Professional Documents
Culture Documents
SAy Say
Uploaded by
Angelo Mercede0 ratings0% found this document useful (0 votes)
47 views8 pagesOriginal Title
SAy say.docx
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
47 views8 pagesSAy Say
Uploaded by
Angelo MercedeCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 8
GLUCOSE –standard spx venous plasma glucose
-fasting glucose in WB 15% lower than serum or plasma
-venous blood 7mg/dl lower than capillary blood; peritoneal fluid gluc same with plasma
-RT (20-25O)- glucose ↓7mg/dl/hr -Ref temp(4OC)- glucose ↓2mg/dl/hr
-Frozen Temp (-20OC)- almost 0mg/dl/hr decrease
I. CHEMICAL METHOD
a. Oxidation Reduction Method
1. Alkaline Copper Reduction Method-
-Reduction of cupric ions to cuprous ions forming cuprous oxide in hot alkaline sol. by glucose
*Alkaline Copper Tartrate ---glucose, heat- Cuprous ions
a. Folin Wu Method- Cuprous ions + Phosphomolybdate↓
Phosphomolybdic acid or Phosphomolybdenum blue
b. Nelson Somogyi- Cuprous ions + Arsenomolybdate ↓
Arenomolybdic acid or Aresnomolybdenum blue
c. Neocuproine Method (2,9 Dimethyl 1,10 Phenantroline Hydrochloride)
Cuprous ion + Neocuproine↓
Cuprous-Neocuproine Comples (yellow or Yellow orange)
d. Benedict’s Method (Modification of Folin-Wu)- detect and quanti reducing subs in body fluid
-use citrate or tartrate as stabilizing agent
2. Alkaline Ferric Reduction Method (Hagedorn Jensen)-
reduction of yellow ferricyanide to colorless ferrocyanide by glucose (Colorimetry)
b. Condensation Method
Ortho-toluidine (Dubowski Method)
Glucose + Aromatic amines ---Glacial HAC, heat glycosylamine + schiff’s base
II. ENZYMATIC METHOD- act on glucose but not on other sugard and not on other reducing subs
1. Glucose oxidase Method- measure B-D glucose
a. Colorimetruc Glucose Oxidase Method (Saifer Gernstenfield Method)
Glucose + O2 ---glucose oxidase Gluconic Acid + H2O2
H2O2 +Chromogenic subs ---peroxidase oxidized chromogenic subs + H2O
b. Polarographic Glucose Oxidase- meas rate of O2 consumotions, prop to gluc conc.
-conversion glucose quantified by consumption of O2 on oxygen-sensing electrode
-H2O2 prevented from re-forming O2 by adding molybdate, iodide, catalase and ethanol
Glucose +O2 ---glucose oxidase Gluconic Acid + H2O2
H2O2 + C2H5OH ---catalase CH3CHO + 2H2O
H2O2 + 2H + 2 I ---molybdate I2 + 2H2O
2. Hexokinase Method- most specific glucose method; reference method;
-plasma -- heparin, EDTA, fluoride, oxalate, or citrate; other sample urine, CSF, serous fluid
Glucose + ATP ---Hexokinase Glucose-6-Phosphate + ADP
G-6-P +NADP---G-6-PD 6Phosphogluconolactone +NADPH-reduced coenzyme meas.
3. Glucose Dehydrogenase Method- gluc red to prod Chrmophore meas by spectrophoto/ electric.
-Mutarotase- shorten time to reach equilibrium; endcolor blue
4. Dextrostics (cellular strip)- imp in establishing correct insulin amount for next dose
5. Interstitial Glucose Measuring Device- for continuous monitoring of glucose level in diabetic px
6. Glycosylated Hgh (HbA1c) or Glycated Hgb- monitoring
-represents a weighted average of glucose level, w/ youngest RBC contributing greater extent
-spx EDTA whole blood; Method electrophoresis, immunoassay, HPLC, Affinity Chromatography
-5.7-6.4% inc risk for diabetes; every 1% = 35mg/dl added to PG
CHOLESTEROL DETERMINATION- can be measure w/o fasting; measured as a whole
-Px prep-usual diet for 2 weeks, neither gaining nor losing weight
I. CHEMICAL METHOD- Principle: Dehydration and oxidation of cholesterol to form a colored compound
a. Lieberman Burchardt Reaction (Colorimetric) Endproduct= Cholestradienyl monosulfonic Acid (green color)
Color Developer Micture (LB rgt)’
-Glacial acetic acid -con. H2SO4
-acetoc anhydride
b. Salkowsk’s Reaction Endproduct= Cholestadieny Disulfonic Acid (red color)
>General Methods:
One Step Method- Colorimetry (Pearson, Stern and Mac Gavack)
Two Step Method- Extraction + Colorimetry (Bloors)
Three Step Method- Saponification + Extraction + Colorimetry (Abell-Kenda)
Four Step Method- Saponification+ Extraction + Colorimetry + Ppt. (Schoenheimer Sperry + Parekh + Jung)
II. ENZYMATIC METHOD- don’t required preliminary extraction step
Cholesterol Oxidase Reaction: commonly used/ routine test
Cholesterol Ester + H2O --chol esterase cholesterol + fatty acid
Cholesterol + O2—cholesterol oxidase cholest-4-en-3-one + H2O2
