Professional Documents
Culture Documents
Palliative Care NEJMcp035232
Uploaded by
NadewdewCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Palliative Care NEJMcp035232
Uploaded by
NadewdewCopyright:
Available Formats
The new england journal of medicine
clinical practice
Palliative Care
R. Sean Morrison, M.D., and Diane E. Meier, M.D.
From the Hertzberg Palliative Care Institute, An 85-year-old man with New York Heart Association class IV heart failure, hyperten-
Brookdale Department of Geriatrics and sion, and moderate Alzheimer’s disease is admitted to the hospital after a hip fracture.
Adult Development, Mount Sinai School of
Medicine, New York. Address reprint re- His postoperative course is complicated by pneumonia, delirium, and pressure ulcers
quests to Dr. Morrison at the Department on his heels and sacrum. He is losing weight and is unable to participate in rehabilita-
of Geriatrics, Box 1070, Mount Sinai School tion because of his confusion. This is his fourth hospitalization in the past year. His
of Medicine, One Gustave L. Levy Place,
New York, NY 10029, or at sean.morrison@ 84-year-old wife, who has been caring for him at home, feels overwhelmed by his
mssm.edu. medical and personal care needs. The patient’s physician is increasingly frustrated by
his frequent readmissions. What might she do to address his needs, alleviate his suf-
N Engl J Med 2004;350:2582-90.
Copyright © 2004 Massachusetts Medical Society.
fering, and facilitate his discharge from the hospital and subsequent care at home?
the clinical problem
By 2030, 20 percent of the U.S. population will be over the age of 65 years.1 For most
people, the years after the age of 65 are a time of good health, independence, and inte-
gration of a life’s work and experience. Eventually, most adults will have one or more
chronic illnesses with which they will live for years before they die. These years are often
characterized by physical and psychological distress, progressive functional depen-
dence and frailty, and increased needs for family and external support.1 Studies sug-
gest that medical care for patients with serious and advanced illnesses is characterized
by the undertreatment of symptoms, conflict about who should make decisions about
the patient’s care, impairments in caregivers’ physical and psychological health, and
depletion of family resources.2-5
strategies and evidence
the role of palliative care
There are many reasons why patients who have advanced illnesses receive inadequate
care, but most of those reasons are rooted in a medical philosophy that is focused al-
most exclusively on curing illness and prolonging life, rather than on improving the
quality of life and relieving suffering. Traditionally, medical care has been articulated as
having two mutually exclusive goals: either to cure disease and prolong life or to provide
comfort care.1 Given this dichotomy, the decision to focus on reducing suffering is
made only after life-prolonging treatment has been ineffectual and death is imminent.6
In the United States, this forced choice is driven largely by the reimbursement system
— that is, regular Medicare covers curative therapies and the Medicare hospice benefit
covers comfort care. That division of services results both in the provision of burden-
some and costly life-prolonging treatments when they are no longer beneficial and in
preventable suffering during all stages of advanced illness.7 In contrast, patients would
benefit most from care that included a combination of life-prolonging treatment (when
possible and appropriate), palliation of symptoms, rehabilitation, and support for care-
givers.
Meeting the needs of patients will require that physicians employ skills that are
2582 n engl j med 350;25 www.nejm.org june 17, 2004
The New England Journal of Medicine
Downloaded from www.nejm.org on November 22, 2010. For personal use only. No other uses without permission.
Copyright © 2004 Massachusetts Medical Society. All rights reserved.
clinical practice
not traditionally taught in medical schools.8 Pal-
liative care aims to relieve suffering and improve the Establishing Goals Communicating Withdrawing
quality of life for patients with advanced illnesses of Medical Care Bad News Treatment
and their families through specific knowledge and
skills, including communication with patients and
Create the right setting: plan what to say, allow adequate time, and determine who
family members; management of pain and other else should be present at the meeting
symptoms; psychosocial, spiritual, and bereave-
ment support; and coordination of an array of
medical and social services.1 Palliative care should Establish what the patient Establish what the patient Establish and review the
knows: clarify the situation knows: clarify what the goals of care
be offered simultaneously with all other medical and context in which the patient can comprehend;
treatment. discussion about goals is reschedule the talk if
occurring necessary
physician–patient communication
Communicating with patients is a core skill of Explore what the patient Establish how much the Establish the context of
palliative medicine.9 Studies suggest that in a typi- is hoping to accomplish: patient wants to know: the current discussion:
help distinguish between recognize and support discuss what has
cal clinical encounter, clinicians elicit fewer than realistic and unrealistic preferences; people handle changed to precipitate
half of patients’ concerns and consistently fail to dis- goals information in different the discussion
ways
cuss patients’ values, goals of care, and preferenc-
es with regard to treatment.10 Empirical evidence
supports the effectiveness of clinicians’ use of spe- Suggest realistic goals: Share the information: Discuss specific treatment
cific communication skills in enhancing disclosure explore how goals can avoid jargon, pause in the context of the goals
be achieved and work frequently, check for of care: talk about whether
of the issues of concern to a patient, decreasing through unrealistic understanding, use the treatment will meet
anxiety, assessing depression, and improving a expectations silence; do not minimize the goals of care
the information
patient’s well-being and the level of the patient’s
and the family’s satisfaction with the treatment.10
Those communication skills include making eye Discuss alternatives to
contact with patients, asking open-ended ques- the proposed treatment:
talk about what will
tions, responding to a patient’s affect, and demon- happen if the patient
strating empathy. When a physician is informing decides not to have the
treatment
a patient about a poor prognosis, conducting an
open, “patient-centered” interview (in which the
emphasis is on empathy, openness, and reassur- Respond empathetically to feelings: be prepared for strong emotions and allow time
ance), rather than the traditional closed, “physician- for response, listen, encourage description of feelings, allow silence
centered” interview (in which the physician is fo-
cused on the task), has been associated with an
Make a plan and follow Follow up: plan for next Plan for the end of
improved level of satisfaction on the part of patients through: discuss which steps, discuss potential treatment: document
and their families.11 treatments will be under- sources of support, a plan for withdrawal
taken to meet the goals, share contact information, of treatment and give
Guidelines have been developed for establishing establish a concrete plan assess the patient’s safety it to the patient, the
goals of medical care, communicating bad news, for follow-up, review and and support, repeat news patient’s family, and
revise the plan periodically at future visits members of the health
and withholding or withdrawing medical treat- as needed care team
ments (Fig. 1).12,13 Whether the use of these proto-
cols actually helps patients and their families has Figure 1. Protocols for Communicating with Patients about Major Topics
not been empirically determined, but we and in Palliative Care.
others12-16 have found these guidelines to be use- Adapted from the Education on Palliative and End-of-life Care Project.12
ful in clinical practice. One randomized trial in the
United Kingdom showed that a postgraduate course
in communication skills that had cognitive, behav-
ioral, and affective components led to improved of care. Outlining realistic and attainable goals
communication skills among the physicians.17 assumes an increased importance in the setting of
Similar courses are offered annually in the United advanced disease, in which treatments intended
States.18,19 to cure the disease and prolong life may be more
Palliative care begins with establishing the goals burdensome than beneficial. Whereas the goal for
n engl j med 350;25 www.nejm.org june 17, 2004 2583
The New England Journal of Medicine
Downloaded from www.nejm.org on November 22, 2010. For personal use only. No other uses without permission.
Copyright © 2004 Massachusetts Medical Society. All rights reserved.
