Professional Documents
Culture Documents
Nejm CER Consent Kass
Uploaded by
Sasha Hidayat FullOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Nejm CER Consent Kass
Uploaded by
Sasha Hidayat FullCopyright:
Available Formats
The n e w e ng l a n d j o u r na l of m e dic i n e
H e a l t h L a w, E t h i c s , a n d H u m a n R i g h t s
Mary Beth Hamel, M.D., M.P.H., Editor
Informed Consent, Comparative Effectiveness,
and Learning Health Care
Ruth R. Faden, Ph.D., M.P.H., Tom L. Beauchamp, Ph.D., and Nancy E. Kass, Sc.D.
Interest in learning health care systems and in We also have put forward an ethics framework
comparative-effectiveness research (CER) is ex- for learning health care to serve as the moral
ploding. One major question is whether in- foundation for a learning health care system.2
formed consent should always be required for Our Common Purpose Framework builds on
randomized comparative-effectiveness studies, traditional principles of clinical and research
particularly studies conducted in a learning health ethics, including the Belmont Report, but is de-
care system. Our answer to this question is no. signed to provide guidance for activities in which
It will often be unethical to go forward with research and practice are integrated to enable
CER in which patients are randomly assigned to rapid, systematic learning. The Framework com-
different interventions without their written, pro- prises seven moral obligations: first, respect the
spective, informed consent. However, in a mature rights and dignity of patients; second, respect the
learning health care system with ethically robust clinical judgments of clinicians; third, provide
oversight policies and practices, some random- optimal care to each patient; fourth, avoid im-
ized CER studies may justifiably proceed with a posing nonclinical risks and burdens on patients;
streamlined consent process and others may not fifth, reduce health inequalities among popula-
require patient consent at all. tions; sixth, conduct activities that foster learn-
The current oversight system, requiring in- ing from clinical care and clinical information;
formed consent for most clinical research, grew and seventh, contribute to the common purpose
out of a scandal-ridden period in which people of improving the quality and value of clinical
were included in research and exposed to con- care and health care systems. The first six obli-
siderable risk without their knowledge or consent. gations fall on researchers, clinicians, health care
In intervening decades, the clinical-research administrators, institutions, payers, and insurers.
enterprise has changed. Some research, includ- The seventh falls on patients to participate in
ing some CER, may pose only minimal risks, certain types of learning activities that will be
yet the potential effect on patients’ welfare of integrated with their clinical care.
answering the core question of CER — which Extensive consultation with patients and other
standard interventions work best for whom — stakeholders is necessary for appropriate speci-
is immense. fication of the institutional implications of the
Elsewhere we have presented an ethical justi- Framework. All involved must appreciate that
fication for the transition to a learning health they are receiving care or working in an institu-
care system and for the streamlining of both tion committed to the shared mission of con-
consent requirements and oversight practices tinuous learning that feeds directly into improv-
within the system.1,2 A key premise in our justi- ing patient care. An ethical learning health care
fication is that current consent and oversight system must have core commitments to engage-
practices too often overprotect patients from re- ment, transparency, and accountability in ways
search that has little effect on what matters to that are keenly sensitive to the rights and inter-
patients, whereas in other cases oversight prac- ests of patients. Patients will be engaged in two
tices underprotect patients from medical errors respects: by helping to set the CER priorities of
and inappropriate medical management because the system and by serving on ethics-oversight
they make research to reduce these problems panels that will review proposed CER studies in
unduly burdensome to conduct. light of the obligations of the Common Purpose
766 n engl j med 370;8 nejm.org february 20, 2014
The New England Journal of Medicine
Downloaded from nejm.org by Robert Califf on February 19, 2014. For personal use only. No other uses without permission.
Copyright © 2014 Massachusetts Medical Society. All rights reserved.
