Professional Documents
Culture Documents
Improper Reduction and Fixation of Bilateral Anterior
Uploaded by
ikeuchi_ogawaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Improper Reduction and Fixation of Bilateral Anterior
Uploaded by
ikeuchi_ogawaCopyright:
Available Formats
Oral Maxillofac Surg (2009) 13:177–179
DOI 10.1007/s10006-009-0162-8
CASE REPORT
Improper reduction and fixation of bilateral anterior
mandibular fractures: a case report
Nakul Uppal & Mohan Baliga & Arvind Ramanathan
Published online: 28 July 2009
# Springer-Verlag 2009
Abstract mandible due to the torsion moments present anteriorly
Introduction Biomechanical principles for osteosynthesis [3, 4]. We present an unusual case of failure of mandibular
are emphasized upon in oral and maxillofacial surgery parasymphysis fracture treatment—caused by violation of
residency programs. several principles of treatment.
Discussion Our case was referred from another specialty
which had treated the patient for bilateral fractures of the
anterior mandible. The gross malunion and other findings Report of a case
in this reported case serve to remind students and surgeons
alike that principles of fracture reduction and fixation must A 12-year-old female was referred to our oral and maxillo-
be respected. facial service bearing a postoperative discharge note that
simply stated “malunion”. History elicited from the parents
Keywords Parasymphysis fracture . Inadequate fixation . revealed that the child sustained injury to the lower jaw in a
Miniplate . Osteosynthesis . Muscle pull . Torsion . road traffic accident 8 weeks earlier. She was then treated at a
Malunion . Open bite hospital. Clinical examination revealed a gross, bilateral
occlusal step in the parasymphysis region of mandible. On
Semirigid fixation of mandibular fractures with the use of
an orthopantomogram, a bilateral parasymphysis fracture
miniplates and screws offers some advantages, in select
with central segment malunited in an inferiorly displaced
cases, over rigid fixation and maxillomandibular fixation
position was noted (Fig. 1). The left side had been fixed
[1, 2]. A striking difference in the application of semirigid
with a single four-hole plate with only two screws used:
miniplates, when compared with rigid systems of osteosyn-
one per side of the fracture line. On the right side, a five-
thesis, is the use of monocortical versus bicortical screws
hole plate had been used, with two screws placed on each
[3]. Monocortical screws engage only one cortex and, being
side of the fracture line. An anterior open bite was also
self-tapping, eliminate the need for using a screw tap in the
appreciated.
drilled hole, but their reduced anchorage also makes
With this fixation, the patient was unable to masticate
fixation less capable than bicortical screws of resisting
efficiently and was in constant pain and discomfort. The
muscle forces especially if principles of fixation are not
lips were incompetent due to anterior open bite and
respected. Champy and colleagues, using in vitro experi-
bimanual palpation revealed mobility of the anterior
mental models and mathematical studies at Strasbourg,
mandibular fragment. There was evidence, clinical and
determined ideal lines of osteosynthesis based on the initial
radiographic, of loss of the canine on the left side and of the
work of Michelet et al. [1–3]. They also highlighted a
first premolar on the right side. We were unable to
second parallel line of osteosynthesis in the anterior
determine whether these teeth had been avulsed during
the traumatic injury or had been removed at the hospital.
N. Uppal (*) : M. Baliga : A. Ramanathan
Based on the unacceptable occlusion, poor esthetics, and
Manipal College of Dental Sciences,
Mangalore, India local discomfort, a decision to correct the malunited fracture
e-mail: drnakul@gmail.com was made. Under general anesthesia, after reopening the
178 Oral Maxillofac Surg (2009) 13:177–179
treatment of fractures in the child patient due to (a)
remaining growth potential, (b) the presence of developing
tooth buds in various stages of eruption, (c) incomplete root
formation, and (d) unreliable cooperation from the child
patient. Pediatric jaw fractures are thus often managed
successfully with closed reduction and indirect fixation
using acrylic splints and maxillomandibular fixation
(MMF) [5]. In the patient who presented to us for
retreatment, there were three reasons why we chose to treat
with open reduction and internal fixation rather than closed
reduction: First, the deciduous teeth had been replaced by
permanent dentition but since root formation was not
complete, MMF would have risked tooth extrusion.