The new england journal of medicine
some patients may be to prolong life at any cost, prevalence of advance directives over the past dec-
studies suggest that what most seriously ill patients ade will improve their effectiveness, as physicians
want is to have their pain and other symptoms re- and patients become more familiar with them and
lieved, improve their quality of life, avoid being a physicians become more comfortable using them
burden to their family, have a closer relationship for assistance in guiding the care of cognitively im-
with loved ones, and maintain a sense of control.9,20 paired adults. A recent report suggested that the
Establishing clear goals can facilitate decision focus of advance care planning should shift from
making regarding treatment. For example, in the discussing specific treatments to defining an ac-
case of a patient with end-stage dementia who has ceptable quality of life and setting goals for care
dysphagia, placement of a percutaneous endoscop- under various likely clinical scenarios.26,27 Whether
ic gastrostomy (PEG) tube may be considered. If the this goal-centered approach to advance care plan-
primary goal is to reduce suffering and enhance the ning will affect clinical outcomes is unknown.
quality of life, then placing a PEG tube is unlikely to
meet these goals, since it requires a painful, inva- assessment and treatment of symptoms
sive procedure; eliminates the pleasurable oral sen- A fundamental goal of palliative care is the relief of
sations of eating and drinking; is associated with pain and other symptoms.9,20 Successful approach-
an increased use of restraints; can cause cellulitis, es to the assessment and management of pain and
vomiting, diarrhea, and fluid imbalances; and is un- some physical and psychological symptoms have
likely to reduce the risk of aspiration.21 Even in been established in controlled trials.12,28-30 Despite
cases in which a primary goal is to prolong life, the these advances, undertreatment of symptoms per-
role of a PEG tube remains questionable; no survival sists in the majority of patients and settings.2,31
benefits have been shown in observational studies Relief of suffering begins with routine and stan-
in which patients with dementia who received feed- dardized symptom assessment with use of vali-
ing tubes were compared with similar patients who dated instruments. Routine assessment has been
did not receive feeding tubes.21 shown to identify overlooked and unreported symp-
Expert opinion suggests that clinicians can as- toms, facilitate treatment, and enhance patient and
sist patients and their families in establishing their family satisfaction.32,33 Clinically useful assessment
own goals by means of open-ended and probing instruments can be found on the Web sites of the
questions. Some examples of the types of questions Center to Advance Palliative Care (www.capc.org)
include “What makes life worth living for you?” and of Brown University’s Center for Gerontology
“Given the severity of your illness, what are the and Health Care Research, which features a tool kit
most important things for you to achieve?” “What of instruments to measure end-of-life care (www.
are your most important hopes?” “What are your chcr.brown.edu/pcoc/toolkit.htm).
biggest fears?” and “What would you consider to be Improved treatment of symptoms has been as-
a fate worse than death?”16 The goals that patients sociated with the enhancement of patient and fam-
establish may overlap, be contradictory, rise and fall ily satisfaction, functional status, quality of life,
in importance, and shift with the progression of the and other clinical outcomes.32,34 Although a com-
disease.12,16 Warning signs of poorly established prehensive review of strategies for assessment and
or conflicting goals can include frequent and therapy of symptoms is beyond the scope of this re-
lengthy hospitalizations; feelings of frustration, view, Table 1 summarizes approaches to common-
anger, or powerlessness on the part of the physician; ly encountered symptoms in advanced illnesses.
and feelings of being burdened on the part of care-
givers.15 psychosocial, spiritual,
Once goals are established, they can be used to and bereavement support
construct advance directives about the types of care Providing psychosocial, spiritual, and bereavement
that patients want. Most studies,22 although not support to patients and caregivers is a key compo-
all,23,24 have shown that few patients have advance nent of palliative care. Patients who experience
directives and that the documents they do have are spiritual and psychological distress are more like-
relatively ineffectual in enhancing physician–patient ly to express a desire for death than are other pa-
communication, facilitating decision making about tients,42 and their family members are more likely
resuscitation,25 or influencing terminal care in hos- to have an extended or complicated grief and be-
pitals.22 It is possible that the gradual rise in the reavement process (defined as grief that lasts for
2584 n engl j med 350;25 www.nejm.org june 17 , 2004
The New England Journal of Medicine
Downloaded from www.nejm.org on November 22, 2010. For personal use only. No other uses without permission.
Copyright © 2004 Massachusetts Medical Society. All rights reserved.
clinical practice
Table 1. Approaches to the Management of Pain and Other Common Symptoms.*
Symptom Assessment Treatment
Anorexia and Is a disease process causing the symptom, or is it Consider megestrol acetate or dexamethasone.
cachexia secondary to other symptoms (e.g., nausea and
constipation) that can be treated? Is the patient
troubled by the symptom?
Anxiety Does the patient exhibit restlessness, agitation, Recommend supportive counseling and consider prescribing ben-
insomnia, hyperventilation, tachycardia, or zodiazepines (in the elderly, avoid benzodiazepines with long
excessive worry? half-lives).
Constipation Is the patient taking opioids? Does the patient have Prescribe a stool softener (ineffective alone) plus escalating doses
a fecal impaction? of a stimulant; if escalation of the dose is ineffectual, agents
from other classes (e.g., osmotic laxatives and enemas) should
be added.
Depression How does the patient respond to the question “Are Recommend supportive psychotherapy, cognitive approaches, be-
you depressed?” Does the patient express or ex- havioral techniques, pharmacologic therapies, or a combination
hibit any of the following feelings: helplessness, of these interventions; prescribe psychostimulants for rapid
hopelessness, anhedonia, loss of self-esteem, treatment of symptoms (within days) or selective serotonin-
worthlessness, persistent dysphoria, and suicidal reuptake inhibitors, which may require three to four weeks to
ideation? (Somatic symptoms are not reliable in- take effect; tricyclic antidepressants are relatively contraindi-
dicators of depression in this population.) cated because of their side effects.
Delirium Was the onset of confusion acute? Is the patient dis- Identify underlying causes and manage symptoms; recommend
oriented or experiencing changes in the level of behavioral therapies, including avoidance of excess stimulation,
consciousness or minute-to-minute fluctuations? frequent reorientation, and reassurance; ensure presence of
Is the condition reversible? family caregivers; prescribe haloperidol, risperidone, or olanza-
pine. (Chlorpromazine can be used for agitated or terminal de-
lirium, but benzodiazepines have been found to exacerbate delir-
ium and should be avoided.)
Dyspnea Does the symptom have reversible causes? Prescribe oxygen to treat hypoxia-induced dyspnea or to provide
symptomatic relief, when hypoxia is absent, through stimulation
of the V2 branch of the trigeminal nerve.
Opioids relieve breathlessness without measurable reductions in
respiratory rate or oxygen saturation; effective doses are often
lower than those used to treat pain.
Consider anxiolytics (e.g., low-dose benzodiazepines) and use re-
assurance, relaxation, distraction, and massage therapy.
Nausea Which mechanism is causing the symptom (e.g., Prescribe an agent directed at the underlying cause. Multiple agents
stimulation of the chemoreceptor trigger zone, directed at various receptors or mechanisms may be required.
gastric stimulation, delayed gastric emptying or
“squashed stomach” syndrome, bowel obstruc-
tion, intracranial processes, or vestibular vertigo)?
