Professional Documents
Culture Documents
Ent Solved Kmu Seqs by RMC Students
Uploaded by
Aamir KhanOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ent Solved Kmu Seqs by RMC Students
Uploaded by
Aamir KhanCopyright:
Available Formats
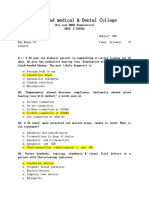
Otorhinolaryngology
KMU PAST PAPERS SOLVED SEQS
SALMAN KHAN | REHMAN MEDICAL COLLEGE
No part of this publication is to be reproduced
for purposes of sale, you may transmit by any
form or by any means, electronic, mechanical,
photocopying, recording or otherwise, without
the prior permission of the author, this eBook is
specifically for educational purposes only
Contents 1
EAR 2
NOSE AND PARANASAL SINUSES 32
ORAL CAVITY PHARYNX LARYNX AND ESOPHAGUS 44
References
1. Diseases of Ear, Nose and Throat (5th Edition) P L Dhingra
KMU Past Papers Solved SEQs
Ear 2
ANS:
Q-1. A lady age 45 years, presented with vertigo and vomiting for the last two days. On
questioning she disclosed that she also has deafness and tinnitus in her right ear which
started before vertigo. She had similar attacks in the past.
a) What is the most likely diagnosis?
b) Name three investigations with justifications.
c) What is medical treatment?
a) DIAGNOSIS:
Meniere’s disease
b) INVESTIGATIONS WITH JUSTIFICATION
1. Pure tone audiometry:
There is sensorineural hearing loss. In early stages, lower frequencies are affected
and the curve is of rising type. When higher frequencies are involved curve
becomes flat or a falling type.
2. Speech audiometry Discrimination score:
55-85% between the attacks but discrimination ability is much impaired during
and immediately following an attack.
3. Special audiometry tests: to differentiate this from retro-cochlear lesions (RCL)
(acoustic neuroma)
a. Recruitment test is positive. (abnormal growth of loudness in affected year)
b. SISI (short increment sensitivity index) test: score is more than 70% (15%
normal)
c. Tone decay test. decay of less than 20 dB (>25dB in RCL)
4. Electrocochleography: (diagnostic of Meniere's disease)
summating potential (SP) to action potential (AP) ratio is greater than 30 (Normal
SP/AP ratio is 30%)
5. Caloric test:
It shows reduced response on the affected side.
6. Glycerol test: Audiogram and speech discrimination scores are recorded before
and 1—2 hours after ingestion of glycerol. An improvement of 10 dB or gain of
10% in discrimination score makes the test positive
7. Glycerol test is combined with electrocochleography.
c) TREATMENT:
A. General Measures
1. Reassurance: relieve the Patient's anxiety can be by reassurance and by
explaining the true nature of disease.
2. Cessation of smoking: Nicotine causes vasospasm.
3. Low salt diet: Patient should take salt-free diet as far as possible.
4. Avoid excessive intake of water
5. Avoid over-indulgence in coffee, tea and alcohol
6. Avoid stress and bring a change in life-style
KMU Past Papers Solved SEQs
Ear 3
7. Avoid activities requiring good body balance, such as flying, under-water diving or
working at great heights should be avoided.
B. Management of Acute Attack
1. Reassurance and psychological support to allay worry and anxiety.
2. Bed rest with head supported on pillows to prevent excessive movements.
3. Vestibular sedatives to relieve vertigo.
dimenhydrinate (Dramamine), prochlorperazine (Stemetil) IM or IV.
Diazepam (Valium or Calmpose IV,
atropine, 0.4 mg, given subcutaneously for acute attack.
4. Vasodilators
Inhalation of carbogen (5% CO with 95% O). It is a good cerebral vasodilator and
improves labyrinthine circulation.
Histamine diphosphate infusion, helps to control acute attacks. (contraindicated
in asthmatics)
C. Management of Chronic Phase
1. Vestibular sedatives: Prochlorperazine (Stemetil) 10mg orally
2. Vasodilators
Nicotinic acid, 50 mg, before meals thrice a day.
Betahistine (Vertin) 8-16 mg, thrice a day, given orally
3. Diuretics: Furosemide, 40 mg tablet, taken on alternate days with potassium
supplement.
4. Propantheline bromide (Probanthine), 15mg, thrice a day,
5. Elimination of allergen through elimination or desensitization.
6. Hormones Replacement therapy in case of hypothyroidism
7. Intra-tympanic gentamicin therapy: (chemical labyrinthectomy). biweekly
injections gentamicin into the middle ear.
8. Microwick is pass though grommet in tympanic membrane to deliver drug,
gentamicin or steroids, to oval windows, it avoids repeated intra-tympanic
injections.
Q-2. 5 years old child presented with right side earache, fever and deafness for the last
seven days. Now he developed swelling behind right post auricular region and his
temperature also increased.
a) What is the most likely diagnosis?
b) What investigation would you order?
c) What are two other differential diagnoses in this case?
d) What is the treatment of this case?
ANS:
a) DIAGNOSIS:
Acute mastoiditis
b) INVESTIGATIONS:
KMU Past Papers Solved SEQs
Ear 4
1. Blood counts show polymorphonuclear leucocytosis.
2. ESR is usually raised.
3. X-ray mastoid There is clouding of air cells due to collection of exudate in them.
Bony partitions between air cells become indistinct, but the sinus plate is seen as a
distinct outline. In later stages, a cavity may be seen in the mastoid.
4. Ear swab for culture and sensitivity.
c) DIFFERENTIAL DIAGNOSIS:
1. Suppuration of mastoid lymph nodes in Scalp infection
2. Furunculosis of meatus.
3. Infected sebaceous cyst
d) TREATMENT:
1. Hospitalisation of the patient.
2. Antibiotics: start with amoxicillin or ampicillin. Specific antimicrobial is started on
the receipt of sensitivity report. chloramphenicol or metronidazole is used for
anaerobic organisms.
3. Myringotomy When pus is under tension it is relieved by wide myringotomy
4. Cortical mastoidectomy It is indicated when there is:
i) Subperiosteal abscess.
ii) Sagging of posterosuperior meatal wall.
iii) Positive reservoir sign,
iv) No change in condition of patient or it worsens in spite of adequate
medical treatment for 48 hours.
v) Mastoiditis, leading to complications, e.g. facial paralysis, labyrinthitis,
intracranial complications, etc.
Q-3. A forty-five years old lady presented with slowly progressive bilateral conductive
deafness and tinnitus. Her brother and elder sister also have same problem. On
examination both tympanic membranes are intact and normal in color and in position.
Rinne are negative in both ears and Weber is liberalized towards the right ear.
a) What is the most likely diagnosis?
b) What investigations are needed to reach the diagnosis?
c) Name different treatment options for this patient.
ANS:
a) DIAGNOSIS:
Otosclerosis
b) INVESTIGATIONS
1. Tuning fork test; show negative Rinne (i.e. BC > AC)
2. Weber test; lateralised to the ear with greater conductive loss.
3. Absolute bone conduction may be normal.
4. Pure tone audiometry; shows loss of air conduction, Normal bone conduction and
Carhart's notch at 2000 Hz
5. Speech audiometry reveals normal discrimination score
KMU Past Papers Solved SEQs
Ear 5
6. Tympanometry; type As (shows a curve of ossicular stiffness)
7. Stapedial reflex is absent if stapes is fixed
c) TREATMENT:
1. Medical:
There is no medical treatment that cures otosclerosis. Sodium fluoride has been tried
but this treatment is not recommended generally.
2. Surgical:
Stapedectomy with a placement of prosthesis is the treatment of choice. Here the
fixed otosclerotic stapes is removed and a prosthesis inserted between the incus and
oval window Prosthesis employed may be a teflon piston, stainless steel piston,
platinum teflon or titanium teflon piston
Q-4. A patient fond of swimming presents to the ENT OPD with complaint of pain in the
right ear. This pain is aggravated if the pinna is even touched with the pillow at night. This
pain was by the itching of the same ear, which tempted the to scratch it with a match stick.
patient also complains of hearing loss in this ear. While performing the tuning fork tests,
Weber test is liberalized to the right ear.
a) What is your diagnosis?
b) Which two pints will be tender on palpation?
c) Give various classification of this condition.
d) What advice would like to give to this patient for future prevention of this
condition?
e) How will you treat this condition?
ANS:
a) Diagnosis:
Diffuse otitis externa
b) points tender on palpation:
tragus, pinna, regional lymph node
c) Classification:
(i) Infective group
Bacterial (Localized otitis externa (Furuncle) Diffuse otitis externa, Malignant otitis
externa)
Fungal (otomycosis)
Viral (Herpes zoster oticus, otitis externa hemorrhagica)
(ii) Reactive group (Eczematous otitis externa Seborrhoeic otitis externa
Neurodermatitis)
d) Advise:
Do not scratch the ear canal with hair pins or match sticks, immediately after bath or
swimming.
e) Treatment:
1. Ear toilet:
KMU Past Papers Solved SEQs
Ear 6
Ear toilet can be done by dry mopping, suction clearance or irrigating the canal
with warm, sterile normal saline.
2. Medicated wicks:
a gauze wick soaked in antibiotic steroid preparation is inserted in the ear canal.
Local steroid drops help to relieve oedema and erythema, and prevent itching.
Aluminium acetate (8%) or silver nitrate (3%) used in the form of a wick used to
form a protective coagulum to dry-up an oozing meatus.
3. Antibiotics:
Broad spectrum systemic antibiotics are used when there is cellulitis and acute
tender lymphadenitis.
4. Analgesics: For relief of pain.
Q-5. A 25 years old female presented with hearing loss and tinnitus. She was diagnosed as a
case of otosclerosis.
a) Define otosclerosis?
b) What will be the findings on tuning fork test, tympanometry and audiogram in a
typical case of otosclerosis?
c) What is paracusis willisii?
d) What treatment options are available for this
ANS:
a) OTOSCLEROSIS:
Otosclerosis (Otospongiosis) is a primary disease of the bony labyrinth in which one or
more foci of irregularly laid spongy bone replace part of normally dense enchondral layer
of bony otic capsule, stapes region leading to stapes fixation and conductive deafness.
However, it may involve certain other areas of the bony labyrinth where it may cause
neurosensory loss,
b) INVESTIGATIONS
1. Tuning fork test; show negative Rinne (i.e. BC > AC)
2. Weber test; lateralised to the ear with greater conductive loss.
3. Absolute bone conduction may be normal.
4. Pure tone audiometry; shows loss of air conduction, Normal bone conduction and
Carhart's notch at 2000 Hz
5. Speech audiometry reveals normal discrimination score
6. Tympanometry; Type As (shows a curve of ossicular stiffness)
7. Stapedial reflex is absent if stapes is fixed
c) PARACUSIS WILLISII:
An otosclerotic patient hears better in noisy than quiet surroundings. This is because a
normal person will raise his voice in noisy surroundings
d) TREATMENT:
1. Medical:
KMU Past Papers Solved SEQs
Ear 7
There is no medical treatment that cures otosclerosis. Sodium fluoride has been tried
but this treatment is not recommended generally.
2. Surgical:
Stapedectomy with a placement of prosthesis is the treatment of choice. Here the
fixed otosclerotic stapes is removed and a prosthesis inserted between the incus and
oval window Prosthesis employed may be a teflon piston, stainless steel piston,
platinum teflon or titanium teflon piston
Q-6. A 40 years old male patient came to the ENT Clinic with history or paroxysmal attacks
of severe vertigo associated with deafness and tinnitus in the left ear for the last six
months. The attack usually does not last more than 24 hours. On examination both the
tympanic membranes are normal, Rinne's test is positive on both sides and weber is
lateralized towards the right.
a) What is your most likely diagnosis?
b) How will you confirm the diagnosis?
c) How will you treat the patient in acute attack?
d) What are the various surgical options for this condition?
ANS:
a) DIAGNOSIS:
Meniere’s disease
b) INVESTIGATIONS WITH JUSTIFICATION
1. Pure tone audiometry:
There is sensorineural hearing loss. In early stages, lower frequencies are affected
and the curve is of rising type. When higher frequencies are involved curve
becomes flat or a falling type.
2. Speech audiometry Discrimination score:
55-85% between the attacks but discrimination ability is much impaired during
and immediately following an attack.
3. Special audiometry tests: to differentiate this from retro-cochlear lesions (RCL)
(acoustic neuroma)
d. Recruitment test is positive (abnormal growth of loudness in affected year)
e. SISI (short increment sensitivity index) test: score is more than 70% (15%
normal)
f. Tone decay test. decay of less than 20 dB (>25dB in RCL)
4. Electrocochleography: (diagnostic of Meniere's disease)
summating potential (SP) to action potential (AP) ratio is greater than 30 (Normal
SP/AP ratio is 30%)
5. Caloric test:
It shows reduced response on the affected side.
KMU Past Papers Solved SEQs
Ear 8
6. Glycerol test: Audiogram and speech discrimination scores are recorded before
and 1—2 hours after ingestion of glycerol. An improvement of 10 dB or gain of
10% in discrimination score makes the test positive
7. Glycerol test is combined with electrocochleography.
c) MANAGEMENT OF ACUTE ATTACK:
A. Management of Acute Attack
1. Reassurance and psychological support to allay worry and anxiety.
2. Bed rest with head supported on pillows to prevent excessive movements.
3. Vestibular sedatives to relieve vertigo.
dimenhydrinate (Dramamine), prochlorperazine (Stemetil) IM or IV.
Diazepam (Valium or Calmpose IV,
atropine, 0.4 mg, given subcutaneously for acute attack.
4. Vasodilators
Inhalation of carbogen (5% CO with 95% O). It is a good cerebral vasodilator and
improves labyrinthine circulation.
Histamine diphosphate infusion, helps to control acute attacks. (contraindicated
in asthmatics)
d) SURGICAL TREATMENT:
1. Conservative procedures: They are used in cases where hearing is still useful and
needs to be preserved.
i. Decompression of endolymphatic sac.
ii. Endolymphatic shunt operation. A tube is put, connecting endolymphatic
sac with subarachnoid space, to drain excess endolymph.
iii. Sacculotomy
Fick's operation It is puncturing the saccule with a needle through
stapes footplate.
Cody's tack procedure consists of placing a stainless steel tack
through the stapes footplate. The tack would cause periodic
decompression of the saccule when it gets distended.
Cochleosacculotomy: instead of saccule, cochlear duct is punctured
and drained into the perilymph.
iv. Section of vestibular nerve. The nerve is exposed by retro-sigmoid or
middle cranial fossa approach and selectively sectioned.
v. Ultrasonic destruction of vestibular labyrinth.
2. Destructive procedures They totally destroy cochlear and vestibular function
i. Labyrinthectomy. Membranous labyrinth is completely destroyed either by
opening through the lateral semicircular canal by transmastoid route or
through the oval window by a transcanal approach.
3. Intermittent low pressure pulse therapy (Meniett device therapy):
Intermittent positive pressure waves can be delivered through this device
i. myringotomy is performed and ventilation tube is inserted.
KMU Past Papers Solved SEQs
Ear 9
ii. the device then delivers pressure waves to the round window membrane
via the ventilation tube.
iii. Pressure waves pass through the perilymph and cause reduction in
endolymph pressure by redistributing it through various communication
channels such as the endolymphatic sac or the blood vessels
iv. Pressure also regulate secretion of endolymph by the stria vascularis
Q-7. A 15 years old boy complaining of left ear discharge or the last three years. The
discharge is foul smelling and scanty. He also gives history of left sided decreased hearing.
For the last one day he is unable to close his left eye with deviation of one angle of the
mouth to the right. The otoscopic examination shows a posterior marginal perforation
with cholestetoma.
a) What is your diagnosis?
b) How Will you investigate this patient?
c) How will you treat this patient?
ANS:
a) Diagnosis:
Chronic suppurative otitis media (CSOM) Atticoantral or unsafe type
b) investigations:
1. Examination under microscope It may reveal presence of cholesteatoma, its site
and extent, evidence of bone destruction, granuloma, condition of ossicles and pockets
of discharge.
2. Tuning fork tests and audiogram They are essential for pre-operative assessment
and to confirm the degree and type of hearing loss.
