chronic glucocorticoid therapy with prednisone. The patient was maintained on her usual daily dose of
prednisone throughout the perioperative period. Blood pressure is 90/60 mm Hg and pulse is 120/min. Compared to the normal physiologic response to surgery, this patient most likely has which of
the following patterns of hypothalamic-pituitary-adrenal axis activity?
This patient is suffering from acute adrenal insufficiency (adrenal crisis) due to suppression of the hypothalamic-pituitary-adrenal (HPA) axis by long-term glucocorticoid therapy. Glucocorticoids
suppress the synthesis and release of corticotropin-releasing hormone (CRH) from the hypothalamus and also block its ACTH stimulatory effect on the anterior pituitary. Long-term suppression leads
to atrophy of hypothalamic CRH-releasing neurons, pituitary corticotrophic cells, and the adrenal zona reticularis (androgen- producing inner zone) and zona fasciculata (cortisol-producing middle
zone).
Chronic glucocorticoid use is characterized by low CRH, ACTH, and cortisol levels that cannot rise in response to stressful situations (eg, infections, surgery). This lack of a stress response can result
in relative glucocorticoid deficiency even when the patient's baseline glucocorticoid regimen is maintained. Because glucocorticoids help maintain normal vascular tone (eg, by increasing
norepinephrine, renin, and angiotensin vasoconstrictive activity), glucocorticoid deficiency can precipitate hypotension/shock. In such cases, a higher stress dose is needed to compensate for the
increased physiologic demands and prevent the development of adrenal crisis.
A 2 year-old boy is brought to the emergency department with fever, vomiting, and sleepiness. He had several episodes of emesis this morning, and his mother was unable to wake him from his
afternoon nap. The boy has had mild rhinorrhea and fever for the past 3 days. Since the newborn period, the parents say that the patient has had multiple illnesses characterized by vomiting and
sleepiness. Prior laboratory testing revealed increased blood ammonia levels during these episodes and markedly increased orotic acid excretion in the urine. Physical examination shows a
tachypneic boy who is unresponsive to all stimuli. Which of the following enzymes is most likely to be deficient in this patient?
Ammonia generated from the metabolism of amino acids is converted into urea by the urea cycle. The combination of bicarbonate (HCO3-), ammonia, and ATP is catalyzed by carbamoyl phosphate
synthetase (rate-limiting enzyme in the urea cycle) to yield carbamoyl phosphate. Carbamoyl phosphate combines with ornithine to form citrulline in a reaction catalyzed by ornithine
transcarbamylase. Citrulline enters the cytosol and is converted to argininosuccinate, which is then converted to arginine. The conversion of arginine to ornithine by arginase completes the urea
cycle by releasing a urea molecule. N-acetylglutamate serves as a regulator of the urea cycle through activation of carbamoyl phosphate synthetase I.
This patient most likely has ornithine transcarbamylase (OTC) deficiency, the most common urea cycle disorder. OTC deficiency results in excess carbamoyl phosphate, which stimulates
pyrimidine synthesis. As an intermediate product in this pathway, orotic acid accumulates and results in increased urinary orotic acid.
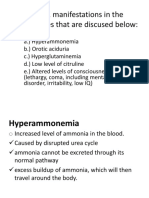
Patients also have hyperammonemia due to impaired ammonia excretion, which is a metabolic emergency. Ammonia is neurotoxic and causes episodes of vomiting and confusion/coma.
Tachypnea also occurs due to cerebral edema from ammonia buildup, resulting in central hyperventilation and respiratory alkalosis. Metabolic decompensation is often triggered by illness (eg, viral
upper respiratory infection, acute otitis media), fasting, or increased protein intake.
Although defects in carbamoyl phosphate synthetase I and N-Acetylglutamate synthetase also result in hyperammonemia, levels of carbamoyl phosphate are low and orotic acid is not
elevated in the urine.
Hypoxanthine-guanine phosphoribosyltransferase deficiency (Lesch-Nyhan syndrome) results in hyperuricemia because purines cannot be salvaged from degraded DNA. Urate kidney stones
and self-mutilation are classic clinical manifestations.
Uridine monophosphate synthetase (UMPS) is part of the pyrimidine synthesis pathway. UMPS deficiency leads to orotic acid buildup (similar to OTC deficiency) but not hyperammonemia.
Characteristic findings include megaloblastic anemia and delayed growth.
A 23-year-old apparently healthy man who recently immigrated to the United States comes to an outpatient clinic to establish care. When asked about his past medical history, he says that he has no
significant medical problems. However, his mother told him that he was born with "a problem metabolizing sugar." The patient maintains no dietary restrictions and regularly eats vegetables, fruits,
meats, and processed foods. Urine samples show a repeatedly positive copper reduction test, but glucose oxidase dipstick testing is negative. Which of the following enzymes is most likely to
be deficient in this patient?
This asymptomatic patient with history of an inborn error of sugar metabolism most likely has essential fructosuria. This benign, autosomal recessive disorder causes some of the dietary fructose
load to be secreted in the urine unchanged due to defective metabolism by fructokinase. Fructose, similar to glucose and galactose, is a reducing sugar and can be detected by a copper reduction
test, which nonspecifically detects the presence of reducing sugar. A urine dipstick, however, uses glucose oxidase to ascertain the presence of urinary glucose and will not test positive in the
presence of fructose or galactose.
Acid α-glucosidase (or acid maltase) deficiency causes glycogen storage disease type II (Pompe disease). Affected infants have cardiomyopathy, muscle weakness, and hypotonia.
Aldolase B deficiency is a life-threatening disorder caused by the inability to metabolize fructose-1-phosphate (a toxic intermediate that accumulates in cells and depletes intracellular phosphate).
Patients become acutely symptomatic after ingesting fructose-containing foods and eventually develop liver failure. Treatment includes elimination of dietary fructose.
Galactosemia is an autosomal recessive disorder caused by galactose-1-phosphate uridyl transferase deficiency. It is characterized by neonatal jaundice, vomiting, cataract formation, hepatomegaly,
and failure to thrive. Treatment includes elimination of all milk products from the diet and feeding with soy-based infant formula.
Lactase is a mucosal enzyme responsible for the digestion of lactose. Acquired lactase deficiency is the most common cause of selective carbohydrate malabsorption. Patients with lactase
deficiency experience gastrointestinal symptoms (eg, bloating, diarrhea) following the ingestion of dairy products.
The 3 main circulating catecholamines are dopamine, norepinephrine, and epinephrine. Norepinephrine and dopamine are produced in the central as well as the peripheral nervous system, whereas
epinephrine is predominantly produced in the adrenal medulla. The first step in the synthesis of catecholamines is the conversion of tyrosine to dihydroxyphenylalanine (DOPA) by tyrosine
hydroxylase. This is the rate-limiting step in the synthesis of catecholamines. DOPA is converted to dopamine by dopa decarboxylase, which is then converted to norepinephrine by dopamine
beta-hydroxylase. In the adrenal medulla, norepinephrine is rapidly converted to epinephrine by phenylethanolamine-N-methyltransferase (PNMT).
Expression of PNMT in the adrenal medulla is upregulated by cortisol. Because the venous drainage of the adrenal cortex passes through the adrenal medulla, cortisol concentrations in the medulla
can be very high, and PNMT is expressed at a high level. However, following pituitary resection, ACTH secretion and subsequent cortisol production would be low. The result would be decreased
PNMT activity and reduced conversion of norepinephrine to epinephrine.
Catechol-O-methyltransferase (COMT) and monoamine oxidase (MAO) are the enzymes responsible for breakdown of catecholamines. COMT converts epinephrine to metanephrine and
norepinephrine to normetanephrine. MAO converts metanephrine and normetanephrine to vanillylmandelic acid.
Tyrosine required for the synthesis of catecholamines is obtained from either dietary intake or by conversion of phenylalanine by phenylalanine hydroxylase in the liver. Deficiency of this enzyme
causes phenylketonuria.
Hyperparathyroidism & hypoparathyroidism
Hyperparathyroidism (↑ PTH) Hypoparathyroidism (↓ PTH)
↑ Calcium, ↓ phosphate ↓ Calcium, ↑ phosphate
Osteoporosis Tingling, numbness
Nephrolithiasis Trousseau & Chvostek signs
Polydipsia, polyuria Muscle spasms
Constipation Seizures
Bone pain
Muscle pain
This patient has signs of hypocalcemia, including muscle cramps, perioral paresthesias, hypotension, and possible laryngospasm. Other signs of hypocalcemia may include Chvostek sign (facial
muscle contraction elicited by tapping on the facial nerve anterior to the ear) and Trousseau sign (carpopedal spasm triggered by prolonged inflation of a blood pressure cuff around the arm). These
signs of neuromuscular hyperexcitability become clinically apparent with serum calcium levels <7.0 mg/dL.
The most common cause of acute hypocalcemia is injury to the parathyroid glands during thyroid surgery due to direct trauma, devascularization, or inadvertent removal. Other causes include
autoimmune hypoparathyroidism, sepsis, tumor lysis syndrome, acute pancreatitis, and severe vitamin D or magnesium deficiency.
A 1-day-old boy is diagnosed with hyperphenylalanemia by newborn screening. He is placed on a special phenylalanine-restricted diet with tyrosine supplementation. The parents are extensively
counseled on the boy's condition and informed of the necessary dietary restrictions. They are also instructed to return to his physician for regular follow-up visits. Several months later, laboratory test
results indicate that the infant has a normal serum phenylalanine level. Careful examination, however, reveals some neurological abnormalities, including axial hypotonia and microcephaly. Further
workup is notable for elevated prolactin, and his physician suspects a cofactor deficiency. Which of the following enzymes is most likely deficient in this patient?
This patient most likely has a deficiency of dihydrobiopterin reductase based on the combination of hyperphenylalanemia and elevated prolactin.
Phenylalanine is converted to tyrosine by phenylalanine hydroxylase using tetrahydrobiopterin (BH4) as a cofactor. Tyrosine is a nonessential amino acid that becomes essential in phenylketonuria
(PKU). Tyrosine is converted to DOPA via the enzyme tyrosine hydroxylase, which also uses BH4 as a cofactor. Once DOPA is synthesized, it is decarboxylated to dopamine by DOPA decarboxylase.
Dopamine ultimately serves as the precursor molecule to the catecholamines epinephrine and norepinephrine.
In classic PKU, supplementation of tyrosine allows for normal catecholamine production due to intact function of tyrosine hydroxylase. Deficiency of dihydrobiopterin reductase, however, leads to
hyperphenylalanemia from impaired phenylalanine hydroxylase activity and low dopamine levels from impaired tyrosine hydroxylase activity.
Disorders involving impaired BH4 levels account for 2% of hyperphenylalanemia cases, and the most common cause is deficiency of dihydrobiopterin reductase, the enzyme responsible for reduction
of dihydrobiopterin (BH2) to BH4. Although phenylalanine levels can be controlled by dietary restriction, downstream deficiencies of neurotransmitters (eg, dopamine, norepinephrine, epinephrine,
serotonin) lead to progressive neurologic deterioration in these patients. Normally, dopamine from the tuberoinfundibular system tonically inhibits prolactin release. Decreased BH4 causes lower
levels of dopamine, which lead to increased prolactin levels. This pathophysiology is similar to the effects of bromocriptine, a dopamine agonist that is used to treat hyperprolactinemia.
A 56-year-old man is evaluated for progressive visual impairment. The patient works as part of the grounds crew at an airport, and says he has trouble identifying aircraft at a distance and with
filling out paperwork at the end of his shift. His medical history includes poorly controlled diabetes mellitus, hypertension, and gout. A year ago, the patient underwent an uncomplicated repair of a
right inguinal hernia. Physical examination shows bilateral clouding of the lens. The remainder of the examination is unremarkable. Which of the following metabolic conversions is most likely
contributing to this patient's current condition?
This patient has cataracts, an opacification of the lens of the eye that can lead to blindness, likely a result of long-standing hyperglycemia due to poorly controlled diabetes mellitus. Certain cells (eg,
retinal, endothelial, lens, renal mesangial, Schwann) are more vulnerable to hyperglycemia-induced damage because they are unable to regulate glucose transport when circulating levels are high.