Pain How severe is the symptom (as assessed with the use Prescribe medications to be administered on a standing or regular
of validated instruments)? basis; as-needed or rescue doses should be available for break-
through pain or pain not controlled by the standing regimen;
start a regimen to prevent constipation for all patients receiving
opioids.
For mild pain: use acetaminophen or a nonsteroidal antiinflamma-
tory agent (consider opioids in older adults). For moderate pain:
titrate short-acting opioids. For severe pain: rapidly titrate short-
acting opioids until pain is relieved or intolerable side effects
develop; start long-acting opioids (e.g., sustained-release mor-
phine or oxycodone and transdermal fentanyl) once pain is well
controlled; use methadone only if experienced in its use.
Rescue doses: prescribe immediate-release opioids consisting of 10%
of the 24-hour total opioid dose to be given every hour (orally) or
every 30 minutes (parenterally) as needed. Concomitant analge-
sics (e.g., corticosteroids, anticonvulsants, tricyclic antidepres-
sants, and bisphosphonates) should be used when applicable.
* For details of recommendations and more information about the management of symptoms, see Foley, 35 American Geriatrics Society Panel
on Persistent Pain in Older Persons,36 Luce and Luce,37 Casarett and Inouye,38 Strasser and Bruera,39 Block,40 and Regnard and Comiskey.41
n engl j med 350;25 www.nejm.org june 17, 2004 2585
The New England Journal of Medicine
Downloaded from www.nejm.org on November 22, 2010. For personal use only. No other uses without permission.
Copyright © 2004 Massachusetts Medical Society. All rights reserved.
The new england journal of medicine
at least 14 months after the death and results in a and family satisfaction than does conventional
failure of the survivor to return to his or her normal care.49,50,52,53
activities) and are at higher risk for illness and Other programs that coordinate care for patients
death.43 who have complex illnesses are available in most
Studies suggest that patients welcome inquiries communities. Programs that coordinate home care
about their spiritual well-being from their physi- services for patients with chronic conditions (e.g.,
cians,44 although interventions to address spiri- depression, heart failure, or the acquired immuno-
tual distress have not been well developed or well deficiency syndrome) have been associated with in-
evaluated. Support groups have been found to re- creased patient and family satisfaction and reduc-
duce stress and depression experienced by care- tions in mortality, use of hospital services, visits
givers.45,46 Although many formal interventions to physicians’ offices, and admission to nursing
to address complicated grief and bereavement have homes.54-56 Case management is usually provid-
been described, data are lacking on their effects ed by managed-care organizations, Medicare man-
on outcomes.47 Two recent studies reported lower aged-care services, commercial insurers, some
morbidity and mortality48 and better emotional home health care agencies, and privately hired case
support49 among surviving family members of hos- managers. The quality, cost, and extent of the ser-
pice patients than among family members of pa- vices provided are highly variable.
tients who did not receive hospice services, although Comprehensive multidisciplinary home care
it is uncertain whether this difference reflects the programs that serve frail older adults have been
nature of families who elect hospice care rather evaluated under Medicare and the Veterans Health
than the effects of the intervention.48 Administration (VHA). The Program of All-Inclu-
sive Care for the Elderly (PACE) is a capitated Medi-
coordination of care care and Medicaid benefit for frail older adults that
Several studies demonstrate that the personal and offers comprehensive medical and social services at
practical care needs of patients who are seriously ill 25 adult day health centers, in homes, and at in-
and their families are not adequately addressed by patient facilities. (More information about the pro-
routine office visits or hospital and nursing home gram is available online at www.cms.hhs.gov/pace/.)
stays and that this failure results in substantial bur- Patients who use the services provided by PACE
dens — medical, psychological, and financial — on have higher rates of completing advance directives
patients and their caregivers.3-5,49,50 In the context for their care57 and lower rates of admission to
of chronic progressive disease, the ability of physi- nursing homes,58 hospitalization,59 and death in
cians to coordinate an array of social and medical the hospital59 than do patients who do not use the
services on behalf of patients and families assumes services. Similar programs of team-coordinated
increased importance. home-based care exist within the VHA.60
Various comprehensive care programs are avail- Until comprehensive palliative care programs
able to help physicians manage the care of their become widely available, the responsibility for coor-
patients who have serious and complex illnesses. dination of care falls to the primary care physician,
Palliative care programs within home care organi- since patients and their families frequently have
zations, hospitals, and nursing homes are increas- problems negotiating the current health care sys-
ingly prevalent in the United States and provide tem. Table 2 details the range of palliative care ser-
comprehensive interdisciplinary care for patients vices that should be considered at various stages
and families in collaboration and consultation with of a serious illness; Table 3 lists services that are
primary care physicians.51 Hospice services, under covered by Medicare.
the Medicare benefit, are available in most U.S.
communities and provide palliative care, primarily areas of uncertainty
at home, for patients with a life expectancy of six
months or less who are willing to forgo insurance Physicians have few data to guide them in improv-
coverage for life-prolonging treatments. Studies ing their communication with patients and in their
suggest that referral to palliative care programs and management of pain and other symptoms. The
hospice results in beneficial effects on patients’ communication guidelines presented in Figure 1,
symptoms, reduced hospital costs, a greater likeli- although widely taught and used by palliative care
hood of death at home, and a higher level of patient experts, have not been shown to be associated with
2586 n engl j med 350;25 www.nejm.org june 17 , 2004
The New England Journal of Medicine
Downloaded from www.nejm.org on November 22, 2010. For personal use only. No other uses without permission.
Copyright © 2004 Massachusetts Medical Society. All rights reserved.
clinical practice
Table 2. Coordination of Care for Early, Middle, and Late Stages of Serious Chronic Illnesses.*
Palliative Care Services Early Stage Middle Stage Late Stage
Goals of care Discuss diagnosis, prognosis, Review patient’s understanding of Assess patient’s understanding of diag-
likely course of the illness, prognosis; review efficacy and nosis, disease course, and progno-
and disease-modifying ther- benefit-to-burden ratio for dis- sis; review appropriateness of dis-
apies; talk about patient- ease-modifying treatments; re- ease-modifying treatments; review
centered goals, hopes, and assess goals of care and expec- goals of care and recommend appro-
expectations for medical tations; prepare patient and priate shifts; help patient explicitly
treatments. patient’s family for a shift in plan for a peaceful death; encourage
goals; encourage paying atten- completion of important tasks and
tion to important tasks, relation- increased attention to relationships
ships, and financial affairs. and financial affairs.
Programmatic support Advise patient to sign up for Advise patient to sign up for visiting Advise patient to sign up for a palliative
visiting nurse and home nurse and home care services; care program in hospital or at home,
care services and case- consider palliative care program case-management services, hospice,
management services in hospital or at home, hospice, or PACE; consider nursing home
(if available). subacute rehabilitation, case- placement with hospice or palliative
management services, and care if patient’s home caregivers are
PACE. overwhelmed.
Financial planning Advise patient to seek help in Advise patient to reassess adequacy Advise patient to review all financial re-
planning for financial, long- of planning for financial, medi- sources and needs; inform patient
term care, and insurance cal, home care, prescription, and family about financial options
needs and to begin transfer long-term care, and family-sup- for personal and long-term care (e.g.,
of assets if patient is con- port needs; consider hospice re- hospice and Medicaid) if resources
sidering a future Medicaid ferral and Medicaid eligibility. are inadequate to meet needs; explic-
application; refer patient to itly recommend hospice and review
a lawyer who is experienced its advantages; consider Medicaid
in health issues. eligibility.