H2O2 + phenol + 4-aminoantipyrine –peroxidase quinoneimine dye
CDC reference method (Abell, Levy and Brodle Method)- 1-Saponification, 2-extration, 3-colorimetry
-use hexane extraction after hydrolysis w/ alcoholic KOH by rxn w/ Lieberman-Burchardt color reagent
TRIGLYCERIDE MEASUREMENT –hydrolyze all fatty acid esters of TAG to produce glycerol
I. CHEMICAL METHOD
a. Colorimetric Method (Van Handel & Zilversmith)
TAG—alcoholic KOHGlycerol + Fatty Acid
Glycerol Oxidized by Periodic Acid Formaldehyde (HCHO)
HCHO + Chromotropic Acid(+)Blue color compound
b. Fluorometric Method (Hanstzch Condensation)
TAG –alc. KOH Glycerol +FA
Glycerol Oxidized by Periodic Acid Formaldehyde (HCHO)
HCHO + Diacetyl Acetone + NH Diacetyl Lutidine Compound
II. ENZYMATIC METHOD
a. Glycerol Kinase Method- hydrolysis TAG to free FA and glycerol, then phosphorylation of glycerol to glyceropho
*CDC reference method (Modified Van Handel and Zilversmith)-colorimetric pink end color
Saponification- KOH (alkaline hydrolysis) Adsorption- Silicic acid Chrom (isolate TAG)
Extraction- Chloroform Color Reaction Chromotropic acid +TAG= PINK
Lipoprotein Methodologies:
-differentiated based on electrophoresis and buoyant density (ultracentrifugation) -TC-HDL-C=non HLD-C
1. Ultracentrifugation (density gradient)- reference method for quantitationof lipoproteins (LPPs)
-based on protein and TAG contents of lipoproteins; epressed in svedsverg(s) units
-Lipid density 1.0g/mL while Protein density 1.4mg/L
-Reagent: Potassium bromide solution w/ 1.063 density
2. Electrophoresis- Pattern: HDL, VLDL, LDL, Chylomicrons
-preferred supporting medium: Agarose-gel-speed; sensitive; resolves LLPs classes
-Lipid staining dyes: Oil Red O, Fat Red 7B or Sudan Black B
-VLDL migrates w/ a-2 globulin (preB); Chylomicrons if present remain at origin
3. Chemical Precipitation- uses polyanions ) and divalent cations such as Mg, Ca, manganese.
a. HDL- uses dextran sulphate (syntheric heparin) w/ magnesium (precipitants)
CDC reference 3-step: ultracentrifugation, heparin manganese precipitation and Abell-Kendall assay
b. LDL- EDTA plasma ..
4. Chromatographic method- utilizes Gel chromatography or affinity chromatography
5. Immunochemical methods0 uses AB specific to epitopes o apolipoproteins
6. Immunoassay or Immunonephelometry- Apolipoprotein assay
-meas turbidity created by apolipoprotein-Ab complexes
Friedewald Method (Indirect Method)
Formula for LDL-Cholesterol (LDL-C)= Total Cholesterol –HDL-VLDL
VLDL (mmol/L)= Plasma TAG/2.175 VLDL(mg/dL)= Plasma TAG/5
DeLong Method (Indirect Method)
VLDL(mmol/L)= Plasma TAG/2.825 VLDL(mg/dL)= Plasma TAG/6.5
KINDEY FUNCTION TESTS
1. BUN Determination: Fluorid, citrate inhibit urease; thriosemicarbazide and ferric ions enhance color
I. Chemical Method (Direct Method)- Diacetyl Monoxime Method Urea+DM Yellow diazine derivative
II. Enzymatic Method (Indirect Method)
a. Hydrolysis of Urea by Urease (Routine metho) Urea+Urease NH3 + CO2
-ammonia then treated with Berthelot rgt
b. Coupled Urease/ Glutamate Dehydrogenase (GLD) method- UV enzymatic method
Urea + Urease NH4 + CO2 NH4+2-oxoglutarate + NADH—GLD Glutamat+NAD+H2)
c. Isotope Dilution Mass Spectromoetry (IDMS)- Reference method
2. Creatinine
I. Chemical Method- Direct Jaffe Method: Red-orange tautomer of creatinine picrate is formed when creatinine
is mexed with alkaline picrate rgt
a. Folin Wu method- sensitive but nonspecific method
b. Lloyd or Fuller’s earth Method- sensitive and specific
Adsorbent: Lloyd’s reagent (Sodium aluminium silicate) Adsorbent: removes interference present
Fuller’s earth rgt (Aluminum Mg silicate) in spx and elution done to separate crea
Jaffe Reagent (Alkaline Picrate): Saturated Picric Acid; 10% NaOH
II. Kinetic Jaffe Method- serum mixed with alkaline picrate sol, rate of change in absorbance measured bet 2points
III. Enzymatic Method- routine method; specific than jaffe
a. Creatinine Aminohydrolase- CK method –require large vol of pre-incubated sample: not widely used
b. Creatinase Hydrogen Peroxide Method- Creatinase aka creatinine aminohydrolase
Creatinine + H2O—creatinase Creatine + H2O—creatinasesarcosine + urea
Sarcosine + H2O + O2—sacrosine oxidaseglycine + HCHO+ H2O2
H2O2+ phenol + 4-aminophenazone –peroxidase benzoquinonemine dye (Red)
IV. Isotope Dilution Mass Spectrometry (IDMS)- reference method
3. Blood Uric Acid-