Second, the spaces created by loss of teeth at the fracture
site would make immobilization with arch bars and/or wires
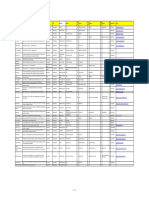
Fig. 1 Bilateral parasymphysis fracture of mandible with gross difficult. Third, the patient presented with a grossly
displacement of fragment as a consequence of inadequate and
improper fixation displaced fragment and open bite after initial surgery and
we did not wish to risk a recurrence after retreatment.
previous incision in the labial sulcus, we removed the plates The strong and thick outer cortex of the mandible
and screws and proceeded to osteotomize the fragment. provides osteosynthesis screws with good anchorage due
Having mobilized the anterior fractured fragment, arch bars to the compact bone [2]. Even though the thickness of
were placed to achieve intermaxillary fixation and immobi- cortex may be as little as 3 mm, its strength offers sufficient
lize the teeth in occlusion. Fixation across the fractured right monocortical anchorage to screws [1]. Although rigid
parasymphysis consisted of a six-hole miniplate secured fixation is stable, dynamic compression plates can be
with five screws and a four-hole miniplate secured with three palpable [3] and uncomfortable to a child or adolescent
screws. For the left parasymphysis, a five-hole miniplate and might therefore require removal. Using miniplates for
with five screws along with a position screw near the lower osteosynthesis has some advantages over rigid fixation
border were placed (Fig. 2). Postoperatively, the patient systems. The smaller dimensions of these plates enable
recovered normal oral function and occlusion. them to be adapted with greater ease to the contours of
bone [3]. However, this reduced mechanical strength and
consequent lack of rigidity makes it important for the
Discussion surgeon to respect Champy’s lines of ideal osteosynthesis
when planning the location of bone plates. In 1976 at
Fractures of the mandible in children are uncommon [5]. Strasbourg, Champy et al. used polarized light to examine
When they do occur, there are special considerations for the isostatic lines of tension that developed in a vertically
loaded, cantilevered araldite bar [1, 2]. They determined
that an osteosynthesis plate placed at the upper border
effectively neutralized masticatory forces of 60 DaN in the
molar region. Two plates would resist forces up to 100 DaN
in the incisor region, due to the additional torsion induced
by the parabolic shape of the mandible [2]. Although one
thicker, more rigid plate might suffice, its palpable profile
would defeat one of the advantages of miniplate osteosyn-
thesis over rigid plating systems. Also, rigid plating might
risk the “stress shielding” effect [1]. In the case reported,
there was a bilateral fracture of the mandibular para-
symphysis. Unlike maxillomandibular fixation, where the
jaws are immobilized, with semirigid miniplate osteosyn-
thesis limited early function is possible [3]. In fact, Champy
et al. in their landmark article mentioned that each of the
183 patients in their series began a soft diet on the first
Fig. 2 Reduction and immobilization of fractured fragment and postoperative day [1]. A bilateral fracture would, however,
placement of functionally stable fixation permit greater movement of the fractured segment. The lack
Oral Maxillofac Surg (2009) 13:177–179 179
of a second plate in our patient, supposed to have been is associated with an incidence of malocclusion thrice as
placed parallel to the first, across each fracture site much as that with MMF [5]. With miniplate systems that
permitted displacement of the anterior mandibular frag- rely on Champy’s lines of ideal osteosynthesis, there is only
ment, probably owing to contraction of the anterior bellies a passive noncompression fixation. Therefore, if principles
of digastric, geniohyoid, and the mylohyoid muscles during are ignored by using inadequate and/or inappropriately
oral function. In the case reported, as the site of the fracture located plates, failure of fixation is imminent when
was parasymphysis, the inadequate hardware used was masticatory loads are applied. Training in residency must
unlikely to have been able to resist flexion and torsion therefore emphasize on the biomechanical principles of
especially since the anterior mandible had fractured reduction, immobilization, and fixation, and the need to
bilaterally. As a bilateral fracture carries a larger risk of restore occlusion. Indeed, it is worthy to note that in their
displacement, we retained the arch bar postoperatively to series of 183 cases, with adherence to biomechanical
act as a tension band. principles, Champy et al. reported an incidence of malunion
After miniplates are adapted to bone contours, it is of just 0.5% [1]. In the case we reported, if these principles
standard to place at least two screws on either side of the had been adhered to during primary surgery itself, the
fracture site [2, 3]. On the left side of mandible, this patient expenditure and morbidity of corrective secondary surgery
had placement of only one screw per fragment. Unless at could have been avoided.
