Professional Documents
Culture Documents
Asthma Management - Adults
Uploaded by
Itharshan IndreswaranOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Asthma Management - Adults
Uploaded by
Itharshan IndreswaranCopyright:
Available Formats
ANNEXES
Annex 4
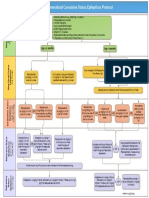
Management of acute severe asthma in adults in hospital
IMMEDIATE TREATMENT
Features of acute severe asthma
Oxygen to maintain SpO2 94-98%
Peak expiratory flow (PEF) 33-50% of Salbutamol 5 mg or terbutaline 10 mg via an oxygen-driven nebuliser
best (use % predicted if recent best Ipratropium bromide 0.5 mg via an oxygen-driven nebuliser
unknown) Prednisolone tablets 40-50 mg or IV hydrocortisone 100 mg
Can’t complete sentences in one breath No sedatives of any kind
Respirations ≥25 breaths/min Chest X ray if pneumothorax or consolidation are suspected or patient
Pulse ≥110 beats/min requires mechanical ventilation
Life threatening features IF LIFE THREATENING FEATURES ARE PRESENT:
Discuss with senior clinician and ICU team
PEF <33% of best or predicted Consider IV magnesium sulphate 1.2-2 g infusion over 20 minutes (unless already
SpO2 <92% given)
Silent chest, cyanosis, or feeble Give nebulised β2 agonist more frequently e.g. salbutamol 5 mg up to every 15-30
respiratory effort minutes or 10 mg per hour via continuous nebulisation (requires special nebuliser)
Arrhythmia or hypotension
Exhaustion, altered consciousness
SUBSEQUENT MANAGEMENT
If a patient has any life threatening feature, IF PATIENT IS IMPROVING continue:
measure arterial blood gases. No other Oxygen to maintain SpO2 94-98%
investigations are needed for immediate Prednisolone 40-50mg daily or IV hydrocortisone 100 mg 6 hourly
management. Nebulised β2 agonist and ipratropium 4-6 hourly
Blood gas markers of a life threatening IF PATIENT NOT IMPROVING AFTER 15-30 MINUTES:
attack: Continue oxygen and steroids
‘Normal’ (4.6-6 kPa, 35-45 mmHg) Use continuous nebulisation of salbutamol at 5-10 mg/hour if an appropriate
PaCO2 nebuliser is available. Otherwise give nebulised salbutamol 5 mg every 15-30
Severe hypoxia: PaO2 <8 kPa minutes
(60mmHg) irrespective of treatment with Continue ipratropium 0.5 mg 4-6 hourly until patient is improving
oxygen
A low pH (or high H+) IF PATIENT IS STILL NOT IMPROVING:
Discuss patient with senior clinician and ICU team
Caution: Patients with severe or life Consider IV magnesium sulphate 1.2-2 g over 20 minutes (unless already given)
threatening attacks may not be distressed Senior clinician may consider use of IV β2 agonist or IV aminophylline or
and may not have all these abnormalities. progression to mechanical ventilation
The presence of any should alert the doctor.