I. Chemical Methods: Reduction-Oxidation (Redox) Reaction
Uric acid + Phosphotungstic Acid –NaCN/NaCO3Tungsten Blue + Allantoin + CO2
*Sodium cyanide—Folin NewtonBenedict Brown
*Sodium carbonate –Archibald Henry Caraway
II. Enzymatic Method
Uricase Method- routine, specific method
Uric acid has absorbance of 293nm, allantoin do not
Uric acid + O2 –uricase allantoim + CO2 + H2O
III. Isotope Dilution Mass Spectroscopy (IDMS)- reference method
Osmolality
a. Direct Method: Freezing point osmometry*; Vapor pressure osmometry (Seebeck effect) ↑Osmo↓FP,VP
b. Indirect Method: -use glocuse or urea in osmolality
Serum Osmolality= 1.86X Na = Gluc(mg/dL)/18 + BUN(mg/dL)/2.8
*Osmolal gap- difference between measured amd calculated plasma osmolality
LIVER FUNCTION TEST
I. Test Measuring Hepatic Synthetic Function- quantitate severity of hepatic dysfunction (Albumin, Vit-K dep CF)
A. Total Protein- RV: 6.5-8.3g/dL
a. Kjeldahl Method- measure Nitrogen(15.1-16.8%) content of CHON; referenc method; 1gN= 6.45g CHON
Serum + tungstic acid Protein-free filtrate (PFF)
-reagent: H2SO4 (digesting agent) -Endproduct: Ammonia
b. Biuret Method- widely used recommended by Int’l federation of clinical chemistry (IFCC) expert panel
-required at least 2 peptide bonds and an alkaline medium
-Principle: Cupric ions complex groups involved In peptide bond forming violet-colored chelate, proportional to
number of peptide bonds present and represent total protein level @454nm
-Reagents: Alkaline Copper Sulfate, Rochelle Salt (NaK Tartrate), NaOH and K iodide
c. Folin-Clocateu (lowry) Method- highest analytical sensitivity
-Priciple: Oxidation of phenolic compounds such as tyrosine, tryptophan, histidine deep blue color
-Reagent: Phosphotungstic-molybdic acid or phenol reagent; Biuret rgt (color enhancer)
d. Ultraviolet Absorption Method- absorbance of CHON @210nm due to abs. of peptide bonds @speci. waveL
e. Serum Protein Electrophoresis (SPE)- migration of charged paticle in an electric field
-important in ID or monoclonal spike of Ig and differentiating them from polyclonal hypergammaglobulinemia
Normal SPE pattern:
Albumin (1st band)- fastest band 53-65%
Alpha 1-Globulin (2nd fastest)- glycoproteins, AAT, AAG, TBG; inc in nonspecific response to inflammation
Alpha 2-globulin (3rd fastest)- haptoglobin, AMG, ceruloplasmin 7-13%
Beta-globulin (4th band)- transferrin, beta-lipoprotein, hemopexin, complement (C3, C4) 8-14%
Gamma-globulin (5th band)- immunoglobulin and CRP 12-22%
Abnormal Serum Electrophoretic Patterns:
i. Gamma spike- multiple myeloma iv. a1-globulin flat curve0 juvenile cirrhosis (AAT deficien.)
ii. beta-gamma bridging- hepatic cirrhosis v. Spikes of a1, a2, B globulin bands- inflammation
iii. a2-globulin band spike- nephrotic syndrome
f. Refractometry- alternative test to chem analysis of serum total protein; refractive index of solutes in serum
g. Turbidimetric and Nephelometric Method- utilizes SSA and TCA
h. Salt Fractionation- globulins can be separated from albumin by salting-out procedures using Na salts
-Rgt: Sodium Sulfate Salts
B. Prothrombin Time (Vit K Response Test)- diff intrahepatic disorder (prolong PT) from extrahepatic obs (NO PT)
Albumin/Globulin Ratio- validate if globulin is higher than albumin
-if globulin > than alb= inverted A/G ratio: cirrhosis, multiple myeloma, Walderstrom’s macroglobulinemia
-RV: 1.3:1 to 3:1
II. Test Measuring Conjugation and Excretion Function *bili (mg/dL) x17.1 (mmol/L)
A. Bilirubin Assay –unconjugated bilirubin reacts slowly, accelerants (Caffeine and Methanol) meas Total Bili
-deletion of accelerants allow determination of direct-reacting or conjugated bilibun
-Accelerators allow indirect bilirubin to react (solubilize) w/ the color reagent; read after 15min
Principle: Van den Berg Reaction- diazotization of bilirubin to produce azobilirubin
a. Evelyn and Malloy Method: Coupling Accelerator Methanol *PINK to PURPLE azobilirubin
b. Jendrassik and Grof*: Coupling Accelerator Caffeine Sodium Benzoate Buffer: Sodium Acetate
*PINK to BLUE azobilirubin
B. Bromsulfonthalein (BSP) Dye Extraction Test –test for hepatocellular func and potency of bile duct
a. Rosenthal White (Double Collection)- dose 2mg/kg BW; collect after 5min(50%) and 30min(0% dye retention)
b. Mac Donald Method (Single Collection)- dose 5mg/kg; collect spx after 45min; NO= +/- 5% dye retention