3. X-ray mastoids/CT scan temporal bone They indicate extent of bone destruction
and degree of mastoid pneumatisation. They are useful to indicate a low-lying dura or
an anteposed sigmoid sinus when operation is being contemplated on a sclerotic
mastoid. Cholesteatoma causes destruction in the area of attic and antrum (key area),
better seen in lateral view. CT scan of temporal bone gives more information and is
preferred to X-ray mastoids.
4. Culture and sensitivity of ear discharge It helps to select proper antibiotic for local
or systemic use.
c) Treatment:
1. Surgical: Two types of surgical procedures are done to deal with cholesteatoma:
(a) Canal wall down procedures. They leave the mastoid cavity open into the external
auditory canal. The commonly performed operations for atticoantral disease are
atticotomy, modified radical mastoidectomy and rarely, the radical mastoidectomy.
(b) Canal wall up procedures. Here disease is removed by combined approach
through the meatus and mastoid but retaining the posterior bony meatal wall intact,
thereby avoiding an open mastoid cavity. It gives dry ear and permits easy
reconstruction of hearing mechanism.
KMU Past Papers Solved SEQs
Ear 10
2. Reconstructive surgery Hearing can be restored by myringoplasty or
tympanoplasty. It can be done at the time of primary surgery or as a second stage
procedure.
3. Conservative treatment: when cholesteatoma is small and easily accessible to
suction clearance under operating microscope. It can also be tried out in elderly
patients above 65 and those who are unfit for general anaesthesia or those refusing
surgery.
Polyps and granulations can also be surgically removed by cup forceps or cauterised
by chemical agents like silver nitrate or trichloroacetic acid.
Other measures like aural toilet and dry ear precautions are also essential.
Q-8. A 10 years old boy presented to ENT OPD with a tender, fluctuant swelling behind the
ear and fever. He has a history of ear discharge for the last 6 years. Examination of the ear
shows granulations in the ear canal.
a) What is your diagnosis?
b) What are differential diagnosis?
c) How will you investigate?
d) How will you treat this patient?
ANS:
a) DIAGNOSIS:
Acute mastoiditis
b) DIFFERENTIAL DIAGNOSIS:
1. Suppuration of mastoid lymph nodes in Scalp infection
2. Furunculosis of meatus.
3. Infected sebaceous cyst
c) INVESTIGATIONS:
1. Blood counts show polymorphonuclear leucocytosis.
2. ESR is usually raised.
3. X-ray mastoid There is clouding of air cells due to collection of exudate in them.
Bony partitions between air cells become indistinct, but the sinus plate is seen as a
distinct outline. In later stages, a cavity may be seen in the mastoid.
4. Ear swab for culture and sensitivity.
d) TREATMENT:
1. Hospitalisation of the patient.
2. Antibiotics: start with amoxicillin or ampicillin. Specific antimicrobial is started on
the receipt of sensitivity report. chloramphenicol or metronidazole is used for
anaerobic organisms.
3. Myringotomy When pus is under tension it is relieved by wide myringotomy
4. Cortical mastoidectomy It is indicated when there is:
i) Subperiosteal abscess.
ii) Sagging of posterosuperior meatal wall.
KMU Past Papers Solved SEQs
Ear 11
iii) Positive reservoir sign,
iv) No change in condition of patient or it worsens in spite of adequate
medical treatment for 48 hours.
v) Mastoiditis, leading to complications, e.g. facial paralysis, labyrinthitis,
intracranial complications, etc.
Q-9. You are asked to see a man who, has trauma to his left ear which resulted in swelling
of pinna. The swelling was obliterated all the natural anatomical contours of the pinna.
The patient feels some pain and discomfort over the swelling. Tuning fork- test shows
normal hearing.
a) What is this condition called?
b) Which two layers of the pinna are separated by this
c) How will you treat the patient?
ANS:
a) DIAGNOSIS:
Hematoma of the auricle
b) BLOOD IS COLLECTED BETWEEN
1. Cartilage
2. perichondrium
c) TREATMENT:
1. aspiration of the haematoma under strict aseptic precautions
2. pressure dressing, carefully packing all concavities of the auricle to prevent
reaccumulation.
3. Aspiration may need to be repeated.
4. incision and drainage should be done when aspiration fails, and pressure applied by
dental rolls tied with through and through sutures.
5. All cases should receive prophylactic antibiotics.
Q-10. A 45-year-Old male complains of right earache for last 2 days after swimming. Pain is
more at night and increase on chewing. Examination showed swollen and edematous
external auditory canal with no clear view of the tympanic membrane. There was also thin
purulent discharge.
a) What is likely diagnosis?
b) Important relevant questions will while taking history of this patient?
c) How will you treat this patient?
ANS:
a) DIAGNOSIS:
Diffuse otitis externa
b) QUESTIONS ASKED IN HISTORY:
KMU Past Papers Solved SEQs
Ear 12
Important question asked while taking history:
1. history of scratching the ear canal with hair pins or match sticks.
2. vigorous cleaning of ear canal after a swim.
3. Any attempt made to remove foreign bodies by unskilled instrumentation.
4. Diabetes status.
5. Immunocompromised or not.
c) TREATMENT:
1. Ear toilet:
Ear toilet can be done by dry mopping, suction clearance or irrigating the canal
with warm, sterile normal saline.
2. Medicated wicks:
a gauze wick soaked in antibiotic steroid preparation is inserted in the ear canal.
Local steroid drops help to relieve oedema and erythema, and prevent itching.
Aluminium acetate (8%) or silver nitrate (3%) used in the form of a wick used to
form a protective coagulum to dry-up an oozing meatus.
3. Antibiotics:
Broad spectrum systemic antibiotics are used when there is cellulitis and acute
tender lymphadenitis.
4. Analgesics: For relief of pain.
Q-11. A 20 years old patient came to ENT OPD with history of left ear foul smelling discharge
for the last two years. Since last three days he is complaining of severe headache.
Examination shows alert patient with ottic cholesteatoma.
a) what is your diagnosis?
b) how will you investigate this patient?
c) how will you treat this patient?
ANS:
a) DIAGNOSIS:
Chronic suppurative otitis media (atticoantral) or unsafe type
b) INVESTIGATIONS:
1. Examination under microscope It may reveal presence of cholesteatoma, its site
and extent, evidence of bone destruction, granuloma, condition of ossicles and pockets
of discharge.
2. Tuning fork tests and audiogram They are essential for pre-operative assessment
and to confirm the degree and type of hearing loss.
3. X-ray mastoids/CT scan temporal bone They indicate extent of bone destruction
and degree of mastoid pneumatisation. They are useful to indicate a low-lying dura or
an anteposed sigmoid sinus when operation is being contemplated on a sclerotic
mastoid. Cholesteatoma causes destruction in the area of attic and antrum (key area),
better seen in lateral view. CT scan of temporal bone gives more information and is
preferred to X-ray mastoids.
KMU Past Papers Solved SEQs
Ear 13
4. Culture and sensitivity of ear discharge It helps to select proper antibiotic for
local or systemic use.
c) TREATMENT:
1. Surgical: Two types of surgical procedures are done to deal with cholesteatoma:
(a) Canal wall down procedures. They leave the mastoid cavity open into the external
auditory canal. The commonly performed operations are
atticotomy,
modified radical mastoidectomy
radical mastoidectomy. (rarely)
(b) Canal wall up procedures. Here disease is removed by combined approach
through the meatus and mastoid but retaining the posterior bony meatal wall intact,
thereby avoiding an open mastoid cavity. It gives dry ear and permits easy
reconstruction of hearing mechanism.
Disease is removed by these approaches
Permeatly
Cortical mastoidectomy and posterior tympanotomy
2. Reconstructive surgery Hearing can be restored by myringoplasty or
tympanoplasty. It can be done at the time of primary surgery or as a second stage
procedure.
3. Conservative treatment: when cholesteatoma is small and easily accessible to
suction clearance under operating microscope. It can also be tried out in elderly
patients above 65 and those who are unfit for general anaesthesia or those refusing
surgery.
Polyps and granulations can also be surgically removed by cup forceps or cauterised
by chemical agents like silver nitrate or trichloroacetic acid.
Other measures like aural toilet and dry ear precautions are also essential.
Q-12. A 7-year-Old girl brought by her parents with history of decreased hearing, snoring at
night earache from time to time. There was no history of ear discharge. On examination
the tympanic membranes ware intact and dull looking and shows reduced mobility on
pneumatic otoscopy. The rest of ENT examination was normal.
a) What is the most probable diagnosis?
b) Name two relevant investigations with justification?
c) How will you treat this patient?
d) Name any two complications of the surgical procedure required in this condition?
ANS:
a) DIAGNOSIS:
Serous otitis media due to adenoids hypertrophy
b) INVESTIGATIONS:
(i) Tuning fork tests show conductive hearing loss.
KMU Past Papers Solved SEQs
Ear 14
(ii) Audiometry. There is conductive hearing loss of20—40 dB. Sometimes, there is
associated sensorineural hearing loss due to fluid pressing on the round window
membrane. This disappears with evacuation of fluid.
(iii) Impedance audiometry. It is an objective test useful in infants and children. Presence
of fluid is indicated by reduced compliance and flat curve with a shift to negative side.
(iv) X-ray mastoids. There is clouding of air cells due to fluid.
c) TREATMENT:
A. Medical
1. Decongestants: Topical decongestants in the form of nasal drops, sprays or systemic
decongestants.
2. Anti-allergic measures: Anti histaminic or steroids are used, if possible, allergen
should be found and desensitization done.
3. Antibiotics: in cases of upper respiratory tract infections or unresolved acute
suppurative otitis media.
4. Middle ear aeration: through Valsalva maneuver, politzerisation or Eustachian tube
catheterization. Children can be given chewing gum to encourage repeated swallowing
which opens the tube.
B. Surgical
1. Myringotomy and aspiration of fluid.
2. Grommet insertion to provide continued aeration of middle ear.
3. Tympanotomy or cortical mastoidectomy.
4. Surgical treatment of causative factor Adenoidectomy, tonsillectomy and/or wash-
out of maxillary antra.
d) COMPLICATION OF MYRINGOTOMY:
1. Injury to incudostapedial joint or stapes.
2. Injury to jugular bulb with profuse bleeding, if jugular bulb is high and floor of the
middle ear dehiscent.
3. Middle ear infection.
Complications of adenoidectomy:
1. Haemorrhage,
2. Injury to eustachian tube opening.
3. Injury to pharyngeal musculature and vertebrae.
4. Griesel syndrome.
5. Velopharyngeal insufficiency.
KMU Past Papers Solved SEQs
Ear 15
6. Nasopharyngeal stenosis
Q-13. A 30 years Old female complained of bilateral hearing loss more on right side following
the delivery of her first child. Hearing loss was marked in quiet places but hearing
improved in a noisy environment. Both tympanic membranes severe mobile and showed a
normal appearance. Rinne’s test was negative on both sides.
a) What is the most likely diagnosis?
b) Enumerate any two differential diagnoses?
c) What relevant investigations will you carry out to reach the diagnosis?
d) What are the treatment options?
e) Name any two complications of the surgical procedure required in this condition.
ANS:
a) DIAGNOSIS:
Otosclerosis
b) DIFFERENTIAL DIAGNOSIS:
1. Serous otitis media,
2. Adhesive otitis media,
3. Tympanosclerosis,
4. Attic fixation of head of malleus,
5. Ossicular discontinuity
6. congenital stapes fixation.
c) INVESTIGATIONS
1. Tuning fork test; show negative Rinne (i.e. BC > AC)
2. Weber test; lateralised to the ear with greater conductive loss.
3. Absolute bone conduction may be normal.
4. Pure tone audiometry; shows loss of air conduction, Normal bone conduction and
Carhart's notch at 2000 Hz
5. Speech audiometry reveals normal discrimination score
6. Tympanometry; shows a curve of ossicular stiffness
7. Stapedial reflex is absent if stapes is fixed
d) TREATMENT:
1. Medical:
There is no medical treatment that cures otosclerosis. Sodium fluoride has been
tried but this treatment is not recommended generally.
2. Surgical:
Stapedectomy with a placement of prosthesis is the treatment of choice. Here the
fixed otosclerotic stapes is removed and a prosthesis inserted between the incus
and oval window Prosthesis employed may be a teflon piston, stainless steel
piston, platinum teflon or titanium teflon piston
e) COMPLICATIONS:
KMU Past Papers Solved SEQs
Ear 16
1. Tear of tympano-meatal flap and perforation of tympanic membrane
2. Injury to chorda tympani with taste disturbance
3. Injury to facial nerve
4. Incus dislocation
5. Vertigo
6. Conductive hearing loss
7. Labyrinthitis
8. Sensorineural hearing loss
9. Dead ear
Q-14. A 17 years old boy came to OPD with history of left ear smelling discharge for the last
three years. The discharge is scanty and sometimes blood stained. Examination showed an
attic perforation. On tuning fork test left rinne’s test was negative and weber lateralize
towards the ipsilateral ear.
a) What is your diagnosis?
b) How will you investigate the patient? Give justifications.
c) What are the treatment option?
d) Name complication of the surgical procedure required in this condition.
ANS:
a) DIAGNOSIS:
Chronic suppurative otitis media (unsafe ear)
b) INVESTIGATIONS:
1. Examination under microscope It may reveal presence of cholesteatoma, its site
and extent, evidence of bone destruction, granuloma, condition of ossicles and pockets
of discharge.
2. Tuning fork tests and audiogram They are essential for pre-operative assessment
and to confirm the degree and type of hearing loss.
3. X-ray mastoids/CT scan temporal bone They indicate extent of bone destruction
and degree of mastoid pneumatisation. They are useful to indicate a low-lying dura or
an anteposed sigmoid sinus when operation is being contemplated on a sclerotic
mastoid. Cholesteatoma causes destruction in the area of attic and antrum (key area),
better seen in lateral view. CT scan of temporal bone gives more information and is
preferred to X-ray mastoids.
4. Culture and sensitivity of ear discharge It helps to select proper antibiotic for
local or systemic use.
c) TREATMENT:
a) Surgical: Two types of surgical procedures are done to deal with cholesteatoma:
i) Canal wall down procedures. They leave the mastoid cavity open into the
external auditory canal. The commonly performed operations for
atticoantral disease are atticotomy, modified radical mastoidectomy and
rarely, the radical mastoidectomy.
KMU Past Papers Solved SEQs
Ear 17
ii) Canal wall up procedures. Here disease is removed by combined approach
through the meatus and mastoid but retaining the posterior bony meatal
wall intact, thereby avoiding an open mastoid cavity. It gives dry ear and
permits easy reconstruction of hearing mechanism.
b) Reconstructive surgery Hearing can be restored by myringoplasty or
tympanoplasty. It can be done at the time of primary surgery or as a second stage
procedure.
c) Conservative treatment: when cholesteatoma is small and easily accessible to
suction clearance under operating microscope. It can also be tried out in elderly
patients above 65 and those who are unfit for general anaesthesia or those
refusing surgery.
d) Polyps and granulations can also be surgically removed by cup forceps or
cauterised by chemical agents like silver nitrate or trichloroacetic acid.
e) Other measures like aural toilet and dry ear precautions are also essential.
d) COMPLICATIONS:
1. Pain: Pain is uncommon in uncomplicated CSOM. Its presence is considered
serious as it may indicate extradural, perisinus or brain abscess. Sometimes, it is
due to otitis externa associated with a discharging ear.
2. Vertigo It indicates erosion of lateral semicircular canal which may progress to
labyrinthitis or meningitis. Fistula test should be performed in all cases.
3. Persistent headache It is suggestive of an intracranial complication.
4. Facial weakness indicates erosion of facial canal.
5. A listless child refusing to take feeds and easily going to sleep (extradural abscess).
6. Fever, nausea and vomiting (intracranial infection).
7. Irritability and neck rigidity (meningitis).
8. Diplopia (Gradenigo's syndrome).
9. Ataxia (labyrinthitis or cerebellar abscess).
10. Abscess round the ear (mastoiditis).
Q-15. A 25-year-old male complains of tight nasal obstructions and right tenderness of cheek
seven days after common cold. On examination there was mucopus in right nostril and
postnasal drip.
a) What is the most probable diagnosis?
b) What are the organisms involved?
c) Name the investigations of choice with justifications
d) How will you treat the patient?