Multiple metabolic pathways are involved in the pathogenesis of hyperglycemia-induced tissue damage:
Advanced glycosylation end-products (AGEs): Glucose can nonenzymatically attach to proteins and lipids, forming reversible glycosylation products that slowly stabilize into irreversible
products. Under hyperglycemic conditions, AGEs accumulate and facilitate deposition of LDL in blood vessel walls and inflammatory cell invasion that causes atherosclerosis and
microangiopathic complications. High glucose levels in the aqueous humor may also induce nonenzymatic glycation of lens proteins, which contributes to cataract formation.
Polyol pathway overactivity: The enzyme aldose reductase converts glucose to sorbitol, which is then oxidized to fructose by the enzyme sorbitol dehydrogenase. With hyperglycemia, formation
of sorbitol occurs faster than its metabolism to fructose, resulting in its accumulation. Sorbitol increases the osmotic pressure in tissues and stimulates the influx of water, leading to osmotic cellular
injury. In addition, oxidative stress resulting from the depletion of NADPH (aldose reductase consumes NADPH) also contributes to cataract formation and other diabetic complications such as
retinopathy, peripheral neuropathy, and nephropathy. Loss of red reflex.
Gynecomastia
Clinical findings Development of glandular breast tissue in males
Pathophysiology Increased estrogen to androgen ratio
Ductal epithelial hyperplasia & stromal fibrosis
Common etiologies Increased estrogen levels (eg, cirrhosis, obesity)
Decreased testosterone levels (eg, chronic kidney disease, hypogonadism)
Medication effect
Decreased androgen production (eg, GnRH agonists, ketoconazole)
Decreased conversion to dihydrotestosterone (eg, 5-α reductase inhibitors)
Inhibition of androgen receptors (eg, spironolactone, bicalutamide)
Gynecomastia is the development of glandular breast tissue in males. It is characterized by ductal epithelial hyperplasia with fibrosis of the surrounding stroma. Breast growth is inhibited by
androgens and promoted by estrogens; conditions that increase the estrogen to androgen ratio can lead to gynecomastia. Common pathologic causes include cirrhosis (increased aromatase
activity, decreased clearance of estrogens), end-stage renal disease (decreased testosterone production), and medications (eg, spironolactone, ketoconazole).
Men with prostate cancer who receive androgen-deprivation therapy (eg, orchiectomy, long-acting GnRH agonists, androgen receptor inhibitors) can develop gynecomastia due to dramatic (>95%)
reductions in circulating testosterone (with lesser reductions in estrogens). Treatment with tamoxifen, a selective estrogen receptor modulator that acts as an estrogen antagonist in the breast, can
reduce the risk of gynecomastia in these patients.
A 4-month-old boy is brought to the office for his first visit since arriving in the United States. The patient was recently adopted, and his adoptive mother says the boy is tremulous compared to her
biological children. Over the past week, the boy has also had episodes of upward eye deviation and bilateral arm and leg shaking for approximately 2 minutes at a time. Biological family history is
not available. His temperature is 36.7 C (98.1 F), blood pressure is 90/40 mm Hg, pulse is 120/min, and respirations are 30/min. Examination shows a fair-skinned infant with blue eyes and a musty
body odor. Which of the following amino acids is most likely essential in this patient?
This patient's clinical presentation suggests phenylketonuria (PKU). Classic PKU (the most common form) occurs most frequently in persons of Scandinavian descent. Individuals who are
homozygous for this autosomal recessive disorder have a severe deficiency of phenylalanine hydroxylase, the enzyme responsible for conversion of phenylalanine to tyrosine. Tyrosine becomes
an essential amino acid in these patients as it cannot be synthesized from phenylalanine, although most patients receive adequate amounts in their diet and do not require supplementation.
Furthermore, the excess phenylalanine inhibits tyrosinase, which normally results in the downstream production of melanin. The lack of melanin causes the fair complexion seen in this patient.
Although development is initially normal, most untreated patients develop intellectual disability by age 6 months. Other classic findings include seizures, eczema, light hair/skin pigmentation, and a
"musty," odor. However, cognitive impairment can be lessened by early detection (newborn screening) and restriction of phenylalanine intake.
Cystinuria is due to impaired transport of renal cystine (a homodimer of cysteine), which leads to cystine renal stone formation. Clinical manifestations typically include flank pain, hematuria, and
possible stone passage in children or adolescents.
The branched-chain amino acids (leucine, isoleucine, valine) are elevated in maple syrup urine disease, an amino acid disorder marked by deficiency of branched-chain alpha-ketoacid dehydrogenase
complex. Buildup of the branched-chain amino acids and their metabolites is toxic, leading to feeding difficulties, seizures, cerebral edema, and a sweet odor of the urine.
Glucagon exerts its effects through G protein-coupled receptors using the adenylate cyclase second messenger system. G protein is a heterotrimer consisting of alpha, beta, and gamma subunits
associated with the intracellular domain of these transmembrane receptors. The alpha subunit of the inactivated G protein is bound to GDP. On receptor activation, the alpha subunit undergoes a
conformational change, which releases GDP and binds GTP. GTP binding allows the alpha subunit to dissociate from the remainder of the G protein complex.
There are multiple subtypes of alpha G proteins, each with different secondary effects. A specific alpha subunit known as Gs (present in glucagon, TSH, and PTH receptor complexes) activates
adenylate cyclase when released from the G protein complex. Adenylate cyclase converts ATP to cAMP, which activates protein kinase A. Protein kinase A phosphorylates specific
serine/threonine residues in various enzymes, leading to their activation or deactivation. Protein kinase A also phosphorylates proteins that bind to the regulatory regions of genes on DNA.
A 3-day-old boy is brought to the office due to poor feeding, vomiting, and progressive lethargy. The parents also report that his diapers have a "burnt sugar smell" differing from their previous
children's diapers. The mother and infant were discharged from the hospital yesterday after a normal pregnancy and spontaneous vaginal delivery. The mother is exclusively breastfeeding. Her other
2 children are healthy and have no medical problems. Physical examination shows a lethargic infant with dry mucous membranes and generalized hypertonia. Which of the following should be
restricted from this infant's diet?
This infant has symptoms typical of maple syrup urine disease (MSUD), an autosomal recessive inborn error of metabolism due to branched-chain α-ketoacid dehydrogenase complex (BCKDC)
deficiency. This enzyme normally allows for the breakdown of leucine, isoleucine, and valine into substrates for entry into the TCA cycle.
BCKDC deficiency is neurotoxic primarily due to elevated levels of leucine. Infants present in the first few days of life with progressive irritability, poor feeding, lethargy, and increased muscle tone.
The urine characteristically has a sweet, "maple syrup" odor. Diagnosis can be confirmed by the presence of elevated branched-chain amino acid levels. Therapy consists of dietary restriction
of branched-chain amino acids, but patients remain at lifelong risk for neurotoxicity in the setting of intercurrent illnesses and fasting.
Galactosemia is an autosomal recessive disorder due to galactose-1-phosphate uridyltransferase deficiency. The buildup of galactose (normally found in breast milk and regular infant formula) leads
to neonatal jaundice, cataracts, hepatomegaly, and frequently Escherichia coli sepsis. Dietary restriction of galactose is the mainstay of treatment.
Homocystinuria is an autosomal recessive disorder marked by a defect in cystathionine β-synthase, resulting in elevated levels of homocysteine and methionine. Restriction of methionine for these
patients is one aspect of therapy.
Phenylketonuria is an autosomal recessive disorder characterized by phenylalanine hydroxylase deficiency, leading to hyperphenylalaninemia. Untreated patients develop intellectual disability,
seizures, decreased hair/skin pigmentation, and a "musty" odor.
Dietary tyrosine restriction may be beneficial for patients with hypertyrosinemia (progressive liver and renal disease) or alkaptonuria (pigmented osteoarthritis).
This patient's pathologic specimen shows normal thyroid follicles containing colloid, consistent with a lingual thyroid. The thyroid gland is formed from an outpouching (evagination) of the pharyngeal
epithelium and subsequently descends to the lower neck anterior to the upper trachea and larynx. The lowest part of the evagination forms the thyroid gland and the remaining portion forms the
thyroglossal duct, which extends from the foramen cecum on the dorsal surface of the tongue to the superior border of the thyroid isthmus.
Due to failure of migration, the thyroid can reside anywhere along the thyroglossal duct's usual path, including the tongue (lingual thyroid). Enlargement of a lingual thyroid can lead to obstructive
symptoms (eg, dysphagia, dysphonia, dyspnea), typically during times of heightened thyroid stimulation (eg, puberty, pregnancy). Sometimes, this lingual thyroid is the only thyroid tissue in the body,
so significant hypothyroidism occurs if it is removed.
The lesion pictured is a xanthelasma, a type of xanthoma usually found on the medial eyelids. Hyperlipidemia
and/or dyslipidemia can result in xanthomas (including xanthelasmas). Xanthelasmas are dermal accumulations
of benign-appearing macrophages with abundant, finely vacuolated (foamy) cytoplasm containing cholesterol
(free and esterified), phospholipids, and triglycerides. Due in part to insulin resistance promoting increased
VLDL production, diabetics may develop a secondary Type IV or V hyperlipidemia (increased VLDL,
chylomicrons) and/or a secondary diabetic dyslipidemia with elevated LDL cholesterol and low HDL
cholesterol. Thus, in order to determine the type of this patient's lipid disorder and to rule out underlying
diabetes, her serum lipids and blood glucose should be measured.
Niemann-Pick disease is an autosomal recessive disorder common among
Ashkenazi Jews and is characterized by sphingomyelinase deficiency.
Sphingomyelinase is responsible for the breakdown of sphingomyelin, a lipid
constituent of cell membranes. In Niemann-Pick disease, sphingomyelin
accumulation within lysosomes results in cells that appear enlarged, foamy, and
vacuolated on electron microscopy. These lipid-laden foam cells (black arrows)
accumulate in the liver and spleen and cause hepatosplenomegaly.
Progressive neuronal accumulation is responsible for hypotonia and neurologic
degeneration (eg, failure to progress developmentally, loss of milestones).
Retinal accumulation leads to a cherry-red macular spot (blue arrow).
This patient presents with the classic infantile type A variant that results in
hepatosplenomegaly, progressive neurologic deterioration, and death by age 3
years.
In patients with metachromatic leukodystrophy, central nervous system accumulation of cerebroside sulfate is caused by arylsulfatase A deficiency. Central and peripheral demyelination leads
to peripheral neuropathy and ataxia.
In Krabbe disease, galactocerebrosidase deficiency causes accumulation of galactocerebroside and psychosine. Infants have developmental delay and/or regression, hypotonia, optic atrophy,
and seizures.
In Fabry disease, α-galactosidase A deficiency causes globotriaosylceramide (ceramide trihexoside) accumulation. Clinical manifestations begin in childhood with neuropathic pain and
dermatologic pathology (eg, telangiectasias, angiokeratomas).
Glucocerebroside accumulation occurs in Gaucher disease, an autosomal recessive disorder of β-glucocerebrosidase deficiency. Patients typically have hepatosplenomegaly, pancytopenia,
and skeletal problems.
Patients with Tay-Sachs disease are deficient in β-hexosaminidase A, which leads to GM2 accumulation in neurons. Neurologic regression and cherry-red macular spots are classic symptoms
(similar to Niemann-Pick disease), but hepatosplenomegaly is absent.
Congenital adrenal hyperplasia (CAH) refers to a group of autosomal recessive disorders that result from defects in the enzymes involved in cortisol biosynthesis. Deficiency of 21-hydroxylase is the
most common cause of CAH, accounting for 90% of all cases. In 21-hydroxylase deficiency, the adrenal gland cannot synthesize aldosterone and cortisol efficiently. This causes increased production
of adrenal androgens because the accumulating cortisol and aldosterone precursors are diverted toward adrenal androgen biosynthesis. The resulting low cortisol levels stimulate pituitary production
of ACTH, which further increases the production of adrenal androgens. 21-hydroxylase deficiency also causes increased serum levels of 17-hydroxyprogesterone as its conversion to 11-deoxycortisol
is impaired by the enzymatic defect.
Increased androgen levels lead to ambiguous genitalia in females (virilization), but males will have normal genitalia. Salt-wasting occurs with more severe enzymatic deficiencies due to lack of
sufficient amounts of mineralocorticoids and presents with vomiting, hypotension, hyponatremia, and hyperkalemia. Severe enzymatic defects can also result in significant cortisol deficiency, which
can cause hypoglycemia and further impair blood pressure maintenance (leading to circulatory collapse).