III. Test for Detoxification Function- involves enzymes and ammonia tests
A. Enzyme Test-assess extent of liver damage & diff. hepatocellular (functional) from obstruct (mechan) disease.
-enzymes secreted by liver: ALP, aminotransferases, 5’nucleotidase, GGT, OCT, LAP, LD
B. Ammonia- from deamination of AA, converted by liver to uea RV: 19-60ug/dL (11-35mmol/L)
↑cirrhosis, hepatitis, Reye’s syndrome, chronic renal disease and acetaminophen poisoning
ENYMES
^Alkaline Phosphatase^
1. Electrophoresis- Liver, Bone most Anodal (neuraminidase,wheat germ lectin-separ.); intestinal ALP least anodal
- High-resolution electrophoresis using polyacrylamide gel and isoelectric focusing resolve bands of ALP
2. Heat Fractination/Stability Test- performed @ 56OC for 10-15min
-placental ALP (most heat stable); bone ALP most heat labile; Order decresing: Placenta, Intestinal, Liver, B
3. Chemical Inhibition Test- use diff conc of phenylalanine, synthetic urea and levamisole
-P and I inhibited by phenylalanine rgt ; 3M urea inhibit Bone; Levamisole inhibit L and B ALP
4. Bowers and Mc Comb (Szasz modification)-most specific method IFCC recommended
-continous-monitoring technique requiring a pH 10.15 and read @405nm
p-nitrophenylphosphate ←ALP→p-nitrophenol + phosphate ion
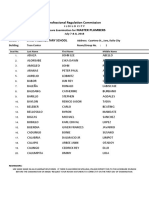
Method Substrate End Product
1. Bodansky
2. Shinowara Beta-glyceroPO4 InorganicPO4 + Glyverol
3. Jones
4. Reinhart
5. King and Armstrong Phenylphosphate Phenol
6. Bessy Lowry & Brock p-nitro phenyl PO4 (PNPP) p-nitrophenol or yellow
nitrophenozide ion
7. Bowers and McComb PNPP p-nitrophenol or yellow
nitrophenozide ion
8. Huggins and Talalay Phenolphthalein PO4 ALpa-naphtol
9. Moss Alpha naphthol PO4 Alpha- naphthol
10. Klein, Babson and Read Buffered phenolphthalein PO4 Free phenolphthalein
-Refrigeration leads to inc ALP; ALP inhibited by phosphorous; Zinc component of ALP
^Acid Phosphatase^ Summary of ACP Methods
Method Substrate End Product
1. Gutman and Gutman Phenyl PO4 Inorganic PO4
2. Shinowara PNPP p-nitrophenol
3. Babson, Read and Phillips Alpha naphthyl PO4-continuous Alpha-naphtol
mon
4. Roy and Hillman Thymolphthalein MonoPO4* Free thymolphthalein
*Tartrate-resistant Acid Phosphatase (TRAP)- present in certain chronic leukemia, esp Hairy Cell Leukemia
*Postatic ACP used together w/ Prostate Specific Anitgen (PSA) to monitor recurrence of prostate cancer
^Aspartate Aminotransferase^
Karmen Method- pH 7.5; 340nm- use malate dehydrogenase (MD), monitor change in absorbance at 340nm
Aspartate + a-ketoglutarate ←AST→ Oxaloacetate + Glumate
Oxaloacetate + NADH + H ←MD→ Malate + NAD
^Alanine Aminotransferase^ -present in plasma, bile, CSF, saliva; require pyridoxal phosphate (vitB6) as coenzym
Coupled Enzymatic Reaction: using pH 7.5 @340nm
Alanine + a-ketoglutarate ←ALT→ Pyruvate + Glutamate
Pyruvate + NADH + H ←LD→ Lactate + NAD
AST/ SGOT ALT/ SGPT
Major Organ Affected Heart Liver
Substrate Aspartic a-ketoglutaric acid Alanine a-ketoglutaric acid
End Product Glutamic Acid + Oxaloacetic Acid Glutamic Acid + Pyruvic Acid
Color Developer 2,4 DNPH 2,4 DNPH
Color Intensifier 0.4N NaOH 0.4N NaOH
Method Reitman and Frankel Reitmand and Frankel
*De Ritis Ratio (ALT:AST) > 1.0, seen in acute hepatitis
^Amylase/ Alpa-1-4-Glucohydrolase (AMS)^ Substrate for all methods Starch- polysaccharide, carbohydrate
1. Saccharogenic- reference method expressed in Somogyi units;
-measure reducing sugars prod by hydrolysis of starch by the usual glucose method
2. Amyloclastic –measure amylase activity by following decreases in substrate conc (defradation of starch)