Near fatal asthma MONITORING
Raised PaCO2
Requiring mechanical ventilation with Repeat measurement of PEF 15-30 minutes after starting treatment
raised inflation pressures Oximetry: maintain SpO2 >94-98%
Repeat blood gas measurements within 1 hour of starting treatment if:
- initial PaO2 <8 kPa (60 mmHg) unless subsequent SpO2 >92%
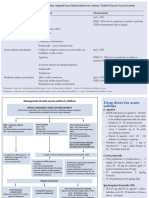
Peak Expiratory Flow Rate - Normal Values - PaCO2 normal or raised
- patient deteriorates
680
Chart PEF before and after giving β2 agonists and at least 4 times daily throughout
hospital stay
660
640
620
600 Transfer to ICU accompanied by a doctor prepared to intubate if:
580 Deteriorating PEF, worsening or persisting hypoxia, or hypercapnea
560
Exhaustion, altered consciousness
540
Poor respiratory effort or respiratory arrest
PEF (l/min) EU Scale
520
500
480 Height
460
Men
190 cm (75 in) DISCHARGE
440
183 cm (72 in)
175 cm (69 in)
420 167 cm (66 in)
160 cm (63 in)
When discharged from hospital, patients should have:
400
Been on discharge medication for 12-24 hours and have had inhaler technique
380
360
checked and recorded
Height
340 Women PEF >75% of best or predicted and PEF diurnal variability<25% unless discharge is
183 cm (72 in)
320 175 cm (69 in)
167 cm (66 in)
agreed with respiratory physician
300
15 20 25 30 35 40 45 50 55 60 65 70 75 80
160 cm (63 in)
85 152 cm (60 in)
Treatment with oral and inhaled steroids in addition to bronchodilators
Age (years) Own PEF meter and written asthma action plan
Adapted by Clement Clarke for use with EN13826 / EU scale peak flow meters
from Nunn AJ Gregg I, Br Med J 1989:298;1068-70
GP follow up arranged within 2 working days
Follow up appointment in respiratory clinic within 4 weeks
Patients with severe asthma (indicated by need for admission) and adverse behavioural
or psychosocial features are at risk of further severe or fatal attacks
Determine reason(s) for exacerbation and admission
Send details of admission, discharge and potential best PEF to GP
113
You might also like
- Special 13 BTS SIGN AsthmaDocument1 pageSpecial 13 BTS SIGN AsthmacositaamorNo ratings yet
- Managing Acute Asthma in Adults - Final160123Document1 pageManaging Acute Asthma in Adults - Final160123Stri LokaNo ratings yet
- AsthmaDocument2 pagesAsthmaAndrei MurariuNo ratings yet
- Management Acute AsthmaDocument1 pageManagement Acute AsthmaMassimo Di BenedettoNo ratings yet
- Keep The Airway Open: Head-DownDocument1 pageKeep The Airway Open: Head-DownzenalNo ratings yet
- Anaph 5Document7 pagesAnaph 5Aprilihardini Laksmi100% (1)
- Anaphylaxis Anaphylactoid ReactionDocument8 pagesAnaphylaxis Anaphylactoid Reactionsringeri2No ratings yet
- Anaphylactic ShockDocument1 pageAnaphylactic ShockAskar ArasNo ratings yet
- 03 SMI Eclampsia Checklist July 2017Document1 page03 SMI Eclampsia Checklist July 2017piano543100% (1)
- Hypertensive Emergency Checklist: Safe Motherhood InitiativeDocument1 pageHypertensive Emergency Checklist: Safe Motherhood InitiativeazimaNo ratings yet
- Seven Ps For RSI BOARDDocument2 pagesSeven Ps For RSI BOARDJames BrownNo ratings yet
- RBCH - PHT Aminophylline Loading Dose GuidelinesDocument2 pagesRBCH - PHT Aminophylline Loading Dose GuidelinesAdrian PrasetioNo ratings yet
- Prescriptions On Asthma & APDDocument9 pagesPrescriptions On Asthma & APDeesha shahNo ratings yet
- 19sm02a170703EclampsiaCheck1 PDFDocument1 page19sm02a170703EclampsiaCheck1 PDFazimaNo ratings yet
- CH 8Document12 pagesCH 8Олександр РабошукNo ratings yet
- 038 AnaphylaxisDocument5 pages038 AnaphylaxisabbuahmedibbuNo ratings yet
- Dosis Ketamin Dan Xylazine RabbitDocument1 pageDosis Ketamin Dan Xylazine RabbitRais RyuzakiNo ratings yet