least two screws are placed per side of fracture, rotation of
the fragment is likely to occur. While reoperating on this
side, we used a position screw in addition to a miniplate. References
“Lag” or “position” screws rigidly hold segments of bone
in a stable relationship and thus resist displacement by 1. Champy M, Loddé JP, Schmitt R, Jaeger JH, Muster D (1978)
muscle forces [6]. Mandibular osteosynthesis by miniature screwed plates via a buccal
The primary goals of fracture management include approach. J Maxillofac Surg 6:14–21
restoration of pre-injury occlusion, necessitating the 2. Champy M, Pape HD, Gerlach KL, Lodde JP (1986) The
Strasbourg miniplate osteosynthesis. In: Krüger E, Schilli W (eds)
achievement of MMF to place the teeth in proper Oral and maxillofacial traumatology, vol. 2. Quintessence, Berlin,
occlusion, usually with arch bars and steel wires. pp 19–43
Although MMF is released after placement of miniplate 3. Frost DE, Tucker MR, White RP (1991) Small bone plate
fixation, the arch bars are usually left wired to the teeth techniques for fixation of mandibular fractures. In: Tucker MR,
Terry BC, White RP, Sickels JEV (eds) Rigid fixation for
and they may, in conjunction with training or guiding maxillofacial surgery. Lippincott, Philadelphia, pp 104–122
elastics, help in “fine-tuning” mild occlusal discrepan- 4. Gerlach KL, Erle A (1999) Surgical management of mandibular
cies since miniplates are malleable [7]. In the case, we fractures. In: Booth PW, Schendel SA, Hausamen J-E (eds)
have reported that arch bars had not been placed either Maxillofacial surgery, vol. 1. Churchill Livingstone, Edinburgh,
pp 57–78
prior to or after initial surgery and this may have 5. Chacon GE, Larsen PE (2004) Principles of management of
contributed to difficulties in achieving secure reduction. mandibular fractures. In: Miloro M, Ghali GE, Larsen PE, Waite
Also, as teeth in the line of fracture bilaterally were lost PD (eds) Peterson’s principles of oral and maxillofacial surgery,
during trauma, reduction would have been technically 2nd edn. Decker, Hamilton, pp 401–434
6. Shetty V, Caputo A (1992) Biomechanical considerations in oral
more challenging, a strong indication for arch bars and and maxillofacial surgery. In: Bell WH (ed) Modern practice in
MMF as a first step—that of fracture reduction—in the orthognathic and reconstructive surgery, vol. 3. Saunders, Phila-
surgical operation. delphia, pp 1956–1995
The findings after initial surgery in this case highlight the 7. Heslop IH, Cawood JI, Stoelinga PJW, Becker R, Blekinsopp P,
Boyne P, Williams JLl (1994) Mandibular fractures: treatment by
pitfalls of fracture treatment if performed without respecting open reduction and direct skeletal fixation. In: Williams JLl (ed)
the principles of reduction, immobilization, and fixation. It Rowe and Williams’ maxillofacial injuries, vol. 1, 2nd edn.