3. Chromogenic- meas amylase activity by increase in color intensity of soluble dye-substrate sol prod in rxn
4. Coupled-enzyme- measure amylase activity by a continuous-monitring technique
^Lipase/ Triacylglycerol Acylhydrolase (LPS)^
-uses Olive oil as substrate bec other esterases can hydrolyze TAG and syntheric diglycerides
-Collipase (CHON from pancreas) and Bile salts- make assay more sensitive and specific
1. Cherry Crandal (reference method)- substrate 50%olive oil; End product Fatty Acid
-Hydrolysis of olive oil after incubation for 24hrs @37OC and titration of FA using NaOH
TAG (olive oil) +2H2O ←LPS→ 2-monoglyceride + 2 Fatty acids
2. Tiets and Flereck
3. Peroxidase coupling- most common; doesn’t use 50% olive oil
^Lactate Dehydrogenase^ -Lactate more specific substrate than pyruvate; LD1 prefer forward; LD5 reverse rnx
1. Wacker Method (forward/direct reaction)- reaction @ pH 8.8; most common
Lactate + NAD –LD Pyruvate + NADH @340nm
2. Wrobleuski La Due (reverse/ indirect reaction)- reaction @ pH7.2; 2x faster; prefer for dry slide technology
Pyruvate + NADH –LD Lactate + NAD
3. Wrobleuski Cabaud
4. Berger Broida
^Creatine Kinase (CK)
1. Tanzer-Gilbarg Assay (forward/direct method) –pH9.0 @340nm
Creatine + ATP –CKCreatine PO4 + ADP + Phosphoenolpyruvate ←PK→ Pyruvate + ATP
Pyruvate + NADH ←LD→ Lactate + NAD
2. Oliver-Rosalki (reverse/indirect method)-most common; faster; pH 6.8 @340nm
Creatine PO4 + ADP –CPK Creatine + ATP + glucose ←hexokinase→ ADP+ glucose-6-PO4
Glucose-6-PO4 + NADP ←G-6-PD→ 6-phosphogluconaye + NADPH
3. Electrophoresis- reference method
*Adenosine monophosphate (AMP)- added to reverse method to inhibit AK (Adenylate kinase)-it hydrol ADP
*imidazole- buffer; urate and cysteine- potent inhibitor of CK; CK light and pH sensitive
^Sodium and Potassium^- use heparinized blood
1. Emission Flame Photometry
2. Ion Selective Electrode (Valinomycin gel)
3. Atomic Absorption Spectrophotometry
4. Colorimetry (Lockhead and Purcell)
^Chloride^
1. Mecurimetric Titration (Schales and Schales) -Diphenylcarbazone –indicator; HgCl2 (blue violet)=end p
2. Spectrophotometric Methods Mercuric Throcyanate (Whiterhorn Titration Method) =Reddish complex
Ferric Perchlorate =colored complex
3. Coulometric Amperometric Titration –Cotlove Chloridometer- Sweat Chloride (cystic fibrosis)
4. Ion Selective Electrode-using ion exchange membrane (tri-n-octylpropylammonium chloride decanol); common
^Calcium^ -serum
1. Precipitation and Redoc Titration: Clark Collip ppt- endproduct (purple color)
Ferro Ham Chloranilic Acid ppt- endproduct: Chloranilic acid (purple color)
2. Ortho-Cresolpthalein Complexone Dyes (Coloremetric Method) Dye: Arzeno III
3. EDTA Titration Method (Bachra, Dawer and Sobel)
4. Ion Selective Electrode (Liquid membrane)
5. Atomic Absorption Spectrophotometry-reference method
6. Emissio Flame Photometry
^Inorganic Phosphorus^- require fasting, high CHO diet dec level; only inorganic phosphate is measured
-affected by circadian rhythm- high level late morning, low in evening
1. Fiske Subbarow Method (Ammonium Molybdate method)- most common
-Reducing agent: *Pictol (Amino Naphthol Sulforic Acid); elon, senidine
-Endproduct: Ammonium molybdate complex (unstable); Reduced form blue color det bet 600 to 700nm
^Magnesium^
1. Colorimetric Methods
a. Calmagite Method= (+) Reddish-violet complex
b. Formazen Dye Method= (+) Colored complex
c. Magnesium Thymol Blue Method= (+) Colored complex
2. Atomic Absorption Spectrophotometry- reference method
3. Dye-Lake Method- Titan Yellow Dye (Clayton Yellow or Thiazole Yellow)