Typical symptoms of hypoglycemia (eg, disorientation, sweating, tremors, palpitations), which are relieved by intake of glucose. The 3 most important predisposing factors for hypoglycemia in
patients with type 1 diabetes are excessive insulin dose, inadequate food intake, and physical activity/exercise.
Glucose uptake by skeletal muscle cells is mediated by glucose transporter type 4 (GLUT-4). GLUT-4 is translocated to cell membranes and transverse tubules (deep invaginations in the cell
membrane) in response to insulin. GLUT-4 translocation also occurs during muscle contraction by an insulin-independent mechanism, which is mediated by several cellular factors, including AMP-
activated kinase, nitric oxide, and calcium-calmodulin-activated protein kinase.
In normal individuals, overt hypoglycemia does not occur with exercise because a drop in blood glucose will stop insulin release from the beta cells and counter-regulatory hormones (eg, glucagon) will
increase endogenous glucose production via glycogenolysis and gluconeogenesis. However, patients taking exogenous insulin are vulnerable to exercise-induced hypoglycemia as insulin will
continue to be released from the injection site despite falling glucose levels. In addition, strenuous exercise may cause changes in skin perfusion that can lead to increased insulin absorption
(especially if the insulin is injected into an exercising limb rather than the abdominal area).
A 34-year-old man comes to the office due to oral and perioral nodules. The nodules appeared several months ago, and the patient reports that they are similar to other lesions that were removed
10 years earlier. He has a history of total thyroidectomy 5 years ago following the discovery of a palpable thyroid mass. On examination, the patient is tall and slender with disproportionately long
arms and legs. His fingers are also long and thin. Oral inspection shows several small, flesh-colored nodules on his lips and tongue. This patient most likely suffers from which of the following
conditions?
This patient has a marfanoid habitus – tall and slender build with disproportionately long arms, legs, and fingers. The flesh-colored nodules on his lips and tongue are likely mucosal neuromas,
which are unencapsulated, thickened proliferations of neural tissue. This combination of clinical findings is consistent with multiple endocrine neoplasia type 2B (MEN2B), which is due to an
inherited mutation in the RET proto-oncogene.
This patient also has a history of total thyroidectomy, which was likely due to medullary thyroid cancer (MTC) (benign thyroid masses are usually treated medically or with partial thyroidectomy).
Early recognition of MEN2B is important as almost all patients will develop MTC and prophylactic thyroidectomy can be life-saving. Other possible manifestations of MEN2B include
pheochromocytoma and intestinal ganglioneuromas (often causing associated constipation).
Neurofibromatosis type 1 is characterized by café-au-lait spots, cutaneous neurofibromas, axillary or inguinal freckling, optic glioma, iris hamartomas, and osseous lesions.
Neurofibromatosis type 2 (the more "central" form) is characterized by bilateral acoustic neuromas, brain meningiomas, and schwannomas of the dorsal roots in the spinal cord. Although this
patient has (mucosal) neuromas, the remainder of his presentation is more consistent with MEN2B.
A 54-year-old male has a palpable neck lump determined to be a 'cold' thyroid nodule on a thyroid scan. Fine-needle aspiration of the nodule shows spindle-shaped cells in an amorphous
background. The patient's serum calcitonin level is elevated. Which of the following gene changes is most likely responsible?
Medullary thyroid cancers are tumors of parafollicular calcitonin-secreting C-cells. 80% of medullary thyroid cancers are sporadic and 20% are familial (as in the MEN type 2 syndrome). Germline
mutations of the RET proto-oncogene are present in more than 95% of patients with familial medullary thyroid cancer. The RET proto-oncogene codes for a membrane-bound tyrosine kinase receptor
involved in cell cycle regulation. RET proto-oncogene mutations are also commonly found in sporadic medullary thyroid cancers.
This patient has new-onset type 2 diabetes mellitus (T2DM), which results from a combination of insulin resistance and relative insulin deficiency. The early course of T2DM is characterized by
increased insulin production and decreased sensitivity of target organs to the effects of insulin, although insulin levels may later decline as the disease progresses. In addition, this patient has
acanthosis nigricans, which is another sign of insulin resistance.
Insulin resistance in adipose cells hinders the antilipolytic effects of insulin, leading to lipolysis and release of free fatty acids. In turn, chronically elevated free fatty acid levels contribute to insulin
resistance by impairing insulin-dependent glucose uptake and increasing hepatic gluconeogenesis. Other factors that contribute to insulin resistance include obesity and a sedentary lifestyle.
Patients with chronic alcoholism are frequently deficient in thiamine, a necessary cofactor for pyruvate dehydrogenase, α-ketoglutarate dehydrogenase, and transketolase. Administration of
glucose to thiamine-deficient patients can cause rapid depletion of the small amount of thiamine remaining in the circulation. This can result in neuronal injury within highly metabolic brain regions,
leading to acute Wernicke encephalopathy.
Wernicke encephalopathy
Associated conditions Chronic alcoholism (most common)
Malnutrition (eg, anorexia nervosa)
Hyperemesis gravidarum
Pathophysiology Thiamine deficiency
Clinical features Encephalopathy
Oculomotor dysfunction (eg, horizontal nystagmus,
bilateral abducens palsy)
Postural & gait ataxia
Treatment Intravenous thiamine followed by glucose infusion
The metabolism of ethanol by alcohol dehydrogenase and aldehyde dehydrogenase consumes NAD+ and increases the NADH to NAD+ ratio. This skewed ratio inhibits all pathways requiring NAD+;
as a result, the entire citric acid cycle is inhibited. However, in the setting of Wernicke encephalopathy, thiamine-dependent enzymes are especially affected due to the lack of NAD+ and thiamine.
A 45-year-old man comes to the office with hoarseness that began 1 week ago. Physical examination shows a large nodular goiter. Fine-needle aspiration biopsy is diagnostic for papillary thyroid
cancer, and the patient is admitted to the hospital for thyroidectomy. On the second postoperative day, he develops muscle cramps in his legs and paresthesias in his fingers and around his lips.
Muscle strength and deep tendon reflexes are normal, but he has twitching of his lower facial muscles on percussion below the zygomatic arch. Which of the following is the most likely cause of this
patient's current symptoms?
Two hormones largely regulate calcium and phosphate homeostasis: parathyroid hormone (PTH), which regulates the minute-to-minute concentrations, and calcitriol, which regulates levels over the
longer term. PTH is a polypeptide hormone produced by the chief cells of the parathyroid glands in response to hypocalcemia and has 3 primary effects:
Increases osteoclastic bone resorption, which releases calcium and phosphate into the circulation
Increases renal calcium reabsorption and reduces phosphate reabsorption
Increases formation of 1,25-dihydroxycholecalciferol (by upregulating renal 1-alpha-hydroxylase), which increases intestinal calcium and phosphate absorption
This patient has symptomatic hypoparathyroidism following thyroid surgery. Postoperative hypoparathyroidism is common in patients who undergo thyroidectomy for thyroid cancer and can be due to
inadvertent surgical removal of or damage to the parathyroid glands. The immediate drop in PTH levels results in decreased calcium and phosphate release from bone and decreased calcium
reabsorption by the kidneys. Inadequate PTH also reduces phosphate excretion by the kidneys and decreases the conversion of calcidiol (25-hydroxycholecalciferol) to calcitriol (1,25-
dihydroxycholecalciferol) in the renal tubular cells. This, in turn, decreases intestinal absorption of calcium and phosphate and lowers total body calcium stores.
Hyperparathyroidism & hypoparathyroidism
Hyperparathyroidism Hypoparathyroidism
↑ Calcium, ↓ phosphate ↓ Calcium, ↑ phosphate
Osteoporosis Tingling, numbness
Nephrolithiasis Trousseau & Chvostek signs
Polydipsia, polyuria Muscle spasms
Constipation Seizures
Bone pain
Muscle pain
Insulin, a polypeptide hormone synthesized by pancreatic beta cells, is released in response to elevated glucose levels. Insulin mRNA codes for preproinsulin, a larger precursor molecule that begins
with a hydrophobic N-terminal signal peptide. Shortly after translation begins, this signal sequence interacts with cytosolic signal recognition peptide, which halts protein synthesis until the ribosome
translocates to the rough endoplasmic reticulum (RER). Once bound to the RER, translation resumes and the growing peptide chain is extruded into the RER. The N-terminal signal peptide is then
cleaved from preproinsulin to yield proinsulin.
Proinsulin undergoes conformational changes and the addition of 3 disulfide bonds in the RER. Proinsulin is then transported to the Golgi apparatus, where it is packed into secretory granules.
Endopeptidases in the secretory granules cleave proinsulin into insulin and C-peptide, which are then stored within the granules until they are secreted from the cell via exocytosis.
Exogenous insulin administered to patients with diabetes does not contain C-peptide. However, C-peptide released from beta cells remains in the circulation with a half-life of approximately 35
minutes and can be assayed as a surrogate marker for endogenous insulin production.
Most proteins destined for the extracellular space have a signaling sequence that directs them to the RER/Golgi apparatus, where they are packaged into secretory vesicles. However, a few proteins,
such as interleukin-1, lack a signaling sequence and are secreted directly from the cytoplasm via an unconventional mechanism.
Diabetic ketoacidosis is a condition that most commonly affects patients with type 1 diabetes mellitus due to their absolute insulin deficiency. Type 1 diabetes mellitus occurs in genetically
susceptible individuals who are exposed to triggering environmental factors (eg, viral infections, environmental toxins, dietary components). This results in an autoimmune response against
pancreatic beta cells that leads to progressive loss of beta cell mass. Overt manifestations of diabetes mellitus tend to develop once >90% of beta cells are destroyed. Although antibodies against
islet antigens are detected in a large number of patients, they are thought to play a permissive role in disease pathogenesis; the destruction of beta cells occurs primarily through cell-mediated
immunity. Infiltration of islets by inflammatory cells is called insulitis and is more prominent during the early stages of disease.
Thiazide diuretics (eg, chlorthalidone, hydrochlorothiazide) are some of the most common agents used for treatment of primary hypertension. The use of high-dose thiazides is associated with a
variety of metabolic and electrolyte complications, including hypercalcemia, hyperglycemia, hypercholesterolemia, hyperuricemia, hyponatremia, and hypokalemia. However, the incidence of these
side effects is relatively low and generally only 1 or 2 will develop in any particular patient.
Thiazide diuretics inhibit the Na+/Cl- cotransporter in the distal tubule, leading to increased excretion of Na+and H2O as well as K+ and H+ ions. This also increases distal tubular Ca2+
reabsorption, which causes both hypercalcemia and hypocalciuria. The increase in serum Ca2+ will result in appropriate suppression of parathyroid hormone (PTH) levels.
Familial hypocalciuric hypercalcemia (FHH) is a benign autosomal dominant disorder caused by defective Ca2+-sensing by parathyroid and renal tubule cells. This defect prevents PTH from being
suppressed in response to an increase in serum Ca2+, resulting in hypercalcemia with normal-to-high serum PTH levels. Although both FHH and primary hyperparathyroidism present with elevated
Ca2+ and PTH levels, FHH will also have low urinary Ca2+ excretion (ie, hypocalciuria) due to impaired renal Ca2+ sensing.
A 50-year-old man comes to the emergency department with a sudden, severe headache. He also complains of mild headaches and decreased libido over the last few months. Physical examination
reveals bilateral deficits involving the temporal visual fields and impaired extraocular eye movements. Shortly after being admitted to the hospital, he becomes severely hypotensive and loses
consciousness. The patient dies despite aggressive resuscitation efforts. Which of the following findings would most likely be seen on autopsy?
Features of pituitary apoplexy
Pathogenesis Acute intrapituitary hemorrhage (occurs most often in patients with preexisting adenoma)
Presentation Severe headache
Bitemporal hemianopsia
Ophthalmoplegia
Panhypopituitarism
Diagnosis Neuroimaging shows pituitary enlargement & signs of hemorrhage
Treatment Glucocorticoid replacement (critical to prevent life-threatening hypotension)
Surgical decompression to treat persistent visual & oculomotor symptoms
This patient most likely developed pituitary apoplexy (acute hemorrhage into the pituitary gland), which occurs most often in patients with preexisting pituitary adenomas. Typically, chronic
symptoms related to the pituitary tumor (eg, headaches, decreased libido) are present for months before the actual hemorrhage event. The bleeding often presents acutely with severe headache and
visual disturbances. Signs of meningeal irritation can also be seen and mimic subarachnoid hemorrhage. However, subarachnoid hemorrhage can be differentiated from a sellar mass with suprasellar
extension by the presence of bitemporal hemianopsia, which is present only in the latter. Patients with pituitary apoplexy can develop cardiovascular collapse due to ACTH deficiency and
subsequent adrenocortical insufficiency. Pituitary apoplexy is a medical emergency that requires urgent neurosurgical consultation and treatment with glucocorticoids.