Family support Inform patient and family Encourage support or counseling for Encourage out-of-town family to visit;
about support groups; ask family caregivers; ensure that refer caregivers to disease-specific
about practical support caregivers have information support groups or counseling; in-
needs (e.g., transportation, about practical resources, stress, quire routinely about health, well-
prescription-drug coverage, depression, and adequacy of being, and practical needs of care-
respite care, and personal medical care; identify respite and givers; offer resources for respite
care); listen to concerns. practical support resources; rec- care; after death, send bereavement
ommend help from family and card and call after one to two weeks;
friends; raise the possibility of screen for complicated bereavement;
hospice and discuss its benefits; maintain occasional contact after
listen to concerns. patient’s death; listen to concerns.
* Early stage refers to the stage of disease at the time of diagnosis, middle stage to progressive disease and increasing functional decline, and
late stage to the stage when death is imminent. PACE denotes Program of All-Inclusive Care for the Elderly.
improved outcomes. Similarly, although data are have advanced chronic illnesses. These guidelines
available to guide the treatment of pain due to encompass many of the recommendations detailed
cancer, data are lacking regarding the treatment of in this article, and the National Consensus Project
other pain syndromes, symptoms other than pain guidelines also include recommendations regard-
(such as dyspnea, fatigue, delirium, and anxiety), ing the spiritual, religious, and existential aspects
spiritual distress, and complicated grief and be- of care; cultural aspects of care; and care of patients
reavement. whose death is imminent.62 Although the guide-
lines of the National Comprehensive Cancer Net-
guidelines work are targeted to patients with terminal cancer,
many patients who have early stages of the disease
The National Comprehensive Cancer Network61 or uncertain prognoses or who are undergoing
has developed guidelines for patients who have active curative or life-prolonging therapies can ben-
advanced incurable cancer, and the National Con- efit from the organization’s recommendations. The
sensus Project for Quality Palliative Care,62 a collab- application of those recommendations should
orative effort of five national palliative care organi- not be restricted to patients with a limited life ex-
zations, has similar guidelines for patients who pectancy.
n engl j med 350;25 www.nejm.org june 17, 2004 2587
The New England Journal of Medicine
Downloaded from www.nejm.org on November 22, 2010. For personal use only. No other uses without permission.
Copyright © 2004 Massachusetts Medical Society. All rights reserved.
The new england journal of medicine
Table 3. Summary of Medicare Coverage for Common Services Required by Patients with Serious and Chronic Illnesses.
Medicare Part A*
Service Coverage Out-of-Pocket Cost
Ambulance Transportation only to a hospital or skilled nursing facility and only if 20% of Medicare-approved amounts
transportation in any other type of vehicle endangers health
Custodial care No coverage for custodial care if this is the only care needed 100%
Home health care Skilled nursing care in the home for treatment of an acute illness if at None; if the patient has only Part B cover-
least one of the following is needed: intermittent skilled nursing age, services are covered by Part B
care, physical or speech therapy, or continuing occupational ther-
apy and if the patient is unable to leave the house except with ma-
jor effort
Hospice Eligibility: life expectancy of 6 mo or less if disease follows its usual None for regular hospice services; copay-
course and willingness to relinquish Medicare-reimbursed servic- ment of up to $5 for outpatient prescrip-
es focused on prolongation of life or cure; coverage includes phy- tion drugs; 5% of Medicare-approved
sician and nursing services, durable medical equipment and sup- amount for inpatient respite care
plies, medications for pain or symptom control, home health aide
and homemaker services (4 hr/day on average), physical and oc-
cupational therapy, short-stay hospitalizations and respite care,
social work services, and bereavement services; regular Medicare
covers services not related to hospice diagnosis; room and board
are covered only for respite care and short hospital stays, not for
nursing home or residential hospice stays
Hospital inpatient General hospital services with semiprivate room For each benefit period, deductible of $812
care for days 1–60, $203/day for days 61–90,
and $406/day for days 91–150; benefit
period begins on hospital day 1 and ends
when hospital or skilled nursing care
has not been received for 60 consecutive
days
Skilled nursing facility If patient has Part A benefit days remaining after hospitalization; qual- For each benefit period, none for days 1–20,
or rehabilitation ified hospital stay (inpatient stay of 3 consecutive days and entry $101.50/day for days 21–100, and
into a skilled nursing facility within 30 days of discharge); need for 100%/day for day 101
a skilled service to treat a medical condition that was treated in the
hospital or started while getting Medicare-covered skilled nursing
care; no coverage for nursing home custodial care
Medicare Part B†
Service Coverage Out-of-Pocket Cost
Custodial care No coverage for custodial care if this is the only care needed 100%
Durable medical “Air-fluidized” beds, canes, commode chairs, crutches, home oxygen Variable after $100 deductible
equipment and equipment (with qualifications), hospital beds, nebulizers,
patient lifts, suction pumps, walkers, and wheelchairs
Office visits to doctors No coverage for routine physical and gynecologic examinations 20% of Medicare-approved rates
Outpatient mental Office visits to physicians, clinical social workers, psychologists, 50% of Medicare-approved rates
health services nurse specialists, and physician assistants
Nonphysician health Office visits to clinical social workers, psychologists, physician assis- 20% of Medicare-approved rates
care services tants, and nurse practitioners (for medically necessary services)
Prescription drugs Limited coverage for erythropoietin only in end-stage renal disease, In 2004, 75 to 90 percent for most prescrip-
injectable drugs, limited oral cancer medications, limited oral an- tions. In 2005, a $35 monthly premium
tiemetics (if a Medicare-covered cancer drug), some infusion ther- and a $250 deductible; 25 percent of
apies (if considered reasonable and necessary). A Medicare dis- pharmacy costs between $250 and
count card is currently available for other prescription drugs and a $2,250 in drug spending, 100 percent
$600 credit is available for qualifying low-income individuals. In of costs between $2,250 and $3,600,
2005, a Medicare prescription-drug plan will become available. and 5 percent of costs over $3,600
Transportation No coverage for transportation to physicians’ offices, laboratory tests, 100%
outpatient physical therapy, or ambulette (van) services
* Under Part A, the patient pays no premium if the patient or the patient’s spouse has paid Medicare taxes while working for 40 or more quarters.
† Under Part B, the patient pays for optional coverage with a premium of $58.70 per month.
2588 n engl j med 350;25 www.nejm.org june 17 , 2004
The New England Journal of Medicine
Downloaded from www.nejm.org on November 22, 2010. For personal use only. No other uses without permission.