Health Law, Ethics, and Human Rights
Framework and other ethical requirements and Consider also a pragmatic, randomized clini-
determine the appropriate forms of consent and cal trial that compares two widely used hyper-
authorization. tension medications, perhaps two diuretics, and
In this system, all patients will be told that in which there are no delineated clinical charac-
patients serve on ethics-oversight panels and how teristics that would favor one drug over another
they operate. The panels will determine whether for many patients. Although an algorithm iden-
particular CER (and quality-improvement) activi- tifies eligible patients, treating physicians make
ties fall above or below a threshold of negative the final enrollment determination. Physicians
effect on expected clinical outcomes or other and patients can override the randomized choice.
outcomes or values that matter morally to pa- Physicians may change drugs, adjust dosages, or
tients. Research that falls below the threshold add therapies for any patient at any time. This
will be integrated into clinical care without spe- study is unlikely to negatively affect expected
cific notification to or consent from individual clinical outcomes for patients, and respect for
patients; however, public notification will be pro- physician judgment is maintained. The drugs
vided to the community of the system, including are similar in administration and side-effect
patients. Other CER studies, determined by panels profiles, both drugs have acceptable side-effect
to have minor but still meaningful effects on profiles, and adverse events are rare. It is un-
patients’ interests, will proceed with specific likely that patients would have personal prefer-
notification to affected patients, who will have ences for one drug over the other. This trial
an option to decline participation. Still other therefore accords well with the obligations in
studies, determined to be clearly above the the Common Purpose Framework requirements.3
threshold, will require prospective, written, in- In a mature learning health care system of the
formed consent before proceeding. The system sort that we envision, simply telling patients
will thus aim to counteract problems of both about the study through a streamlined process
underprotection and overprotection. and giving them an opportunity to decline par-
Transparent mechanisms will ensure that pa- ticipation would be an ethically acceptable, war-
tients and other stakeholders can easily learn ranted mechanism of authorization. It may even
which CER studies are ongoing. In addition, and be acceptable for an ethics-oversight panel to
critically, a learning health care system will be permit the study to proceed with broad notifica-
accountable for rapid modifications of clinical tion to the community of the system, without
practice that are supported by CER findings and requiring that individual patients be told about
for providing public reasons when modifications the randomization.
are not made. However, some randomized CER studies in
In learning health care systems with these learning health care systems cannot be ethically
ethically robust practices, it will be ethically ac- authorized by either of these mechanisms. Ex-
ceptable for some randomized CER studies, hav- plicit informed consent will be required if risk,
ing no or only minor effects on important patient uncertainty, or informational need is higher. In-
interests, to proceed without informed consent cluded would be studies in which the prospect
from or specific notification to individual pa- of differential clinical outcomes or considerable
tients. Consider, for example, randomized stud- risk looms large as well as studies in which in-
ies that compare the effectiveness of sending terventions are different in terms of other con-
medication reminders by text or e-mail to pa- siderations that matter to patients. Consider a
tients who have previously given permission to study that randomly assigns patients with back
be contacted by either mechanism or the useful- pain to acupuncture or to a home exercise regi-
ness of repeating a routine laboratory test once men or that randomly assigns patients with scoli-
or twice during a patient hospitalization when osis to surgery or to bracing. Even if the alterna-
both are standard practice. In a mature learning tive treatments were considered standard practice
health care system, an ethics-oversight panel and even if clinicians were uncertain and evi-
might justifiably approve the integration of these dence was lacking about which is more effec-
studies into clinical care routines with only tive, the two options have such different impli-
public notification to the community of the sys- cations for patients’ lives that informed consent
tem that the research is being conducted. is essential. Among the critical functions of hav-
n engl j med 370;8 nejm.org february 20, 2014 767
The New England Journal of Medicine
Downloaded from nejm.org by Robert Califf on February 19, 2014. For personal use only. No other uses without permission.
Copyright © 2014 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
ing substantial patient engagement in ethics the streamlined process, physicians would in-
oversight of CER (and other research) in learning form their patients about the study and the use
health care is to ensure that patients’ values, be- of randomization. Their explanations would be
yond their interest in securing the best possible brief, akin to the conversation that physicians
clinical outcomes, are respected. typically have with patients about a new pre-
Our position that informed consent is not a scription, and accompanied by a short, written
morally necessary condition for the conduct of description. Patients would be given an oppor-
all randomized CER assumes a learning health tunity to opt out of the research and to learn
care system grounded in a set of moral commit- more if they wish, but patients would not be
ments against which specific studies have been asked for written informed consent. This ap-
vetted and found to satisfy the conditions that proach could be designed to be respectful of pa-
permit authorization through processes other tients and less burdensome for them and for
than informed consent. The transformation to a clinicians than the lengthier process entailed
learning health care system is still in its infan- by current informed-consent requirements, there-
cy, and no system on the path to this important by increasing the numbers of clinicians willing
goal has yet to adopt an ethical framework with to take part and increasing the numbers of im-
accompanying policies and practices of the sort portant clinical questions that can be addressed.