ANS:
a) DIAGNOSIS:
Acute maxillary sinusitis
b) ORGANISMS INVOLVED
KMU Past Papers Solved SEQs
Ear 18
1. Streptococcus pneumonae
2. H influnzae
3. Morazella catarrhalis
4. Strep pyogens
5. Stap aurus
6. Klebsellia
c) INVESTIGATION:
1. transillumination test the sinus will opaque
2. X ray water’s view show opacities or fluid in the sinus
3. CT scan show for any bone erosion
d) TREATMENT
Medical:
1. Anti-microbial drugs
2. Nasal decongested drops
3. Steam inhalation
4. Analgesics
5. Hot fomentation
Surgical:
1. Antral lavage
2. Antral puncure and iregation
3. Intranasal antrostomy
4. caldwell luc operation
Q-16. A 30 years old female complained of bilateral hearing loss more on the right side
following the delivery of her first child. Hearing loss was marked in quiet places but
improved in a noisy environment. Both tympanic membranes were mobile and showed a
normal appearance. Rinne’s test was negative on both sides.
a) What is the most likely diagnosis?
b) Enumerate the differential diagnosis
c) What investigations with justifications will you perform to reach the diagnosis?
ANS:
a) DIAGNOSIS:
Otosclerosis
b) DIFFERENTIAL DIAGNOSIS:
1. Serous otitis media,
2. Adhesive otitis media,
3. Tympanosclerosis,
4. Attic fixation of head of malleus,
5. Ossicular discontinuity
6. Congenital stapes fixation.
KMU Past Papers Solved SEQs
Ear 19
c) INVESTIGATIONS
1. Tuning fork test; show negative Rinne (i.e. BC > AC)
2. Weber test; lateralised to the ear with greater conductive loss.
3. Absolute bone conduction may be normal.
4. Pure tone audiometry; shows loss of air conduction, Normal bone conduction and
Carhart's notch at 2000 Hz
5. Speech audiometry reveals normal discrimination score
6. Tympanometry; shows a curve of ossicular stiffness
7. Stapedial reflex is absent if stapes is fixed
Q-17. A young boy of 7 years presents to Ent OPD complaining of marked earache on right
side with high grade fever. He was treated by his family physician for right acute otitis
media. On examination tympanic membrane is red and bulging with erection of pinna md
mastoid tenderness.
a) What is the most likely diagnosis?
b) What are your differential diagnosis?
c) How will you investigate?
d) How Will treat this patient?
ANS:
a) DIAGNOSIS:
Acute mastoiditis
b) DIFFERENTIAL DIAGNOSIS:
1. Suppuration of mastoid lymph nodes in Scalp infection
2. Furunculosis of meatus.
3. Infected sebaceous cyst
c) INVESTIGATIONS:
1. Blood counts show polymorphonuclear leucocytosis.
2. ESR is usually raised.
3. X-ray mastoid There is clouding of air cells due to collection of exudate in them.
Bony partitions between air cells become indistinct, but the sinus plate is seen as a
distinct outline. In later stages, a cavity may be seen in the mastoid.
4. Ear swab for culture and sensitivity.
d) TREATMENT:
1. Hospitalisation of the patient.
2. Antibiotics: start with amoxicillin or ampicillin. Specific antimicrobial is started on
the receipt of sensitivity report. chloramphenicol or metronidazole is used for
anaerobic organisms.
3. Myringotomy When pus is under tension it is relieved by wide myringotomy
4. Cortical mastoidectomy It is indicated when there is:
i) Subperiosteal abscess.
KMU Past Papers Solved SEQs
Ear 20
ii) Sagging of posterosuperior meatal wall.
iii) Positive reservoir sign,
iv) No change in condition of patient or it worsens in spite of adequate
medical treatment for 48 hours.
v) Mastoiditis, leading to complications, e.g. facial paralysis, labyrinthitis,
intracranial complications, etc.
Q-18. A 4-year-old child was brought to ENT outpatient of hospital with history of nose &
mouth breathing snoring at night for the last 17 months. The parent also observed that he
is hard of hearing for the last 4 months. Clinical examination shows mucous in nasal
cavities, both tympanic membranes are intact and shows signs of pathology inside.
Systemic and hematological testes are unremarkable.
a) What are two most likely diagnoses?
b) Enumerate two most investigations?
c) Advise treatment options?
d) Name two procedure for this patient?
ANS:
a) DIAGNOSIS:
1. Adenoids causing serous otitis media
2. Chronic rhinitis causing serous otitis media
b) INVESTIGATIONS:
1. Tuning fork tests show conductive hearing loss.
2. Audiometry. There is conductive hearing loss of20—40 dB. Sometimes, there is
associated sensorineural hearing loss due to fluid pressing on the round window
membrane. This disappears with evacuation of fluid.
3. Impedance audiometry. It is an objective test useful in infants and children. Presence
of fluid is indicated by reduced compliance and flat curve with a shift to negative side.
4. X-ray mastoids. There is clouding of air cells due to fluid.
c) TREATMENT:
Medical
1. Decongestants: Topical decongestants in the form of nasal drops, sprays or
systemic decongestants.
2. Anti-allergic measures: Anti histaminic or steroids are used, if possible, allergen
should be found and desensitization done.
3. Antibiotics: in cases of upper respiratory tract infections or unresolved acute
suppurative otitis media.
4. Middle ear aeration: through Valsalva maneuver, politzerisation or Eustachian
tube catheterization. Children can be given chewing gum to encourage repeated
swallowing which opens the tube.
d) SURGICAL PROCEDURE:
1. Myringotomy and aspiration of fluid.
KMU Past Papers Solved SEQs
Ear 21
2. Grommet insertion to provide continued aeration of middle ear.
3. Tympanotomy or cortical mastoidectomy.
4. Surgical treatment of causative factor Adenoidectomy, tonsillectomy and/or wash-
out of maxillary antra.
Q-19. A 27 years old patient presented to ENT OPD with complaint of foul smelling discharge
from the right ear for several years. The discharge is scanty and sometimes blood stained.
Clinical examination shows right side mixed hearing loss. On otoscopy there is
posterosuperior marginal perforation
a) What is your diagnosis?
b) How will you investigate him?
c) What surgical procedures are available for the patient?
d) What complications can occur if the condition goes untreated?
ANS:
a) Diagnosis:
Chronic suppurative otitis media (unsafe ear)
b) investigations:
1. Examination under microscope It may reveal presence of cholesteatoma, its site and
extent, evidence of bone destruction, granuloma, condition of ossicles and pockets of
discharge.
2. Tuning fork tests and audiogram They are essential for pre-operative assessment and
to confirm the degree and type of hearing loss.
3. X-ray mastoids/CT scan temporal bone They indicate extent of bone destruction and
degree of mastoid pneumatisation. They are useful to indicate a low-lying dura or an
anteposed sigmoid sinus when operation is being contemplated on a sclerotic
mastoid. Cholesteatoma causes destruction in the area of attic and antrum (key area),
better seen in lateral view. CT scan of temporal bone gives more information and is
preferred to X-ray mastoids.
4. Culture and sensitivity of ear discharge It helps to select proper antibiotic for local or
systemic use.
c) treatment:
1. Surgical: Two types of surgical procedures are done to deal with cholesteatoma:
i) Canal wall down procedures. They leave the mastoid cavity open into the
external auditory canal. The commonly performed operations for atticoantral
disease are atticotomy, modified radical mastoidectomy and rarely, the radical
mastoidectomy.
ii) Canal wall up procedures. Here disease is removed by combined approach
through the meatus and mastoid but retaining the posterior bony meatal wall
intact, thereby avoiding an open mastoid cavity. It gives dry ear and permits
easy reconstruction of hearing mechanism..
KMU Past Papers Solved SEQs
Ear 22
2. Reconstructive surgery Hearing can be restored by myringoplasty or
tympanoplasty. It can be done at the time of primary surgery or as a second stage
procedure.
3. Conservative treatment: when cholesteatoma is small and easily accessible to
suction clearance under operating microscope. It can also be tried out in elderly
patients above 65 and those who are unfit for general anaesthesia or those
refusing surgery.
4. Polyps and granulations can also be surgically removed by cup forceps or
cauterised by chemical agents like silver nitrate or trichloroacetic acid.
5. Other measures like aural toilet and dry ear precautions are also essential.
d) complications:
1. Pain: Pain is uncommon in uncomplicated CSOM. Its presence is considered
serious as it may indicate extradural, perisinus or brain abscess. Sometimes, it is
due to otitis externa associated with a discharging ear.
2. Vertigo It indicates erosion of lateral semicircular canal which may progress to
labyrinthitis or meningitis. Fistula test should be performed in all cases.
3. Persistent headache It is suggestive of an intracranial complication.
4. Facial weakness indicates erosion of facial canal.
5. A listless child refusing to take feeds and easily going to sleep (extradural abscess).
6. Fever, nausea and vomiting (intracranial infection).
7. Irritability and neck rigidity (meningitis).
8. Diplopia (Gradenigo's syndrome).
9. Ataxia (labyrinthitis or cerebellar abscess).
10. Abscess round the ear (mastoiditis).
Q-20. A 45 years old lady presented with itching, excruciating pain, ear discharge and ear
blockage for the last one week. On examination granulations are seen in the floor of
external auditory meatus. Her random blood sugar is 300mg/100 ml.
a) What is your diagnosis and the common causative organism?
b) What complications can occur?
c) How do you treat the patient?
ANS:
a) DIAGNOSIS:
Malignant (nacrotizing) otitis externa and the organism is pseudomonas
b) COMPLICATIONS:
1. Facial paralysis is common
2. Infection may spread to the skull base and jugular foramen causing multiple cranial
nerve palsies.
3. Anteriorly, infection spreads to temporomandibular fossa,
4. Posteriorly to the mastoid causing mastoidites
KMU Past Papers Solved SEQs
Ear 23
5. Medially into the middle ear and petrous bone causing otitis media and Petrositis
respectively
c) TREATMENT:
1. High doses of IV antibiotics directed against pseudomonas (tobramycin, ticarcillin or
third generation cephalosporin). Antibiotics are given for 6-8 weeks or longer.
2. Diabetes should be controlled.
3. Surgical debridement of devitalized tissue and bone should be done judiciously.
4. Radical resections.
Q-21. A 9-year-old child was brought to emergency having headache and vomiting the
attending physician examined him and found neither surgical nor medical nor
gastrointestinal cause for vomiting. The parents reported right offensive ear discharge
since early childhood. Otologic examination showed a left retracted tympanic membrane
and a right red fleshy pedunculated mass with an offensive otorrhea. Temperature was 38
degrees Celsius and there was staggering gait and slowness of speech.
a) What is most likely diagnosis?
b) Describe the required investigation to confirm the diagnosis.
c) How will you treat this patient?
ANS:
a) DIAGNOSIS:
Otogenic brain abscess
b) INVESTIGATIONS:
1. Skull X-rays to see:
i. midline shift,
ii. pineal gland calcification
iii. gas in the abscess cavity.
2. CT scan:
i. to find the site and size of an abscess
ii. associated complications such as extradural abscess, sigmoid sinus
thrombosis,
3. MRI for further improved the diagnosis.
4. X-ray mastoids or CT scan: for associated ear disease.
5. Lumbar puncture: CSF will show
i. rise in pressure,
ii. increase in protein content
iii. normal glucose level.
iv. White cell count is raised but less than that of meningitis.
v. polymorphs or lymphocytes some time present.
c) TREATMENT:
1. Medical High doses of antibiotics are given parenterally,
i. Chloramphenicol and third generation cephalosporin are usually effective.
KMU Past Papers Solved SEQs
Ear 24
ii. Metronidazole for obligate anaerobe Bacteroides fragilis, brain abscess,
iii. Gentamicin, for pseudomonas or proteus.
iv. dexamethasone, or mannitol for lowering Raised intracranial tension.
v. Discharge from the ear should be treated by suction clearance and use of
topical ear drops.
2. Neurosurgical Abscess is approached through a sterile field
i. repeated aspiration through a burr hole, followed by repeat CT or MRI
scans to see if it diminishes in size
ii. excision of abscess, in expanding abscess, or one that does not decrease in
size,
iii. open incision of the abscess and evacuation of pus.
iv. Penicillin can be instilled into the abscess after aspiration.
3. Otologic
i. Acute otitis media might have resolved with the antibiotics given for the
abscess.
ii. Chronic otitis media would require radical mastoidectomy to remove the
irreversible disease and to exteriorise the infected area.
iii. Surgery of the ear is undertaken only after the abscess has been controlled
by antibiotics and neurosurgical treatment.
d) OPTIONAL (for study)
Stages of otogenic brain abscess formation
(a) Stage of invasion (initial encephalitis)
(b) Stage of localisation (latent abscess)
(c) Stage of enlargement (manifest abscess)
(d) Stage of termination (rupture of abscess) resulting in fatal meningitis.
Q-22. A 48-year-old male patient has been complaining over the last 5 year of attacks of
incapacitating vertigo tinnitus and decreasing hearing during the attack there was a sense
of aural fullness, in between the attacks that usually occur twice or three time in a year.
The patient feels fine. the patent also reported that his ability is decreasing over the years,
examination of the ears showed bilateral normal tympanic membrane
a) What is the most probable diagnosis?
b) Name three important differential diagnosis.
c) How will you treat the patient?
ANS:
a) DIAGNOSIS:
Meniere’s disease
b) DIFFERENTIAL DIAGNOSIS
1. Vestibular neuronitis: viral infection of vestibular ganglion
2. Perilymph fistula
3. Congenital syphilis
KMU Past Papers Solved SEQs
Ear 25
4. Head injury
5. Cogan syndrome
6. Otosclerosis.
c) TREATMENT:
Medical treatment:
A. General Measures
1. Reassurance: relieve the Patient's anxiety can be by reassurance and by
explaining the true nature of disease.
2. Cessation of smoking: Nicotine causes vasospasm.
3. Low salt diet: Patient should take salt-free diet as far as possible.
4. Avoid excessive intake of water
5. Avoid over-indulgence in coffee, tea and alcohol
6. Avoid stress and bring a change in life-style
7. Avoid activities requiring good body balance, such as flying, under-water diving or
working at great heights should be avoided.
B. Management of Acute Attack
1. Reassurance and psychological support to allay worry and anxiety.
2. Bed rest with head supported on pillows to prevent excessive movements.
3. Vestibular sedatives to relieve vertigo.
dimenhydrinate (Dramamine), prochlorperazine (Stemetil) IM or IV.
Diazepam (Valium or Calmpose IV,
atropine, 0.4 mg, given subcutaneously for acute attack.
4. Vasodilators
Inhalation of carbogen (5% CO with 95% O). It is a good cerebral vasodilator and
improves labyrinthine circulation.
Histamine diphosphate infusion, helps to control acute attacks. (contraindicated
in asthmatics)
C. Management of Chronic Phase
1. Vestibular sedatives: Prochlorperazine (Stemetil) 10mg orally
2. Vasodilators
Nicotinic acid, 50 mg, before meals thrice a day.
Betahistine (Vertin) 8-16 mg, thrice a day, given orally
3. Diuretics: Furosemide, 40 mg tablet, taken on alternate days with potassium
supplement.
4. Propantheline bromide (Probanthine), 15mg, thrice a day,
5. Elimination of allergen through elimination or desensitization.
6. Hormones Replacement therapy in case of hypothyroidism
7. Intra-tympanic gentamicin therapy: (chemical labyrinthectomy). biweekly
injections gentamicin into the middle ear.
8. Microwick is pass though grommet in tympanic membrane to deliver drug,
gentamicin or steroids, to oval windows, it avoids repeated intra-tympanic
injections.
KMU Past Papers Solved SEQs
Ear 26
Surgical treatment:
A. Conservative procedures: They are used in cases where hearing is still useful and
needs to be preserved.
i. Decompression of endolymphatic sac.
ii. Endolymphatic shunt operation. A tube is put, connecting endolymphatic sac with
subarachnoid space, to drain excess endolymph.
iii. Sacculotomy
Fick's operation It is puncturing the saccule with a needle through stapes
footplate.
Cody's tack procedure consists of placing a stainless steel tack through the
stapes footplate. The tack would cause periodic decompression of the saccule
when it gets distended.
Cochleosacculotomy: instead of saccule, cochlear duct is punctured and
drained into the perilymph.
iv. Section of vestibular nerve. The nerve is exposed by retro-sigmoid or middle
cranial fossa approach and selectively sectioned.
v. Ultrasonic destruction of vestibular labyrinth.