A 31-year-old previously healthy man comes to the office due to myalgias, anorexia, and skin rash. He does not use tobacco, alcohol, or illicit drugs. The patient works as a personal trainer and is a
bodybuilding enthusiast. He denies using anabolic steroids but has been consuming large amounts of raw egg whites for the past several months. Physical examination shows macular
dermatitis of the extremities. A water-soluble vitamin deficiency is suspected as the cause of his condition. Which of the following biochemical conversions most likely uses the deficient vitamin as
a cofactor?
Biotin (vitamin B7) is an important cofactor for several carboxylase enzymes. It functions as a CO2 carrier and plays an essential role in carbohydrate, lipid, and amino acid metabolism. In the liver,
the conversion of pyruvate to oxaloacetate for gluconeogenesis requires pyruvate carboxylase and biotin.
Biotin deficiency is rare but can occur secondary to poor diet, excessive raw egg white consumption (due to high levels of biotin-binding avidin in egg whites), and congenital disorders of biotin
metabolism. Patients with biotin deficiency present with nonspecific symptoms, including changes in mental status, myalgias, anorexia, and chronic dermatologic changes such as macular
dermatitis. Biotin-deficient individuals can also develop metabolic acidosis as a result of increased conversion of pyruvate to lactic acid.
Niacin (vitamin B3), in the form of NADP+, is used to oxidize glucose-6-phosphate in the pentose phosphate pathway, generating ribose-5-phosphate and NADPH in the process.
Thiamine (vitamin B1), riboflavin (vitamin B2), niacin (vitamin B3), pantothenic acid (vitamin B5), and lipoic acid are the 5 cofactors required by the mitochondrial enzyme complex pyruvate
dehydrogenase. In their absence, the metabolism of pyruvate to acetyl-CoA is not possible.
Pyridoxal phosphate (vitamin B6) acts as a cofactor for alanine transaminase, which catalyzes the reversible reaction between pyruvate and glutamate to alanine and alpha-ketoglutarate in the liver
and muscle tissue.
Production of oxaloacetate from succinate in the TCA cycle requires 2 enzymes (succinate dehydrogenase and malate dehydrogenase), along with riboflavin (vitamin B2) and niacin (vitamin B3) in the
forms of cofactors FAD+ and NAD+, respectively.
A 34-year-old man comes to the office due to excessive thirst and frequent urination. Several years ago, he developed similar symptoms after prolonged hospitalization for multiple injuries due to a
motorcycle collision. The symptoms resolved after the appropriate therapy was started, and the patient had been compliant until he ran out of his prescribed medication a week ago while vacationing
in Europe. His urinary osmolality after 2 hours of water restriction is 250 mOsm/L, and it increases to 700 mOsm/L after administering antidiuretic hormone. The persistence of this patient's condition
is most likely explained by direct damage to which of the following structures?
This patient has diabetes insipidus (DI), a disease characterized by polyuria (excessive urination) and polydipsia (excessive thirst). These symptoms occur due to impaired antidiuretic hormone
(ADH) activity and the resulting production of large volumes of very dilute urine. DI can be due to deficient ADH production (central) or resistance to ADH in the kidneys (nephrogenic). Injection of
exogenous ADH can distinguish between central and nephrogenic DI: ADH increases urine osmolality in patients with central DI, whereas patients with nephrogenic DI have no significant change in
urine osmolality after ADH administration.
ADH is synthesized in the paraventricular and supraoptic nuclei of the hypothalamus. After synthesis, ADH is transported to the posterior pituitary for storage and later release into the circulation.
Head trauma, neurosurgery (eg, transsphenoidal), and tumors (eg, craniopharyngioma) can lead to injury of the hypothalamus and posterior pituitary. Isolated posterior pituitary/infundibular injury may
cause transient central DI as the hypothalamic nuclei are intact and axonal regeneration and hypertrophy can allow adequate ADH release into the circulation. However, damage to the hypothalamic
nuclei results in loss of vasopressinergic neurons, which often leads to permanent central DI. Other features of hypothalamic injury may include autonomic dysfunction, temperature dysregulation,
and eating disorders.
Features of glucagonoma
Clinical presentation Necrolytic migratory erythema
Erythematous papules/plaques on face, perineum & extremities
Lesions enlarge & coalesce, leaving a central indurated area with peripheral blistering & scaling
Diabetes mellitus/hyperglycemia
Gastrointestinal symptoms (diarrhea, anorexia, abdominal pain)
Diagnosis Markedly elevated glucagon levels
Glucagonoma, a rare tumor arising from the alpha cells of the pancreatic islets of Langerhans. Glucagonomas secrete large quantities of glucagon, so affected patients often have hyperglycemia or
overt diabetes mellitus. A characteristic skin finding is necrolytic migratory erythema, an elevated painful and pruritic rash typically affecting the face, groin, and extremities. Over time, small
erythematous papules coalesce to form large, indurated plaques with a central clearing that often appears brown or bronze-colored. Diagnosis is made by detecting elevated levels of glucagon in the
serum.
A 5-month-old boy is brought to the office due to poor feeding. His mother says that he has difficulty holding his head up while breastfeeding and his suckling seems weaker than it used to be. His
current weight is between the 5th-10th percentile, and length and head circumference are tracking along the 25th percentile. Physical examination shows hepatomegaly and hypotonia in all 4 limbs.
Cardiac auscultation reveals a gallop rhythm, and chest x-ray shows severe cardiomegaly. Muscle biopsy shows enlarged lysosomes containing periodic acid-Schiff (PAS)-positive material. Which of
the following enzymes is most likely deficient in this patient?
This patient most likely has glycogen storage disease type II (Pompe disease). This condition is caused by deficiency of acid α-glucosidase (acid maltase), an enzyme responsible for breaking down
glycogen within the acidic environment of lysosomes. Although most glycogen is degraded in the cytoplasm, a small amount is inadvertently engulfed by lysosomes, especially in cells containing high
amounts of glycogen such as hepatocytes and myocytes. As such, deficiency of acid maltase results in pathologic accumulation of glycogen within liver and muscle lysosomes. Cardiac and skeletal
muscle are particularly susceptible, as the ballooning lysosomes interfere with contractile function.
The classic form of the disease presents in early infancy with marked cardiomegaly, severe generalized hypotonia, macroglossia, and hepatomegaly. Blood glucose levels are normal, unlike with
glycogen storage diseases that primarily affect the liver (eg, von Gierke). A key distinguishing feature is that muscle biopsy will show accumulation of glycogen in lysosomes.
A 2-month-old boy is brought to the emergency department due to progressively worsening "floppiness" and poor feeding. The infant was born in Eastern Europe via an uncomplicated vaginal
delivery to a 38-year-old woman and then immigrated to the United States with his family. The parents describe the infant as a "good baby" who rarely cries and sleeps through the night but has lately
been difficult to rouse for breastfeeding. Stools have also decreased to every other day and are small and pellet-like. Physical examination shows a hypotonic infant with a large anterior fontanelle,
large tongue, and a reducible umbilical hernia. He has low tone and is unable to hold his head erect on his own. No other abnormalities are seen. Which of the following is the most likely cause of
this patient's condition?
Congenital hypothyroidism is one of the most common causes of preventable intellectual disability. Most cases are due to thyroid dysgenesis (agenesis, hypoplasia, or ectopy), and iodine
deficiency is a common cause in areas endemic for iodine deficiency (eg, Europe).
Neonates initially have no significant symptoms due to the presence of maternal thyroxine (T4) from transplacental transfer. T4 is responsible for the stimulation of protein synthesis as well as
carbohydrate and lipid catabolism in many cells; as maternal T4 wanes, metabolism is impaired and marked by a slowing of physical and mental activity (lethargy, poor feeding, constipation,
hypotonia). Accumulation of matrix substances cutaneously and internally results in nonpitting edema (eg, "puffy" face), umbilical hernia, protruding tongue, and a large anterior fontanelle. In addition,
T4 is essential for normal brain development and myelination during early life, and infants are at risk of severe and irreversible intellectual disability.
Treatment with levothyroxine by age 2 weeks can normalize cognitive and physical development.
The combination of hyponatremia and a lung mass is suggestive of the syndrome of inappropriate antidiuretic hormone secretion (SIADH). ADH is normally produced in the hypothalamus and
secreted from the posterior pituitary in response to changes in plasma osmolality and intravascular volume. However, small cell lung carcinomas, which are tumors of neuroendocrine origin, often
release ADH independent of feedback inhibition (paraneoplastic effect). This inappropriate secretion of ADH leads to hyponatremia, decreased plasma osmolality, and elevated urine osmolality (which
normally should be <100 mOsm/kg given the degree of hyponatremia). The profound hyponatremia that occurs in SIADH can cause headache, weakness, altered mental status, and seizures.
In SIADH, increased ADH causes excessive water absorption by the kidneys, leading to a transient, subclinical hypervolemia. This mild increase in extracellular fluid volume suppresses the renin-
aldosterone axis and stimulates the production of natriuretic peptides, leading to excretion of sodium in the urine (natriuresis). As a result, patients with SIADH have a clinically normal extracellular fluid
volume and low plasma osmolality (euvolemic hyponatremia). Features of volume overload (eg, peripheral edema, pulmonary crackles, elevated jugular venous pressure) are not seen.
Patients with SIADH have inappropriately concentrated urine (generally >100 mOsm/kg) for their degree of hyponatremia. Hyponatremia with a urine osmolality of <100 mOsm/kg (maximally dilute
urine) indicates appropriate suppression of ADH secretion (as would be seen in primary polydipsia).
This patient has primary hyperthyroidism with an elevated thyroxine (T4) and suppressed TSH level. In light of her diffuse goiter, this is likely due to Graves disease. Hyperthyroidism causes
upregulation of beta-adrenergic receptor expression, leading to increased catecholamine effect manifesting as hypertension, palpitations/tachycardia, heat intolerance, tremor, and hyperreflexia.
Beta blockers (eg, propranolol) are used to blunt the adrenergic manifestations of hyperthyroidism while awaiting definitive management (eg, surgery, radioiodine). In addition, lipid-soluble beta
blockers (including propranolol) reduce conversion of T4 to triiodothyronine (T3), the more active form of thyroid hormone, by inhibiting 5'-monodeiodinase in peripheral tissues. Peripheral conversion
of T4 to T3 is also decreased by glucocorticoids and propylthiouracil.
Pulsatile secretion of gonadotrophin-releasing hormone (GnRH) from the hypothalamus
stimulates the release of follicle-stimulating hormone (FSH) and luteinizing hormone (LH). Both
FSH and LH are produced by the gonadotroph cells of the anterior pituitary. LH stimulates the
release of testosterone from the Leydig cells of the testes; FSH stimulates the release of inhibin
B from the Sertoli cells of the testes. Testosterone has a negative feedback effect on LH and
GnRH secretion, and inhibin B suppresses FSH secretion.
Sertoli cells are present within the seminiferous tubules of the testes. In patients with 1 testicle,
the mass of Sertoli cells is significantly reduced. Therefore, the circulating levels of inhibin B
are likely to be low in these patients. Low inhibin B levels will not provide adequate negative
feedback on FSH secretion, thus FSH levels will tend to be elevated in males who only
have 1 testicle.
Pulsatile secretion of gonadotrophin-releasing hormone from the hypothalamus stimulates the
release of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) from the gonadotroph
cells in the anterior pituitary. LH stimulates the release of testosterone from the Leydig cells in
the interstitium of the testicles, and FSH stimulates the release of inhibin B from the Sertoli cells
in the seminiferous tubules of the testicles. Testosterone and inhibin B induce negative
feedback on LH and FSH production, respectively.
FSH also stimulates the Sertoli cells to produce androgen-binding protein locally, within the
seminiferous tubules. This androgen-binding protein is responsible for the high local
testosterone concentration and is different from sex hormone-binding globulin, which is found
in the blood. High local levels of testosterone and FSH are necessary for spermatogenesis.
