Professional Documents
Culture Documents
Postpolio Syndrome
Uploaded by
Johnpeter Esporlas100%(1)100% found this document useful (1 vote)
65 views3 pagesPost polio
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentPost polio
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
100%(1)100% found this document useful (1 vote)
65 views3 pagesPostpolio Syndrome
Uploaded by
Johnpeter EsporlasPost polio
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 3
Post-Poliomyelitis Syndrome (PPS) the course of years.
This leads to distal
degeneration of the motor units and
Definition
worsening denervation, causing clinical
- It is a disorder typically characterized by the symptoms.
gradual onset and slow progression of new - Peripheral disintegration model Commented [JPE1]: Most widely held theory for PPS
weakness, fatigue, and pain in survivors of - Over-sprouting of new axon terminals from surviving
Physical Findings & Clinical Presentation LMNs occur in the immediate
paralytic poliomyelitis after a period of aftermath of the acute paralytic poliomyelitis
partial or complete recovery and many New weakness and atrophy, asymmetrical, - This compensatory distal reinnervation expands the
years of neurologic stability. proximal and slowly progressive in size of motor units and provides effective motor function;
- The symptoms are persistent and cannot be distribution. Occurs in both initially weak and this stabilizes muscle strength for many years.
- However, this extensive nerve sprouting also increases
explained by the presence of other uninvolved muscles.
the metabolic burden of surviving LMNs, so after many
neurologic, medical, or orthopedic Abnormal fatigue: may not be related to years, an un-identified process 1st causes nerve terminal
conditions activity levels, doesn't recover easily with dysfunction presenting as fatigue and then nerve
usual rest periods. terminal disintegration presenting as muscle weakness
Other Names and atrophy.
Pain: myalgia, cramping pain, joint pain with
Post-polio syndrome repetitive injury, hypersensitivities
Decreased function with reduced Commented [JPE2]: Hitting a wall phenomenon/Polio
Progressive post-poliomyelitis muscular wall: lack of energy with minimal activity; occurs primarily in
atrophy endurance for routine activities.
the afternoon
Slow progression, either steady or step-wise Most disabling accompaniment and most debilitating
EPIDEMIOLOGY Environmental cold intolerance symptoms; may affect patient’s cognition & thinking
Brain fatigue-generator model Fatigue occurs commonly in late afternoon/early evening
Gender Atypical Fatigue: Fatigue that last throughout the day
Sleep disturbances & weakness in respiratory
- Female > Male (Harrison’s Internal Medicine) system
- Depression Commented [JPE3]: Joint pain may d/t wear & tear on
Neurologic examination reveals evidence of joints, poor posture & deterioration of soft-tissue or
Incidence surgeries done to treat the residual effects of polio
asymmetric, lower motor neuron weakness
with or without musculoskeletal deformities Commented [JPE4]: More than 65% of individuals with
- Estimates vary from 22% to 85% of individuals
PPS have reported
who survive acute poliomyelitis secondary to longstanding polio such as
neck, shoulder, and back pain radiating to the hip and leg
asymmetric limb size, kyphoscoliosis, (Umphred)
Peak Incidence degenerative joint disease, and joint
Commented [JPE5]: Difficulty in concentration, memory
instability d/t the use of assistive devices and
- About 30 to 36 years following acute attention; damage in reticular formation, hypothalamus,
wheelchairs for decades dopaminergic neurons
poliomyelitis, although cases have been
Postural abnormalities
reported between 8 and 71 years. Commented [JPE6]: Nocturnal hypoventilation occurs
Less Common Presentation less frequently
Risk Factors
Commented [JPE7]: -Forward head, forward-leaning
Fasciculations
- Increasing age and greater length of time trunk, (-) lumbar curve, uneven pelvis, scoliosis, lateral trunk
Dysphagia shifts
since the episode of acute poliomyelitis
Dysarthria
- Acute poliomyelitis at an older age
- Greater severity of the acute poliomyelitis or Criteria for Diagnosing Post-Poliomyelitis Syndrome
chronic deficits after recovery
- AKA: Halstead-Ross Criteria
Pathology - Hx of polio
- recovery period & neurological stability at
- Loss of the anterior horn cell
least 15 years
Etiology - Onset of >2 S/Sx:
fatigue,
- unknown; possible hyperfunctioning of mm/joint pain
motor neurons, long-term overuse at high weakness & atrophy in new mm,
levels resulting in new denervation functional loss
(Siegelman) cold intolerance
- The most popular hypothesis is - persistent S/Sx for 1 yr.
that the reduced population of enlarged - Rule out other diagnosis
motor units after acute poliomyelitis is
subject to increased stress and overuse over
- any sensory deficit is due to other etiology
(sensation is unaffected in PPS).