^Bicarbonate^ -spx blood anaerobically collected
1. Ion selective electrode (using pCO2 electrode)
2. Enzymatic (Phosphoenolpyruvate carboxylase and dehydrogenase)
*Cystic Fibrosis-
Sweat Inducer: Pilocarpine]
Diagnostic test:Sweat-teest Coulometry (↑Sodium and Cl)
Reference Method: Gibson and Cooke Pilocarpine Iontophoresis
>50mg sweat sample collected w/in 30min
(+) Result: >65 mmol/L sweat electrolytes (RV: 5-40mmol/L)
*Iron
1. Colorimetry (HCl and ferrozine) –(+) Blue Color
2. Anodic Stripping Voltammetry- 1st separation form transferrin by acidification,
^Blood Gas^- spx Arterial Blood; Anticoagulant: 0.05mL heparin/mL blood
1. Gasometer 2. Electrodes
a. Van Slyke a. pH (potentiometry)
b. Natelson i. Silver-silver chloride electrode- reference electrode
i. mercury- to produce vacuum ii. Calomel electrode (Hg2CL2)- reference electrode
ii. caprylic alcohol- anti-foam reagent iii. Gas electrode- most common, used for pH
iii. Lactic acid b. pO2 Clark electrode- polarography-amperometry
iv. NaOH and NaHSO3 c. pCO2 Severinghaus electrode –potentiometry
Thyroid Function Test:
1. TRH Stimulation Test (Thryrotropin Releasing Hormone)- measure relationship bet TRH and TSH secretions
-differentiate euthyroid and hyperthyroid Px w/ both undetected TSH; detect thyroid hormone resistance synd.
-↑1O hypothyroidism; ↓hyperthyroidism
2. TSH Test- most important thyroid function test- best from detecting clinically significant thyroid dysfunction
-detect 1O thyroid disorfers; differentiate 1O from 2Ohypothyroidism
↑1O hypothyroidism, hashimoto’s thyroiditis. TSH Ab; ↓1O hyperthyroidism, 2O and 3O hypothyroidism
3. Radioactive Iodine Uptake (RAIU)- measure ability of thyroid gland to trap iodine; ..hyperthyroidism
-high uptake =metabolically active; high uptake + TSH deficiency= autonomous thyroid activity
4. Thyroglobulin (Tg) assay- normally used as postoperative marker thyroid cancer,
↑untreated and metastatic differentiated thyroid cancer, nodular goiter and hyperthyroidism
↓infants w/ goitorous hypothyroidism and thyrotoxicoxis factitia
Method: double-Ab RIA, ELISA, IRMA, immunochemiluminescent assay (ICMA)
5. Reverse T3 (rT3)- formed by removal one iodine from inner ring of T4; enproduct of T4 metabolism
-identifies px w/ euthyroid sick syndrome (↑rT3)
6. Free Thyroxine Index (FTI or T7)- indirectly assess level of free T4 in blood;↑hyperthyroidism; ↓hypothyroid
7. Total 3 (TT3), Free T3 (FT3) and FreeT4 (FT4)- FT4 used to differentiate drug induced TSH elev and hypothyroid
-TT3 or FT3 confirm hyperthyroidism; direct/reference method: Equilibrium dialysis (FT4)
8. T3 Uptake- measure number available binding sites of thyroxine-binding proteins, a test for TBG
-reflects serum level of TBG, inversely related to TBG- ↓T3 uptake ↑TBG, vice versa
↑hyperthydoisim, ↓hypothyroidism
9. Thyroxine binding globuline (TBG)- confirm results of FT3 and FT4, or abnormalities in relation to TT4 and THBR
-hyperthydoism (↑T4 + NO TBG); euthyrdoism (↑T4 and TBG); hypothyroidism ↓TBG
10. Fine-needle aspiration- most accurate tool in evaluation of thyroid nodules
11. Recombinant Human TSH- test pc w/ thyroid cancer
12. Tanned Erythrocyte Hemagglutination- measure antithyroglobulin Ab
13. Serum Calcitonin- tumor marker for detecting thyroid metastasis in medullary thyroid carcinoma
14. Pentagastrin (Pg) Stimulation Test- diagnose MTC
^Pheochromocytoma^: Pharmacologic Tests:
a. Clonidine Tests- diff. pheochromocytoma (not suppressed) to neurogenic hypertension (50% ↓catecholamine)
b. Glucagon Stimulation Test- for indiv w/ normal blood pressure and when catecholamines only modestly elev.