we are proposing. However, the Common Pur- Clinical research varies widely in the risks
pose Framework can provide helpful guidance to which patients are exposed and the degree to
in current health care settings. Some random- which research alters the care that patients re-
ized CER studies that would assess favorably ceive in ways that matter to them. The impor-
against the first four obligations of the Frame- tance of streamlining oversight and consent re-
work could proceed ethically with a streamlined quirements, so that higher-risk research gets
consent process. These include studies that, in the focused attention it deserves and less conse-
comparison with what patients would otherwise quential research can proceed more rapidly, is
encounter in their care, have no expected nega- increasingly being acknowledged. As more low-
tive effects on clinical outcomes or on other risk CER is planned, it will be essential to iden-
considerations that matter to patients. tify additional, valid authorization mechanisms,
Consider now the previously mentioned ran- rather than using a one-size-fits-all approach to
domized clinical trial comparing two similar informed consent. The transformation to ethical
hypertension drugs to see what authorization ly robust learning health care systems is critical
approaches might be justified in the current en- to this goal.
vironment. We suggested that in an ethically ro- Disclosure forms provided by the authors are available with the
bust learning health care system, characterized full text of this article at NEJM.org.
by extensive patient engagement, transparency, From the Berman Institute of Bioethics, Johns Hopkins Univer-
and accountability, it would be ethically accept- sity, Baltimore (R.R.F., N.E.K.); and the Kennedy Institute of
able for the study to proceed with a streamlined Ethics, Georgetown University, Washington, DC (T.L.B.).
consent process and potentially even without 1. Kass NE, Faden RR, Goodman SN, Pronovost P, Tunis S,
specific notification to affected patients. In the Beauchamp TL. The research-treatment distinction: a problem-
present context, in which morally relevant fea- atic approach for determining which activities should have ethi-
cal oversight. Hastings Cent Rep 2013;43:S4-S15.
tures of a mature learning health care system 2. Faden RR, Kass NE, Goodman SN, Pronovost P, Tunis S,
are not in place, proceeding without specific no- Beauchamp TL. An ethics framework for a learning healthcare
tification to patients would not be ethically ac- system: a departure from traditional research ethics and clinical
ethics. Hastings Cent Rep 2013;Spec No:S16-S27.
ceptable. However, it may still be ethically justi- 3. Faden R, Kass N, Whicher D, Stewart W, Tunis S. Ethics and
fiable to use a streamlined consent process, informed consent for comparative effectiveness research with
similar to that suggested by others,4,5 because prospective electronic clinical data. Med Care 2013;51:Suppl 3:
S53-S57.
the study has no apparent effects on the risks or 4. Truog RD, Robinson W, Randolph A, Morris A. Is informed
burdens that patients otherwise face in clinical consent always necessary for randomized, controlled trials?
care (the third and fourth obligations), clinician N Engl J Med 1999;340:804-7.
5. Morris MC, Nelson RM. Randomized, controlled trials as
judgment is respected (the second obligation), minimal risk: an ethical analysis. Crit Care Med 2007;35:940-4.
and the interventions do not differ on matters of DOI: 10.1056/NEJMhle1313674
importance to patients (the first obligation). In Copyright © 2014 Massachusetts Medical Society.
768 n engl j med 370;8 nejm.org february 20, 2014
The New England Journal of Medicine
Downloaded from nejm.org by Robert Califf on February 19, 2014. For personal use only. No other uses without permission.
Copyright © 2014 Massachusetts Medical Society. All rights reserved.