Ancillary Procedure
6. Respiratory Function
1. Nerve Conduction Velocity (NCV) - Examine for dyspnea, difficulty in speaking
- SNAP: Normal and weak cough
- CMAP: Abnormal (Low maximum CMAP 7. Aerobic Capacity
amplitudes) - use ergometer that involves both upper and
2. EMG lower extremities; e.g., Schwinn Air-Dyne,
- Abnormal activity discontinuous protocoL submaximal test
- Delayed Recruitment (ACSM recommendation)
- (+)Giant motor neuron unit, may indicative
Drugs
of chronic denervation and reinnervation
- Fasciculations can be unusually coarse and - There are no specific drugs to treat Post-
large in keeping with the giant motor units polio syndrome
detectable a. Anti-depressants
3. Low Rate Repetitive Stimulation (LRRS) - e.g., amitriptyline (Elavil), fluoxetine (Prozac)
- Normal activity b. Neurotransmitters inhibitors
4. SFEMG (Single Fiber EMG) - decreases fatigue and sleep disorders; e.g.,
- Increased jitter, fiber density and blocking serotonin, norepinephrine
5. Muscle Biopsy
- usually shows acute and chronic
neurogenic atrophy and often marked PT GOALS, OUTCOMES
group muscle fiber atrophy and fiber type
grouping 1. Maintain respiratory function
- Teach breathing exercises, supportive
Lab Exam cough maneuvers, postural drainage as
indicated
1. CBC, Electrolytes, Thyroid Function Test
2. Teach energy conservation techniques,
- To rule out other cause of fatigue
activity pacing: balance activity with
- Typically normal
frequent rest periods to decrease fatigue,
2. Erythrocyte Sedimentation Rate (ESR)
prevent overwork damage in weakened,
- Normal
denervated muscle.
- To rule out auto-immune disorders
- Teach relaxation techniques to maximize
- Increase Creatine-Kinase
rest
Examination - Avoid unnecessary activities to maximize
important work.
1. History
3. Preserve or increase muscle strength
- confirm original acute polio illness;
- Provide moderate exercise program (non-
document onset of present symptoms,
exhaustive exercise): modified strengthening
presentation, course, chronology.
and conditioning; use low-intensity,
2. Motor: strength, atrophy, muscle
discontinuous non-fatiguing exercise with
fatigue, muscle twitching and cramps
increased rest periods.
- strength, atrophy, muscle fatigue, muscle
- Caution against widespread use of strength
twitching and cramps
training, it may trigger fatigue
- Identify functional contractions (fair grades
- Consider pool programs: minimizes overwork Commented [JPE8]: Aquatic exercise can be very
or above)
relieves pain; general body conditioning beneficial because water decreases the stress on the joints,
- Look for spotty involvement, asymmetrical
4. Aerobic Conditioning bones, and muscles.
paralysis
- moderate to low-level training depending
3. ROM & Deformity
upon class of disease, discontinuous
4. Pain
protocol. In severe atrophic polio, exercise is
- Muscle pain: check tenderness to touch
contraindicated
- Skeletal, soft tissue pain: chronic overuse or
5. Maintain or increase function
poor alignment
5. Sensory function
- provide recommendations for lifestyle
modification; minimize abnormal postures,
gait deviations.
6. Prescribe appropriate orthoses, mobility aids Commented [JPE9]: The most frequently prescribed
(motorized cart), assistive devices, orthoses include
environmental modifications shoe lifts, AFOs (rocker bottom) and KAFOs.