^Neuroblastoma^ Spx: 24hr urine and blood (plasma)
a. Chromatography- HPLC or GC-MS (VMA and metanephrines)
b. Radioimmunoassay- sensitive screening test for total plasma catecholamines
>2000pg/mL plasma catecholamines- diagnostic for pheochromocytoma
-Urine preservation: 10mL 6N HCl
^Hormonal Assay^
1. Whole blood- LH, testosterone
2. Plasma- EDTA (ACTH, ADH, PTH) and Heparin (Catecholamines, cortisol, dopamine, FSH)
3. Serum- aldosterone, androstenedione, DHEA, estrogen, FSH, GH, HCG, progesterone
4. Urine- for measurement of estriol
-Boric acidin a concentration of 1g/dL urine elements such as estriol and estrogen for up to 7days
-for catecholamines, VMA, 5-HIAA collections, 10mL 6N HCl in 3-4L container
-HCl establishes a pH of approximately <3.0, good for chemical testing
a. Classical Assay
-Bioassay-
- Competitive Protein Binding (CPB)
b. Immunologic Assays
-Radioimmunoassay (RIA)
-Immunoradiometric (IRMA)
-Enzyme-Linked Immunosorbent Assay (ELISA)
-Enzyme Multiplied Immunosorbent Technique (EMIT)-for TDM
-Immunometric- for TSH
c. Fluorescent Technique- FPIA
d. High Performance Liquid Chromatography (HPLC)
e. Colorimetry
i. Porter-Silber Method- for 17-OHCS
ii. Zimmerman Reaction- measure those steroid w. 17-keto structure
iii. Pisano Method- for quantitating metanephrines and normetanephrines
iv. Kober Reaction- for estrogen (H2SO4 + hydroquinone = (+) reddish-brown color
You might also like
- RA SOCIALWORKER TUGUE July2018 PDFDocument10 pagesRA SOCIALWORKER TUGUE July2018 PDFPhilBoardResultsNo ratings yet
- RA SOCIALWORKER PAGADIAN July2018 PDFDocument27 pagesRA SOCIALWORKER PAGADIAN July2018 PDFPhilBoardResultsNo ratings yet
- Ra Radtech Cdo July2018Document4 pagesRa Radtech Cdo July2018Angelo MercedeNo ratings yet
- Opto WRDocument1 pageOpto WRAngelo MercedeNo ratings yet
- Ra Socialworker Legazpi July2018Document11 pagesRa Socialworker Legazpi July2018Angelo MercedeNo ratings yet
- Opto C18Document11 pagesOpto C18Angelo MercedeNo ratings yet
- RA SOCIALWORKER CEBU July2018 PDFDocument8 pagesRA SOCIALWORKER CEBU July2018 PDFPhilBoardResultsNo ratings yet
- Ra Socialworker Davao July2018Document42 pagesRa Socialworker Davao July2018Angelo MercedeNo ratings yet
- RA SOCIALWORKER MANILA July2018 PDFDocument36 pagesRA SOCIALWORKER MANILA July2018 PDFPhilBoardResultsNo ratings yet
- RA RADTECH TUGUE July2018 PDFDocument10 pagesRA RADTECH TUGUE July2018 PDFPhilBoardResultsNo ratings yet
- Ra Xray Cdo July2018Document1 pageRa Xray Cdo July2018Angelo MercedeNo ratings yet
- Ra Radtech Cebu July2018Document8 pagesRa Radtech Cebu July2018Angelo MercedeNo ratings yet
- RA MASTERPLUMBING ILOILO July2018 PDFDocument4 pagesRA MASTERPLUMBING ILOILO July2018 PDFPhilBoardResultsNo ratings yet
- Ocular 18Document1 pageOcular 18Angelo MercedeNo ratings yet
- RA MASTERPLUMBING DAVAO July2018 PDFDocument18 pagesRA MASTERPLUMBING DAVAO July2018 PDFPhilBoardResultsNo ratings yet
- RA MASTERPLUMBING TACLOBAN July2018 PDFDocument6 pagesRA MASTERPLUMBING TACLOBAN July2018 PDFPhilBoardResultsNo ratings yet
- Clinical Chem 2016Document13 pagesClinical Chem 2016Angelo MercedeNo ratings yet
- RA MASTERPLUMBING CEBU July2018 PDFDocument21 pagesRA MASTERPLUMBING CEBU July2018 PDFPhilBoardResults0% (1)
- Mycology VirologyDocument16 pagesMycology VirologyAngelo MercedeNo ratings yet
- Questionnaire CC 1Document16 pagesQuestionnaire CC 1Rasty BakuNo ratings yet
- Questionnaire (HM)Document15 pagesQuestionnaire (HM)Angelo Mercede100% (2)
- Questionnaire (HTMLE)Document16 pagesQuestionnaire (HTMLE)Angelo Mercede100% (1)
- Recall Questions September 2014Document6 pagesRecall Questions September 2014Angelo MercedeNo ratings yet
- Questionnaire (CM)Document15 pagesQuestionnaire (CM)Angelo MercedeNo ratings yet
- CC Musttoknow RodriguezDocument44 pagesCC Musttoknow RodriguezAngelo Mercede100% (1)
- MicroPara Viro Questions by ApollonDocument13 pagesMicroPara Viro Questions by ApollonAngelo MercedeNo ratings yet
- Sept 2015 Sample ExamDocument22 pagesSept 2015 Sample ExamAngelo MercedeNo ratings yet