You might also like
- Medical ErrorDocument11 pagesMedical ErrorLakshya BansalNo ratings yet
- Redesigning Primary Care Practice To Incorporate Health Behavior ChangeDocument3 pagesRedesigning Primary Care Practice To Incorporate Health Behavior ChangeDebbie CharlotteNo ratings yet
- Health Education: Evidenced Based PracticesDocument58 pagesHealth Education: Evidenced Based PracticesChantal Raymonds90% (41)
- Clinical Research and Medical CareDocument7 pagesClinical Research and Medical CareNino MdinaradzeNo ratings yet
- Ethical Coded and Regulations For NursesDocument5 pagesEthical Coded and Regulations For NursesKhylamarie VillalunaNo ratings yet
- HealthCare Ethics - Edited.edited - EditedDocument5 pagesHealthCare Ethics - Edited.edited - EditedJuliana ChesireNo ratings yet
- Patient Safety USMLEDocument18 pagesPatient Safety USMLEsdroyafmc100% (2)
- How Bureaucracy Can Foster Burnout: Standardization FirstDocument7 pagesHow Bureaucracy Can Foster Burnout: Standardization FirstRakesh ChoudhuryNo ratings yet
- Bab 6Document16 pagesBab 6rinanurbaniNo ratings yet
- Ethics Final Notes NewDocument6 pagesEthics Final Notes NewFaisal HameedNo ratings yet
- Self-assessment Questions for Clinical Molecular GeneticsFrom EverandSelf-assessment Questions for Clinical Molecular GeneticsRating: 5 out of 5 stars5/5 (1)
- Setting A Research Agenda For Medical Over UseDocument7 pagesSetting A Research Agenda For Medical Over UsemmNo ratings yet
- Chaps 9 and 2Document65 pagesChaps 9 and 2Lady DanielleNo ratings yet
- Hoffman 2011Document12 pagesHoffman 2011Dima KassoufNo ratings yet
- The Role of Ethical Principles in Health Care and The Implications For Ethical CodesDocument6 pagesThe Role of Ethical Principles in Health Care and The Implications For Ethical CodesNewfaceNo ratings yet
- Ethics in OBGDocument36 pagesEthics in OBGManinder SekhonNo ratings yet
- Morris 1992Document13 pagesMorris 1992Lorena PăduraruNo ratings yet
- Ethical Issues in PhlebotomyDocument6 pagesEthical Issues in Phlebotomylisalov100% (1)
- A Randomized Controlled Trial of A Computer-Based Physician Workstation in An Outpatient Setting: Implementation Barriers To Outcome EvaluationDocument9 pagesA Randomized Controlled Trial of A Computer-Based Physician Workstation in An Outpatient Setting: Implementation Barriers To Outcome EvaluationDith Rivelta CallahanthNo ratings yet
- Leonardi A. GoenawanDocument33 pagesLeonardi A. GoenawanJaneNo ratings yet
- Bioethics - 2023 - Heynemann - Therapeutic Misunderstandings in Modern ResearchDocument15 pagesBioethics - 2023 - Heynemann - Therapeutic Misunderstandings in Modern ResearchPaulo Afonso do PradoNo ratings yet
- CH 08Document8 pagesCH 08john mwangiNo ratings yet
- The Patient Perspective On Clinical TrialsDocument15 pagesThe Patient Perspective On Clinical TrialsAlessandra BendoNo ratings yet
- CAMDocument6 pagesCAMDrogNo ratings yet
- Ethical Issues in Clinical Trials in Developing CountriesDocument20 pagesEthical Issues in Clinical Trials in Developing Countrieszehan iraniNo ratings yet
- Ethics in Midwifery PracticeDocument42 pagesEthics in Midwifery PracticeDivya Grace95% (19)
- Need For PolicyDocument13 pagesNeed For PolicyRahman OlaitanNo ratings yet
- What Is Evidence PracticeDocument80 pagesWhat Is Evidence PracticeIndrajith LiyanageNo ratings yet
- Pros and Cons of Experimental Drugs (Medical Treatment)Document3 pagesPros and Cons of Experimental Drugs (Medical Treatment)kingfish1021No ratings yet
- Perspective: Comparative Effectiveness: Asking The Right Questions, Choosing The Right MethodDocument5 pagesPerspective: Comparative Effectiveness: Asking The Right Questions, Choosing The Right MethodamkroegeNo ratings yet
- Primary Health Care and Family MedicineDocument5 pagesPrimary Health Care and Family MedicineCATHERINE HAYNESNo ratings yet