B. Destructive procedures They totally destroy cochlear and vestibular function
i. Labyrinthectomy. Membranous labyrinth is completely destroyed either by
opening through the lateral semicircular canal by transmastoid route or through
the oval window by a transcanal approach.
C. Intermittent low pressure pulse therapy (Meniett device therapy):
Intermittent positive pressure waves can be delivered through this device
i. myringotomy is performed and ventilation tube is inserted.
ii. the device then delivers pressure waves to the round window membrane via the
ventilation tube.
iii. Pressure waves pass through the perilymph and cause reduction in endolymph
pressure by redistributing it through various communication channels such as
the endolymphatic sac or the blood vessels
iv. Pressure also regulate secretion of endolymph by the stria vascularis
Q-23. What are the different causes of mixed hearing loss?
What are different treatment option for otosclerosis?
ANS:
a) Causes of mixed hearing loss:
1. Otosclerosis
2. Chronic suppurative otitis media
b) Treatment of otosclerosis:
1. Medical:
KMU Past Papers Solved SEQs
Ear 27
There is no medical treatment that cures otosclerosis. Sodium fluoride has been tried
but this treatment is not recommended generally.
2. Surgical:
Stapedectomy with a placement of prosthesis is the treatment of choice. Here the
fixed otosclerotic stapes is removed and a prosthesis inserted between the incus and
oval window Prosthesis employed may be a teflon piston, stainless steel piston,
platinum teflon or titanium teflon piston
Q-24. A 60 years old female presented with severe right otalgia and right facial palsy for the
last 3 days, on further questioning she was diabetic for the last 5 years with on oral
antidiabetic therapy, on examination there are granulation tissues in the external auditory
canal lower motor neuron facial palsy random glucose estimation is 300mg/dl
a) What is most probable diagnosis?
b) Enumerate 3 condition which are considered to be predisposing?
c) What investigation would you like to order for the patient?
d) How will you treat this patient?
ANS:
a) Diagnosis:
Malignant (nacrotizing) otitis externa
b) predisposing conditions:
1. advancing age
2. diabetes mellitus
3. those on immunosuppressive drugs
4. HIV positive individuals
c) Investigations:
1. CT scan to know the extent of disease
2. Gallium 67 for the soft tissue infections because it is taken by reticular endothelial
cells
3. Technetium 99 bone scan
d) Treatment:
1. High doses of IV antibiotics directed against pseudomonas (tobramycin, ticarcillin or
third generation cephalosporin). Antibiotics are given for 6-8 weeks or longer.
2. Diabetes should be controlled.
3. Surgical debridement of devitalized tissue and bone should be done judiciously.
KMU Past Papers Solved SEQs
Ear 28
4. Radical resections.
Q-25. A 9 years old child was brought to emergency having headache and vomiting. The
attending physician examined him and found neither surgical nor medical or
gastrointestinal causes for such vomiting. The parents reported right offensive ear
discharge since early childhood. Otologic examination showed a left retraced tympanic
membrane and a right red flashy pedunculated mass with an offensive otorrhea.
Temperature was 38 degrees Celsius and there was staggering gait and slowness of
speech.
a) What is the most likely diagnosis?
b) Describe the required investigation to confirm the diagnosis?
c) How will you treat this patient?
ANS:
a) DIAGNOSIS:
Otogenic brain abscess
b) INVESTIGATIONS:
1. Skull X-rays to see:
i. midline shift,
ii. pineal gland calcification
iii. gas in the abscess cavity.
2. CT scan:
i. to find the site and size of an abscess
ii. associated complications such as extradural abscess, sigmoid sinus
thrombosis,
3. MRI for further improved the diagnosis.
4. X-ray mastoids or CT scan: for associated ear disease.
5. Lumbar puncture: CSF will show
i. rise in pressure,
ii. increase in protein content
iii. normal glucose level.
iv. White cell count is raised but less than that of meningitis.
v. polymorphs or lymphocytes some time present.
c) TREATMENT:
1. Medical High doses of antibiotics are given parenterally,
i) Chloramphenicol and third generation cephalosporin are usually effective.
ii) Metronidazole for obligate anaerobe Bacteroides fragilis, brain abscess,
iii) Gentamicin, for pseudomonas or proteus.
iv) dexamethasone, or mannitol for lowering Raised intracranial tension.
v) Discharge from the ear should be treated by suction clearance and use of
topical ear drops.
KMU Past Papers Solved SEQs
Ear 29
2. Neurosurgical Abscess is approached through a sterile field
i) repeated aspiration through a burr hole, followed by repeat CT or MRI
scans to see if it diminishes in size
ii) excision of abscess, in expanding abscess, or one that does not decrease in
size,
iii) open incision of the abscess and evacuation of pus.
iv) Penicillin can be instilled into the abscess after aspiration.
3. Otologic
i) Acute otitis media might have resolved with the antibiotics given for the
abscess.
ii) Chronic otitis media would require radical mastoidectomy to remove the
irreversible disease and to exteriorise the infected area.
iii) Surgery of the ear is undertaken only after the abscess has been controlled
by antibiotics and neurosurgical treatment.
d) OPTIONAL (for study)
Stages of otogenic brain abscess formation
(a) Stage of invasion (initial encephalitis)
(b) Stage of localisation (latent abscess)
(c) Stage of enlargement (manifest abscess)
(d) Stage of termination (rupture of abscess) resulting in fatal meningitis.
Q-26. A 6 years old boy presented to ENT OPD with complaints of being hard of hearing for
the last 6 months. On further questioning he has snoring and nasal Obstruction for the last
1 year. Examination revealed mucous in the nose, swelling in the nasopharynx and dull
tympanic membrane on otoscopy. Systemic and blood examinations are unremarkable.
a) What is your most probable diagnosis?
b) What minimal investigations will you prefer in this case? Justify your investigation
(not more than three lines)?
c) Enumerate surgical treatment of this condition?
d) What structural abnormalities can be caused if not treated?
ANS:
a) DIAGNOSIS:
Serous otitis media (Glue ear)
b) INVESTIGATIONS WITH JUSTIFICATION:
(i) Tuning fork tests show conductive hearing loss.
(ii) Audiometry. There is conductive hearing loss of20—40 dB. Sometimes, there is
associated sensorineural hearing loss due to fluid pressing on the round window
membrane. This disappears with evacuation of fluid.
KMU Past Papers Solved SEQs
Ear 30
(iii) Impedance audiometry. It is an objective test useful in infants and children. Presence
of fluid is indicated by reduced compliance and (type B) flat curve with a shift to negative
side.
(iv) X-ray mastoids. There is clouding of air cells due to fluid.
c) SURGICAL TREATMENT:
1. Myringotomy and aspiration of fluid.
2. Grommet insertion to provide continued aeration of middle ear.
3. Tympanotomy or cortical mastoidectomy.
4. Surgical treatment of causative factor Adenoidectomy, tonsillectomy and/or wash-out
of maxillary antra.
d) COMPLICATIONS:
1. Atrophic tympanic membrane and atelectasis of the middle ear.
2. Ossicular necrosis.
3. Tympanosclerosis and ossicular fixation.
4. Retraction pockets and cholesteatoma.
5. Cholesterol granuloma.
Q-27. A fifth class student received slap on his face from his teacher. He presents to ENT
specialist with complaints of blocked left ear and slight bleed from the ear which stopped
itself after itself after sometime.
a) What is your most probable diagnosis?
b) What point would you tell to patient/attendant during counseling?
a) How will you treat this patient?
ANS:
a) DIAGNOSIS:
Perforation of tympanic membrane
b) COUNSELING:
1. Take care of ear
2. Do not let water get into that ear until tympanic membrane is healed,
3. Use cotton swab while taking bath.
c) TREATMENT:
1. Antibiotic oral
2. Splintage: It is used in fresh traumatic perforations. The torn edges of the
perforation are carefully everted under the microscope and splinted with
absorbable gel foam placed in the middle ear through the tear. Smaller tears can
be splinted on the outer surface of the tympanic membrane with a piece of
cigarette paper, gelfdm or silicon sheet.
KMU Past Papers Solved SEQs
Ear 31
Q-28. One-year-old child having acute rhinitis was crying the whole night. He became calm
quiet and slept early in morning, presented to ENT specialist with reddish purulent
discharge from left ear.
a) what is the likely diagnosis?
b) How will you treat him?
c) What instructions would you like to give to the parents?
ANS:
a) DIAGNOSIS:
Acute suppurative otitis media
b) TREATMENT:
1. Antibacterial therapy:
For Strept. pneumoniae and H. influenza, effective drugs are ampicillin, amoxicillin. Those
allergic to these penicillins can be given cefaclor, co-trimoxazole or erythromycin.
In cases where beta-lactamase-producing H. influenzae or Moraxella catarrhalis are
isolated, antibiotics like amoxicillin clavulanate, augmentin, cefuroxime axetil or cefixime
may be used.
2. Decongestant nasal drops:
Ephedrine nose drops, oxymetazoline or xylometazoline if nasal drops are difficult to
administer use Oral nasal decongestants Pseudoephedrine or a combination of
decongestant and antihistamine.
4. Analgesics and antipyretics:
Paracetamol helps to relieve pain and bring down temperature.
5. Ear toilet If there is discharge in the ear, it is dry mopped with sterile cotton buds
and a wick moistened with antibiotic may be inserted.
6. Dry local heat It helps to relieve pain.
7. Myringotomy It is incising the drum to evacuate pus and is indicated only when
(a) drum is bulging and there is acute pain,
(b) there is an incomplete resolution despite antibiotics when drum remains full with
persistent conductive deafness,
(c) there is persistent effusion beyond 12 weeks.
c) INSTRUCTIONS:
Antibacterial therapy must be continued for a minimum of 10 days, till tympanic
membrane regains normal appearance and hearing returns to normal.
Not to discontinue therapy early with relief of earache and fever, or therapy given in
inadequate doses may lead to secretory otitis media and residual hearing loss.
Follow all cases of acute suppurative otitis media should be carefully followed till drum
membrane returns to its normal appearance.
KMU Past Papers Solved SEQs
Nose and Paranasal Sinuses 32
Q-1. A 5 years old child brought by mother to ENT OPD with right side nasal obstruction
and blood stained foul smelling discharge on the right side. General physical examination
and the rest of ENT examination is unremarkable.
a) What is the most probable diagnosis?
b) Give at least two differential diagnoses?
c) How will you treat this Child?
d) What are the indications for general and anesthesia in this case?
e) While treating under GA is intubation required?
ANS:
a) DIAGNOSIS:
Foreign body
b) DD’S
1. Rhinolith
2. Nasal diphtheria,
3. Nasal myasisi,
c) TREATMENT
1. Under proper light use pair of forceps, or if round body use uestachian catherther,
2. If not visible directly through naso endoscope foreign body is removed
d) INDICATION FOR GENERAL ANESTHESIA
Uncooperative child
e) yes, obviously endotracheal tube is required for general anesthesia
Q-2. A 40 years old woman has attended ENT OPD on several occasions per preceding
years. She gave a long H/O symptom the most important being constant mucopurulent
nasal discharge and nasal obstruction. She frequently suffered from headache and facial
pain. her sense of smell was also impaired. On examination there were crusts and
purulent secretion in both nasal cavities. Standard sinus x-rays demonstrated maxillary
sinuses.
a) What is the most likely diagnosis?
b) Enlist etiological factor of sinusitis in general.
c) Enumerate briefly discuss both medical and surgical treatment options.
ANS:
a) DIAGNOSIS
Bilateral chronic maxillary sinusitis
b) ETIOLOGICAL FACTORS
A. Exciting causes:
1. Nasal infections
2. Swimming and diving
3. Trauma
KMU Past Papers Solved SEQs
Nose and Paranasal Sinuses 33
4. Dental infection
B. Predisposing condition:
1. Obstruction of ventilation and drainage of sinuses
i) Nasal packing
ii) Deviated septum
iii) Hypertrophic turbinate
iv) Edema of sinus ostia
v) Nasal polyp
vi) Tumors
2. Stasis of secretion in the nasal cavity ie cystic fibrosis enlarge adenoids coanal
atresia
3. Previous attack of sinuses
C. Bacterial infections:
1. Streptococcus pneumonae,
2. H influnzae
3. Morazella catarrhalis,
4. Strep pyogens,
5. Stap aurus,
6. Klebsellia
c) TREATMENT OPTIONS:
A. Medical:
1. Anti-microbial drugs
2. Nasal decongested drops
3. Steam inhalation
4. Analgesics
5. Hot fomentation
B. Surgical:
1. Antral lavage
2. Antral puncture and irrigation
3. Intranasal antrostomy
4. Caldwell luc operation
Q-3. A 10. years Old patient was brought to ENT OPD history of nose bleeding.
a) what points will you asked in the history to reach the diagnosis.
b) how will you Confirm the diagnosis?
ANS:
a) POINT ASKED IN HISTORY:
In any case of epistaxis, it is important to know:
1. Mode of onset. Spontaneous or finger nail trauma.
2. Duration and frequency of bleeding.
3. Amount of blood loss.
KMU Past Papers Solved SEQs
Nose and Paranasal Sinuses 34
4.Side of nose from where bleeding is occurring.
5.Whether bleeding is of anterior or posterior type.
6.Any known bleeding tendency in the patient or family.
7.History of known medical ailment (hypertension, leukaemias, mitral valve disease,
cirrhosis, nephritis).
8. History of drug intake (analgesics, anticoagulants, etc.).
b) INVESTIGATIONS FOR DIAGNOSIS:
1. Anterior rhinoscopy for the sight of bleeding and any spur
2. Posterior rhinoscopy
3. X ray CT scan MRI for any tumor
4. Blood studies for any coagulation disorders
Q-4. A 25 years old male presented to ENT OPD with nasal obstruction. sneezing and
rhinorrhea. On examination the nasal mucosa is bluish looking with enlarged inferior
turbinate and thin nasal discharge. The rest of ENT examination was normal.
a) What is the most probable diagnosis?
b) What are the tow differential diagnoses?
c) How will you investigate this patient?
d) What are different treatment options?
ANS:
a) DIAGNOSIS:
Allergic rhinitis
b) DDs
1. Chronic simple rhinitis
2. Hypertrophic rhinitis
c) INVESTIGATION:
1. Total DLC peripheral eosinophilia
2. Nasal smear increased number of eosinophils
3. Skin test skin prick test and specific IgE measurement
4. Radioallergosorbent Test RAST measure IgE antibodies in patient serum
5. Nasal provocation test
d) TREATMENT:
A. Avoidance of allergen
B. Treatment with drugs ie
1. Antihistamines (diphehydramines)
2. Sympathomimetic (phenylephrine)
3. Corticosteroids (belcomethasone)
4. Sodium chromo glycated mast cell stabilizers
5. Anticholinergics (ipratropium bromide)
6. Leukotrienes receptor antagonists (zafirlukast montelukast)
KMU Past Papers Solved SEQs
Nose and Paranasal Sinuses 35
7. Anti IgE (omalizumab)
Q-5. A 45 years old male came toe ENT OPD with chief complaints of bilateral nasal
obstruction, rhinorrhea and sneezing for the last 3 years. On examination the nasal
cavities contained multiple grapes like masses which were soft, pedunculated and
insensitive to touch on probe test.
a) What is your diagnosis?
b) What is the medical treatment of this condition?
c) What surgical options are available for this condition?
ANS
a) DIAGNOSIS:
Bilateral ethmoidal polyp
b) MEDICAL TREATMENT:
1. Antihistamines
2. Steroids
c) SURGICAL:
1. Polypectomy
2. Intranasal ethmoidectomy
3. Extranasal ethmoidectomy
4. Transantral ethmoidectomy
5. Endoscopic sinus surgery (functional endoscopic sinus surgery fess)
Q-6. A 55 years old male presented to ENT ware with mass in the right nasal cavity of
three-month duration. This mass was small to start with but increased over the three-
month period so much as to fill up the nasal fossa rather protruding through. The mass is
also associated with some pain and a blood stained discharge.
a) What is your probable diagnosis?
b) What surgical procedure would you like to perform before you order expensive
investigation?
c) Which type of nasal polyp must be bropside?
d) What imaging investigations. would you like to carry out?
e) Give 4 differential diagnoses of unilateral nasal mass?