7. Eliminate or control pain: provide options for
pain controL foster self-control
8. Teach patient and family all care, activities
of daily living; lifestyle modifications
9. Provide psychological support and
reassurance
You might also like
- B. The Contrecoup Injury Occurs Directly Opposite To The Point of ImpactDocument4 pagesB. The Contrecoup Injury Occurs Directly Opposite To The Point of ImpactJohnpeter EsporlasNo ratings yet
- Amyotrophic Lateral SclerosisDocument3 pagesAmyotrophic Lateral SclerosisJohnpeter EsporlasNo ratings yet
- Parables of Jesus ChristDocument4 pagesParables of Jesus ChristJohnpeter EsporlasNo ratings yet
- Mes 3Document4 pagesMes 3Johnpeter EsporlasNo ratings yet
- Assistive Devices RealDocument3 pagesAssistive Devices RealJohnpeter EsporlasNo ratings yet
- Achalasia: Proximal Dysphagia Due To Neuromuscular Cause Distal Dysphagia Due To Mechanical ObstructionDocument10 pagesAchalasia: Proximal Dysphagia Due To Neuromuscular Cause Distal Dysphagia Due To Mechanical ObstructionJohnpeter EsporlasNo ratings yet
- Bible FactsDocument28 pagesBible FactsJohnpeter EsporlasNo ratings yet
- Bell's PalsyDocument9 pagesBell's PalsyJohnpeter EsporlasNo ratings yet
- Pediatric Milestones Age Gross Motor Fine Motor Personal/Social Speech and LanguageDocument3 pagesPediatric Milestones Age Gross Motor Fine Motor Personal/Social Speech and LanguageJohnpeter EsporlasNo ratings yet
- Tep 11 Reflexes PrintoutDocument2 pagesTep 11 Reflexes PrintoutJohnpeter EsporlasNo ratings yet
- ReviewDocument10 pagesReviewJohnpeter EsporlasNo ratings yet
- Electrotherapy Parameters For Grand PraxDocument3 pagesElectrotherapy Parameters For Grand PraxJohnpeter EsporlasNo ratings yet
- Introduction To PharmacologyDocument6 pagesIntroduction To PharmacologyJohnpeter EsporlasNo ratings yet
- KneeDocument14 pagesKneeJohnpeter Esporlas100% (1)
- Immob Med BackDocument14 pagesImmob Med BackJohnpeter EsporlasNo ratings yet
- TEP 2, Thera Ex 1 and Physiology 2 SyllabusDocument2 pagesTEP 2, Thera Ex 1 and Physiology 2 SyllabusJohnpeter EsporlasNo ratings yet
- Patient Survey: Step 1 - Group Formation and ProfilesDocument6 pagesPatient Survey: Step 1 - Group Formation and ProfilesJohnpeter EsporlasNo ratings yet
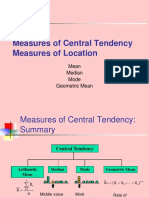
- Central TendencyDocument25 pagesCentral TendencyJohnpeter EsporlasNo ratings yet
- Neuroanatomy Pictures Part 2 - WaxmanDocument6 pagesNeuroanatomy Pictures Part 2 - WaxmanJohnpeter EsporlasNo ratings yet
- Chapter 12Document22 pagesChapter 12John EmmanuelNo ratings yet
- 1st Lecture Sir JomaDocument7 pages1st Lecture Sir JomaJohnpeter EsporlasNo ratings yet
- CBR Topic Outline 2017-2018Document3 pagesCBR Topic Outline 2017-2018Johnpeter EsporlasNo ratings yet
- CVA - Compilation of All BooksDocument4 pagesCVA - Compilation of All BooksJohnpeter EsporlasNo ratings yet
- Atlas of Digestive SystemDocument3 pagesAtlas of Digestive SystemJohnpeter EsporlasNo ratings yet
- Normal Body TemperaturesDocument5 pagesNormal Body TemperaturesJohnpeter EsporlasNo ratings yet
- Anthropometric SDocument3 pagesAnthropometric SJohnpeter EsporlasNo ratings yet
- Down SyndromeDocument2 pagesDown SyndromeJohnpeter EsporlasNo ratings yet
- Cardiovascular RehabilitationDocument5 pagesCardiovascular RehabilitationJohnpeter EsporlasNo ratings yet
- Etiology, Epidemiology & Differential Diagnosis For CADDocument9 pagesEtiology, Epidemiology & Differential Diagnosis For CADJohnpeter EsporlasNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- N118 0XYGEN Checklist FinalDocument7 pagesN118 0XYGEN Checklist FinalAmandaNo ratings yet