Copyright © 2004 Massachusetts Medical Society. All rights reserved.
clinical practice
bisphosphonates, avoidance of hospitalization, and
conclusions
and recommendations a trial of physical and occupational therapy with
the aim of regaining function. The patient’s dis-
The aim of palliative care is to relieve suffering and charge services will depend on the goals, the pa-
improve the quality of life for patients with ad- tient’s insurance coverage and financial resources,
vanced illnesses and their families. It is based on an and available home care services. Since a hospice
interdisciplinary approach that is offered simulta- program will support these goals, a referral to hos-
neously with other appropriate medical treatments pice should be considered. If hospice is not an op-
and involves close attention to the emotional, spiri- tion (e.g., because of limited home care hours or
tual, and practical needs and goals of patients and uncertainty about the prognosis), the patient should
of the people who are close to them. The patient be referred to a case-management program, PACE,
who is described in the vignette, who has multiple or a certified home care agency. The family’s ability
chronic and serious medical conditions but is not to afford medications should be evaluated, and al-
actively dying, is ideally suited to receive high-quality ternative sources (such as mail-order drug plans or
palliative care. Specifically, we suggest the follow- state-sponsored prescription plans for low-income
ing approach. The patient’s symptoms should be elderly people) or less costly medications should be
assessed and treated, as discussed in Table 1. If considered. Before discharge, a home-safety and
available, consultation with a palliative care team home-needs evaluation should be performed either
should be strongly considered to help with evaluat- by an occupational therapist or through a structured
ing and managing his symptoms. Once the patient interview with the patient’s caregiver. An assess-
is comfortable, a discussion about realistic goals ment of support requirements for the caregiver
should be held, with particular attention given to should be conducted to ensure that the personal
clarifying the patient’s opinion about an acceptable care needs of the patient and the patient’s family are
quality of life, identifying conditions under which met. Referral to a social worker can help identify
the patient would consider life not worth living, es- community alternatives and determine Medicaid
tablishing attainable short- and long-term goals, eligibility. Finally, a regular system of communi-
and designating a health care proxy. We recommend cation should be established between the treating
that this discussion be summarized in a treatment physician and the home care team.
directive and that a health-care-proxy form be com- Dr. Morrison is a Paul Beeson Faculty Scholar in Aging Research,
pleted. Once goals are clarified, appropriate treat- an Open Society Institute Project on Death in America Faculty Scholar,
and the recipient of a Mid-Career Investigator Award in Patient-
ment and discharge planning can begin. Oriented Research (K24AG022345) from the National Institute on
In the case described in the vignette, for example, Aging. Dr. Meier is an Open Society Institute Project on Death in
the treatment goal might be to focus on the pa- America Faculty Scholar, the recipient of an Academic Career Leader-
ship Award (K07AG00903) from the National Institute on Aging,
tient’s comfort and on caring for him at home, and and the director of the Center to Advance Palliative Care, a program
the appropriate treatments might be spoon-feeding office of the Robert Wood Johnson Foundation.
rather than placement of a PEG tube, diuretics and
references
1. Field MJ, Cassel CK, eds. Approaching tance from family members, friends, paid life care: a national report. J Gen Intern Med
death: improving care at the end of life. care givers, and volunteers in the care of ter- 2003;18:685-95.
Washington, D.C.: National Academy Press, minally ill patients. N Engl J Med 1999;341: 9. Steinhauser KE, Christakis NA, Clipp
1997. 956-63. EC, McNeilly M, McIntyre L, Tulsky JA. Fac-
2. The SUPPORT Principal Investigators. 5. Covinsky KE, Goldman L, Cook EF, et tors considered important at the end of life
A controlled trial to improve care for serious- al. The impact of serious illness on patients’ by patients, family, physicians, and other
ly ill hospitalized patients: the Study to Un- families. JAMA 1994;272:1839-44. care providers. JAMA 2000;284:2476-82.
derstand Prognoses and Preferences for Out- 6. Christakis NA, Escarce JJ. Survival of 10. Tulsky JA. Doctor-patient communica-
comes and Risks of Treatments (SUPPORT). Medicare patients after enrollment in hospice tion. In: Morrison RS, Meier DE, eds. Geri-
JAMA 1995;274:1591-8. [Erratum, JAMA programs. N Engl J Med 1996;335:172-8. atric palliative care. New York: Oxford Uni-
1996;275:1232.] 7. Fisher ES, Wennberg DE, Stukel TA, versity Press, 2003:314-31.
3. Emanuel EJ, Fairclough DL, Slutsman J, Gottlieb DJ, Lucas FL, Pinder EL. The impli- 11. Dowsett SM, Saul JL, Butow PN, et al.
Emanuel LL. Understanding economic and cations of regional variations in Medicare Communication styles in the cancer consul-
other burdens of terminal illness: the expe- spending. 2. Health outcomes and satisfac- tation: preferences for a patient-centered
rience of patients and their caregivers. Ann tion with care. Ann Intern Med 2003;138: approach. Psychooncology 2000;9:147-56.
Intern Med 2000;132:451-9. 288-98. 12. The EPEC Project: Education on Pallia-
4. Emanuel EJ, Fairclough DL, Slutsman J, 8. Sullivan AM, Lakoma MD, Block SD. tive and End-of-life Care. (Accessed April
Alpert H, Baldwin D, Emanuel LL. Assis- The status of medical education in end-of- 21, 2004, at http://www.epec.net.)
n engl j med 350;25 www.nejm.org june 17, 2004 2589
The New England Journal of Medicine
Downloaded from www.nejm.org on November 22, 2010. For personal use only. No other uses without permission.
Copyright © 2004 Massachusetts Medical Society. All rights reserved.
clinical practice
13. Buckman R. How to break bad news: Management of pain in elderly patients with 48. Christakis NA, Iwashyna TJ. The health
a guide for health care professionals. Balti- cancer. JAMA 1998;279:1877-82. [Erratum, impact of health care on families: a matched
more: Johns Hopkins University Press, 1992. JAMA 1999;281:136.] cohort study of hospice use by decedents
14. Goold SD, Williams B, Arnold RM. Con- 32. Bookbinder M, Coyle N, Kiss M, et al. and mortality outcomes in surviving, wid-
flicts regarding decisions to limit treatment: Implementing national standards for cancer owed spouses. Soc Sci Med 2003;57:465-75.
a differential diagnosis. JAMA 2000;283: pain management: program model and 49. Teno JM, Clarridge BR, Casey V, et al.
909-14. evaluation. J Pain Symptom Manage 1996; Family perspectives on end-of-life care at
15. Meier DE, Back AL, Morrison RS. The 12:334-47. the last place of care. JAMA 2004;291:88-93.
inner life of physicians and care of the seri- 33. Manfredi PL, Morrison RS, Morris J, 50. Miller SC, Mor V, Teno J. Hospice enroll-
ously ill. JAMA 2001;286:3007-14. Goldhirsch SL, Carter JM, Meier DE. Pallia- ment and pain assessment and manage-
16. Quill TE. Perspectives on care at the tive care consultations: how do they impact ment in nursing homes. J Pain Symptom
close of life: initiating end-of-life discus- the care of hospitalized patients? J Pain Manage 2003;26:791-9.
sions with seriously ill patients: addressing Symptom Manage 2000;20:166-73. 51. Center to Advance Palliative Care home
the “elephant in the room.” JAMA 2000; 34. Morrison RS, Magaziner J, McLaughlin page. (Accessed April 21, 2004, at http://
284:2502-7. MA, et al. The impact of post-operative pain www.capc.org.)
17. Fallowfield L, Jenkins V, Farewell V, Saul on outcomes following hip fracture. Pain 52. Finlay IG, Higginson IJ, Goodwin DM,
J, Duffy A, Eves R. Efficacy of a Cancer Re- 2003;103:303-11. et al. Palliative care in hospital, hospice, at
search UK communication skills training 35. Foley KM. Advances in cancer pain. home: results from a systematic review. Ann
model for oncologists: a randomised con- Arch Neurol 1999;56:413-7. Oncol 2002;13:Suppl 4:257-64.
trolled trial. Lancet 2002;359:650-6. 36. AGS Panel on Persistent Pain in Older 53. Smith TJ, Coyne P, Cassel B, Penberthy
18. Harvard Medical School Center for Pal- Persons. The management of persistent L, Hopson A, Hager MA. A high-volume
liative Care. Practical aspects in palliative pain in older persons. J Am Geriatr Soc specialist palliative care unit and team may
medicine: integrating palliative care into 2002;50:Suppl:S205-S224. reduce in-hospital end-of-life care costs.
clinical practice. (Accessed April 21, 2004, at 37. Luce JM, Luce JA. Perspectives on care at J Palliat Med 2003;6:699-705.
http://www.hms.harvard.edu/cdi/pallcare.) the close of life: management of dyspnea in 54. West JA, Miller NH, Parker KM, et al.