ANS:
a) DIAGNOSIS:
Inverted papilloma
b) SURGICAL PROCEDURE
Endoscopy
c) NASAL POLYP BIOPSIED
Unilateral nasal polyp
KMU Past Papers Solved SEQs
Nose and Paranasal Sinuses 36
d) INVESTIGATIONS
1. CT scan and MRI shows the extent of lesion
2. Biopsy
e) DDS
1. Squamous papilloma
2. Squamous cell carcinoma
3. Antroconal polyp
4. Dermoid
Q-7. 13 years old boy presented to ENT OPD with nasal obstruction, which was on one side
initially and only in expiration, but later on became bilateral and in both t phases of
respiration. Anterior rhinoscopy does not reveal significant obstructive lesion while on
posterior rhinoscopy a smooth glistening mass can be visualized in nasopharynx. There is
no history of epistaxis at all.
a) What is the most probable diagnosis?
b) How will you treat this condition?
c) Give three differential diagnosis of mass in the nasopharynx.
d) How will you treat it if recurred though it rarely recurs?
ANS:
a) DIAGNOSIS:
Antrochoanal polyp
b) TREATMENT:
Polypectomy: Removed by avulsion either through nasal or oral route
c) DD
1. A blob of mucus
2. Hypetrophied middle turbinate
3. Juvenile naso-angiofibroma
d) TREATMENT IF RECURS
1. Caldwell luc operation to remove the polyp form the site of its origin ie maxillary
antrum and also treat coexistent sinusitis
2. Endoscopic sinus surgery is more common
KMU Past Papers Solved SEQs
Nose and Paranasal Sinuses 37
Q-8. 7 years Old child presented to the ENT clinic with the recurrent nose bleed. especially
in summer season when the child would be playing outside in hot sunny weather.
Examination of the nose revealed that bleeding is 'mainly from the anterior part of the
nose. The medical history of the child is unremarkable. The child is quite docile and
cooperative.
a) Which area of the is most probable site of bleeding in this case?
b) Name the vessels participating in a plexus around this area. Also name the main
origin of each vessel in bracket i.e ( )
c) What factors predispose this particular area to easy bleeding?
d) How will you manage this case?
e) What advice would you give to the attending mother?
ANS:
a) LITTLE AREA
b) VESSELS PARTICIPATING
1. Anterior artery branch of ophthalmic artery
2. Sphenopalatine artery branch of maxillary artery
3. Septal branch of greater palatine artery branch of maxillary artery
4. Septal branch of superior labial artery branch of fascial artery
c) PRE DISPOSING FACTORS
A. Local Factors
i) Nose picking finger nail Trauma
ii) Sinusitis
iii) Upper respiratory tract infections
iv) Allergies
v) Septal deviations ie nasal spur
vi) Tumors
B. Systemic Factors
i) Hereditary hemorrhagic telangiectasia
ii) Use of anticoagulants such as aspirin, clopidogrel, warfarin
iii) Wegener’s granulomatosis
iv) Thrombocytopenia
v) Hypertension
vi) Von Willabrand’s disease (most common)
vii) Factor VIII deficiency (Hemophilia A)
viii) Factor IX deficiency (Hemophilia B)
ix) Factor XI deficiency
d) MANAGEMENT:
1. First AID
2. Cauterization vasoconstrictor application
3. Anterior nasal packing
4. Endoscopic cauterization
KMU Past Papers Solved SEQs
Nose and Paranasal Sinuses 38
5. Elevation of mucoperichondrial flap and SMR
6. Ligation of vessel through transnasal endoscopic procedure and embolization
In any case of epistaxis, it is important to know:
1. Mode of onset. Spontaneous or finger nail trauma.
2. Duration and frequency of bleeding.
3. Amount of blood loss.
4. Side of nose from where bleeding is occurring.
5. Whether bleeding is of anterior or posterior type.
6. Any known bleeding tendency in the patient or family.
7. History of known medical ailment (hypertension, leukaemias, mitral valve disease,
cirrhosis, nephritis).
8. History of drug intake (analgesics, anticoagulants, etc.).
e) ADVISE:
tell the patient not to prick nose, avoid forceful blowing, avoid sneezing.
Q-9. A young boy aged 20 years presented to physician with nasal and palatal irritation
sneezing nasal discharge and nasal obstruction off and on usually during March to May
a) What is the most likely diagnosis?
b) Give four investigations for diagnosis of this case
c) How will you treat this patient?
ANS:
a) DIAGNOSIS:
Allergic rhinitis
b) INVESTIGATION:
1. Total DLC peripheral eosinophilia
2. Nasal smear increased number of eosinophils
3. Skin test skin prick test and specific IgE measurement
4. Radioallergosorbent Test RAST measure IgE antibodies in patient serum
5. Nasal provocation test
c) TREATMENT:
Avoidance of allergen
Treatment with drugs ie
1. Antihistamines (diphehydramines)
2. Sympathomimetic (phenylephrine)
3. Corticosteroids (belcomethasone)
4. Sodium chromo glycated mast cell stabilizers
5. Anticholinergics (ipratropium bromide)
6. Leukotrienes receptor antagonists (zafirlukast montelukast)
7. Anti IgE (omalizumab)
KMU Past Papers Solved SEQs
Nose and Paranasal Sinuses 39
Q-10. A 25-year young lady presented to ENT department with history of epistaxis, crusting
in the nose, nasal blockage and headache. On examination there was foul smelling from
nose and both the nasal cavities were roomy.
a) What is your diagnosis
b) Give a brief outline on its pathogenesis
c) How will you treat her?
ANS:
a) DIAGNOSIS:
Atrophic rhinitis (OZAENA)
b) PATHOGENESIS:
Various theories advanced regarding its causation are: (Mnemonic HERNIA)
a) Hereditary factors. Disease is known to involve more than one member in the same
family.
b) Endocrinal disturbance. Disease usually starts at puberty, involves females more than
males, the crusting and foetor associated with disease tends to cease after
menopause; these factors have raised the possibility of disease being an endocrinal
disorder.
c) Racial factors. White and yellow races are more susceptible than natives of equatorial
Africa.
d) Nutritional deficiency. Disease may be due to deficiency of vitamin A, D or iron or
some other dietary factors. The fact that incidence of disease is decreasing in western
countries and is rarely seen in wellto-do families raises the possibility of some
nutritional deficiency.
e) Various infections
Organisms have been cultured from cases of atrophic rhinitis such as Klebsiella
ozaenae, (Perez bacillus), diphtheroids, P. vulgaris, Esch. coli, Staphylococci and
Streptococci but they are all considered to be secondary invaders responsible for foul
smell rather than the primary causative organisms of the disease, i
f) Autoimmune process. The body reacts by a destructive process to the antigens
released from the nasal mucosa. Viral infection or some other unspecified agents may
trigger antigenicity of nasal mucosa.
c) TREATMENT
A. Medical
1. Nasal irrigation and removal of crusts. Warm normal saline or an alkaline
solution is used to irrigate the nasal cavities.
2. After crusts are removed, nose is painted with 25% glucose in glycerine.
3. Local antibiotics. Kemicetine™ antiozaena solution contains Chloromycetin,
oestradiol and vitamin D, and may be found useful.
4. Oestradiol spray. Helps to increase vascularity of nasal mucosa and
regeneration of seromucinous glands.
5. Placental extract injected submucosally in the nose may provide some relief.
KMU Past Papers Solved SEQs
Nose and Paranasal Sinuses 40
6. Systemic use of streptomycin. 1 g/day for 10 days has given good results in
reducing crusting and odour. It is effective against Klebsiella organisms.
7. Potassium iodide given by the mouth promotes and liquefies nasal secretion.
B. Surgical
1. Young's operation.
Both the nostrils are closed completely just within the nasal vestibule by
raising flaps. They are opened after 6 months or later. In these cases, mucosa
may revert to normal and crusting reduced.
2. Modified Young's operation.
To avoid the discomfort of bilateral nasal obstruction, modified Young's
operation aims to partially close the nostrils.
3. Narrowing the size of the nasal airway relieve the symptoms.
i) Submucosal injection of teflon paste.
ii) Insertion of fat, cartilage, bone or teflon strips under the
mucoperiosteum of the floor and lateral wall of nose and the
mucoperichondrium of the septum.
iii) Section and medial displacement of lateral wall of nose.
Q-11. A 28 years old female patient come with the complaint of bilateral nasal obstruction
sneezing and watery rhinorrhea for the past 8 to 10 years. Anterior rhinoscopy revealed
multiple pale smooth and shiny grapes like masses completely filling both nasal cavities
a) What is the most likely diagnosis in this case?
b) How will you investigate the patient?
c) How will you treat the patient?
ANS
a) DIAGNOSIS:
Bilateral ethmoidal polyp
b) INVESTIGATION:
1. Anterior rhinoscopy
2. Endoscopy
3. CT scan of paranasal sinuses is essential to exclude the bony erosion and expansion
suggestive of neoplasia.
c) MEDICAL TREATMENT:
3. Antihistamines
4. Steroids
d) SURGICAL:
6. Polypectomy
7. Intranasal ethmoidectomy
8. Extranasal ethmoidectomy
9. Transantral ethmoidectomy
10. Endoscopic sinus surgery (functional endoscopic sinus surgery fess)
KMU Past Papers Solved SEQs
Nose and Paranasal Sinuses 41
Q-12. A 60 years old male started to develop right sided progressively increasing nasal
obstruction for the last 6 months. This was followed by blood tinged nasal discharged
from the right side as well. Due to looseness of the right second upper molar tooth the
patient consulted a dentist who advised extraction. This resulted in an oroantral fistula,
on examination of neck there was firm swelling in the right upper neck.
a) What is your diagnosis and how will you justify the diagnosis?
b) What investigation are needed to confirm the diagnosis?
c) What are the treatment option?
ANS:
a) DIAGNOSIS
Carcinoma of maxillary sinus
justification:
1. Old age
2. Chronic obstruction
3. Blood tinged nasal discharge
4. Looseness of right second upper molar tooth probably due extension of
malignancy to base of maxillary sinus
5. Oroantral fistula formation
6. Swelling in right upper neck probably cervical lymph node involvement.
b) INVESTIGATIONS:
1. Radiograph of sinuses. Opacity of the involved sinus with expansion and
destruction of the bony walls.
2. CT scan. If available, this is the best non-invasive method to find the extent of
disease. CT scan should be done both in axial and coronal planes. It also helps
in the staging of disease.
3. Biopsy. If growth presents in the nose or mouth, biopsy can be easily taken. In
early cases, with suspicion of malignancy, sinus should be explored by
Caldwell-Luc operation. Direct visualisation of the site of tumour in the sinus
also helps in staging of the tumour.
4. Endoscopy of the nose and maxillary sinus will provide detailed examination.
An accurate biopsy can also be taken.
c) TREATMENT:
1. For squamous cell carcinoma, a combination of radiotherapy and surgery gives
better results than either alone.
2. Radiotherapy can be given before or after surgery.
3. full course of pre-operative telecobalt therapy is given, followed 4—6 weeks
later by surgical excision of the growth by total or extended maxillectomy
using Weber-Fergusson's incision.
KMU Past Papers Solved SEQs
Nose and Paranasal Sinuses 42
Q-13. A 58 years Old lady reported left nasal obstruction and discharge off and on for last 23
months, she underwent nasal surgery 3 year back for similar complaint histopathology is
not available. Her left nasal and posterior rhinosopy shows polynomial ugly looking
swellings, her plane radiograph of paranasal sinuses shows positive findings left side.
a) What is the most likely diagnosis?
b) Name two most important investigations?
c) Name treatment option.
d) Enumerate two surgical approaches.
ANS:
a) DIAGNOSIS:
Antro choanal polyp
b) INVESTIGATIONS:
1. Posterior rhynoscopy
2. Endoscopic examination
3. X ray lateral view
c) TREATMENT OPTION:
Removed by avulsion through nasal or oral route
d) SURGICAL PROCEDURE:
Caldwell luc and endoscopic sinus surgery
Q-14. A 65-year-old male developed following problem three days after visiting a barber
shop
Swollen shining tip of nose and sever pain in nose on touching
a) What is your diagnosis?
b) Give local complications
c) Name fatal compilations
d) Trace route of spread of infection for that fatal complication
e) How will our treat the patient?
ANS:
a) DIAGNOSIS:
Furuncle or boil
b) LOCAL COMPLICATIONS:
1. septal abscess
2. cellulitis of upper lip
c) FATAL COMPLICATION:
1. cavernous sinus thrombosis
d) ROUTE:
Through superior and inferior ophthalmic veins, the infection can be spread to cavernous
sinus.
e) TREATMENT
KMU Past Papers Solved SEQs
Nose and Paranasal Sinuses 43
1. warm compresses
2. analgesics to relieve pain
3. topical and systemic antibiotics directed against staphylococcus
4. Incision and drainage If a fluctuant area appears
KMU Past Papers Solved SEQs
Oral cavity Pharynx Larynx and Esophagus 44
Q-1. A 16 years Old male presented to ENT OPD with sore, throat, fever and difficulty in
opening the mouth for the last two days. On examination he was trismus and the right side
tonsil was congested. enlarged and pushed medially. His saliva was dribbling from his
mouth. His temperature was 101 OF. He also gives history of recurrent sore throat in the
past.
a) What is the most likely diagnosis?
b) What are the causative organisms involved?
c) Name four complications of this condition?
d) What are the different treatment options with justification?
ANS:
a) DIAGNOSIS:
Peri-tonsillar abscess
b) CAUSATIVE ORGANISMS:
1. Streptococcus pyogene,
2. Staph aurus,
3. Anaerobic organism
c) COMPLICATIONS:
1. Parapharyngeal abcess.
2. Odema of larynx
3. Septicemia
4. Pneumonitis or lung abcess
5. Jugular vein thrombosis
6. Spontaneous hemorrhage from carotic artery or jugular vein
D) TREATMENT:
A. Medical
1. hospitalization
2. intravenous fluid
3. antibiotics
4. analgesics
5. oral hygene
B. surgical
1. incision and drainage
2. interval tonsillectomy
3. hot tonssilectomy
KMU Past Papers Solved SEQs
Oral cavity Pharynx Larynx and Esophagus 45
Q-2. A 4 years Old child brought by his parents to clinic Complaining of breathing difficulty
and fever for last 24 hours. On examination he was having drooling of saliva, inspiratory
stridor and using his accessory muscles of respiration. He temperature was 102 0F. On
auscultation of chest air entry was equal on both sides.
a) What care should be taken while examining the patient?
b) What is the most probable diagnosis?
c) What are the causative organisms involved in this condition?
d) What is typical radiological sigh of the condition?
e) How will you treat the child?
ANS:
a) CARE TAKEN WHILE EXAMINATION
Indirect laryngoscopy is avoided for the fear of precipitating complete obstruction
It should be done in OT where intubation facilities are available
b) DIAGNOSIS:
Acute epiglottitis
c) CAUSATIVE ORGANISM
Hemophilus influnzae type B
d) RADIOLOGICAL SIGN
Thumb sign on lateral view Xray (swollen epiglottis)
e) TREATMENT
1. Hospitalization
2. Antibiotic ampicillin or third gen cephalosporins iv
3. Steroids hydrocortisone
4. Adequate hydration
5. Humidification and oxygen
6. intubation or tracheosotomy
Q-3. A middle age female is frequently visiting ENT clinic for her sore throat,
a) classify pharyngitis.
b) write at least five points you will ask in the history to differentiate pharyngitis and
tonsillitis.
c) how will you treat chronic nonspecific pharyngitis?
ANS
a) CLASSIFICATION
1. Acute pharyngitis
2. Chronic pharyngitis
b) RELEVANT HISTORY
1. Age: child most present with tonsillitis and adult with pharyngitis
2. Fever: high grade and unexplained fever in tonsillitis and low grade in pharyngitis
KMU Past Papers Solved SEQs
Oral cavity Pharynx Larynx and Esophagus 46
3. Ear ach: there is earache in tonsillitis while absent commonly in pharyngitis
4. Abdominal pain due to lymphadenitis present in tonsillitis and absent in pharyngitis
5. Constitutional symptoms ie headache body ach malaise are more severe in tonsilits
while mild in pharyngitis
c) TREATMENT
1. Sought and remove etiological agent ie smoking
2. Voice rest and speech therapy
3. Warm saline gargles
4. Application of Mandl’s paint on pharyngeal mucosa
5. Cautery of lymphoid granules through silver nitrate electrocautery or diathermy
under general anesthesia.