- Quiz 2Document3 pagesQuiz 2air france bargamentoNo ratings yet
- Stress Management OutlineDocument7 pagesStress Management OutlineJericko Allen Resus100% (1)
- Speech Contest - Stunting in Indonesia2Document2 pagesSpeech Contest - Stunting in Indonesia2Hermawan ChenNo ratings yet
- Example of Health GenogramDocument1 pageExample of Health Genogramapi-322059527No ratings yet
- These Are The Characteristics of The K To 12 Health CurriculumDocument2 pagesThese Are The Characteristics of The K To 12 Health CurriculumKe An U100% (7)
- REGO ET EL TQUK Assessment Syllabus 5-15-2023Document41 pagesREGO ET EL TQUK Assessment Syllabus 5-15-2023Itz Lovaboi ChurchillNo ratings yet
- Swadesh FoundationDocument8 pagesSwadesh FoundationKunal RajNo ratings yet
- REFERENCEDocument2 pagesREFERENCErodolfo opidoNo ratings yet
- Review Related LiteratureDocument3 pagesReview Related LiteraturerdsamsonNo ratings yet
- Reynolds Child Depression Scale ArticleDocument9 pagesReynolds Child Depression Scale ArticleColette MeeNo ratings yet
- Livelihood Sustainabilityof Street Vendors AStudyin Dhaka CityDocument8 pagesLivelihood Sustainabilityof Street Vendors AStudyin Dhaka CityNathaniel PohNo ratings yet
- Nhóm 3 - For MergeDocument5 pagesNhóm 3 - For Mergetrongphap.0203No ratings yet
- Pembukaan Survei Pendampingan Akreditasi Rsu Permata Bunda - GroboganDocument14 pagesPembukaan Survei Pendampingan Akreditasi Rsu Permata Bunda - GroboganAli MuhsonNo ratings yet
- Final - 2022 Nutrition Month PresentationDocument44 pagesFinal - 2022 Nutrition Month PresentationRaynaldo Jr. Del ValleNo ratings yet
- Gianna Graziani Cover LetterDocument1 pageGianna Graziani Cover Letterapi-733890262No ratings yet
- The Concept of Value AdditionDocument5 pagesThe Concept of Value AdditionNura BasmerNo ratings yet
- Benedict James Roldan BermasDocument4 pagesBenedict James Roldan BermasBenedict James BermasNo ratings yet
- Resume - 2022 07 03 095726Document4 pagesResume - 2022 07 03 095726Nessa LarrierNo ratings yet
- Answer No 3-EditedDocument2 pagesAnswer No 3-EditedAlb AklbNo ratings yet
- Hospital Team Match These Following Jobs Below With Their Definition A B ADocument2 pagesHospital Team Match These Following Jobs Below With Their Definition A B AIlhamNo ratings yet
- ElephantiasisDocument21 pagesElephantiasisPutri Anena AyuNo ratings yet
- Breast CA SeminarDocument60 pagesBreast CA SeminarAliyi MuktarNo ratings yet
- Miraculous Self Healing Homoeopathic Principals Therapeutics Materia Medica Ajit Singh Barn.05633 2foreword PrefaceDocument8 pagesMiraculous Self Healing Homoeopathic Principals Therapeutics Materia Medica Ajit Singh Barn.05633 2foreword PrefacemoumonaNo ratings yet
- Medicine - IJGMP - HUMAN IMMUNO DEFFICIENCY - Adetunji Oladeni Adeniji - NigeriaDocument10 pagesMedicine - IJGMP - HUMAN IMMUNO DEFFICIENCY - Adetunji Oladeni Adeniji - Nigeriaiaset123No ratings yet
- Allergo-Immunology Hour: Food AllergyDocument32 pagesAllergo-Immunology Hour: Food AllergyJill PNo ratings yet
- Full Download Health Safety and Nutrition For The Young Child 9th Edition Marotz Test BankDocument26 pagesFull Download Health Safety and Nutrition For The Young Child 9th Edition Marotz Test Bankretainalgrainascjy100% (37)
- BENEFITS and Advantages of Love Moon Anion Sanitary NapkinsDocument3 pagesBENEFITS and Advantages of Love Moon Anion Sanitary NapkinsJeamie Janson De GuzmanNo ratings yet
- English: Quarter 2 - Module 1Document12 pagesEnglish: Quarter 2 - Module 1Raquel FranciscoNo ratings yet
- Insomnia: Ola AyeshDocument31 pagesInsomnia: Ola AyeshSalih TahsinNo ratings yet