- Brief Outline Questions To Ask: Acute AsthmaDocument15 pagesBrief Outline Questions To Ask: Acute AsthmaLevina AudreyNo ratings yet
- Postpartum Preeclampsia Checklist: SafemotherhoodinitiativeDocument1 pagePostpartum Preeclampsia Checklist: SafemotherhoodinitiativeazimaNo ratings yet
- Contrast Reaction Card AdultDocument2 pagesContrast Reaction Card AdultJenniffer FlorenciaNo ratings yet
- UNC ED Pediatric Asthma Protocol 1-29-15 KJRDocument2 pagesUNC ED Pediatric Asthma Protocol 1-29-15 KJRMax ImousNo ratings yet
- Status EpilepticusDocument4 pagesStatus Epilepticusypk13579No ratings yet
- 6.1 Quick Ref Guide MNGT Antivenom Reactions SGB2021 Ver. 2Document3 pages6.1 Quick Ref Guide MNGT Antivenom Reactions SGB2021 Ver. 2anju sulishaNo ratings yet
- Emergency Parenteral Drugs ListDocument4 pagesEmergency Parenteral Drugs ListRem Remoreras75% (4)
- COVID MX BsmmuDocument2 pagesCOVID MX BsmmuNuhiat NahreenNo ratings yet
- Status AsthmaticusDocument18 pagesStatus AsthmaticusUmar Azlan0% (1)
- Anaphylaxis & Allergic Reactions GuideDocument2 pagesAnaphylaxis & Allergic Reactions Guidemadimadi11No ratings yet
- Management of Convulsions in Pregnancy 3Document29 pagesManagement of Convulsions in Pregnancy 3Monisha ArulalanNo ratings yet
- Adrenaline (Epinephrine) : Is A Directly Acting Sympathomimetic Amine That Is An Agonist of Alpha-AndDocument55 pagesAdrenaline (Epinephrine) : Is A Directly Acting Sympathomimetic Amine That Is An Agonist of Alpha-AndinnyNo ratings yet
- 04 Chapter Respiratory SystemDocument18 pages04 Chapter Respiratory SystemMSKCNo ratings yet
- Anaphylaxis Wallchart 2018Document1 pageAnaphylaxis Wallchart 2018simranNo ratings yet
- Contrast Reaction Card PediatricDocument2 pagesContrast Reaction Card PediatricJenniffer FlorenciaNo ratings yet
- Bagan KejangDocument10 pagesBagan KejangNie' MKNo ratings yet
- Table 1. Essential Emergency DrugsDocument3 pagesTable 1. Essential Emergency DrugsMariel Febreo MerlanNo ratings yet
- AtropinDocument9 pagesAtropinarfitaaaaNo ratings yet
- Guideline 133FM PDFDocument13 pagesGuideline 133FM PDFPangestu DhikaNo ratings yet
- Child With Fits in ED - Srl.Document2 pagesChild With Fits in ED - Srl.azeemNo ratings yet
- Atracurium BesylateDocument3 pagesAtracurium BesylateWidya WidyariniNo ratings yet
- Rapid Tranquilization Treatment FlowchartDocument1 pageRapid Tranquilization Treatment FlowchartKaren C. ManoodNo ratings yet
- ACLS Pocket GuideDocument5 pagesACLS Pocket Guidedragnu100% (1)
- Postpartum Preeclampsia Checklist: Emergency Department ExampleDocument1 pagePostpartum Preeclampsia Checklist: Emergency Department ExamplewijeNo ratings yet
- Acute Wheeze Flowchart PDFDocument2 pagesAcute Wheeze Flowchart PDFgeonMMNo ratings yet
- StatusDocument14 pagesStatusSyeda HaniaNo ratings yet
- EpinephrineDocument4 pagesEpinephrinegovind_soni_15No ratings yet
- Seizures/Epilepsy: Case PersentationDocument14 pagesSeizures/Epilepsy: Case PersentationAbdulmalik AliNo ratings yet
- Age 2 Months Age 2monthsDocument1 pageAge 2 Months Age 2monthsd'Agung NugrohoNo ratings yet
- Acls Algorithms 2012Document12 pagesAcls Algorithms 2012kivuNo ratings yet
- Drug Study: Epinephrine: RecommendedDocument5 pagesDrug Study: Epinephrine: RecommendedShara Lailanie A. AzisNo ratings yet
- StatusEpilepticus Pocket CardDocument2 pagesStatusEpilepticus Pocket CardDiana MihaiNo ratings yet
- Adult and Pediatric Emergency DrugsDocument61 pagesAdult and Pediatric Emergency DrugsYu, Denise Kyla BernadetteNo ratings yet
- Anaesthesia Drugs Used CommonlyDocument6 pagesAnaesthesia Drugs Used CommonlyAmar Mahesh KalluNo ratings yet