has been stated that the use of bone plates for osteosynthesis Churchill Livingstone, Edinburgh, pp 341–385
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- ParesthesiaoftheupperlipDocument4 pagesParesthesiaoftheupperlipikeuchi_ogawaNo ratings yet
- European Journal of OrthodonticsDocument288 pagesEuropean Journal of Orthodonticsikeuchi_ogawaNo ratings yet
- Volume Xliv Number 1 JANUARY 2010: 19 2009 Practice StudyDocument1 pageVolume Xliv Number 1 JANUARY 2010: 19 2009 Practice Studyikeuchi_ogawaNo ratings yet
- WelcomeDocument5 pagesWelcomeCatNo ratings yet
- Matakuliah S2Document4 pagesMatakuliah S2Bayu Aji KurniawanNo ratings yet
- Pertamina PertashopDocument4 pagesPertamina Pertashopikeuchi_ogawa79% (19)
- Surat Kepala BKN Nomor K.26 30V.72 299Document4 pagesSurat Kepala BKN Nomor K.26 30V.72 299ikeuchi_ogawaNo ratings yet
- Text BookDocument1 pageText Bookikeuchi_ogawaNo ratings yet
- Correction of An Anterior Crossbite With A Fixed Partial DentureDocument4 pagesCorrection of An Anterior Crossbite With A Fixed Partial Dentureikeuchi_ogawaNo ratings yet
- Soal CPNS Paket 3Document8 pagesSoal CPNS Paket 3icoirs 2016No ratings yet
- Forced Eruption of Adjoining Maxillary Premolars Using A Removable Orthodontic Appliance: A Case ReportDocument4 pagesForced Eruption of Adjoining Maxillary Premolars Using A Removable Orthodontic Appliance: A Case Reportikeuchi_ogawaNo ratings yet
- The Editor'S Corner: Mouthguards and OrthodonticsDocument2 pagesThe Editor'S Corner: Mouthguards and Orthodonticsikeuchi_ogawaNo ratings yet
- Anterior Crossbite Correction in Primary and Mixed Dentition With Removable Inclined Plane (Bruckl Appliance)Document5 pagesAnterior Crossbite Correction in Primary and Mixed Dentition With Removable Inclined Plane (Bruckl Appliance)Amr Eldok100% (1)
- 084 05Document1 page084 05ikeuchi_ogawaNo ratings yet
- Iatrogenic Mandibular Fracture Associated With Third Molar RemovalDocument3 pagesIatrogenic Mandibular Fracture Associated With Third Molar Removalikeuchi_ogawaNo ratings yet
- OverdenturesDocument29 pagesOverdenturesShyam K MaharjanNo ratings yet
- Asian Journal of Pharmaceutical and Clinical ResearchDocument2 pagesAsian Journal of Pharmaceutical and Clinical Researchikeuchi_ogawaNo ratings yet
- Interesting - Case - Report - of - Tooth - Inside - Nasal - Cavity (+)Document3 pagesInteresting - Case - Report - of - Tooth - Inside - Nasal - Cavity (+)ikeuchi_ogawaNo ratings yet
- Asian Journal of Pharmaceutical and Clinical ResearchDocument2 pagesAsian Journal of Pharmaceutical and Clinical Researchikeuchi_ogawaNo ratings yet
- Bds Tutorial Overdentures 1Document7 pagesBds Tutorial Overdentures 1ikeuchi_ogawaNo ratings yet
- 12 Ectopic Supernumerary Nasal Tooth Case Report 2Document3 pages12 Ectopic Supernumerary Nasal Tooth Case Report 2ikeuchi_ogawaNo ratings yet
- Maat 08 I 2 P 173Document2 pagesMaat 08 I 2 P 173ikeuchi_ogawaNo ratings yet
- 10.conservative Management of A Dentigerous Cyst Secondary To PrimaryDocument4 pages10.conservative Management of A Dentigerous Cyst Secondary To Primaryikeuchi_ogawaNo ratings yet
- 85-6403 e (C) F (T) PF1 (MH) Pfa (H)Document3 pages85-6403 e (C) F (T) PF1 (MH) Pfa (H)ikeuchi_ogawaNo ratings yet
- A Denture Swallowed. Case Report 1995Document3 pagesA Denture Swallowed. Case Report 1995ikeuchi_ogawaNo ratings yet
- A Denture Swallowed. Case Report 1995Document3 pagesA Denture Swallowed. Case Report 1995ikeuchi_ogawaNo ratings yet
- 6 TissueManagementDocument4 pages6 TissueManagementikeuchi_ogawaNo ratings yet
- Grafik, PersentilDocument22 pagesGrafik, PersentilkadekpramithaNo ratings yet
- E Plaque PDFDocument10 pagesE Plaque PDFjemmysenseiNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Drug Study - HRZEDocument4 pagesDrug Study - HRZEEunice Ordonez67% (3)