Defective FSH receptors will prevent spermatogenesis and cause low inhibin B levels, because
FSH is responsible for both spermatogenesis and inhibin B production.
A male patient of any age who has only 1 testicle requires further evaluation. Since there is an
increased cancer risk in men with an undescended testicle, most of these “abdominal testicles”
are either removed (orchiectomy) or receive surgery that allows descent into the scrotum
(orchiopexy).
Although the number of Leydig cells is reduced when only 1 testicle is present, androgen levels
are not affected due to compensation by the remaining Leydig cell mass. Additionally, this
patient has a normal LH level, indicating that there is adequate androgenic feedback to the
hypothalamus and pituitary. Testosterone, dihydrotestosterone, and DHEA cause LH feedback
inhibition, but they are not part of the FSH feedback loop.
In a series of animal experiments, the insulin concentration in the pancreatic veins is measured after the administration of various agents. Epinephrine administration is found to cause a decrease in
insulin levels. However, after pretreatment with Drug A, epinephrine injection causes a paradoxical increase in insulin concentration. Which of the following receptors does Drug A most likely block?
Pancreatic beta cell insulin secretion is influenced by serum glucose levels and other factors such as autonomic nervous system activity. Parasympathetic stimulation of muscarinic M3 receptors
promotes insulin secretion and is induced by the smell and/or sight of food. In contrast, sympathetic stimulation is more complex, since both alpha-2 and beta-2 adrenergic receptors are present on
pancreatic beta cells and exert opposite effects. Stimulation of beta-2 receptors promotes insulin secretion while stimulation of alpha-2 receptors inhibits insulin release. However, the alpha-2-
mediated inhibitory effect is predominant, causing sympathetic stimulation to lead to overall inhibition of insulin secretion. Likewise, epinephrine administration activates both alpha-2 and beta-2
receptors, but the overriding inhibitory effect results in decreased insulin secretion. Following pretreatment with an alpha-2 receptor blocker (Drug A), epinephrine's effect on beta-2 receptors would
become dominant, resulting in increased insulin secretion.
A 20-year-old woman is brought to the emergency department due to intractable vomiting and abdominal pain. She has a several-week history of anorexia and weight loss. The patient has well-
controlled primary hypothyroidism treated with levothyroxine but has not taken her medication for 2 days because of vomiting. Temperature is 37.6 C (99.7 F), blood pressure is 80/40 mm Hg, pulse is
120/min, and respirations are 18/min. On physical examination, she is mildly lethargic but oriented. Generalized hyperpigmentation is present and is most conspicuous over the face, neck, and dorsal
surface of the hands. Urinalysis and chest x-ray are within normal limits. Finger-stick blood glucose is 60 mg/dL. A 1-L bolus of normal saline is rapidly infused, and high-flow intravenous fluids are
continued. This patient also requires immediate treatment with which of the following medications?
This patient most likely has acute adrenal crisis. Her history of hypothyroidism puts her at increased risk for other autoimmune endocrinopathies (eg, autoimmune adrenalitis), and her weight loss and
hyperpigmentation are suggestive of chronic primary adrenal insufficiency(Addison disease). In normal individuals, the adrenal glands respond to acute stress (eg, illness, surgery) with a
compensatory increase in glucocorticoid production, but patients with adrenal insufficiency cannot mount such a response.
Adrenal crisis is characterized by severe hypotension and refractory shock. Associated symptoms include abdominal pain, vomiting, weakness, and fever. In addition to aggressive fluid
resuscitation, treatment of adrenal crisis requires immediate glucocorticoid supplementation with hydrocortisone or dexamethasone. Treatment should begin immediately without waiting for results
of diagnostic studies, and the response is usually rapid.
Glucocorticoids are potent stimulators of liver gluconeogenesis and upregulate the synthesis of key gluconeogenic enzymes (eg, phosphoenolpyruvate carboxykinase, glucose-6-phosphatase).
Glucocorticoids also increase hepatic glycogen reserves by increasing expression of glycogen synthase, thereby improving glucose availability during periods of acute stress. These actions lead to an
overall increase in liver protein synthesis.
Peripherally, glucocorticoids antagonize the actions of insulin in skeletal muscle, favoring catabolism and proteolysis to provide substrates for gluconeogenesis and glycogenesis within the liver. This
effect can manifest as proximal muscle weakness (glucocorticoid myopathy). The effect on adipose tissue is mixed, with lipolytic and antilipolytic effects, altered fat distribution (eg, central obesity,
hypertrophy of the dorsocervical fat pad), and increased appetite and caloric intake. The net effect of gluconeogenesis and insulin antagonism is hyperglycemia.
General manifestations of hyperthyroidism
Symptoms Anxiety & insomnia
Palpitations
Heat intolerance
Increased perspiration
Weight loss without decreased appetite
Physical examination Goiter
Hypertension
Tremors involving fingers/hands
Hyperreflexia
Proximal muscle weakness
Lid lag
Atrial fibrillation
Graves' disease is an autoimmune disorder characterized by anti-thyroid antibodies, most prominently thyroid-stimulating immunoglobulin (TSI). TSI binds to TSH receptors in the thyroid and
triggers release of thyroid hormones, leading to thyrotoxicosis. Hyperthyroidism is associated with increased expression of beta-adrenergic receptors in various organs, and the subsequent
hyperadrenergic state can cause hypertension, tachycardia, sweating, heat intolerance, weight loss, and hyperreflexia. Patients with Graves' disease are frequently given beta adrenergic-blocking
medications (eg, propranolol) to control these manifestations while awaiting definitive management.
In contrast, the exophthalmos of Graves’ disease (Graves' ophthalmopathy) is caused by lymphocytic infiltration, enlargement of the extraocular muscles from myositis, fibroblast proliferation, and
overproduction of mucopolysaccharides in response to anti-thyroid antibodies. Some patients also develop pretibial myxedema (Graves' dermopathy) by a similar mechanism. These manifestations
are not adrenergic and do not respond to beta blocker therapy.
Although beta blockers can cause fatigue and depressive symptoms, they help reduce fatigue and mood lability in patients with Graves' disease by ameliorating sympathetic overactivation.
In the well-fed state, the abundance of ATP in hepatocytes inhibits isocitrate dehydrogenase, leading to high levels of citrate in the mitochondria. Citrate is transferred to the cytosol via the citrate
shuttle and cleaved by ATP citrate lyase to form acetyl-CoA. High citrate levels (in addition to elevated insulin caused by high carbohydrate intake) causes upregulation of Acetyl-CoA carboxylase.
This cytosolic enzyme catalyzes the conversion of acetyl-CoA to malonyl-CoA in the rate-limiting step of de novo fatty acid synthesis. Fatty acid synthase then catalyzes the condensation of
malonyl-CoA with acetyl-CoA to create a 4-carbon molecule that will undergo subsequent condensation reactions to form a 16-carbon fatty acid.
Beta-oxidation of fatty acids takes place primarily within the mitochondrial matrix. Mitochondrial membranes are impermeable to fatty acids due to their negative charge, so a specialized membrane
carrier (carnitine) must be used to shuttle them into the matrix. Malonyl-CoA inhibits carnitine acyltransferase, preventing the transfer of acyl groups into the mitochondria. This inhibitory action
functions to prevent the breakdown of newly synthesized fatty acids.
Ketone bodies (eg, acetoacetate) are a major source of fuel for muscle, brain, and cardiac tissue that are produced during times of starvation or fasting when oxaloacetate is in short supply and acetyl-
CoA is in excess.
Carnitine is an amino acid that is essential for the transport of fatty acids through the mitochondrial membrane. It is a necessary component of fatty acid oxidation.
Citrate is an intermediate in the TCA cycle. It can be exported out of the mitochondrial matrix and into the cytosol, where it is broken down into acetyl-CoA for use in de novo fatty acid synthesis.
NADPH is a reducing molecule necessary for the synthesis of fatty acids. In contrast, beta-oxidation of fats produces FADH2 and NADH-reducing equivalents.
In glycolysis, glucose is metabolized to pyruvate. Under aerobic conditions, pyruvate is converted to acetyl-CoA to enter the tricarboxylic acid (TCA) cycle. When oxygen is depleted (eg, in exercising
muscle), pyruvate is converted to lactate (anaerobic glycolysis).
During glycolysis, glyceraldehyde-3-phosphate (G3P) is converted to 1-3-bisphosphoglycerate (BPG) by the enzyme G3P dehydrogenase. This enzyme reduces NAD+ to NADH. NAD+ is present in
limited amounts in most cells, and it must be regenerated from NADH for glycolysis to continue. Under aerobic conditions, NAD+ is converted to NADH in the TCA cycle. NADH is then reconverted to
NAD+ in the electron transport chain as the energy in NADH is utilized to synthesize ATP.
In anaerobic glycolysis, NAD+ is regenerated from NADH when pyruvate is converted to lactate via lactate dehydrogenase. In patients with lactate dehydrogenase deficiency, glycolysis is inhibited
in strenuously exercising muscle as muscle cells cannot regenerate NAD+. Consequently, high-intensity physical activity leads to muscle breakdown, pain, and fatigue as insufficient amounts of
energy are being produced in the exercising muscle.
During muscle contraction, glycogen is broken down via glycogen phosphorylase for energy production by the glycolytic pathway. Epinephrine causes cyclic AMP-mediated phosphorylation of
glycogen phosphorylase, which activates this enzyme. Non-phosphorylation-dependent activation of glycogen phosphorylase can occur during muscle contraction via increased intracellular calcium
concentrations and via AMP under extreme conditions.
Carnitine is an amino acid derivative responsible for transporting fatty acids into the mitochondria for beta-oxidation. Carnitine is synthesized from lysine and methionine; vitamin C is essential for this
synthesis.
Citrate is formed from the condensation of acetyl CoA with oxaloacetate in the first step of the TCA cycle. Increased citrate concentrations decrease glycolysis as citrate is a powerful allosteric
inhibitor of phosphofructokinase-1. In exercising muscles under anaerobic conditions, oxidative phosphorylation of glucose through the citric acid cycle is not a dominant pathway; therefore, excess
citrate is not produced.
FADH2 is not produced in glycolysis. FADH2 is produced from FAD during the conversion of succinate to fumarate in the TCA cycle by the enzyme succinate dehydrogenase.
In glycolysis, pyruvate is formed from phosphoenolpyruvate by a unidirectional enzyme called pyruvate kinase. In the absence of lactate dehydrogenase activity, pyruvate will accumulate in the cell
under anaerobic conditions.
A 45-year-old man is referred to an endocrinologist for newly diagnosed diabetes mellitus. A week ago, his primary care physician noted an elevated fasting serum glucose level. The endocrinologist
discusses the different treatment options available, including oral and injectable medications. He recommends treatment with a medication that alters glucose metabolism within the liver by increasing
the concentration of fructose 2,6-bisphosphate within hepatocytes. Which of the following conversions will be inhibited by high intracellular concentrations of this metabolite?
Fructose 2,6-bisphosphate helps control the balance between gluconeogenesis and glycolysis through inverse regulation of phosphofructokinase-1 (PFK-1) and fructose 1,6-bisphosphatase.
Fructose 2,6-bisphosphate activates PFK-1, the main regulatory enzyme involved in glycolysis, which converts fructose 6-phosphate to fructose 1,6-bisphosphate. The opposite reaction (fructose
1,6-bisphosphate to fructose-6-phosphate) occurs in gluconeogenesis and is catalyzed by the enzyme fructose-1,6-bisphosphatase (inhibited by fructose 2,6-bisphosphate).
The interconversion of fructose-6-phosphate and fructose 2,6-bisphosphate is achieved by a bifunctional enzyme complex composed of PFK-2 (increases fructose 2,6-bisphosphate levels) and
fructose 2,6-bisphosphosphatase (decreases fructose 2,6-bisphosphate levels). Insulin causes activation of PFK-2, leading to increased fructose 2,6-bisphosphate levels and augmented
glycolysis. High concentrations of fructose 2,6-bisphosphate also inhibit gluconeogenesis, leading to decreased conversion of alanine and other gluconeogenic substrates to glucose.
Fatty acid synthesis is upregulated by insulin and high citrate levels (which increase when acetyl-CoA is abundant, as with active glycolysis). Therefore, fatty acid synthesis is likely to be upregulated in
metabolic states in which fructose 2,6-bisphosphate concentration is increased.