19. American Academy on Physician and patients with far-advanced lung disease: A comprehensive management system for
Patient. Upcoming courses and meetings. “once I lose it, it’s kind of hard to catch heart failure improves clinical outcomes
(Accessed April 21, 2004, at http://www. it. . . .” JAMA 2001;285:1331-7. and reduces medical resource utilization.
physicianpatient.org/default.htm.) 38. Casarett DJ, Inouye SK. Diagnosis and Am J Cardiol 1997;79:58-63.
20. Singer PA, Martin DK, Kelner M. Quality management of delirium near the end of 55. Wasson J, Gaudette C, Whaley F, Sau-
end-of-life care: patients’ perspectives. JAMA life. Ann Intern Med 2001;135:32-40. vigne A, Baribeau P, Welch HG. Telephone
1999;281:163-8. 39. Strasser F, Bruera ED. Update on ano- care as a substitute for routine clinic follow-
21. Finucane TE, Christmas C, Travis K. rexia and cachexia. Hematol Oncol Clin up. JAMA 1992;267:1788-93.
Tube feeding in patients with advanced de- North Am 2002;16:589-617. 56. Elkan R, Kendrick D, Dewey M, et al. Ef-
mentia: a review of the evidence. JAMA 40. Block SD. Assessing and managing de- fectiveness of home based support for older
1999;282:1365-70. pression in the terminally ill patient. Ann In- people: systematic review and meta-analy-
22. Miles SH, Koepp R, Weber EP. Advance tern Med 2000;132:209-18. sis. BMJ 2001;323:719-25.
end-of-life treatment planning: a research 41. Regnard C, Comiskey M. Nausea and 57. Mukamel DB, Bajorska A, Temkin-
review. Arch Intern Med 1996;156:1062-8. vomiting in advanced cancer — a flow dia- Greener H. Health care services utilization
23. Hammes BJ, Rooney BL. Death and end- gram. Palliat Med 1992;6:146-51. at the end of life in a managed care program
of-life planning in one midwestern commu- 42. McClain CS, Rosenfeld B, Breitbart W. integrating acute and long-term care. Med
nity. Arch Intern Med 1998;158:383-90. Effect of spiritual well-being on end-of-life Care 2002;40:1136-48.
24. Morrison RS, Meier DE. High rates of ad- despair in terminally-ill cancer patients. 58. Eng C, Pedulla J, Eleazer GP, McCann R,
vance care planning in New York City’s elder- Lancet 2003;361:1603-7. Fox N. Program of All-Inclusive Care for the
ly. Arch Intern Med (in press). 43. Stroebe MS, Stroebe W. The mortality of Elderly (PACE): an innovative model of inte-
25. Teno J, Lynn J, Wenger N, et al. Advance bereavement: a review. In: Stroebe MS, grated geriatric care and financing. J Am
directives for seriously ill hospitalized pa- Stroebe W, Hansson RO, eds. Handbook of Geriatr Soc 1997;45:223-32.
tients: effectiveness with the Patient Self- bereavement: theory, research, and inter- 59. Wieland D, Lamb VL, Sutton SR, et al.
Determination Act and the SUPPORT inter- vention. Cambridge, England: Cambridge Hospitalization in the Program of All-Inclu-
vention. J Am Geriatr Soc 1997;45:500-7. University Press, 1993:175-95. sive Care for the Elderly (PACE): rates, con-
26. Fried TR, Bradley EH, Towle VR, Allore 44. Ehman JW, Ott BB, Short TH, Ciampa comitants, and predictors. J Am Geriatr Soc
H. Understanding the treatment preferenc- RC, Hansen-Flaschen J. Do patients want 2000;48:1373-80. [Erratum, J Am Geriatr
es of seriously ill patients. N Engl J Med physicians to inquire about their spiritual or Soc 2001;49:835.]
2002;346:1061-6. religious beliefs if they become gravely ill? 60. Hughes SL, Weaver FM, Giobbie-Hur-
27. Meier DE, Morrison RS. Autonomy re- Arch Intern Med 1999;159:1803-6. der A, et al. Effectiveness of team-managed
considered. N Engl J Med 2002;346:1087-9. 45. Mittelman MS, Ferris SH, Shulman E, home-based primary care: a randomized
28. Doyle D, Hanks GW, Cherny NI, Cal- Steinberg G, Levin B. A family intervention multicenter trial. JAMA 2000;284:2877-85.
man K. Oxford textbook of palliative medi- to delay nursing home placement of patients 61. The National Comprehensive Cancer
cine. 3rd ed. Oxford, England: Oxford Uni- with Alzheimer disease: a randomized con- Network. Guidelines for supportive care.
versity Press, 2004. trolled trial. JAMA 1996;276:1725-31. (Accessed April 21, 2004, at http://www.
29. TIME: Toolkit of Instruments to Mea- 46. Mittelman MS, Ferris SH, Shulman E, et nccn.org/physician_gls/f_guidelines.html.)
sure End of life care. (Accessed April 21, al. A comprehensive support program: effect 62. The National Consensus Project for
2004, at http://www.chcr.brown.edu/pcoc/ on depression in spouse-caregivers of AD Quality Palliative Care (NCP) home page.
toolkit.htm.) patients. Gerontologist 1995;35:792-802. (Accessed April 21, 2004, at http://www.
30. Morrison RS, Meier DE. Geriatric pallia- 47. Stroebe MS, Stroebe W, Hansson RO. nationalconsensusproject.org.)
tive care. New York: Oxford University Press, Handbook of bereavement: theory, re- Copyright © 2004 Massachusetts Medical Society.
2003. search, and intervention. Cambridge, En-
31. Bernabei R, Gambassi G, Lapane K, et al. gland: Cambridge University Press, 1993.
2590 n engl j med 350;25 www.nejm.org june 17 , 2004
The New England Journal of Medicine
Downloaded from www.nejm.org on November 22, 2010. For personal use only. No other uses without permission.
Copyright © 2004 Massachusetts Medical Society. All rights reserved.