- عملیات شفاء امراض Amliyat Shifa Amraz 0091-33-23607502 - DIL KE AMRAZ KA RUHANI ELAJ (Spiritual Treatment of Heart Diseases)Document4 pagesعملیات شفاء امراض Amliyat Shifa Amraz 0091-33-23607502 - DIL KE AMRAZ KA RUHANI ELAJ (Spiritual Treatment of Heart Diseases)msmpaki@yahoo.comNo ratings yet
- Safety For LabDocument14 pagesSafety For LabAravind B PatilNo ratings yet
- LCB ResponseDocument13 pagesLCB ResponseLas Vegas Review-JournalNo ratings yet
- Instant Healing Meditation (Basic) - David Alan RamsdaleDocument31 pagesInstant Healing Meditation (Basic) - David Alan Ramsdaledeichem88% (8)
- Science and Practice of Pressure Ulcer ManagementDocument213 pagesScience and Practice of Pressure Ulcer ManagementRoy GoldenNo ratings yet
- Post Retirement Medical Facilities Scheme (PRMFS) For Employees of D.S.I.I.Dc. Ltd. TitleDocument4 pagesPost Retirement Medical Facilities Scheme (PRMFS) For Employees of D.S.I.I.Dc. Ltd. Titleanand#99No ratings yet
- Sample of Psychological ReportDocument4 pagesSample of Psychological ReportRochelle Joyce Olmilla Bersamin67% (3)
- Biederman 1962Document15 pagesBiederman 1962Luisa Fernanda PerdomoNo ratings yet
- Migraine Patient HandoutDocument14 pagesMigraine Patient HandoutthiautamiNo ratings yet
- Antepartum HemorrhageDocument48 pagesAntepartum HemorrhageJoshua EvansNo ratings yet
- NAGC 0910 Tulsa Final BTDocument40 pagesNAGC 0910 Tulsa Final BTlparliNo ratings yet
- Alat Alat MedisDocument6 pagesAlat Alat MedisDiasTikaNo ratings yet
- Serenity: Violence, Inequality, and Recovery On The Edge of Mexico CityDocument18 pagesSerenity: Violence, Inequality, and Recovery On The Edge of Mexico CityE Panchi NuñezNo ratings yet
- Speaker Dr. Annisa Tridamayanti, SPJP, Fiha Sesi 5Document3 pagesSpeaker Dr. Annisa Tridamayanti, SPJP, Fiha Sesi 5thiadinaNo ratings yet
- Genetic Engineering Applications in Animal BreedingDocument6 pagesGenetic Engineering Applications in Animal BreedingFadilla HadiwijayaNo ratings yet
- Setup Rak ObatDocument161 pagesSetup Rak Obatmuna barajaNo ratings yet
- Mendiguchia 2012 Rectus Femoris Muscle Injuries in Football-A Clinically Relevant Review of Mechanisms of Injury, Risk Factors and Preventive Strategies PDFDocument11 pagesMendiguchia 2012 Rectus Femoris Muscle Injuries in Football-A Clinically Relevant Review of Mechanisms of Injury, Risk Factors and Preventive Strategies PDFJuan PalomoNo ratings yet
- Cons 3 QuestionsDocument23 pagesCons 3 QuestionsŇøoř ĄłhųdàNo ratings yet
- Kansas Foodborne Illness ManualDocument186 pagesKansas Foodborne Illness ManualLeo M. Pedro Jr.No ratings yet
- Supraspinatus Tendon Pathomechanics: A Current Concepts ReviewDocument12 pagesSupraspinatus Tendon Pathomechanics: A Current Concepts Reviewgia purnamaNo ratings yet
- BooksDocument5 pagesBooksDanijela VukcevicNo ratings yet
- Evidence-Based Care SheetDocument6 pagesEvidence-Based Care SheetTITINNo ratings yet
- Discharge Planning: MedicationDocument3 pagesDischarge Planning: MedicationLeasNo ratings yet
- ECAM2015 324369 PDFDocument6 pagesECAM2015 324369 PDFLuiz Otavio CostaNo ratings yet
- Name Clinic/Hosp/Med Name &address Area City Speciality SEWA01 Disc 01 SEWA02 DIS C02 SEWA03 Disc 03 SEWA04 DIS C04 Contact No. EmailDocument8 pagesName Clinic/Hosp/Med Name &address Area City Speciality SEWA01 Disc 01 SEWA02 DIS C02 SEWA03 Disc 03 SEWA04 DIS C04 Contact No. EmailshrutiNo ratings yet
- H3C Abstract Final 11262014Document204 pagesH3C Abstract Final 11262014AAPI ConventionNo ratings yet
- MollyDocument7 pagesMollyapi-534233456No ratings yet
- SPE GanjaDocument4 pagesSPE Ganjaintan kusumaningtyasNo ratings yet
- Braden ScaleDocument2 pagesBraden ScaleAJ Tuban CompelioNo ratings yet