The conversion of fructose-6-phosphate to fructose-1,6-bisphosphate is catalyzed by the enzyme PFK-1. This enzyme is allosterically activated by high levels of fructose-2,6-bisphosphate, and so
conversion would be increased.
Glycogen formation is stimulated by increased levels of insulin and glucose-6-phosphate. Because elevated insulin levels also increase fructose 2,6-bisphosphate formation, the rise of fructose 2,6-
bisphosphate levels in hepatocytes is typically concurrent with increased glycogen synthesis.
The rise in fructose-2,6-bisphosphate accelerates glycolysis, leading to increased conversion of NAD+ to NADH.
A 51-year-old woman comes to the office due to progressively worsening fatigue, weight gain, and constipation for the past 6 months. The patient has had difficulty performing daily activities due to
fatigue. She has no significant medical history and takes no medications. The patient has no drug allergies and does not use tobacco, alcohol, or illicit drugs. Blood pressure is 110/80 mm Hg and
pulse is 55/min. Physical examination shows mild, diffuse enlargement of the thyroid gland. Cardiopulmonary and abdominal examinations are normal. Biopsy of this patient's thyroid is most likely to
show which of the following f
This patient has progressive symptoms of hypothyroidism (eg, fatigue, weight gain, constipation) and a diffuse goiter, consistent with chronic lymphocytic (Hashimoto) thyroiditis. This disease
occurs predominately in women, with a peak incidence at age 45-65, and is the most common cause of hypothyroidism in iodine-sufficient regions such as the United States.
As with all forms of primary hypothyroidism, laboratory studies show low serum thyroxine (T4) levels and an elevated TSH. Elevated antithyroid peroxidase antibody levels can confirm the diagnosis. If
the diagnosis is uncertain (eg, thyroid nodularity), a biopsy can be performed to rule out malignancy. Characteristic findings of Hashimoto thyroiditis include an intense mononuclear
infiltrateconsisting of lymphocytes and plasma cells, often with germinal centers (arrow in image above). Residual follicles are often surrounded by Hürthle cells (large oxyphilic cells filled with
granular cytoplasm) that represent follicular epithelial cells that have undergone metaplastic change in response to inflammation.
Histopathology in papillary thyroid cancer shows branching papillary structures with concentric calcifications (psammoma bodies) and ground-glass or empty-appearing nuclei ("Orphan Annie eye"
nuclei). However, papillary thyroid cancer typically presents as an enlarging nodule in a clinically euthyroid patient.
Riedel thyroiditis is characterized by extensive fibrosis of the thyroid gland extending into the surrounding structures. The fibrotic thyroid gland in Riedel thyroiditis is typically hard and fixed to
surrounding structures, often resembling a malignancy.
Graves disease presents with a diffusely enlarged thyroid gland associated with hyperthyroidism, exophthalmos, and pretibial myxedema. The thyroid follicular epithelium is tall and crowded with
hyperactive reabsorption, causing scalloping around the edges of the colloid. Follicular hyperplasia with elongated epithelial cells is also seen in the tall-cell variant of papillary thyroid cancer, typically
presenting in older adults as an enlarging thyroid mass.
Subacute granulomatous (de Quervain) thyroiditis is characterized by disruption of follicles and a mixed cellular infiltrate with occasional multinuclear giant cells. Patients typically present after a viral
upper respiratory infection with fever and a painful, tender thyroid gland.
The endoplasmic reticulum (ER) is a continuous system of folded membranes that
enclose a single cisternal space. The rough ER (RER) has ribosomes attached and is
the site of synthesis of secretory, lysosomal, and integral membrane proteins. Once
synthesized, many proteins undergo post-translational modification inside the RER
and most are targeted for export to the Golgi apparatus. These proteins pass from the
RER to the Golgi apparatus within COP II coated transport vesicles. The Golgi
apparatus sorts and distributes proteins to the cell membrane, organelles, and
secretory granules.
In contrast to the RER, the smooth ER (SER) contains enzymes for steroid and
phospholipid biosynthesis. All steroid-producing cells (eg, cells in the adrenals,
gonads, and liver) contain a well-developed SER. ACTH primarily stimulates the cells
in the adrenal cortex to produce glucocorticoids, but it also increases adrenal
production of mineralocorticoids and androgens to a lesser extent. These are all
cholesterol-derived steroid hormones, and the cells that synthesize them contain
prominent SERs. The SER is also involved in the detoxification of numerous drugs,
especially in hepatocytes. In addition, a specialized SER functions as the
sarcoplasmic reticulum in striated muscle cells.
Enzymes and the biochemical processes they catalyze often require distinct chemical environments for optimal function; small variations in temperature, molecular concentrations, and pH may render
them ineffective. Cellular compartmentalization provides a means by which multiple heterogeneous environments can exist within a cell. Organelles such as the nucleus and mitochondria form
distinct, membrane-bound regions with a chemical composition different from the cytosol. This allows multiple biochemical processes to occur simultaneously at maximum efficiency.
The cytosol and mitochondria are the predominant sites of metabolism in the cell. Mitochondria are the site of beta-oxidation of fatty acids, the citric acid cycle, and the carboxylation of pyruvate
(gluconeogenesis). The cytosol is home to enzymes necessary for glycolysis, fatty acid synthesis, and the pentose phosphate pathway. Transketolase is an enzyme of the pentose phosphate
pathway that uses thiamine (vitamin B1) as a cofactor to shuttle 2-carbon fragments between sugar molecules. Other processes such as heme synthesis, the urea cycle, and gluconeogenesis rely on
a complex interplay between the mitochondria and cytosol to function optimally; enzymes present in both cellular compartments are required for these metabolic pathways.
3-Hydroxy-3-methylglutaryl-CoA (HMG CoA) lyase is a mitochondrial enzyme necessary for ketogenesis. It is also responsible for metabolism of the ketogenic amino acid, leucine.
Ornithine transcarbamylase catalyzes the combination of ornithine and carbamoyl phosphate to form citrulline in the urea cycle. This reaction occurs within the mitochondria.
Pyruvate carboxylase catalyzes the initial step in gluconeogenesis by converting pyruvate to oxaloacetate. This enzyme requires biotin as a cofactor, and functions within the mitochondria.
Succinate dehydrogenase is a TCA cycle enzyme that converts succinate to fumarate. It is an inner mitochondrial membrane protein and functions as part of the electron transport chain.
G protein-coupled receptors that bind glycoprotein hormones (eg, TSH, LH, FSH) contain 3 major domains: an extracellular domain responsible for ligand binding, a transmembrane domain, and an
intracellular domain coupled with heterotrimeric G proteins.
The transmembrane domain is made up of nonpolar, hydrophobic amino acids (eg, alanine, valine, leucine, isoleucine, phenylalanine, tryptophan, methionine, proline, glycine). These amino acids are
arranged in an alpha-helical fashion and project their hydrophobic R groups outwardly, anchoring the transmembrane region of the protein to the hydrophobic core of the phospholipid bilayer. The
transmembrane domain may also play an important role in cellular signaling and transport.
Binding of a ligand to the extracellular domain of a transmembrane receptor can result in activation of the cAMP or phosphatidylinositol second messenger system, activation of receptor tyrosine
kinases, opening of ion channels, and activation of the calcium-calmodulin system. The extracellular domain of these receptors is typically composed of hydrophilic amino acids.
Activation of G protein-coupled receptors utilizing the cAMP second messenger system results in increased synthesis of intracellular cAMP and subsequent activation of protein kinase A. Protein
kinase A then phosphorylates cytosolic proteins that translocate into the nucleus and bind to DNA promotor regions to modulate transcription.
Intracellular iron-containing proteins (hemeproteins) include hemoglobin, myoglobin, and cytochrome oxidase. Heme is a complex of protoporphyrin IX and iron. Hemoglobin A, the most common
hemoglobin in adults, consists of 2 alpha and 2 beta globin chains held together by noncovalent interactions. Each subunit contains stretches of alpha helices that form a heme-binding pocket lined
by nonpolar amino acids.
Insulin and IGF-1 bind to receptors that possess tyrosine kinase on their intracellular domain (receptor tyrosine kinases). These receptors dimerizes on ligand binding to the extracellular domain, which
subsequently activates tyrosine kinase. Tyrosine kinase phosphorylates tyrosine residues, triggering a downstream cellular response.
Amenorrhea can be categorized as primary (failure of menarche prior to age 15) or secondary
(cessation of menstruation in premenopausal women who previously have had menses).
Secondary amenorrhea can be due to hypothalamic, pituitary, ovarian, uterine, or other
endocrine (eg, thyroid) disorders.
This patient has secondary amenorrhea associated with low body weight, frequent strenuous
exercise, and lanugo (fine hair indicating inadequate caloric intake), suggesting functional
hypothalamic amenorrhea (FHA). FHA is commonly seen in competitive athletes, dancers,
fashion models, and others who maintain very low body weights. The underlying
pathophysiology of FHA is incompletely understood but appears to involve reduced
circulating leptin levels as a result of diminished adipose tissue stores. The decrease in leptin
levels inhibits pulsatile gonadotropin-releasing hormone (GnRH) release from the
hypothalamus, causing decreased pituitary LH and FSH secretion, low circulating estrogen
levels, and amenorrhea.
Excessive male-pattern hair growth in a woman is called hirsutism. Hirsutism can be due to increased androgen production (eg, polycystic ovary syndrome, Cushing syndrome, ovarian and adrenal
tumors), increased local conversion of testosterone to dihydrotestosterone (DHT), or higher sensitivity of hair follicles to DHT (eg, idiopathic hirsutism). With excessive androgen exposure, soft, non-
pigmented villous hair changes to coarse pigmented terminal hair in androgen-dependent areas of the body (eg, face, chest, back). Virilization occurs with very high androgen levels and is
characterized by clitoromegaly, increased muscularity, and voice deepening in addition to hirsutism.
The most common cause of hirsutism is polycystic ovary syndrome (PCOS), which is often associated with elevated androgen levels. Combination oral contraceptive pills (OCPs) are usually the first
choice for treating hirsutism in PCOS. OCPs work by suppressing LH secretion from the pituitary, thereby decreasing ovarian androgen production. They also increase sex hormone-binding globulin
synthesis by the liver, decreasing free testosterone levels.
Ornithine decarboxylase is involved in DNA stabilization and repair. Inhibition leads to decreased cell growth and increased apoptosis. Eflornithine is a topical ornithine decarboxylase inhibitor used to
decrease the rate of facial hair growth.
Patients with PCOS who develop diabetes mellitus are usually treated with metformin, which increases insulin sensitivity. Metformin can also help normalize menses but would not improve hirsutism.
Testosterone receptor antagonists (eg, spironolactone) are effective in suppressing androgen-dependent hair growth. 5-α-reductase inhibitors (eg, finasteride) decrease peripheral conversion of
testosterone to DHT but are less effective than testosterone receptor antagonists in treating hirsutism. Both are strongly teratogenic.
Poor glucose control before or during pregnancy is associated with adverse effects on the fetus and newborn. Macrosomia (>4 kg [8 lb 14 oz]) is a common finding in infants of diabetic mothers.
Poor maternal glucose control leads to excessive transplacental glucose transfer to the fetus, which stimulates fetal insulin production. Chronic stimulation of the fetal beta cells leads to beta cell
hyperplasia and hyperinsulinism. Elevated insulin levels contribute to increased fat deposition and enhanced fetal growth, resulting in macrosomia.
After delivery, the infant experiences a sudden interruption in transplacental glucose transfer, but the hyperinsulinism remains due to the beta cell hyperplasia. This can result in rapid development of
profound hypoglycemia, and affected infants require frequent feedings or parenteral glucose to prevent hypoglycemia and subsequent neurologic injury. In most cases, supportive care is all that is
required; the beta cell hyperplasia will resolve over time.
Metformin is the most commonly prescribed medication for type 2 diabetes mellitus. Metformin inhibits mitochondrial glycerophosphate dehydrogenase and complex I (first electron transport chain
enzyme). The resulting decrease in cellular energy stores causes AMPK activation, leading to decreased hepatic gluconeogenesis. Metformin also increases peripheral glucose utilization. It does
not increase endogenous insulin secretion and does not cause hypoglycemia when used as monotherapy.