You might also like
- Achieving Cultural Competency: A Case-Based Approach to Training Health ProfessionalsFrom EverandAchieving Cultural Competency: A Case-Based Approach to Training Health ProfessionalsNo ratings yet
- Lessons You Can Learn From Fitness Classes: 'This Book Below Will Show You Exactly What You Need To Do To Finally Have All The Skills Required for Optimal Health!'From EverandLessons You Can Learn From Fitness Classes: 'This Book Below Will Show You Exactly What You Need To Do To Finally Have All The Skills Required for Optimal Health!'Rating: 5 out of 5 stars5/5 (1)
- Forced-To-Care Nanako Glenn PDFDocument269 pagesForced-To-Care Nanako Glenn PDFEli SaNo ratings yet
- Hospitalist Program Toolkit: A Comprehensive Guide to Implementation of Successful Hospitalist ProgramsFrom EverandHospitalist Program Toolkit: A Comprehensive Guide to Implementation of Successful Hospitalist ProgramsNo ratings yet
- Survival Manual for Elders: Encouraging Elders' Resiliency PotentialFrom EverandSurvival Manual for Elders: Encouraging Elders' Resiliency PotentialNo ratings yet
- Lesson 1Document8 pagesLesson 1Random RandomNo ratings yet
- Understanding end-of-life care for individuals with dementiaDocument5 pagesUnderstanding end-of-life care for individuals with dementiaBlaize JonesNo ratings yet
- Corona Virus: Information You Need and How to Protect Yourself and Your Fellow Human BeingsFrom EverandCorona Virus: Information You Need and How to Protect Yourself and Your Fellow Human BeingsNo ratings yet
- FOOT HEALTH FOR THE HOMELESSDocument41 pagesFOOT HEALTH FOR THE HOMELESSLyanne Daisy Duarte-VangNo ratings yet
- Game of Life Chances Instruction BookletDocument20 pagesGame of Life Chances Instruction BookletcloseandremoteNo ratings yet
- Hospice and End of Life Care PaperDocument6 pagesHospice and End of Life Care Paperapi-570837257No ratings yet
- Medicaid in Long Term CareDocument7 pagesMedicaid in Long Term Carerara100% (1)
- Care at The Time of DeathDocument11 pagesCare at The Time of DeathmultiusosvariadosNo ratings yet
- Draft-Palliative Care Training Manual (CHO)Document168 pagesDraft-Palliative Care Training Manual (CHO)NIYA SHOWNo ratings yet
- The Eleventh HourDocument14 pagesThe Eleventh HourJeric IsraelNo ratings yet
- Caring at The End of Life - Approaching Death - NCBI Bookshelf PDFDocument18 pagesCaring at The End of Life - Approaching Death - NCBI Bookshelf PDFBelaislam Belaulama100% (1)
- End-of-Life Care For The Newly Licensed Practical Nurse: State of Nebraska Transition GrantDocument8 pagesEnd-of-Life Care For The Newly Licensed Practical Nurse: State of Nebraska Transition GrantGee YorkNo ratings yet
- Aged Care QuestionsDocument9 pagesAged Care QuestionsElie RizkNo ratings yet
- Grief Process and Coping with DeathDocument33 pagesGrief Process and Coping with DeathRajaNo ratings yet
- OWL at Purdue University Printable Handouts Using American Psychological Association (APA) FormatDocument28 pagesOWL at Purdue University Printable Handouts Using American Psychological Association (APA) Formatrryan100% (3)
- Kerala's Palliative Care Policy ObjectivesDocument33 pagesKerala's Palliative Care Policy Objectivesjajaja hshsjsNo ratings yet
- 1 Emotional Labor and Organizational Emotional CareDocument29 pages1 Emotional Labor and Organizational Emotional CareCarola GonzálezNo ratings yet
- HOSPICE CARE: A TEAM APPROACH TO COMPASSIONATE END-OF-LIFE CAREDocument7 pagesHOSPICE CARE: A TEAM APPROACH TO COMPASSIONATE END-OF-LIFE CAREJason SteelNo ratings yet
- The Imprtance of End of Life Care in Nursing Home Settings Is Not Diminished by A DisasterDocument14 pagesThe Imprtance of End of Life Care in Nursing Home Settings Is Not Diminished by A DisasterIrfan FauziNo ratings yet
- Role of OT in End of Life CareDocument13 pagesRole of OT in End of Life Carekori holubNo ratings yet
- Palliative Care: Mrs. Grace Lydia Asst - Professor OacnDocument133 pagesPalliative Care: Mrs. Grace Lydia Asst - Professor OacnSophia Alexa Cassandra AlcantaraNo ratings yet
- Trainin On Compassionate, Respectful and Caring Health ProfessionalsDocument21 pagesTrainin On Compassionate, Respectful and Caring Health ProfessionalsnibretzwNo ratings yet
- Chapter 4 Palliative CareDocument21 pagesChapter 4 Palliative CareEINSTEIN2DNo ratings yet
- Home Care: Caring For The Sick at HomeDocument7 pagesHome Care: Caring For The Sick at HomeAris KurniawanNo ratings yet
- Client Care Worksheet For Companion AideDocument4 pagesClient Care Worksheet For Companion Aideapi-282865731No ratings yet
- Activities of Daily Living Checklist and AssessmentsDocument7 pagesActivities of Daily Living Checklist and AssessmentsFitriana WarliatyNo ratings yet
- Palliative Care Guidelines-20 November2013Document69 pagesPalliative Care Guidelines-20 November2013Olga ŢiuNo ratings yet
- End-Of-Life Decision Making Across CulturesDocument15 pagesEnd-Of-Life Decision Making Across CulturesPamNo ratings yet
- Ibs (Conceptmap)Document4 pagesIbs (Conceptmap)Carly Beth Caparida LangerasNo ratings yet
- Facing DeathDocument188 pagesFacing DeathFrancisco MartinezNo ratings yet
- Quality of LifeDocument13 pagesQuality of Lifeapi-35009285075% (4)
- CGAtoolDocument17 pagesCGAtoolGlory Anne Joy WillyNo ratings yet
- Palliative CareDocument8 pagesPalliative Careapi-402433242No ratings yet
- FinalintegrativereviewDocument17 pagesFinalintegrativereviewapi-346349076No ratings yet
- Reflection About Palliative Care and End of Life CareDocument5 pagesReflection About Palliative Care and End of Life CareVILLEJO JHOVIALENNo ratings yet
- Reiki Therapy Reduces HypertensionDocument34 pagesReiki Therapy Reduces HypertensionYayu AlawiiahNo ratings yet
- Nurse Involvement in End of Life DecisionDocument4 pagesNurse Involvement in End of Life Decisiontri hardaniNo ratings yet
- SBAR ToolkitDocument48 pagesSBAR ToolkitRidwan Ari AntoNo ratings yet
- Research in Palliative Care PresentationDocument20 pagesResearch in Palliative Care PresentationNICKY SAMBONo ratings yet
- End of Life CareDocument11 pagesEnd of Life CareBelindaNo ratings yet
- Atlas Palliative Care in Europe 2013 PDFDocument410 pagesAtlas Palliative Care in Europe 2013 PDFeduard rusuNo ratings yet
- Integrating Palliative Care and Hospice Services in Long Term Care: An Eightfold Path Health Policy AnalysisDocument8 pagesIntegrating Palliative Care and Hospice Services in Long Term Care: An Eightfold Path Health Policy AnalysisIJPHSNo ratings yet