- Questionnaire (MP)Document15 pagesQuestionnaire (MP)Angelo MercedeNo ratings yet
- Questionnaire (ISBB)Document14 pagesQuestionnaire (ISBB)Angelo Mercede100% (1)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Neonatología PolinDocument601 pagesNeonatología Polinnohemi baezNo ratings yet
- 【Zybio】EXI 1800 Series Price List-Published V6.0Document3 pages【Zybio】EXI 1800 Series Price List-Published V6.0Grupo CatamedicNo ratings yet
- Interpretation of Laboratory Thyroid Function Tests: The "Hidden" Health ProblemDocument38 pagesInterpretation of Laboratory Thyroid Function Tests: The "Hidden" Health Problemalanoud.877No ratings yet
- Diagnosis of and Screening For Hypothyroidism in Nonpregnant AdultsDocument22 pagesDiagnosis of and Screening For Hypothyroidism in Nonpregnant AdultsJoseline Stephanie Pérez ChacónNo ratings yet
- Thyroid Function Test PDFDocument2 pagesThyroid Function Test PDFAlizaPinkyNo ratings yet
- TDAH ADHD e Def de Iodo 2004Document7 pagesTDAH ADHD e Def de Iodo 2004Pollyana Furtado JunqueiraNo ratings yet
- Foods To Avoid If You Have Thyroid Problems 1Document7 pagesFoods To Avoid If You Have Thyroid Problems 1Arinda PatriciaNo ratings yet
- H-046-003247-00 TT3 KIT (CLIA) Muti LaguageDocument14 pagesH-046-003247-00 TT3 KIT (CLIA) Muti LaguageSinari AlfatNo ratings yet
- Monobind Assay Technical GuideDocument16 pagesMonobind Assay Technical GuideLuis GomezNo ratings yet
- Sashikant Modi Comprehensive Full Body Checkup Includes 107 Tests 12092017 131456Document9 pagesSashikant Modi Comprehensive Full Body Checkup Includes 107 Tests 12092017 131456Sashikant ModiNo ratings yet
- Pathophysiology of EndocrinologyDocument25 pagesPathophysiology of EndocrinologyISRAELNo ratings yet
- Lyphochek Assayed Chemistry Control Levels 1 and 2: Tanggal Revisi 2023-04-06 Menunjukkan Informasi Yang DirevisiDocument8 pagesLyphochek Assayed Chemistry Control Levels 1 and 2: Tanggal Revisi 2023-04-06 Menunjukkan Informasi Yang Direvisiheru ramadhanNo ratings yet
- Thyroid Function TestDocument2 pagesThyroid Function Testhannah lanasaNo ratings yet
- 07122022am326c71270060893425 RLSDocument2 pages07122022am326c71270060893425 RLSPt computerNo ratings yet
- TiroideDocument10 pagesTiroideRosália CoutadaNo ratings yet
- Biomarkers of AgingDocument12 pagesBiomarkers of AgingLjón BjörnNo ratings yet
- Management of Hypothyroidism and Hypothyroxinemia During Pregnancy-AaceDocument8 pagesManagement of Hypothyroidism and Hypothyroxinemia During Pregnancy-Aacegu mailNo ratings yet
- Congenital Hypothyroidism: Screening, Diagnosis, Management, and OutcomeDocument7 pagesCongenital Hypothyroidism: Screening, Diagnosis, Management, and OutcomeIbrahim Abdul KareemNo ratings yet
- VIDAS Menu Jan 2016Document2 pagesVIDAS Menu Jan 2016طلال الخولانيNo ratings yet
- Mrs Anar DeviDocument14 pagesMrs Anar DeviM.DNo ratings yet
- NBME 7 Block-1 PDFDocument52 pagesNBME 7 Block-1 PDFzdakra60% (10)
- Normal Ranges For Thyroid Function Tests in Infants and ChildrenDocument1 pageNormal Ranges For Thyroid Function Tests in Infants and ChildrenjuanungaNo ratings yet
- Cobas e 411 COBI-CD 1.1 EN PDFDocument89 pagesCobas e 411 COBI-CD 1.1 EN PDFKanva NagarbhaviNo ratings yet
- Euthyroid Sick SyndromeDocument3 pagesEuthyroid Sick Syndromemonday125No ratings yet
- Pedendo Proceedings Book Foutput Ok 2019 Permasalahan Dalam Skrining Hipotiroid Kongenital DiDocument186 pagesPedendo Proceedings Book Foutput Ok 2019 Permasalahan Dalam Skrining Hipotiroid Kongenital DiDamar Prasetya, Sp.ANo ratings yet
- Thyroid Disorders (Final Draft)Document17 pagesThyroid Disorders (Final Draft)mogesie1995No ratings yet
- @MedicalBooksStore 2007 Self AssessmentDocument289 pages@MedicalBooksStore 2007 Self AssessmentOkka Soe OoNo ratings yet
- Agappe I1000 Clia - CPT NewDocument2 pagesAgappe I1000 Clia - CPT Newsrikanth7210No ratings yet
- Hyperthyroidism Article PubmedDocument12 pagesHyperthyroidism Article PubmedSandu AlexandraNo ratings yet
- MTAPDocument19 pagesMTAPCaressa Marie EstradaNo ratings yet