- Rational Decision Making in MedicineDocument11 pagesRational Decision Making in MedicineSanti AraratNo ratings yet
- Making Informed Decisions: Assessing Strengths and Weaknesses of Study Designs and Analytic Methods For Comparative Effectiveness ResearchDocument36 pagesMaking Informed Decisions: Assessing Strengths and Weaknesses of Study Designs and Analytic Methods For Comparative Effectiveness ResearchNational Pharmaceutical CouncilNo ratings yet
- Nursing Code of Ethics: Statements Last Modified in 2015, It Contains Nine Provisions, Which DetailDocument3 pagesNursing Code of Ethics: Statements Last Modified in 2015, It Contains Nine Provisions, Which Detailrosita d. ramosNo ratings yet
- Evidence Based Practice Lec 9Document38 pagesEvidence Based Practice Lec 9Nk Prince100% (1)
- Integrating CAM Practices Into The Conventional Health Systems (Integrative Medicine)Document12 pagesIntegrating CAM Practices Into The Conventional Health Systems (Integrative Medicine)Joud D.No ratings yet
- Clinical Decision Support Systems (CDSSS) Name Year AffiliationDocument16 pagesClinical Decision Support Systems (CDSSS) Name Year AffiliationPATRICK OTIATONo ratings yet
- Executive SummaryDocument9 pagesExecutive SummaryconnieNo ratings yet
- AHA Hypertension JournalDocument10 pagesAHA Hypertension JournalTiwi QiraNo ratings yet
- Medical Ethics: A Physician's Guide to Clinical MedicineFrom EverandMedical Ethics: A Physician's Guide to Clinical MedicineNo ratings yet
- Etica Epidemiologicos enDocument14 pagesEtica Epidemiologicos enAlina PopaNo ratings yet
- Using Pragmatic Clinical Trials To Test The Effectiveness of Patient-Centered Medical Home Models in Real-World Settings PCMH Research Methods SeriesDocument11 pagesUsing Pragmatic Clinical Trials To Test The Effectiveness of Patient-Centered Medical Home Models in Real-World Settings PCMH Research Methods SeriesJames LindonNo ratings yet
- The Underlying Principles of Ethical Patient CareDocument7 pagesThe Underlying Principles of Ethical Patient CareGulshanNo ratings yet
- Evidencebased Healthcare and Quality ImprovementDocument8 pagesEvidencebased Healthcare and Quality ImprovementJemimah BureresNo ratings yet
- Evidence Based Medicine: What It Is and What It Isn'tDocument3 pagesEvidence Based Medicine: What It Is and What It Isn'tCristian EstradaNo ratings yet
- EBMDocument636 pagesEBMDaniel SalaNo ratings yet
- What It Is and What It Is NotDocument4 pagesWhat It Is and What It Is NotshrikantNo ratings yet
- Edited Belmont Principles ReflectionDocument6 pagesEdited Belmont Principles ReflectionDanyNo ratings yet
- Ethics and Medico Legal AspectsDocument5 pagesEthics and Medico Legal AspectsmkumNo ratings yet
- Adherence To Informed Consent Standards in Shiraz Hospitals: Matrons' PerspectiveDocument6 pagesAdherence To Informed Consent Standards in Shiraz Hospitals: Matrons' PerspectiveLaxmi Kant SahaniNo ratings yet
- 2004 Beyond RCT - AjphDocument6 pages2004 Beyond RCT - AjphSamuel Andrés AriasNo ratings yet
- Domain Study Healthcare AnalyticsDocument3 pagesDomain Study Healthcare AnalyticsAzeem KhaliphaNo ratings yet
- Wiley Milbank Memorial FundDocument42 pagesWiley Milbank Memorial FundLuciana NovaesNo ratings yet
- Evidence-Based Practice in Pediatric Physical Therapy by BarryDocument14 pagesEvidence-Based Practice in Pediatric Physical Therapy by BarryFe TusNo ratings yet
- The Slim Book of Health Pearls: The Complete Medical ExaminationFrom EverandThe Slim Book of Health Pearls: The Complete Medical ExaminationNo ratings yet
- Medical Professionalism in The New Millennium: A Physician CharterDocument2 pagesMedical Professionalism in The New Millennium: A Physician CharterNewfaceNo ratings yet