- Pilot Project ReportDocument26 pagesPilot Project ReportInclusionNorthNo ratings yet
- RPN Home Health Care Resume 2018Document5 pagesRPN Home Health Care Resume 2018api-436304259100% (1)
- Rns Can Work in A Variety of Healthcare Settings, IncludingDocument6 pagesRns Can Work in A Variety of Healthcare Settings, IncludingpriyagerardNo ratings yet
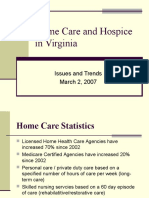
- Home Care and Hospice Trends in VirginiaDocument12 pagesHome Care and Hospice Trends in Virginiarismawati rizalNo ratings yet
- Cure Palliative 1Document64 pagesCure Palliative 1Mr. LNo ratings yet
- Original EssayDocument3 pagesOriginal EssayAj AquinoNo ratings yet
- Analisis Jurnal End of Life-Tedi&saidDocument5 pagesAnalisis Jurnal End of Life-Tedi&saidYulia JuniartiNo ratings yet
- An Electrophysiological Severity Scale in Tarsal Tunnel SyndromeDocument6 pagesAn Electrophysiological Severity Scale in Tarsal Tunnel SyndromeNadewdewNo ratings yet
- Ondansetron vs Domperidone for Acute Gastroenteritis in ChildrenDocument1 pageOndansetron vs Domperidone for Acute Gastroenteritis in ChildrenIntan Winta PratiwiNo ratings yet
- Psi Kia Tri JournalDocument11 pagesPsi Kia Tri JournalRiris SihotangNo ratings yet
- Singh 2012Document6 pagesSingh 2012NadewdewNo ratings yet
- CONSORT 2010 Checklist of Information To Include When Reporting A Randomised TrialDocument2 pagesCONSORT 2010 Checklist of Information To Include When Reporting A Randomised TrialIntan Winta PratiwiNo ratings yet
- Update On Diarrhea 2016Document12 pagesUpdate On Diarrhea 2016sanlupinNo ratings yet
- Tonsil Anatomy Review PDFDocument3 pagesTonsil Anatomy Review PDFElisabethLisyeKonnyNo ratings yet
- RTC-SW 2014 10 P Anaemia in Pregnancy GuidelineDocument5 pagesRTC-SW 2014 10 P Anaemia in Pregnancy GuidelineShiina LeeNo ratings yet
- HisterektomiDocument21 pagesHisterektomiVenny MelindaNo ratings yet
- S1 Text Definitions of Acute Gastroenteritis and VomitingDocument1 pageS1 Text Definitions of Acute Gastroenteritis and VomitingIntan Winta PratiwiNo ratings yet
- SalerioDocument28 pagesSalerioRizqaFebrilianyNo ratings yet
- Jurnal ReadingDocument3 pagesJurnal ReadingNadewdewNo ratings yet
- Guideline 9 3 2 March 2014Document4 pagesGuideline 9 3 2 March 2014Reza AnwarNo ratings yet
- Pediatric DosageDocument10 pagesPediatric DosageNadewdewNo ratings yet
- Nice 14105Document16 pagesNice 14105nevermore11No ratings yet
- RagozineDocument28 pagesRagozineMoisés MedinaNo ratings yet
- Unsaved Preview Document 3Document6 pagesUnsaved Preview Document 3NadewdewNo ratings yet
- DTSCH Arztebl Int-114-0757Document20 pagesDTSCH Arztebl Int-114-0757NadewdewNo ratings yet
- Jurnal Disfagia LagiDocument8 pagesJurnal Disfagia LagiNadewdewNo ratings yet
- SalerioDocument28 pagesSalerioRizqaFebrilianyNo ratings yet
- Isw Wan To',: Pola Pencarian Pengobatan D L Indonesia Analisis Data SusenasDocument15 pagesIsw Wan To',: Pola Pencarian Pengobatan D L Indonesia Analisis Data SusenasNadewdewNo ratings yet
- Notulen RapatDocument13 pagesNotulen RapatNadewdewNo ratings yet
- Clinical Features of Hhs Dka1Document1 pageClinical Features of Hhs Dka1NadewdewNo ratings yet
- Colorful insights into mental wellnessDocument4 pagesColorful insights into mental wellnessJonrheym RemegiaNo ratings yet
- Knowledge Regarding Contraceptive Methods Among Married Women of Reproductive Age GroupDocument3 pagesKnowledge Regarding Contraceptive Methods Among Married Women of Reproductive Age GroupIJAR JOURNALNo ratings yet
- Chairside Diagnostic Kit - Dr. PriyaDocument25 pagesChairside Diagnostic Kit - Dr. PriyaDr. Priya PatelNo ratings yet
- E. coli Myths vs Facts GuideDocument5 pagesE. coli Myths vs Facts GuideRhea CabillaNo ratings yet
- Antepartum HemorrhageDocument3 pagesAntepartum Hemorrhagenur1146No ratings yet
- Physical Fitness TestDocument33 pagesPhysical Fitness Testdeepuphysio100% (1)
- Jurnal Utama Kelompok 1 (Position in Labour)Document9 pagesJurnal Utama Kelompok 1 (Position in Labour)retnoNo ratings yet
- What Is ExerciseDocument3 pagesWhat Is ExerciseJehada AbdukadilNo ratings yet
- White Paper: On Joint ReplacementDocument144 pagesWhite Paper: On Joint ReplacementCosme MejiaNo ratings yet
- Reading Hospital Discharge PlanningDocument1 pageReading Hospital Discharge PlanningAthiaNo ratings yet
- ValuCare University of Santo Tomas Hospital Plan Coordinators and SpecialistsDocument2 pagesValuCare University of Santo Tomas Hospital Plan Coordinators and SpecialistsAnonymous HH3c17osNo ratings yet
- Functions of Parotid GlandDocument32 pagesFunctions of Parotid GlandAsline JesicaNo ratings yet
- 2012conference Detailedschedule2Document4 pages2012conference Detailedschedule2api-171700653No ratings yet
- Intensive-Care Unit: TypesDocument2 pagesIntensive-Care Unit: TypesRavi KantNo ratings yet
- Progyluton-26 1DDocument16 pagesProgyluton-26 1DUsma aliNo ratings yet
- Nursing Career Ladder System in Indonesia The Hospital ContextDocument9 pagesNursing Career Ladder System in Indonesia The Hospital Contextners edisapNo ratings yet
- JensenDocument19 pagesJensencarol colmenaresNo ratings yet
- Neonatal Asphyxia PresentationDocument10 pagesNeonatal Asphyxia PresentationGrae TaclobNo ratings yet
- Family Nursing and Home NursingDocument35 pagesFamily Nursing and Home NursingSamjhana Neupane100% (1)
- Case Study DM 2 PWDTDocument8 pagesCase Study DM 2 PWDTsantis_8No ratings yet
- DiabetesDocument515 pagesDiabetesPaola Rivera DiazNo ratings yet
- Preparation of Nurses To Disaster ManagementDocument10 pagesPreparation of Nurses To Disaster Managementai nisa hasnasariNo ratings yet
- Carboprost Drug StudyDocument3 pagesCarboprost Drug StudyAjay SupanNo ratings yet
- 12 - Terapia Pulpar para Dientes Primarios y Permanentes JovenesDocument4 pages12 - Terapia Pulpar para Dientes Primarios y Permanentes JovenesJeanNo ratings yet
- Soa New DocumentsDocument1 pageSoa New Documentsjhoy visitacionNo ratings yet
- Cintya - Jurnal SDHDocument6 pagesCintya - Jurnal SDHCintya Dyah ayu SNo ratings yet
- INTL ARRIVALSDocument9 pagesINTL ARRIVALSKoushik SekharNo ratings yet
- ENdo FellowshipDocument2 pagesENdo FellowshipAli FaridiNo ratings yet
- 1.maternal and Child Health NursingDocument33 pages1.maternal and Child Health NursingBhie Bhie100% (1)
- TP-L3-402 Nursing Admin Checklist 5.1Document2 pagesTP-L3-402 Nursing Admin Checklist 5.1عبيدة محمد ابو عابدNo ratings yet