- BCCH ED Croup Algorithm 2012Document1 pageBCCH ED Croup Algorithm 2012john morzNo ratings yet
- 7698alorithm SeizureDocument3 pages7698alorithm Seizureboromeus abyasa daniswara100% (1)
- Fentanyl-Intravenous ANMFv4.0 20231012Document5 pagesFentanyl-Intravenous ANMFv4.0 20231012manohar094No ratings yet
- Rapid Sequence Intubation: Dr. Zulkarnain, SpanDocument26 pagesRapid Sequence Intubation: Dr. Zulkarnain, SpanNisa AprianiNo ratings yet
- RFH COVID-19 ICU Resource Pack FULL PDFDocument15 pagesRFH COVID-19 ICU Resource Pack FULL PDFQuique GarciaNo ratings yet
- Peak Expiratory Flow RateDocument35 pagesPeak Expiratory Flow RateLiya RafeekhNo ratings yet
- Fentanyl NeomedDocument3 pagesFentanyl NeomedmuarifNo ratings yet
- PCOS - Summary PDFDocument1 pagePCOS - Summary PDFItharshan IndreswaranNo ratings yet
- Amenorrhea - Algorithm & DifferentialsDocument9 pagesAmenorrhea - Algorithm & DifferentialsItharshan IndreswaranNo ratings yet
- Gastroeneteritis - Pediatrics (Nelson's)Document20 pagesGastroeneteritis - Pediatrics (Nelson's)Itharshan IndreswaranNo ratings yet
- Carcinogens - Carcinogens by Sites of Body (IARC) PDFDocument1 pageCarcinogens - Carcinogens by Sites of Body (IARC) PDFItharshan IndreswaranNo ratings yet
- Asthma (Acute) Management - Children (Pediatrics)Document2 pagesAsthma (Acute) Management - Children (Pediatrics)Itharshan IndreswaranNo ratings yet
- Pharmacology - Anti-Inflammatory Drugs - Corticosteroid, NSAID, Leukotriene (Eicosanoids)Document9 pagesPharmacology - Anti-Inflammatory Drugs - Corticosteroid, NSAID, Leukotriene (Eicosanoids)Itharshan IndreswaranNo ratings yet
- Spirometry Curve Errors Correction PDFDocument1 pageSpirometry Curve Errors Correction PDFItharshan IndreswaranNo ratings yet
- Rash - Severely Ill (Differentials) PDFDocument11 pagesRash - Severely Ill (Differentials) PDFItharshan IndreswaranNo ratings yet
- Bradycardia PDFDocument1 pageBradycardia PDFItharshan IndreswaranNo ratings yet
- Circulatory System - Arterial & Venous TreesDocument28 pagesCirculatory System - Arterial & Venous TreesItharshan IndreswaranNo ratings yet
- Poster2 Arrhythmia Recognition eDocument1 pagePoster2 Arrhythmia Recognition eItharshan IndreswaranNo ratings yet
- Martyrs Park PDFDocument5 pagesMartyrs Park PDFItharshan IndreswaranNo ratings yet
- Asthma Management - AdultsDocument1 pageAsthma Management - AdultsItharshan IndreswaranNo ratings yet
- Abdomen Diagnoses PDFDocument2 pagesAbdomen Diagnoses PDFLaura Lopez RocaNo ratings yet
- Pharmacology - Mnemonics PDFDocument140 pagesPharmacology - Mnemonics PDFItharshan Indreswaran76% (17)
- Cardiovascular Regulation - PhysiologyDocument9 pagesCardiovascular Regulation - PhysiologyItharshan IndreswaranNo ratings yet
- PE - Quizlet - Flash Card (Table)Document6 pagesPE - Quizlet - Flash Card (Table)Itharshan IndreswaranNo ratings yet
- Martyrs ParkDocument6 pagesMartyrs ParkItharshan IndreswaranNo ratings yet
- Pharmacology - Mnemonics PDFDocument140 pagesPharmacology - Mnemonics PDFItharshan Indreswaran76% (17)
- Chapter 22Document14 pagesChapter 22Itharshan IndreswaranNo ratings yet
- Introduction To Chinese Society and CultureDocument5 pagesIntroduction To Chinese Society and CultureItharshan IndreswaranNo ratings yet
- Martyrs Park PDFDocument5 pagesMartyrs Park PDFItharshan IndreswaranNo ratings yet
- Normal Lab Values PDFDocument2 pagesNormal Lab Values PDFItharshan Indreswaran83% (18)
- Classification of Cardiac MurmursDocument1 pageClassification of Cardiac MurmursItharshan IndreswaranNo ratings yet
- Introduction in Human ParasitologyDocument53 pagesIntroduction in Human ParasitologyItharshan IndreswaranNo ratings yet