In normal individuals, lactate produced in the intestine is converted to glucose via gluconeogenesis in the liver. Inhibition of mitochondrial enzymes by metformin increases intestinal production of
lactate (due to increased anaerobic glycolysis) and reduces hepatic metabolism of lactic acid (due to decreased gluconeogenesis). This increases the risk of lactic acidosis, particularly in older
patients and those with significant hepatic or renal dysfunction. Renal function should be assessed by serum creatinine measurement prior to initiation of metformin therapy. Metformin should also
be avoided in patients with congestive heart failure or alcoholism due to the increased risk of lactic acidosis in these populations.
This patient's vomiting, volume depletion, glucosuria, and ketonuria are consistent with diabetic ketoacidosis (DKA). DKA is treated with an intravenous infusion of regular insulin that begins to
lower serum glucose and ketone levels within minutes of administration. Regular insulin has a half-life of 5 minutes, allowing rapid adjustment of the infusion rate based on glucose levels.
Regular insulin can also be used subcutaneously in the long-term management of diabetes, usually in combination with a long-acting insulin analog. (Regular insulin and neutral protamine Hagedorn
[NPH] are the only human recombinant insulins without any amino acid modification. All other preparations are properly referred to as insulin analogs.) When given subcutaneously, regular insulin
starts working within 30 minutes, peaks in 2-4 hours, and lasts 5-8 hours. Subcutaneous regular insulin should not be used in patients with DKA as they are usually volume depleted and have erratic
subcutaneous absorption.
Insulin lispro, aspart, and glulisine are rapid-acting insulin analogs. Due to various amino acid modifications, they do not polymerize into hexamers like regular insulin, allowing them to be absorbed
rapidly after subcutaneous injection. They have an onset of action of about 15 minutes and peak in 45-75 minutes. These analogs are not usually given intravenously, as their kinetics via this route are
the same as regular insulin and they are more expensive.
NPH insulin is an intermediate-acting insulin composed of a crystalline suspension of insulin with protamine and zinc. This delays absorption of insulin from the subcutaneous injection site. NPH
usually starts working within 2 hours, peaks in 4-12 hours, and lasts about 18 hours.
Detemir is a long-acting insulin analogue with a fatty acid bound to one of the lysine amino acids on the insulin molecule. This fatty acid side chain allows detemir to bind to albumin and slowly
dissociate, resulting in prolonged action. It usually starts working within 2 hours, peaks between 3-9 hours, and lasts up to 24 hours.
Glargine is an insulin analog with a long duration of action. Glargine has a pH of 4 and forms a microprecipitate in the subcutaneous tissue after injection, resulting in a very slow release of insulin.
Glargine lasts about 24 hours and does not have a pronounced peak.
A 33-year-old man comes to the emergency department due to headaches, tremulousness, and sweating. His symptoms have been intermittent over the last several months. The patient's past
medical history is unremarkable, but he has a family history of primary hyperparathyroidism. Blood pressure is 200/120 mm Hg while standing and 190/110 mm Hg while supine. Laboratory
evaluation shows increased urinary metanephrines and catecholamines. CT scan of the abdomen shows a 4.5-cm right-sided adrenal mass. The cells responsible for this patient's disease most likely
have a common embryological origin with which of the following cells?
This patient with severe hypertension, increased urinary excretion of catecholamines and metanephrines, and an adrenal mass has typical features of pheochromocytoma. Pheochromocytoma can
be sporadic or associated with several familial disorders, especially multiple endocrine neoplasia (MEN) type 2. MEN type 2 is associated with germ line mutations in the RET proto-oncogene and is
characterized by:
Pheochromocytomas
Medullary thyroid cancer (malignancy of parafollicular C cells)
Either parathyroid hyperplasia (MEN 2A) or mucosal neuromas and marfanoid habitus (MEN 2B)
The neural crests are embryological structures comprised of bilateral, paired strips of cells arising from the ectoderm at the margin of the neural tube. Both the thyroid parafollicular C cells and
chromaffin cells of the adrenal medulla are derived from neural crest tissue (the adrenal cortex is derived from the mesoderm). Structures arising from neural crest cells are summarized by the
mnemonic MOTEL PASS: melanocytes, odontoblasts, tracheal cartilage, enterochromaffin cells, laryngeal cartilage, parafollicular cells of the thyroid, adrenal medulla and all ganglia, Schwann cells,
and spiral membrane.
A 20-year-old woman comes to the emergency department with lethargy, abdominal pain, and nausea. She has had polyuria and excessive thirst for one day. She also complains of dysuria and chills
over the last few days but did not seek medical care until today. Physical examination shows tachycardia and dry mucous membranes. Laboratory results are as follows:
Serum chemistry panel
Sodium 130 mEq/L
Chloride 93 mEq/L
Bicarbonate 12 mEq/L
Blood urea nitrogen 30 mg/dL
Creatinine 1.3 mg/dL
Calcium 10.0 mg/dL
Glucose 698 mg/dL
Which of the following electrolyte findings would most likely be seen in this patient?
This young patient has both clinical (eg, polyuria, polydipsia, volume depletion) and
biochemical (eg, hyperglycemia, low bicarbonate, high anion gap, decreased
serum sodium levels) signs of diabetic ketoacidosis (DKA). DKA is often
precipitated by infections, including urinary tract infections (likely in this patient).
Patients with DKA lose significant amounts of potassium in the urine, primarily via
glycosuria-induced osmotic diuresis and hypovolemia-mediated increase in
aldosterone secretion. This results in a total body potassium deficit that is
reflected by decreased intracellular potassium stores (since 98% of the body's
potassium is stored intracellularly). Despite the low intracellular potassium levels,
extracellular potassium concentrations are normal or increased due to the
following mechanisms:
1. Loss of intracellular free water caused by increased plasma osmolality
leads to extracellular movement of potassium secondary to increasing
intracellular potassium concentration
2. Lack of insulin also causes extracellular shifting of potassium as insulin
normally promotes cellular uptake of potassium
Clinicians must be careful when giving insulin and intravenous fluids during
resuscitation of dehydrated, hyperglycemic patients. These interventions force
potassium back into the cells, causing a precipitous drop in serum potassium due
to the total body deficit. Despite normal or elevated serum potassium, timely
administration of potassium supplementation is essential when treating a patient
with DKA.
56-year-old man comes to the emergency department with severe right foot pain. The pain began acutely, and there is no history of recent trauma. The patient has associated redness and swelling
but no fever. He has had no similar symptoms in the past. Past medical history is significant for mixed hyperlipidemia treated with lifestyle modifications and several medications. Physical
examination shows a swollen, tender first metatarsophalangeal joint. Aspiration reveals a high leukocyte count, negative Gram stain, and numerous needle-shaped negatively birefringent crystals.
Which of the following drugs is most likely to have precipitated this patient's condition?
This patient has an acute flare of gouty arthritis likely due to treatment with niacin (nicotinic acid). Niacin improves hyperlipidemia by decreasing hepatic synthesis of triglycerides and VLDL and
reducing clearance of HDL. It is the most effective agent for raising HDL levels; however, as it has not been shown to reduce the risk of cardiac events, it is primarily used in patients who have failed
other lipid-lowering drugs.
The use of niacin is limited by several significant side effects, including flushing, hyperglycemia, and hepatotoxicity. In addition, niacin can decrease renal excretion of uric acid, leading to elevated
blood levels and an increased risk for acute gouty arthritis.
A 34-year-old woman comes to the clinic due to dizziness and mild confusion over the last week. The patient has a history of seizures beginning in childhood and was recently started on
carbamazepine by her neurologist. Her temperature is 36.7 C (98 F), blood pressure is 121/72 mm Hg, pulse is 68/min, and respirations are 13/min. Physical examination is within normal limits.
Laboratory studies show a low serum sodium concentration. It is determined that the patient's condition is caused by increased release of a hormone that is co-secreted with neurophysins. This
hormone is most likely secreted into the circulation at which of the following sites?
This patient most likely has the syndrome of inappropriate antidiuretic hormone secretion (SIADH), which can be caused by a multitude of drugs, including carbamazepine, cyclophosphamide, and
selective serotonin reuptake inhibitors.
Antidiuretic hormone (vasopressin) and oxytocin are synthesized within magnocellular neurons found in the supraoptic and paraventricular nuclei of the hypothalamus. Most magnocellular neurons
produce either vasopressin or oxytocin. Once translated, these hormones are packaged into vesicles and travel via anterograde axonal transport to the posterior pituitary (neurohypophysis). There,
the hypothalamic axons terminate into Herring bodies, which are specialized nerve terminals that act as storage sites for the secretory vesicles. These vesicles also contain proteins known as
neurophysins that are involved in posttranslational hormone processing and stabilization during axonal transport. Vasopressin and oxytocin and their associated neurophysins are then secreted from
the posterior pituitary into the hypophysial vein to enter the systemic circulation.
Circulating thyroid hormone consists of 2 fractions, a protein-bound fraction and a free fraction that is available to enter target cells via a carrier-mediated mechanism. More than 99% of circulating
thyroid hormone is bound to plasma proteins, creating a large circulating reservoir pool of thyroid hormone. Thyroxine-binding globulin (TBG) accounts for approximately 70% of thyroid hormone
binding, with an additional share bound by albumin and transthyretin.
An increase in estrogen activity (eg, pregnancy, oral contraceptive use, post-menopausal hormone replacement therapy) raises circulating TBG levels, causing a corresponding reduction in free T4
and free T3 levels. In patients with a normal hypothalamic-pituitary-thyroid axis, this reduction will result in a transient increase in thyroid hormone production until the additional quantity of TBG
becomes saturated with thyroid hormone and free T4 and free T3 levels are restored. Therefore, an increase in TBG levels leads to an increase in total T4(bound T4 plus free T4) as well as total T3.
However, the level of free thyroid hormones remains normal, patients remain euthyroid, and TSH levels remain in the normal range.
A 23-year-old man is brought to the emergency department by his roommate due to progressive weakness and confusion. The roommate says that the patient has been "drinking water all of the time
and using the bathroom constantly" since he got sick with a cold 2 days ago. Temperature is 37.8 C (100 F), blood pressure is 96/58 mm Hg, and pulse is 112/min. Physical examination shows dry
mucous membranes and his urine has a strong, fruity odor. Laboratory results are as follows:
Serum chemistry
Sodium 134 mEq/L
Potassium 3.8 mEq/L
Chloride 100 mEq/L
Bicarbonate 14 mEq/L
Creatinine 1.0 mg/dL
Glucose 498 mg/dL
pH 7.17
PaCO2 40 mm Hg
The combination of acute-onset polyuria, polydipsia, volume depletion, and a fruity odor to the urine or breath is suggestive of diabetic ketoacidosis, which in this patient was most likely precipitated
by a viral infection. The laboratory findings of hyperglycemia and anion gap metabolic acidosis confirm the diagnosis. The anion gap is due to the presence of unmeasured anionic ketoacids (eg,
beta-hydroxybutyrate, acetoacetate) that bind and lower serum HCO3−.
Patients with metabolic acidosis usually develop a compensatory respiratory alkalosis by hyperventilating (eg, Kussmaul respirations), which helps mitigate the acidemia by causing a drop in the
PaCO2. However, if the PaCO2 persists above the expected compensatory range (given by Winter formula, where PaCO2 = [1.5 * HCO3−] + 8 ± 2), it indicates a superimposed respiratory acidosis
that is interfering with normal respiratory compensation.
This patient's serum HCO3− of 14 mEq/L should be compensated by a PaCO2 in the range of 27-31 mm Hg. However, his PaCO2 is higher than expected, indicating that he has a mixed acid-base
disturbance consisting of metabolic and respiratory acidoses. Severe diabetic ketoacidosis can cause pulmonary edema, respiratory fatigue, and decreased mental status, which may lead to
hypoventilation and subsequent hypercarbic respiratory failure.