Q-4. A patient presented with dysphagia to ENT clinic. On physical examination the patient
was sitting comfortable in the bed neck examination reveal nothing unusual. IDL
examination was unmark able.
a) how will you classify dysphagia?
b) write at least three specific investigations this patient.
c) what are treatment options for carcinoma esophagus?
ANS:
a) DYSPHAGIA CLASSIFICATION:
A. Pre-oesophageal Causes
i) Oral phase.
1. Disturbance in mastication:
2. Disturbance in lubrication: xerostomia following radiotherapy, Mikulicz
disease.
3. Disturbance in mobility of tongue:
4. Defects of palate: cleft palate, oronasal fistula.
5. Lesions of buccal cavity and floor of mouth: stomatitis, ulcerative lesions,
Ludwig's angina.
ii) Pharyngeal phase.
1. Obstructive lesions of pharynx,
2. Inflammatory conditions
3. Spasmodic conditions, e.g. tetanus, rabies.
4. Paralytic conditions.
5. Paralysis of larynx-lesions of vagus and bilateral superior laryngeal nerves
cause aspiration of food into the larynx.
B. Oesophageal Causes
i) Lumen. Obstruction to lumen can occur in atresia, foreign body, strictures,
benign or malignant tumours.
KMU Past Papers Solved SEQs
Oral cavity Pharynx Larynx and Esophagus 47
ii)Wall. It can be acute or chronic oesophagitis, or motility disorders. The latter
are:
Hypomotility disorders, e.g. achalasia, sclerodenna, amyotrophic lateral
sclerosis.
Hypermotility disorders, e.g. cricopharyngeal spasm, diffuse oesophageal
spasm.
iii) Outside the wall. The lesions cause obstruction by pressing on the oesophagus
from outside:
1. Hypopharyngeal diverticulum (see page 290).
2. Hiatus hernia.
3. Cervical osteophytes.
4. Thyroid lesions, e.g. enlargement, tumours, Hashimoto's thyroiditis.
5. Mediastinal lesions, e.g. tumours of mediastinum, lymph node
enlargement, aortic aneurysm, cardiac enlargement.
6. Vascular rings (dysphagia lusoria).
b) INVESTIGATION
1. Barium meal
2. X-ray neck Lateral view
3. Gastro-esophageal endoscopy
4. CT-scan
c) TREATMENT
1. Radiotherapy upper two third
2. Surgery lower two third
3. Bypass operation
4. Esophageal intubation
5. Permanent gastrostomy
6. Laser surgery using ND YAG laser
Q-5. A 60 years old man chronic smoker was diagnosed with carcinoma of right Vocal cord,
with sluggish movements and an ipsilateral 2 cm lymph node in the neck.
a) write at least three predisposing factors of carcinoma larynx.
b) how do you stage this patient according to TNM staging system?
c) name three specific investigations for carcinoma.
d) name different treatment options glottis carcinoma.
ANS:
a) PREDISPOSING FACTORS FOR CARCINOMA LARYNX
1. Smoking
2. Alcohol
3. Previous radiation
4. Genetic factors
KMU Past Papers Solved SEQs
Oral cavity Pharynx Larynx and Esophagus 48
5. Asbestos and mustard gas exposure
6. Petroleum products
b) STAGE
Stage-3
c) INVESTIGATION:
1. Indirect laryngioscopy
2. Flexible fibroptic or rigid laryngioscopy or video laryngioscopy
3. Radiography CT, X ray, MRI
4. Direct laryengeoscopy
5. Microlaryngeoscopy
6. Supravital staining (toluidine blue) and biopsy
d) TREATMENT OPTION
1. Surgery
i) Cordectomy via laryengiofissure
ii) Partial frontolateral laryngectomy
iii) Partial horizontal laryngectomy
iv) Complete laryngectomy
v) Laryngectomy with neck dissection
2. Radiotherapy
3. Combine surgery with pre and postoperative radiation
4. Endoscopic CO2 laser resection
5. Organ preservation: chemotherapy followed by radiotherapy
Q-6. A 37 years old man presented to the ENT clinic with 3-month history of intermittent
swelling beneath the left lower jaw. The swelling increases in size and becomes painful
during eating specially of citrus food. Examination of the anterior floor of mouth shows
that there is a prominent collection of debris (cheesy type) just on the left side of the
frenulum linguae. The surrounding area was also congested for few millimeters around.
a) What is your clinical diagnosis?
b) Why is this lesion more common at this site?
c) What type of radiograph would you request to get information about this
condition?
d) How will you treat this patient?
e) What will the possible complications of this condition?
ANS:
a) DIAGNOSIS
Stone in submandibular duct
b) REASON
The submandibular duct is more horizontal
Flow of saliva is comparatively slow
KMU Past Papers Solved SEQs
Oral cavity Pharynx Larynx and Esophagus 49
c) RADIOGRAPH
Occlusal view
d) TREATMENT
Stones in peripheral part of submandibular or parotid ducts can be removed intraorally,
while those at the hilum or in the parenchyma require excision of the gland.
e) COMPLICATION
Recurrent Sialadenitis
Q-7. A 65years old lady presented with progressive dysphagia for the last 6 months. On
examination patient was thin emaciated with pooling of saliva in pyriform sinuses and
absent laryngeal crepitus.
a) What is the most likely diagnosis?
b) What investigations would your advice in this case?
c) What premalignant lesion can lead to this condition?
ANS:
a) DIAGNOSIS
Post cricoid carcinoma of the esophagus
b) INVESTIGATIONS
1. Lateral soft tissue X ray
2. Barium swallow
3. Endoscopy
4. Biopsy
c) PREMALIGNANT LESION:
Plummer vinson symdrome
Q-8. A 6 months old child was referred from pediatric department to ENT clinic for the
management of breathing difficulty. Breathing was coarse when the child was lying in
supine position and during crying. He was comparatively relieved when lying in a prone
position. The cry of the child was essentially normal. Also there were no signs of
respiratory infection.
a) What is the most likely diagnosis?
b) Name three possible causes of laryngeal stridor at this stage?
c) How will you confirm the diagnosis?
d) What will be the management of this patient?
ANS:
a) DIAGNOSIS:
Laryngomalacia
b) CAUSES OF STRIDOR
KMU Past Papers Solved SEQs
Oral cavity Pharynx Larynx and Esophagus 50
1. Laryngomalacia
2. Laryngeal web
3. Subglottic stenosis
4. Haemangioma
5. Vocal cord paralysis
6. Tongue and jaw abnormalities
c) INVESTIGATIONS
1. Direct laryngeoscopy shows omega sign
2. flexible laryngeoscopy
d) MANAGEMENT:
1. Mostly become normal with increasing age
2. tracheostomy
3. supraglottoplasty
Q-9. A 65 years old man presented with two years of history of gradually worsening
dysphagia. He described food sticking in the throat and episodic of regurgitation of
undigested food stuff which especially at night leads to choking and severe bout of
coughing. He is otherwise fit and well had been admitted to hospital with an episode of
pneumonia six month prior to his attendance to ENT clinic He chews the food very fine
while swallowing. The dysphagia increases as he continues eating thus he avoids to go to
parties with friends. He sometimes gets swelling in the left side of the neck which on
pressing gives rise to gurgling sound.
a) what is the probable clinical diagnosis?
b) How does such a lesion cause dysphagia?
c) Name two imaging investigations in order to reach the diagnosis?
d) What treatment options are available for this condition?
e) What is the potential long term complication?
ANS:
a) DIAGNOSIS
Zenker’s diverticulum (hypopharyngeal diverticulum)
b) CAUSE OF DYSPHAGIA
Dysphagia appears after a few swallows when the pouch gets filled with the food and
presses on esophagus
c) IMAGING INVESTIGATIONS
1. Lateral view neck radiograph
2. barium swallow
3. CT-scan
d) TREATMENT OPTIONS
1. excision of the pouch and cricopharyngeal myotomy
KMU Past Papers Solved SEQs
Oral cavity Pharynx Larynx and Esophagus 51
2. dohlmann procedure: remove the partition between esophageal wall and puch wall
via diathermy through endoscope
3. endoscopic laser treatment: similar to dohlmaan but partition is made through co2
laser using operating microscope
e) LONG TERM COMPLICATION:
1. Hiatal hernia
2. Carcinoma of the pharyngeal pouch
Q-10. A 15 Years old boy presented to ENT OPD with recurrent epistaxis for the last 6
months. Posterior rhinoscopy revealed a fleshy mass in the nasopharynx.
a) What is your most probable diagnosis?
b) What investigations will you offer which will help you in establishing the diagnosis
and treatment plan?
c) What preoperative measures will you take before embarking on surgery?
d) What surgical approaches can be can be adapted for this patient?
ANS:
a) DIAGNOSIS
Juvenile nasopharyngeal angiofibroma
b) INVESTIGATIONS
1. CT scan (hollman meller sign or antral sign)
2. MRI
3. Carotid angiography
c) PREOPERATIVE MEASURES
1. Arrangement for blood transfusion
2. Preoperative angiography for embolization of feeder arteries (only external carotid
artery)
3. Resection of tumor should not be delayed after 24 to 48 hour due to collateral vessels
formation
4. Estrogen were use before the era of embolization to reduce blood supply
d) SURGICAL APPROACHES:
1. Transpalatal approach
2. Transpalatine plus sublabial (sardana approach)
3. Transmaxillary approach
4. Lateral rhinotomy with medial maxellectomy done through facial incision or
degloving approach
5. Fascial translocation or maxillary swing approach
6. Infratemporal fossa approach
7. Endoscopic approach
8. Extracranal and intracranial approach
KMU Past Papers Solved SEQs
Oral cavity Pharynx Larynx and Esophagus 52
Q-11. A 42 years Old female presented to ENT OPD with history of progressive dysphasia for
solids for last 2 years. On examination she is pale looking and oral cavity examination
shows angular chelitis and smooth looking tongue. On general physical examination the
patient is having koilonychias. The rest of ENT examination was unremarkable. Her HB is
7.4gm/dl
a) What is your diagnosis?
b) Name two differential diagnoses?
c) Name two relevant investigations?
d) How will you treat this patient?
e) What is potential dangerous complication of this disease?
ANS:
a) DIAGNOSIS:
Plummer vinson syndrome
b) DIFFERENTIAL DIAGNOSIS:
1. Post cricoid carcinoma of pharynx
2. Esophageal carcinoma
c) INVESTIGATION
1. Indirect laryngeoscopy
2. Barium swallow
3. Esophagoscopy endoscopy
d) TREATMENT:
1. Treatment of anemia by oral or parental iron, associated B6 and B 12 def should
corrected
2. Esophageal bouges for dialatation
e) COMPLICATION:
Post cricoid carcinoma of pharynx formation
Q-12. A 73 years old male presented to ENT OPD with hoarseness of voice for last 6 months
and breathing difficulty for last one month. He used to smoke at least 20 cigarettes a day
for a long time. On examination the left vocal cord is fixed with an exophytic lesion. Neck is
clear on palpation and the rest of ENT and systemic examination is unremarkable.
a) What is the most probable diagnosis?
b) Name 3 relevant investigations with justification.
c) Write T staging of tumors?
d) What are the different treatment options?
ANS:
a) DIAGNOSIS:
Laryngeal carcinoma
b) INVESTIGATION:
KMU Past Papers Solved SEQs
53
1. Indirect laryngoscopy for appearance of lesion, vocal cord mobility, extent of
disease
2. Flexible fibroptic or rigid laryngoscopy or video laryngoscopy detailed
examination
3. Radiography
CT, extent of tumor
X ray for coexistent metastasis
MRI use full for recurrent cancers
4. Direct laryngoscopy for hidden areas and extent of disease
5. Micro-laryngoscopy make accurate biopsy without damaging vocal cords
6. Supravital staining (toluidine blue) and biopsy differentiate carcinoma insitu
(take dye) from leukoplakia (doesn’t take dye)
c) STAGE 3
d) TREATMENT OPTION
1. Surgery
Cordectomy via laryengiofissure
Partial frontolateral laryngectomy
Partial horizontal laryngectomy
Complete laryngectomy
Laryngectomy with neck dissection
2. Radiation
3. Combine surgery with pre and postoperative radiation
4. Endoscopic Co2 laser resection
5. Organ preservation: chemotherapy followed by radiotherapy
Q-13. A 60 years old lady developed progressive difficulty in swallowing first for solids for
the last three months. For the last two weeks the patient has absolute dysphagia. On
examination there is pooling of saliva in the pyriform sinuses and laryngeal crepitus is
absent. The lady appeared thin emaciated, dehydrated and anemic. Neck is clear.
a) What is the most likely diagnosis?
b) What investigations would you advice? Justify your answer
c) How will you treat her?
ANS:
a) DIAGNOSIS:
Post-cricoid carcinoma
b) INVESTIGATIONS:
1. Indirect laryngoscopy postcricoid growth seen
2. Lateral soft tissue radiograph prevertebral shadow
3. Barium swallow to find the lower extent of disease
4. Endoscopy to take biopsy and find the extent of disease
KMU Past Papers Solved SEQs
Oral cavity Pharynx Larynx and Esophagus 54
a) TREATMENT:
1. Radiotherapy
2. If fail then laryngo-pharyngo-esophagectomy with stomach pull-up of colon
transposition
3. initial surgery gives better result
Q-14. A 30-Year-Old Qari Sahib Developed hoarseness of voice for the last 03 months he has
received 3-4 Courses of antibiotics. There was no cough no pain no fever. Laryngeal
mirror examination is difficult to perform.
a) What is the most likely diagnosis?
b) What is your treatment?
a) Give differential diagnosis of hoarseness of voice?
ANS:
a) DIAGNOSIS:
Vocal cord nodule
b) TREATMENT:
1. Proper use of voice
2. Surgical excision under operating microscope with cold instrument or laser
3. Avoid any trauma to under lying vocal cord ligament
4. Speech therapy to prevent reoccurrence
c) DIFFERENTIAL DIAGNOSIS:
A. non neoplastic lesion
1. Vocal cord nodule
2. Vocal polyp
3. Renkes edema
4. Contact ulcer or granuloma
5. Intubation granuloma
6. Ductal cyst
7. Saccular cyst
8. Ductal cyst
B. Neoplastic lesion:
1. Squamous papilloma
2. Glottis carcinoma
Q-15. A 12 old girl with sore throat. On examination is membrane on tonsils.
a) What are differential diagnosis of membrane tonsil?
b) How will you investigate this case?
ANS:
a) DD’S
KMU Past Papers Solved SEQs
Oral cavity Pharynx Larynx and Esophagus 55
1. Membranous tonsillitis
2. Diphtheria
3. Infectious mononucleosis
4. Agranulocytosis
5. Leukemia
b) INVESTIGATION:
Diagnosis of ulceromembranous lesion of throat thus requires:
1. History.
2. Physical examination.
3. Total and differential counts (for agranulocytosis, leukaemia, neutropenia,
infectious mononucleosis).
4. Blood smear (for atypical cells).
5. Throat swab and culture (for pyogenic bacteria), Vincent's angina, diphtheria
candidal infection.
6. Bone marrow aspiration or needle biopsy.
7. Other tests. Paul-Bunnell or mono spot test and biopsy of the lesion
Q-16. A 60 years old male presented to ENT OPD with swelling right side of the neck at level
II for the last 3 months. It was associated with obstruction, blood stained discharge and
impaired hearing on the same side.
a) what is your most probable diagnosis?
b) How will you to reach to diagnosis List three of them.
c) How wily treat this patient?
ANS:
a) DIAGNOSIS:
Nasopharyngeal carcinoma
b) DIAGNOSIS:
1. Endoscopic evaluation
2. Imaging studies (X ray CT scan, MRI, PET)
3. Biopsy
4. Audiogram
c) TREATMENT:
1. Radiotherapy stage 1 and 2
Through three dimentional conformal radio therapy and intesnsity modulated
radiotherapy IMRT
2. Concomitant Radiotherapy and chemotherapy stage 3 and 4
3. Chemotherapy stage 3 and 4
4. Brachytherapy
5. Nasopharyngeotomy
KMU Past Papers Solved SEQs
Oral cavity Pharynx Larynx and Esophagus 56
Q-17. A 26-Year-Old Male was brought to accident and emergency department with history
of road traffic accident with history of road traffic accident he has perfuse bleeding in the
oropharynx which he is spitting out his tongue is lacerated mandible is fractured. He is
conscious and has no neurological deficit.
a) What surgical procedure will you adopt to secure the airway?
b) What are the other indication of the procedure? Name only 4 of them.
c) Enumerate the complications which can and after the procedure?
d) How will you take care of the patient after the procedure?