- Dr. Mohamed Mosaad Hasan MD, MPH, CPHQ, CPPS, GbssDocument48 pagesDr. Mohamed Mosaad Hasan MD, MPH, CPHQ, CPPS, GbssKristine Marie PateñoNo ratings yet
- Theroleofpatients: Shared Decision-MakingDocument20 pagesTheroleofpatients: Shared Decision-MakingMaryela MenachoNo ratings yet
- The Fine Line of Defensive Medicine PDFDocument3 pagesThe Fine Line of Defensive Medicine PDFEMMA LAURA MORALES GONZALEZNo ratings yet
- Best Evidence-Based Practices To Treat Intravenous InfiltrationDocument1 pageBest Evidence-Based Practices To Treat Intravenous InfiltrationSasha Hidayat FullNo ratings yet
- Infiltration and Extravasation Update On.10Document9 pagesInfiltration and Extravasation Update On.10Beauty CassieNo ratings yet
- Ekstravasasi PDFDocument7 pagesEkstravasasi PDFSasha Hidayat FullNo ratings yet
- Revista Paulista DE PediatriaDocument6 pagesRevista Paulista DE PediatriaSasha Hidayat FullNo ratings yet
- _____ ______ __ _ ____Document6 pages_____ ______ __ _ ____Sasha Hidayat FullNo ratings yet
- Genetic Journal PDFDocument12 pagesGenetic Journal PDFSasha Hidayat FullNo ratings yet
- Askep Meningitis AnakDocument10 pagesAskep Meningitis AnakSasha Hidayat FullNo ratings yet
- Evid Based Nurs 2012 Meek 84 5Document3 pagesEvid Based Nurs 2012 Meek 84 5Sasha Hidayat FullNo ratings yet
- Hipospadia Ej1083631 OkDocument17 pagesHipospadia Ej1083631 OkSasha Hidayat FullNo ratings yet
- Four Perspectives On Child Care Quality: Deborah Ceglowski and Chiara BacigalupaDocument7 pagesFour Perspectives On Child Care Quality: Deborah Ceglowski and Chiara BacigalupaSasha Hidayat FullNo ratings yet
- P H & S J: The Ace Scoring SystemDocument6 pagesP H & S J: The Ace Scoring SystemSasha Hidayat FullNo ratings yet
- Genetic Journal PDFDocument12 pagesGenetic Journal PDFSasha Hidayat FullNo ratings yet
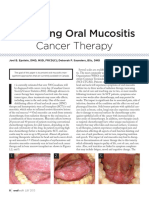
- Managing Oral Mucositis Oral Health July 2015Document4 pagesManaging Oral Mucositis Oral Health July 2015fiora.ladesvitaNo ratings yet
- MucositisDocument6 pagesMucositisHarry ArdiyantoNo ratings yet
- B - PDF PDFDocument11 pagesB - PDF PDFSasha Hidayat FullNo ratings yet
- Harrison Prevention and Management of Pain and Stress in The Neonate 2015Document8 pagesHarrison Prevention and Management of Pain and Stress in The Neonate 2015Sasha Hidayat FullNo ratings yet
- Ok JurnalDocument6 pagesOk JurnalSasha Hidayat FullNo ratings yet
- Position 2Document8 pagesPosition 2Sasha Hidayat FullNo ratings yet
- 212Document5 pages212Sasha Hidayat FullNo ratings yet
- Acute Respiratory Distress Syndrome in Pediatric Intensive Care UnitDocument4 pagesAcute Respiratory Distress Syndrome in Pediatric Intensive Care UnitSasha Hidayat FullNo ratings yet
- Position 3Document5 pagesPosition 3Sasha Hidayat FullNo ratings yet
- Overweight and Obesity Among White, Black, and Mexican American Children: Implications For When To InterveneDocument10 pagesOverweight and Obesity Among White, Black, and Mexican American Children: Implications For When To InterveneSasha Hidayat FullNo ratings yet
- JCCNC v1n4p205 enDocument6 pagesJCCNC v1n4p205 enSasha Hidayat FullNo ratings yet
- Massase For Cancer 2Document16 pagesMassase For Cancer 2Sasha Hidayat FullNo ratings yet
- Oral Care For Cancer PDFDocument10 pagesOral Care For Cancer PDFSasha Hidayat FullNo ratings yet
- Gynecologic Oncology: Nozomi Donoyama, Toyomi Satoh, Tetsutaro Hamano, Norio Ohkoshi, Mamiko OnukiDocument8 pagesGynecologic Oncology: Nozomi Donoyama, Toyomi Satoh, Tetsutaro Hamano, Norio Ohkoshi, Mamiko OnukiSasha Hidayat FullNo ratings yet
- Ethical SkillDocument8 pagesEthical SkillSasha Hidayat FullNo ratings yet
- 4as To Rise Above Moral Distress PDFDocument14 pages4as To Rise Above Moral Distress PDFOscar PerezNo ratings yet