You might also like
- Molecular Biology and Pathology: A Guidebook for Quality ControlFrom EverandMolecular Biology and Pathology: A Guidebook for Quality ControlDaniel H. FarkasNo ratings yet
- Plasma Enzyme DiagnosisDocument30 pagesPlasma Enzyme DiagnosisKayode IbitoyeNo ratings yet
- Problem-based Approach to Gastroenterology and HepatologyFrom EverandProblem-based Approach to Gastroenterology and HepatologyJohn N. PlevrisNo ratings yet
- Physiology. Hrd.Document549 pagesPhysiology. Hrd.Sʌɩĸʌt PʌʋɭNo ratings yet
- Structure and Function of HaemoglobinDocument21 pagesStructure and Function of HaemoglobinSonam JoshiNo ratings yet
- Biochem - (With Answers and Achievement Chart)Document11 pagesBiochem - (With Answers and Achievement Chart)Valine Cysteine MethionineNo ratings yet
- Kerala PG Medical Admission Prospectus 2015Document63 pagesKerala PG Medical Admission Prospectus 2015doctor82No ratings yet
- Chemistry of Nucleic Acid (2) - Doc Viliran 06/11/09Document162 pagesChemistry of Nucleic Acid (2) - Doc Viliran 06/11/09lowellaNo ratings yet
- Thalassemia and HaemoglobinopathiesDocument28 pagesThalassemia and HaemoglobinopathiesJared Khoo Er HauNo ratings yet
- Biochemistry One Liner PDFDocument13 pagesBiochemistry One Liner PDFMinaz PatelNo ratings yet
- Water An Electrolyte Metabolism and Their DisordersDocument60 pagesWater An Electrolyte Metabolism and Their DisordersAbigail AdegbuluNo ratings yet
- AS Biology BYB1 Core Principles 10.4 Enzymes TestDocument5 pagesAS Biology BYB1 Core Principles 10.4 Enzymes TestormattNo ratings yet
- Amino Acid Conversion and Specialized Nitrogen ProductsDocument62 pagesAmino Acid Conversion and Specialized Nitrogen Productsendale gebregzabherNo ratings yet
- Lipoproteins Lecture For 1st Year MBBs by DR Sadia HaroonDocument15 pagesLipoproteins Lecture For 1st Year MBBs by DR Sadia HaroonIMDCBiochemNo ratings yet
- Biochem Lab Con Ast AltDocument31 pagesBiochem Lab Con Ast AltMarvel Delos SantosNo ratings yet
- ThalassemiaDocument93 pagesThalassemiaHafdzi MaulanaNo ratings yet
- Amino Acids Metabolism Part II: Conversion of amino acids to specialized products and porphyrinsDocument35 pagesAmino Acids Metabolism Part II: Conversion of amino acids to specialized products and porphyrinsTimothy George100% (1)
- Basic Tech in Clinical ChimistryDocument84 pagesBasic Tech in Clinical ChimistryAhmed AboamerNo ratings yet
- Clinical Biochemistry HSST CurriculumDocument111 pagesClinical Biochemistry HSST CurriculumChengyuan ZhangNo ratings yet
- Plasma ProteinsDocument23 pagesPlasma ProteinsNgonie Dube100% (1)
- MD Biochem Lab Logbook: Enzyme ActivityDocument40 pagesMD Biochem Lab Logbook: Enzyme ActivityRamesh Babu Manivannan100% (1)
- Organ BiochemistryDocument158 pagesOrgan Biochemistryyodi2801No ratings yet
- Shelly HyperlipidemiaDocument22 pagesShelly Hyperlipidemiaale marilNo ratings yet
- Hormonal Control of Calcium and Phosphate MetabolismDocument50 pagesHormonal Control of Calcium and Phosphate MetabolismhamidNo ratings yet
- 4 HGBDocument38 pages4 HGBChona_Delos_Re_1233No ratings yet
- Explain The Ff. Manifestations in The Different Cases That Are Discused BelowDocument29 pagesExplain The Ff. Manifestations in The Different Cases That Are Discused BelowRodel Paulo Tangunan GarciaNo ratings yet
- CHR InflammationDocument33 pagesCHR InflammationAlnzeer6No ratings yet
- Clinical Questions: Histidine To HistamineDocument28 pagesClinical Questions: Histidine To HistamineNancy AkunnaNo ratings yet
- Acid-Base DisordersDocument40 pagesAcid-Base DisordersHelenNo ratings yet
- The Complement SystemDocument24 pagesThe Complement Systemhkatniwala100% (1)
- Describe The Molecular Basis Underlying Haematological MalignancyDocument3 pagesDescribe The Molecular Basis Underlying Haematological MalignancyAlison HinesNo ratings yet
- Hiv, Hepa C: Lab Test Ordered Order Received Prepare The Necessary Things To Be UsedDocument7 pagesHiv, Hepa C: Lab Test Ordered Order Received Prepare The Necessary Things To Be UsedmaineNo ratings yet
- Hematopoiesis DiagramDocument1 pageHematopoiesis DiagramApril Rose Airoso - AramburoNo ratings yet
- Clinical Biochemistry: Understanding Disease through Laboratory TestingDocument14 pagesClinical Biochemistry: Understanding Disease through Laboratory TestingbsmallahNo ratings yet
- Lipid Profile: by Micheal and ChristianDocument15 pagesLipid Profile: by Micheal and ChristianMichealNo ratings yet
- Plasma Enzyme Levels and Their Clinical SignificanceDocument18 pagesPlasma Enzyme Levels and Their Clinical SignificanceNur LiyanaNo ratings yet
- RINJUDocument35 pagesRINJUதீபன்குமார் கதிரேசன்100% (1)
- Oxygen Transport: Dr. Phoebe Bacalso-LetabaDocument36 pagesOxygen Transport: Dr. Phoebe Bacalso-LetabaMaria Nicole EconasNo ratings yet
- Lab 9++10 Pathological UrinlysisDocument38 pagesLab 9++10 Pathological UrinlysisSai SreedharNo ratings yet
- BM Program at KazNMUDocument15 pagesBM Program at KazNMUAlok Kumar100% (1)
- Best Physiology TextbookDocument3 pagesBest Physiology TextbookPeterNo ratings yet
- EnzymesDocument19 pagesEnzymesوليد. وفي الروح0% (1)
- Xenobiotic MetabolismDocument64 pagesXenobiotic MetabolismBelajar dan berdoaNo ratings yet
- Haem Lecture 2.2016 PDFDocument12 pagesHaem Lecture 2.2016 PDFdorsa koraeiNo ratings yet
- Sickle Cell DiseaseDocument18 pagesSickle Cell DiseaseHabib UllahNo ratings yet
- Bone Marrow TransplantationDocument21 pagesBone Marrow TransplantationMorrison George100% (1)
- Biochemistry Recent NEET PG Pattern Questions PrepladderDocument25 pagesBiochemistry Recent NEET PG Pattern Questions PrepladderAman SharmaNo ratings yet
- Manchester Anaemia GuideDocument13 pagesManchester Anaemia Guidemubzy14No ratings yet
- Praktikum BiokimiaDocument148 pagesPraktikum BiokimiaZuniva AndanNo ratings yet
- Epimer of GlucoseDocument8 pagesEpimer of GlucoseMohammad BaberNo ratings yet
- Biochemistry of Digestive SystemDocument55 pagesBiochemistry of Digestive SystemSyam UnhasNo ratings yet
- EnzymesDocument229 pagesEnzymesJimwell AxalanNo ratings yet
- Chemical Pathology Job Description December 2011Document9 pagesChemical Pathology Job Description December 2011Chengyuan ZhangNo ratings yet
- Hemoglobin MetabolismDocument80 pagesHemoglobin MetabolismSurya BudikusumaNo ratings yet
- Managing HIV Patients & HAART Metabolic ComplicationsDocument33 pagesManaging HIV Patients & HAART Metabolic ComplicationsSimeon AdebisiNo ratings yet
- LONGLIVE Lifestyle To Conquer AgingDocument21 pagesLONGLIVE Lifestyle To Conquer AgingRakesh SharmaNo ratings yet
- Atlas of Diseases of The KidneyDocument1,095 pagesAtlas of Diseases of The KidneyYanka IlarionovaNo ratings yet
- Pathophysiology Cell Injury GuideDocument7 pagesPathophysiology Cell Injury GuideWendy SuhNo ratings yet
- 11 Reproductive System PhysiologyDocument38 pages11 Reproductive System PhysiologyKaye Alyssa EnriquezNo ratings yet
- Hematology & Lymphoid System Study Guide - Y1 2025Document43 pagesHematology & Lymphoid System Study Guide - Y1 2025Wahaj Mujahid100% (1)
- Acute Multiple Sclerosis RelapseDocument16 pagesAcute Multiple Sclerosis RelapseHabib G. Moutran BarrosoNo ratings yet
- Chemical Coordination and IntegrationDocument8 pagesChemical Coordination and IntegrationsuryababaNo ratings yet
- Stress and Skin Disorders, 2017Document257 pagesStress and Skin Disorders, 2017Elisa Carrera50% (4)
- 5 HDocument4 pages5 HDee GeeNo ratings yet
- Adrenal Glands Disorders: Cushing's Syndrome, Addison's DiseaseDocument34 pagesAdrenal Glands Disorders: Cushing's Syndrome, Addison's DiseaseTabish KhalidNo ratings yet
- (2014) Cognitive Behavioral Approach To Understanding Irritable Bowel SyndromeDocument16 pages(2014) Cognitive Behavioral Approach To Understanding Irritable Bowel SyndromeAlex SolorzanoNo ratings yet
- Quiz EndocrineDocument84 pagesQuiz EndocrineMedShare92% (12)
- Pharmacology ChartDocument23 pagesPharmacology ChartKelly Milaski0% (1)
- Abnormal Psychology: Causal Factors and ViewpointsDocument9 pagesAbnormal Psychology: Causal Factors and ViewpointsEya Morales100% (1)
- 11 - The Evolving Science of Chiropractic Philosophy PDFDocument10 pages11 - The Evolving Science of Chiropractic Philosophy PDFAnca Daniela CuldaNo ratings yet
- JytjtyjDocument262 pagesJytjtyjarkaprava paulNo ratings yet
- Group 1 hormonesDocument5 pagesGroup 1 hormonesCarrie Joy DecalanNo ratings yet
- Chapter 9 The Endocrine SystemDocument62 pagesChapter 9 The Endocrine SystemchastityNo ratings yet
- Haynes Et Al Poststress Recovery 1991Document10 pagesHaynes Et Al Poststress Recovery 1991Fabián OlazNo ratings yet
- Pituitary and Hypothalamus: The Body's Control Center: Lesson A2.2Document40 pagesPituitary and Hypothalamus: The Body's Control Center: Lesson A2.2Khobie PabilicoNo ratings yet
- Pituitary Tumors BrochureDocument20 pagesPituitary Tumors BrochureAnonymous M6HzvK6bNo ratings yet
- My LDDocument140 pagesMy LDAnanth Chaams100% (1)
- Bao Swaab 2011Document13 pagesBao Swaab 2011BeatrizCamposNo ratings yet
- Melanin What Makes Black People BlackDocument58 pagesMelanin What Makes Black People BlackAlfred IDunno100% (22)
- The Mechanisms of Postpartum DepressionDocument70 pagesThe Mechanisms of Postpartum Depressionazniahsyam8269No ratings yet
- Anatomy and Physiology of Adrenal GlandDocument26 pagesAnatomy and Physiology of Adrenal GlandYAMINIPRIYANNo ratings yet
- Signaling Pathways of EndocDocument1 pageSignaling Pathways of Endocashleighlong2014No ratings yet
- Kibreet With ImagesDocument260 pagesKibreet With Imagesعباس عبداللهNo ratings yet
- Clinical Manifestations of Adrenal Insufficiency in AdultsDocument13 pagesClinical Manifestations of Adrenal Insufficiency in AdultsAnonymous L7snCkaNo ratings yet
- Kuliah Patofisiologi Trauma - DR Raden Ajeng Sri WulandariDocument22 pagesKuliah Patofisiologi Trauma - DR Raden Ajeng Sri WulandariAgung Budi SuristioNo ratings yet
- Topic 1 Endocrine SystemDocument140 pagesTopic 1 Endocrine SystemmasdfgNo ratings yet
- Adrenal Function TestsDocument103 pagesAdrenal Function TestsPriyanshu MandalNo ratings yet
- Consideration of Steroids For Endodontic PainDocument11 pagesConsideration of Steroids For Endodontic PainArturo Trejo VeraNo ratings yet
- Anatomy and Physiology Chapter 17Document21 pagesAnatomy and Physiology Chapter 17Dawlat SlamaNo ratings yet
- The Metabolic and Endocrine Systems NotesDocument15 pagesThe Metabolic and Endocrine Systems Notesrozelle28No ratings yet