ANS:
a) SURGICAL PROCEDURE
Tracheostomy
b) INDICATIONS
A. Respiratory obstruction.
1. Infections
2. Neoplasm
3. Foreign body
B. Retained secretions.
1. Inability to cough
2. Painful cough
3. Paralysis
C. Respiratory insufficiency.
1. Chronic lung diseases
c) COMPLICATION
A. Immediate (at the time of operation):
1. Haemorrhage.
2. Apnoea. This follows opening of trachea in a patient who had prolonged
respiratory obstruction. This is due to sudden washing out of CO, which was acting
as a respiratory stimulus. Treatment is to administer 5% CO, in oxygen or assisted
ventilation.
3. Pneumothorax due to injury to apical pleura.
4. Injury to recurrent laryngeal nerves.
5. Aspiration of blood.
6. Injuiy to oesophagus. This can occur with tip ofknife while incising the trachea and
may result in tracheooesophageal fistula.
B. Intermediate (during first few hours or days):
1. Bleeding, reactionary or secondary.
2. Displacement of tube.
3. Blocking of tube.
4. Subcutaneous emphysema.
5. Tracheitis and tracheobronchitis with crusting in trachea.
6. Atelectasis and lung abscess.
KMU Past Papers Solved SEQs
Oral cavity Pharynx Larynx and Esophagus 57
7. Local wound infection and granulations.
C. Late (with prolonged use of tube for weeks and months):
1. Haemorrhage, due to erosion of major vessel.
2. Laryngeal stenosis, due to perichondritis of cricoid cartilage.
3. Tracheal stenosis, due to tracheal ulceration and infection.
4. Tracheo-oesophageal fistula, due to prolonged use of cuffed tube or erosion of
trachea by the tip of tracheostomy tube.
5. Problems of decannulation. Seen commonly in infants and children. (>. Persistent
tracheocutaneous fistula.
6. Problems of tracheostomy scar. Keloid or unsightly scar. 8. Corrosion of
tracheostomy tube and aspiration of its fragments into the tracheobronchial tree.
d) CARE AFTER PROCEDURE
1. Constant supervision. for bleeding, displacement or blocking of tube and removal of
secretions is essential.
2. Suction. Depending on the amount of secretion, suction may be required every half an
hour or so;
3. Prevention of crusting and tracheitis. By (a) Proper humidification of air (b) If
crusting occurs, a few drops of normal or hypotonic saline or Ringer's lactate are
instilled into the trachea A mucolytic agent such as acetylcysteine solution, can be
instilled to liquify tenacious secretions or to loosen the crusts.
4. Care of tracheostomy tube.
Q-18. A 17 years old boy underwent tonsillectomy operation started bleeding in ward.
Doctor examined the patient in afternoon. On examination there was blood in his throat
and clot in left tonsillar fossa. The patient was tachycardia and having low volume pulse.
a) What is the diagnosis
b) What are the causes of his bleeding?
c) How will you manage the patient?
ANS:
a) DIAGNOSIS:
Reactionary hemorrhage
b) CAUSES:
Poor ligation of vessels and trauma due to sneezing or coughing
c) MANAGEMENT:
1. Removal of the clot, application of pressure or vasoconstrictor.
2. Presence of a clot prevents the clipping action of the superior constrictor muscle on
the vessels which
3. Pass through it
4. If above measures fail, ligation or electrocoagulation of the bleeding vessels can be
done under general anesthesia
KMU Past Papers Solved SEQs
58
General measures:
1. Blood transfusion in case of shock
Q-19. A 60 years old man from china presented to ENT OPD with right side neck swelling
and right side nasal obstruction and ear blockage of 3-month duration. On examination
there is mass in nasopharynx right side and dull right tympanic membrane. Neck
examination shows enlarged lymph node in posterior triangle on right side. On tuning fork
tests, weber was lateralized to right side
a) What is your diagnosis
b) Name the investigations with justifications to reach the diagnosis
c) How will you treat the patient?
ANS:
a) DIAGNOSIS:
Nasopharyngeal carcinoma
b) INVESTIGATION:
1. Endoscopic evaluation for growth, proliferation nature and for biopsy
2. Imaging studies
X ray for secondary involvement of lungs
CT scan for extent of invasion of tumor
MRI better for soft tissue extension
PET for distant metastasis
3. Biopsy for histological nature
4. Audiogram for diagnosis of serous otitis media
c) TREATMENT:
1. Radiotherapy stage 1 and 2
Through three dimentional conformal radio therapy and intesnsity modulated
radiotherapy IMRT
2. Concomitant Radiotherapy and chemotherapy stage 3 and 4
3. Chemotherapy stage 3 and 4
4. Brachytherapy
5. Nasopharyngeotomy
KMU Past Papers Solved SEQs
Oral cavity Pharynx Larynx and Esophagus 59
Q-20. A 3 years old child was brought to ENT OPD by his mother with swelling in the midline
of the neck for the last one year. It is freely mobile from side to side and rises on
swallowing and protrusion of the tongue.
a) What is the most probable diagnosis?
b) what investigations will you carry out in this case
c) how will you treat the case?
d) What complication can occur if not treated?
e) Write two differential diagnosis of the condition
ANS:
a) DIAGNOSIS:
Thyroglossal cyst
b) INVESTIGATIONS:
1. Cyst aspiration
2. Ultrasound
3. CT scan
4. MRI
5. FNAC
c) TREATMENT
1. Simple excision
2. Sistrunk’s operation: excision of body of hyoid bone, core of tongue, tissue around the
tract in the supra hyoid tongue base to foramen caecum
d) COMPLICATION:
Rarely carcinoma develop in the cyst
e) DDS
1. Sub lingual dermoid cyst
2. Ludwigs angina
3. Plunging ranula
Q-21. A 5 years old boy was referred to an ENT specialist with history of nasal obstruction
for the last one year. The mother reported that her child snores during sleep and has
repeated upper respiratory tract infection. On examination he was having open mouth
and nasal patency was reduced
a) What is the most probable diagnosis?
b) How will you investigate the child?
c) How will you treat the patient?
d) What are the steps of operation for the above pathology?
ANS:
a) DIAGNOSIS:
Adenoid hyperplasia
KMU Past Papers Solved SEQs
Oral cavity Pharynx Larynx and Esophagus 60
b) INVESTIGATION:
1. Posterior rhinoscopy and the adenoids will be hypertrophied
2. Rigid or flexible nasopharyngoscope can be used in cooperative child
3. X ray Lateral view of pharynx
c) TREATMENT
A. For mild symptoms:
1. Breathing exercise
2. Nasal decongestant
3. Antihistamines
B. For sever symptoms adenoidectomy is done
d) STEPS:
1. Boyle davis mouth gag is inserted
2. Proper size adenoid curette is with guard in introduced into nasopharynx
3. Adenoids are shaved through this curette by sweeping movement
4. Pack the area
5. Electrocoagulation
6. Posterior nasal pack for 24 hours
Q-22. A 15 years old boy presented to ENT OPD with recurrent epistaxis for the last 6
months, progressive nasal obstruction, posterior phonoscope revealed a fleshy mass, X-
rays shows anterior bowing of the posterior maxillary wall,
a) What is you most probable diagnosis?
b) How will you. investigate this boy?
c) What preoperative measures will you take before embarking on surgery?
d) What surgical procedure can be adapted for this patient?
ANS:
a) DIAGNOSIS
Juvenile nasopharyngeal angiofibroma
b) INVESTIGATIONS
1. CT scan (hollman meller sign or antral sign)
2. MRI
3. Carotid angiography
c) PREOPERATIVE MEASURES
1. Arrangement for blood transfusion
2. Preoperative angiography for embolization of feeder arteries (only external carotid
artery)
3. Resection of tumor should not be delayed after 24 to 48 hour due to collateral vessels
formation
4. Estrogen were use before the era of embolization to reduce blood supply
d) SURGICAL APPROACHES:
KMU Past Papers Solved SEQs
Oral cavity Pharynx Larynx and Esophagus 61
1. Transpalatal approach
2. Transpalatine plus sublabial (sardana approach)
3. Transmaxillary approach
4. Lateral rhinotomy with medial maxellectomy done through facial incision or
degloving approach
5. Fascial translocation or maxillary swing approach
6. Infratemporal fossa approach
7. Endoscopic approach
8. Extracranal and intracranial approach
Q-23. A 45 years old female presented with Dysphagia for the last 2 months without the
history of foreign body impaction.
a) What question will you ask to differentiate between paralytic and obstructive
dysphagia?
b) What is the importance of laryngeal crepitus and X ray neck lateral view in a
patient with dysphagia?
ANS:
a) QUESTIONS REGARDING DYSPHAGIA:
1. Onset (foreign body or impaction of food on a preexisting stricture or malignancy,
neurological disorders),
2. Progressive (malignancy),
3. Intermittent (spasms or spasmodic episodes over an organic lesion),
4. More to liquids (paralytic lesions),
5. More to solids and progressing even to liquids (malignancy or stricture),
6. Intolerance to acid food or fruit juices (ulcerative lesions).
b) IMPORTANCE OF
Laryngeal crepitus: laryngeal crepitus is lost in most of laryngeal carcinoma.
X-ray
1. X-ray chest: To exclude cardiovascular, pulmonary and mediastinal diseases.
2. Lateral view neck: To exclude cervical osteophytes and any soft tissue lesions of
post-cricoid or retropharyngeal space.
Q-24. A 25 years old female presented to ENT ward with inflammation in the floor of the
mouth and respiratory distress. She gives history of tooth extraction one week
a) What is your provisional diagnosis?
b) How you divide sub mandibular space?
c) How will you treat this patient?
ANS:
KMU Past Papers Solved SEQs
Oral cavity Pharynx Larynx and Esophagus 62
a) DIAGNOSIS:
Ludwig angina (submandibular space abscess)
b) SUBMANDIBULAR SPACE DIVISION:
1. Sublingual compartment above the mylohyoid)
2. Submaxillary and submental compartment below the mylohyoid).
c) TREATMENT:
1. Systemic antibiotics.
2. Incision and drainage of abscess.
i) Intraoral if infection is still localised to sublingual space.
ii) External if infection involves submaxillary space. A transverse incision
extending from one angle of mandible to the other is made with vertical
opening of midline musculature of tongue with a blunt haemostat. Very
often it is serous fluid rather than frank pus that is encountered.
3. Tracheostomy, if airway is endangered.
Q-25. A 28 years old male patient came with the complaint that three days back during lunch
a sharp fish bone got penetrated into the posterior wall of his throat which was then
removed by an ENT doctor. After 4 days the patient developed severe pain in the throat
along with difficulty in swallowing. Fever and difficulty in opening his mouth, throat
examination showed a smooth bulge in the posterior pharyngeal wall. Tonsils, tonsillar
pillars and soft palate were normal.
a) What is the most probable diagnosis in this case?
b) How will you investigate this case?
c) How will you treat this case?
ANS:
a) DIAGNOSIS:
Retropharyngeal abscess
b) INVESTIGATION
Radiograph of soft tissue lateral view of the neck shows widening of prevertebral
shadow and possibly even the presence of gas
c) TREATMENT:
1. Incision and drainage of abscess. This is usually done without anesthesia as there
is risk of rupture of abscess during intubation.
2. Child is kept supine with head low. Mouth is opened with a gag. A vertical incision
is given in the most fluctuant area of the abscess. Suction should always be
available to prevent aspiration of pus.
3. Systemic antibiotics. Suitable antibiotics are given.
4. Tracheostomy. A large abscess may cause mechanical obstruction to the airway or
lead to laryngeal edema. Tracheostomy becomes mandatory in these cases
KMU Past Papers Solved SEQs
Oral cavity Pharynx Larynx and Esophagus 63
Q-26. A father brought his 4-year-old child in emergency with the complaint that his child
was unable to swallow any food or liquid for last 8 hours. There is no history of
breathlessness or cyanosis. Examination of throat showed pooling of saliva and there was
no positive finding on auscultation of the chest.
a) What is most probable diagnosis?
b) How will you confirm the diagnosis?
c) How will you manage this case?
d) What complications can occur during management of this patient?
ANS:
a) DIAGNOSIS:
Acute epiglottitis
b) INVESTIGATION:
Thumb sign on lateral view Xray (swollen epiglottis)
c) TREATMENT
1. Hospitalization
2. Antibiotic ampicillin or third gen cephalosporins iv
3. Steroids hydrocortisone
4. Adequate hydration
5. Humidification and oxygen
6. Intubation or tracheostomy
d) COMPLICATIONS:
1. During examination:
Indirect laryngoscopy is avoided for the fear of precipitating complete obstruction
It should be done in OT where intubation facilities are available
2. Complication due to intubation and tracheostomy
Q-27. A 4-year-old female child brought to ENT OPD with marked difficulty in swallowing
drooling of saliva of 48-hour duration followed by severe respiratory distress. On
examination she was very toxic having temperature of 102 f with a flexed neck.
Oropharyngeal examination showed a congested large swelling on right side of posterior
pharyngeal wall.
a) What is the most probable diagnosis?
b) Write two differential diagnosis?
c) Name at least three potential space of the neck
d) How will you treat this child?
ANS:
a) DIAGNOSIS:
Retropharyngeal abscess
b) DD’S
KMU Past Papers Solved SEQs
Oral cavity Pharynx Larynx and Esophagus 64
Abscess in
1. Parapharyngeal,
2. Retropharyngeal,
c) POTENTIAL SPACES IN NECK
1. Parapharyngeal,
2. Retropharyngeal,
3. Perivertebral,
d) TREATMENT:
1. Incision and drainage of abscess. This is usually done without anesthesia as there
is risk of rupture of abscess Retropharyngeal abscess.
during intubation. Child is kept supine with head low. Mouth is opened with a gag.
A vertical incision is given in the most fluctuant area of the abscess. Suction should
always be available to prevent aspiration of pus.
2. Systemic antibiotics. Suitable antibiotics are given.
3. Tracheostomy. A large abscess may cause mechanical obstruction to the airway or
lead to laryngeal edema.
Q-28. A 55 years old gentle man presented with Hoarseness of voice for the last 3 months. On
indirect Laryngoscopy there is a mass on the right vocal card which extends supra-glottically.
The right larynx is fixed.
a) What is your diagnosis?
b) How will you confirm you diagnosis?
c) What is T3 lesion of vocal cord?
d) Write in there lines the ideal treatment of this patient.
e) How you will rehabilitative voice of this patient after giving treatment.
ANS
a) DIAGNOSIS:
Carcinoma Larynx
b) INVESTIGATIONS:
1. Indirect laryngoscopy for;
i) Appearance of lesion.
ii) Vocal cord mobility.
iii) Extent of disease.
2. Radiography
i) X-ray Soft tissue lateral view neck.
ii) X-ray chest is essential for co-existent lung disease (e.g. tuberculosis), pulmonary
metastasis or mediastinal nodes.
3. Contrast laryngograms. Radio-opaque dye, dionosil, is instilled into the larynx.
Laryngograms outline the surface extent of tumours.
4. CT scan. It is a very useful investigation to find the extent of tumour,
KMU Past Papers Solved SEQs
Oral cavity Pharynx Larynx and Esophagus 65
5. Direct laryngoscopy It is done to see
i) the hidden areas of larynx
ii) extent of disease
6. Microlaryngoscopy for small lesions of vocal cords, laryngoscopy is done under
microscope to better visualise the lesion and take more accurate biopsy specimens
without damaging the cord.