- Gynecologic Oncology: Nozomi Donoyama, Toyomi Satoh, Tetsutaro Hamano, Norio Ohkoshi, Mamiko OnukiDocument8 pagesGynecologic Oncology: Nozomi Donoyama, Toyomi Satoh, Tetsutaro Hamano, Norio Ohkoshi, Mamiko OnukiSasha Hidayat FullNo ratings yet
- FreeMarkets: Procurement & Outsourcing StrategiesDocument44 pagesFreeMarkets: Procurement & Outsourcing StrategiesFarhaad MohsinNo ratings yet
- The Machine StopsDocument14 pagesThe Machine StopsMICHAEL HARRIS USITANo ratings yet
- Measures-English, Metric, and Equivalents PDFDocument1 pageMeasures-English, Metric, and Equivalents PDFluz adolfoNo ratings yet
- English Lesson PlanDocument3 pagesEnglish Lesson PlanJeremias MartirezNo ratings yet
- MISKDocument134 pagesMISKmusyokaNo ratings yet
- Unsaturated Polyester Resins: Influence of The Styrene Concentration On The Miscibility and Mechanical PropertiesDocument5 pagesUnsaturated Polyester Resins: Influence of The Styrene Concentration On The Miscibility and Mechanical PropertiesMamoon ShahidNo ratings yet
- Organigation DeveDocument3 pagesOrganigation Devemerin sunilNo ratings yet
- What Are RussiaDocument3 pagesWhat Are RussiaMuhammad SufyanNo ratings yet
- Role of Courts in Granting Bails and Bail Reforms: TH THDocument1 pageRole of Courts in Granting Bails and Bail Reforms: TH THSamarth VikramNo ratings yet
- Quarter 2-Module 7 Social and Political Stratification: Department of Education Republic of The PhilippinesDocument21 pagesQuarter 2-Module 7 Social and Political Stratification: Department of Education Republic of The Philippinestricia100% (5)
- Implementation of 7s Framenwork On RestuDocument36 pagesImplementation of 7s Framenwork On RestuMuhammad AtaNo ratings yet
- Life in The Past - Year 6 WorksheetsDocument11 pagesLife in The Past - Year 6 WorksheetstinaNo ratings yet
- CURRICULUM VITAE Kham Khan Suan Hausing, PHDDocument8 pagesCURRICULUM VITAE Kham Khan Suan Hausing, PHDCinpu ZomiNo ratings yet
- The Bible Does Not Condemn Premarital SexDocument16 pagesThe Bible Does Not Condemn Premarital SexKeith502100% (3)
- Impact of Micro FinanceDocument61 pagesImpact of Micro FinancePerry Arcilla SerapioNo ratings yet
- Navamsa Karma and GodDocument9 pagesNavamsa Karma and GodVisti Larsen50% (2)
- Epic Story of IbalonDocument30 pagesEpic Story of IbalonKi Ko100% (3)
- Tamil Ilakkanam Books For TNPSCDocument113 pagesTamil Ilakkanam Books For TNPSCkk_kamalakkannan100% (1)
- Friedman LawsuitDocument12 pagesFriedman LawsuitChris GothnerNo ratings yet
- Sri Guru Parampara Stotram CompressDocument14 pagesSri Guru Parampara Stotram CompressSatishPavurayalaNo ratings yet
- 9.2 Volumetric Analysis PDFDocument24 pages9.2 Volumetric Analysis PDFJoaquinNo ratings yet
- Grade 5 Forces Acting On Structures and Mechanisms CirriculumDocument3 pagesGrade 5 Forces Acting On Structures and Mechanisms Cirriculumapi-2072021750% (1)
- Number SystemsDocument165 pagesNumber SystemsapamanNo ratings yet
- Bug Tracking System AbstractDocument3 pagesBug Tracking System AbstractTelika Ramu86% (7)
- Lesson I. Background InformationDocument21 pagesLesson I. Background InformationsuidivoNo ratings yet
- SAP CRM Tax ConfigurationDocument18 pagesSAP CRM Tax Configurationtushar_kansaraNo ratings yet
- Paradigm Shift in Teaching: The Plight of Teachers, Coping Mechanisms and Productivity in The New Normal As Basis For Psychosocial SupportDocument5 pagesParadigm Shift in Teaching: The Plight of Teachers, Coping Mechanisms and Productivity in The New Normal As Basis For Psychosocial SupportPsychology and Education: A Multidisciplinary JournalNo ratings yet
- Corporation Law Case Digests Philippines Merger and ConsolidationDocument7 pagesCorporation Law Case Digests Philippines Merger and ConsolidationAlpha BetaNo ratings yet
- Oracle QuestDocument521 pagesOracle Questprasanna ghareNo ratings yet
- Module6 (Margie Ybanez)Document3 pagesModule6 (Margie Ybanez)Margie Ybañez82% (17)