- Abdominal Aorta SonogramDocument3 pagesAbdominal Aorta SonogramItharshan IndreswaranNo ratings yet
- Pharmacology: For Health Science StudentsDocument211 pagesPharmacology: For Health Science StudentssafibayNo ratings yet
- Pulm 2005 Exam QuestionsDocument32 pagesPulm 2005 Exam QuestionsItharshan IndreswaranNo ratings yet
- General PathologyDocument261 pagesGeneral PathologyHanif SharNo ratings yet
- Oet PDFDocument8 pagesOet PDFMary JisNo ratings yet
- Peritonsillar Abscess in Emergency MedicineDocument14 pagesPeritonsillar Abscess in Emergency Medicinerissa neNo ratings yet
- Barnard 2 Amplitudo AkomodasiDocument7 pagesBarnard 2 Amplitudo AkomodasiBonita AsyigahNo ratings yet
- Pendidikan Pasien Cath LabDocument10 pagesPendidikan Pasien Cath LabAgnesthesiaNo ratings yet
- Lithoskop Product BrochureDocument20 pagesLithoskop Product BrochureJaseel AkNo ratings yet
- Pulse Diagnosis of Chinese MedicineDocument69 pagesPulse Diagnosis of Chinese MedicineYanikdj100% (3)
- ORS Program Book 2015 WebDocument164 pagesORS Program Book 2015 Webaiakoby100% (1)
- Prepaid PlansDocument27 pagesPrepaid PlansDee ReyesNo ratings yet
- Spondilitis TBDocument14 pagesSpondilitis TBaswad 0008No ratings yet
- Intensive & Critical Care NursingDocument7 pagesIntensive & Critical Care NursingFernando PintoNo ratings yet
- Radiotherapy NursingDocument35 pagesRadiotherapy NursingMarlon Rey AnacletoNo ratings yet
- Medical Emergencies in OSDocument62 pagesMedical Emergencies in OSAditi RapriyaNo ratings yet
- Generic MedicinesDocument16 pagesGeneric MedicinesAnn Christine C. ChuaNo ratings yet
- Chronic Lymphocytic Leukemia/ Small Lymphocytic LymphomaDocument84 pagesChronic Lymphocytic Leukemia/ Small Lymphocytic LymphomasimplyrosalynNo ratings yet
- Healthcare ProfessionalismDocument28 pagesHealthcare ProfessionalismAnjo CincoNo ratings yet
- Askep Pada Acute Coronary Syndrome AcsDocument62 pagesAskep Pada Acute Coronary Syndrome Acsdefi rhNo ratings yet
- Assessing Older DriversDocument246 pagesAssessing Older DriversSundar RamanathanNo ratings yet
- Joe Dispenza You Are The Placebo PDF 21Document4 pagesJoe Dispenza You Are The Placebo PDF 21Humaidhan0% (2)
- Pfeiffer 5 Ppts Chapter05 - The Psychology of Injury (Student Copy)Document13 pagesPfeiffer 5 Ppts Chapter05 - The Psychology of Injury (Student Copy)api-287615830No ratings yet
- Discharge PlanDocument1 pageDischarge PlanGail GenturalezNo ratings yet
- Patheon Dosage CapabilitiesDocument6 pagesPatheon Dosage CapabilitiesHariharan90No ratings yet
- Medico Graph I A 123Document124 pagesMedico Graph I A 123Rafael CastilloNo ratings yet
- Communicable Disease Nursing Part II Diseases (1) 2Document21 pagesCommunicable Disease Nursing Part II Diseases (1) 2MK LiNo ratings yet
- 3 Review ArticleDocument4 pages3 Review ArticleMohammad Abdullah BawtagNo ratings yet
- Dubai Healthcare Professional Licensing Guide - Final - 2Document141 pagesDubai Healthcare Professional Licensing Guide - Final - 2Fahad IqbalNo ratings yet
- Cna Program Outline April 2023Document5 pagesCna Program Outline April 2023Andrea WilliamsNo ratings yet
- CPG Management of Hypertension (4th Edition)Document98 pagesCPG Management of Hypertension (4th Edition)ssfdsNo ratings yet
- Evaluation of The R One Robotic System For Percutaneous Coronary Intervention THDocument11 pagesEvaluation of The R One Robotic System For Percutaneous Coronary Intervention THNeranga SamaratungeNo ratings yet
- Irritable Bowel Syndrome CASE STUDY REVISEDDocument51 pagesIrritable Bowel Syndrome CASE STUDY REVISEDJenjen 23No ratings yet
- Postoperative Care in MedicalDocument5 pagesPostoperative Care in MedicalMark Russel Sean LealNo ratings yet