7. Supravital staining and biopsy Toluidine blue is applied to the laryngeal lesion and then
washed with saline and examined under the operating microscope. Carcinomain-situ and
superficial carcinomas take up the dye while leukoplakia does not. Thus, it helps to select
the area for biopsy in a leukoplakic patch.
c) T3 LESION OF VOCAL CORD:
Tumour limited to larynx with vocal cord fixation and/or invades any of the following:
postcricoid area, pre-epiglottic tissues, paraglottic space and/or minor thyroid cartilage
invasion
d) TREATMENT:
e) REHABILITATION:
Voice rehabilitation through
1. Oesophageal speech,
2. Artificial larynx,
3. Tracheo-esophageal speech
Q-29. A 30 years old female presented with fever, severe sore throat and odynophagia for
the last 2 days On examination patient is unable to open her mouth and the left tonsil is
swollen and is pushed medially. Jugulodigastric lymph nodes on the same side are also
enlarged.
a) What is your most probable diagnosis?
b) What complications can arise if this condition is not treated in time? Name any two.
c) What is the cause for trismus in this patient?
d) Name 3 surgical options for treating such conditions.
ANS:
a) DIAGNOSIS:
Peritonsillar abscess
b) COMPLICATION
1. Parapharyngeal abscess (a peritonsillar abscess is a potential parapharyngeal
abscess).
2. Oedema of larynx. Tracheostomy may be required.
3. Septicaemia.
4. Other complications like endocarditis, nephritis, brain abscess may occur.
KMU Past Papers Solved SEQs
Oral cavity Pharynx Larynx and Esophagus 66
5. Pneumonitis or lung abscess. Due to aspiration of pus, if spontaneous rupture of
abscess has taken place.
6. Jugular vein thrombosis.
7. Spontaneous haemorrhage from carotid artery or jugular vein.
c) CAUSES OF TRISMUSS
Due to pterygoid muscles inflammation.
d) SURGICAL PROCEDURES
1. Incision and drainage of abscess: With the help of a guarded knife, a small stab
incision is made and then a sinus forceps inserted to open the abscess.
2. Interval tonsillectomy Tonsils are removed four to six weeks following an attack of
quinsy.
3. Abscess or hot tonsillectomy Some people prefer to do 'hot' tonsillectomy instead of
incision and drainage.
Q-30. A four years old boy presented to ENT OPD with history of nasal obstruction and
snoring at night for the last 6 months. There is no history of trauma. Nasal examinations
revealed no anatomical abnormalities.
a) What is your most probable diagnosis?
b) What single investigation would you advised to confirm the diagnosis and what
will be the findings?
c) How do you treat this patient?
ANS:
a) ADENOID HYPERPLASIA
b) INVESTIGATION:
Posterior rhinoscopy and the adenoids will be hypertrophied
Rigid or flexible nasopharyngoscope can be used in cooperative child
X ray Lateral view of pharynx
c) TREATMENT
For mild symptoms:
1. Breathing exercise
2. Nasal decongestant
3. Antihistamines
For sever symptoms adenoidectomy is done
KMU Past Papers Solved SEQs
You might also like
- Epistaxis (Nose Bleed), A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandEpistaxis (Nose Bleed), A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- ENT Past Years CompilationDocument7 pagesENT Past Years CompilationYee Wei HoongNo ratings yet
- An Evidence-Based Approach to the Management of Nasopharyngeal Cancer: From Basic Science to Clinical Presentation and TreatmentFrom EverandAn Evidence-Based Approach to the Management of Nasopharyngeal Cancer: From Basic Science to Clinical Presentation and TreatmentBaharudin AbdullahNo ratings yet
- 1st Term ENTDocument9 pages1st Term ENThassan qureshi0% (1)
- Ent MCQDocument2 pagesEnt MCQtariq_siddiqui_11100% (1)
- ENT MCQforstudents AnswersDocument30 pagesENT MCQforstudents AnswersOlaNo ratings yet
- ENT MCQsDocument13 pagesENT MCQsSheikha100% (2)
- Ent ExaminationDocument9 pagesEnt ExaminationSheikha100% (2)
- Ent Bcqs 3Document18 pagesEnt Bcqs 3Ghazi Uddin Ahmed0% (1)
- Chapter 64Document20 pagesChapter 64Prince K. TaileyNo ratings yet
- MCQs EntDocument10 pagesMCQs EntMarrium Habib100% (3)
- MCQZDocument55 pagesMCQZyasinoNo ratings yet
- (ENT-OPT-FRS) End-Posting Examination Questions (G5) - 20180208 - 175513Document23 pages(ENT-OPT-FRS) End-Posting Examination Questions (G5) - 20180208 - 175513Steph StephanieNo ratings yet
- EennttDocument13 pagesEennttSuresh Kumar BansalNo ratings yet
- MCQ ENT 2Document3 pagesMCQ ENT 2api-26186766100% (1)
- EntDocument128 pagesEntNaila Omer100% (1)
- A. It Consists of Squamous EpitheliumDocument7 pagesA. It Consists of Squamous EpitheliumUzair KhanNo ratings yet
- ENT McqsDocument15 pagesENT McqsVitorLópezNo ratings yet
- Multiple Choices Questions For ENT ResidentsDocument5 pagesMultiple Choices Questions For ENT Residentsadham bani younesNo ratings yet
- MCQ Bank: Mcqs by TopicDocument136 pagesMCQ Bank: Mcqs by TopicHadzrie HamdanNo ratings yet
- Ent Mcqs 3Document8 pagesEnt Mcqs 3Uzair KhanNo ratings yet
- MCQ EntDocument5 pagesMCQ EntShashi LimbachiyaNo ratings yet
- Otology Ent McqsDocument134 pagesOtology Ent McqsAbouzr Mohammed ElsaidNo ratings yet
- ENT Paper 2Document13 pagesENT Paper 2John M. Hemsworth100% (1)
- ENT End-of-Posting Questions (30 Sep'05)Document6 pagesENT End-of-Posting Questions (30 Sep'05)John M. HemsworthNo ratings yet
- 3 RfajDocument81 pages3 RfajSheikhaNo ratings yet
- MCQ ENT. DR NemerDocument7 pagesMCQ ENT. DR Nemeradham bani younesNo ratings yet
- 5) EntDocument16 pages5) EntZH. omg sarNo ratings yet
- امتحان ENT دفعة ٣١Document14 pagesامتحان ENT دفعة ٣١محمد عبد القاهر السروريNo ratings yet
- MCQS New 60 EntDocument10 pagesMCQS New 60 Entzoyaa4512100% (1)
- Ent Mcqs 4Document7 pagesEnt Mcqs 4Uzair KhanNo ratings yet
- ENT Practice MCQs With Key 4th Year MBBSDocument7 pagesENT Practice MCQs With Key 4th Year MBBSPatrick BatemanNo ratings yet
- Questions&Answers: Meniere's Disease PresentationDocument55 pagesQuestions&Answers: Meniere's Disease Presentationimran qazi100% (1)
- ENT MCQs Eiad NahlaDocument11 pagesENT MCQs Eiad Nahlaadham bani younesNo ratings yet
- Ent NotesDocument3 pagesEnt Notesapi-26186766No ratings yet
- Ent Imp Points To Diagnose ScenariosDocument46 pagesEnt Imp Points To Diagnose Scenariosusmandumassar0% (1)
- ENTDocument2 pagesENTNikita Nanwani0% (1)
- ENT MCQs Basic 13Qs.Document5 pagesENT MCQs Basic 13Qs.adham bani younesNo ratings yet
- MCQ Ent ThroatDocument16 pagesMCQ Ent ThroatDr-Firas Nayf Al-ThawabiaNo ratings yet
- ENT Best Answer Select The One Best Answer:-: Omdurman Islamic University Medical Students AssociationDocument22 pagesENT Best Answer Select The One Best Answer:-: Omdurman Islamic University Medical Students AssociationAbd AlsalihiNo ratings yet
- ENT QuestionsDocument6 pagesENT QuestionsJohn M. HemsworthNo ratings yet
- Aiims Adr Plexus EntDocument32 pagesAiims Adr Plexus Entkishorechandra75% (4)
- MRCS ENT Content Guide FINAL Jan 22Document18 pagesMRCS ENT Content Guide FINAL Jan 22monirul islam shohanNo ratings yet
- Clinical Medicine-ENT Self-Assessment: D. Laryngitis Often Lasts A Month or MoreDocument7 pagesClinical Medicine-ENT Self-Assessment: D. Laryngitis Often Lasts A Month or MoretaraNo ratings yet
- ENT MCQ (Not Answered)Document75 pagesENT MCQ (Not Answered)mohamed mowafeyNo ratings yet
- Wa0000Document16 pagesWa0000hassan qureshi100% (1)
- Davinci Medical AcademyDocument9 pagesDavinci Medical AcademyskNo ratings yet
- OtologiDocument13 pagesOtologimr_curiousityNo ratings yet
- MCQ in Orl CourseDocument46 pagesMCQ in Orl CoursesulnaikNo ratings yet
- 1-The Eustachian Tube Is Opened by Contraction ofDocument10 pages1-The Eustachian Tube Is Opened by Contraction ofNofouz MaswadaNo ratings yet
- Otolaryngology Mcqs & SBAs 2nd EditionDocument6 pagesOtolaryngology Mcqs & SBAs 2nd EditionJohn M. Hemsworth100% (1)
- E.N.T-Otorhinolaryngology Instructions: Read Each Question Carefully and Then Select The Single Best Answer Part I: Otology/EarDocument3 pagesE.N.T-Otorhinolaryngology Instructions: Read Each Question Carefully and Then Select The Single Best Answer Part I: Otology/EarJohn M. Hemsworth100% (1)
- Osce - Nose & PnsDocument19 pagesOsce - Nose & Pnsaakash maanNo ratings yet
- ENTDocument8 pagesENTapi-19863548No ratings yet
- Bailey CH 7 1 - 20Document42 pagesBailey CH 7 1 - 20rama mandelaNo ratings yet
- I Am Sharing '100-mcq-complete-ENT' With YouDocument31 pagesI Am Sharing '100-mcq-complete-ENT' With Youhassan qureshi100% (1)
- Ent 25 ExamDocument8 pagesEnt 25 ExamAbd AlsalihiNo ratings yet
- Chhabhadiya Laxman (Ent)Document7 pagesChhabhadiya Laxman (Ent)Venkatesh GarikapatiNo ratings yet
- Diagnosis of Ent Disorders You Make The CallDocument137 pagesDiagnosis of Ent Disorders You Make The Callsaifsaffa2No ratings yet
- Name: Bhanderi Akashkumar H. Clinical Clerk BCCM. ROTATION: OCT. 11-20, 2020Document7 pagesName: Bhanderi Akashkumar H. Clinical Clerk BCCM. ROTATION: OCT. 11-20, 2020Venkatesh GarikapatiNo ratings yet
- PathoDocument1 pagePathoAamir KhanNo ratings yet
- Special Pathology PointsDocument1 pageSpecial Pathology PointsAamir KhanNo ratings yet
- Community Medicine Solved KMU SEQs by RMC StudentsDocument106 pagesCommunity Medicine Solved KMU SEQs by RMC StudentsAamir Khan67% (3)
- Special Pathology Solved KMU SEQs by RMC StudentsDocument145 pagesSpecial Pathology Solved KMU SEQs by RMC StudentsAamir Khan0% (1)
- 6th Central Pay Commission Salary CalculatorDocument15 pages6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- Pharmacology Mnemonics Collection For Medical StudentsDocument21 pagesPharmacology Mnemonics Collection For Medical StudentsAamir KhanNo ratings yet
- Organophosphorus Compounds by Medical Study CenterDocument9 pagesOrganophosphorus Compounds by Medical Study CenterAamir KhanNo ratings yet
- Antibiotics Spectrum Pharmacology by Medical Study CenterDocument5 pagesAntibiotics Spectrum Pharmacology by Medical Study CenterAamir KhanNo ratings yet
- 6th Central Pay Commission Salary CalculatorDocument15 pages6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- Alcohol Poisoning by Medical Study CenterDocument5 pagesAlcohol Poisoning by Medical Study CenterAamir KhanNo ratings yet
- Montessori Vs WaldorfDocument4 pagesMontessori Vs WaldorfAbarnaNo ratings yet
- Abbott 2021 ApJL 915 L5Document24 pagesAbbott 2021 ApJL 915 L5Manju SanthakumariNo ratings yet
- Attitude of Tribal and Non Tribal Students Towards ModernizationDocument9 pagesAttitude of Tribal and Non Tribal Students Towards ModernizationAnonymous CwJeBCAXpNo ratings yet
- Development and Growth of Teeth: Dr. Madhusudhan ReddyDocument48 pagesDevelopment and Growth of Teeth: Dr. Madhusudhan ReddysiyaNo ratings yet
- 1941 Iraq and The IlluminatiDocument4 pages1941 Iraq and The IlluminatiZaneWeltonNo ratings yet
- Laminar Premixed Flames 6Document78 pagesLaminar Premixed Flames 6rcarpiooNo ratings yet
- Manual ML 1675 PDFDocument70 pagesManual ML 1675 PDFSergio de BedoutNo ratings yet
- Film Interpretation and Reference RadiographsDocument7 pagesFilm Interpretation and Reference RadiographsEnrique Tavira67% (3)
- Project 2 Analysis of Florida WaterDocument8 pagesProject 2 Analysis of Florida WaterBeau Beauchamp100% (1)
- ZEROPAY WhitepaperDocument15 pagesZEROPAY WhitepaperIlham NurrohimNo ratings yet
- Microcontrollers DSPs S10Document16 pagesMicrocontrollers DSPs S10Suom YnonaNo ratings yet
- Tablet Time - Student GuideDocument5 pagesTablet Time - Student GuideAyesha BaigNo ratings yet
- Important Instructions For Winter-2020 MCQ Based Online ExaminationDocument1 pageImportant Instructions For Winter-2020 MCQ Based Online Examinationdenoh32751No ratings yet
- Prevention of Power Theft Using Concept of Multifunction Meter and PLCDocument6 pagesPrevention of Power Theft Using Concept of Multifunction Meter and PLCMuhammad FarhanNo ratings yet
- Hydraulics Sheet 5 Energy ADocument19 pagesHydraulics Sheet 5 Energy AMohamed H AliNo ratings yet
- Method Statement For Construction of Concrete Batching Plant (Combined)Document72 pagesMethod Statement For Construction of Concrete Batching Plant (Combined)NP Dien100% (1)
- Vehicles 6-Speed PowerShift Transmission DPS6 DescriptionDocument3 pagesVehicles 6-Speed PowerShift Transmission DPS6 DescriptionCarlos SerapioNo ratings yet
- Water Works RTADocument15 pagesWater Works RTAalfaza3No ratings yet
- Family Planning MethodsDocument20 pagesFamily Planning MethodsRoel Marcial100% (2)
- Chapter 4 PDFDocument26 pagesChapter 4 PDFMeloy ApiladoNo ratings yet
- P&CDocument18 pagesP&Cmailrgn2176No ratings yet
- Sullivan's Interpersonal TheoryDocument27 pagesSullivan's Interpersonal TheoryJezalen GonestoNo ratings yet
- TextdocumentDocument254 pagesTextdocumentSaurabh SihagNo ratings yet
- Forlong - Rivers of LifeDocument618 pagesForlong - Rivers of LifeCelephaïs Press / Unspeakable Press (Leng)100% (15)
- BIR REliefDocument32 pagesBIR REliefJayRellvic Guy-ab67% (6)
- Amazon VS WalmartDocument5 pagesAmazon VS WalmartBrandy M. Twilley100% (1)
- Reaction Paper GattacaDocument1 pageReaction Paper GattacaJoasan PutongNo ratings yet
- Unwrapping The StandardsDocument2 pagesUnwrapping The Standardsapi-254299227100% (1)
- Quiz EditedDocument6 pagesQuiz EditedAbigail LeronNo ratings yet
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (80)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (1)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (26)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (404)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (3)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (44)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Gut: the new and revised Sunday Times bestsellerFrom EverandGut: the new and revised Sunday Times bestsellerRating: 4 out of 5 stars4/5 (392)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- The Marshmallow Test: Mastering Self-ControlFrom EverandThe Marshmallow Test: Mastering Self-ControlRating: 4.5 out of 5 stars4.5/5 (58)
- Dark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingFrom EverandDark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingRating: 4 out of 5 stars4/5 (1138)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningFrom EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningRating: 4 out of 5 stars4/5 (3)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- A Brief History of Intelligence: Evolution, AI, and the Five Breakthroughs That Made Our BrainsFrom EverandA Brief History of Intelligence: Evolution, AI, and the Five Breakthroughs That Made Our BrainsRating: 4.5 out of 5 stars4.5/5 (6)