Professional Documents
Culture Documents
Pulmonary Disorder
Uploaded by
Ike RilleraOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pulmonary Disorder
Uploaded by
Ike RilleraCopyright:
Available Formats
Surgery Block
SECTION VIII: MEDICAL & SURGICAL COMPLICATIONS
2012
CHAPTER 46
Pulmonary Disorders
Dr.
REVIEW ON MATERNAL PHYSIOLOGY
CARDIOVASCULAR CHANGES IN
Pregnancy
Heart
Changes that occurs as the diaphragm becomes
progressively elevated
Heart is displaced to the left and upward and rotated
somewhat on its long axis
Apex is moved somewhat laterally from its usual
position, causing a larger cardiac silhouette on chest
radiograph
⚜ pregnant women normally have some degree of
benign pericardial effusion, which may increase
the cardiac silhouette
Pulmonary Function during Pregancy
RESPIRATORY RATE
essentially unchanged
INCREASES during Pregnancy
Vital capacity and inspiratory capacity
⚜ by 20% by late pregnancy
Tidal volume
⚜ by 40% as a result of the respiratory
stimulant properties of Progesterone
Minute ventilation
⚜ by 30 to 40% due to tidal volume
Arterial pO2
⚜ from 100 to 105 mm Hg
CARDIAC OUTLINE that occurs in pregnancy. Carbon dioxide production & diffusion capacity
⚜ BLUE LINES: represent the relations between ⚜ production by 30%
⚜ diffusion capacity
the heart and thorax in the nonpregnant woman
Ventilation
⚜ BLACK LINES: represent the conditions existing
⚜ d/t deeper but not more frequent breathing
in pregnancy DECREASED during Pregnancy
Expiratory reserve volume
⚜ from 1300 mL to 1100 mL
RESPIRATORY TRACT CHANGES IN pCO2
Pregnancy
⚜ w/ alveolar hyperventilation, the pCO2 from
40 to 32 mm Hg
Residual volume
⚜ by 20% from 1500 mL to 1200 mL
Respiratory Tract Changes
functional residual capacity
DIAPHRAGM ⚜ sum of expiratory reserve and residual volumes
rises about 4 cm during pregnancy
⚜ by 10 to 25%
SUBCOSTAL ANGLE
⚜ d/t expanding uterus & abdominal
widens appreciably
pressure causing chest wall compliance to by
transverse diameter of the thoracic cage 2 cm. rd
1/3
THORACIC CIRCUMFERENCE
CHANGES presumably are induced by:
by 6 cm
basal oxygen consumption
not sufficiently to prevent a reduction in the residual
lung volume created by the elevated diaphragm. ⚜ incrementally by 20 to 40 mL/min in the
DIAPHRAGMATIC EXCURSION second half of pregnancy.
greater in pregnant than in nonpregnant women KIDNEYS
bicarbonate excretion serum levels to 15 to
20 meq/L
pH is slightly alkalotic at 7.45
1 Williams Obstetrics 23rd Edition
Surgery Block
SECTION VIII: MEDICAL & SURGICAL COMPLICATIONS
2012
PULMONARY COMPLICATIONS CLINICAL COURSE
Clinical illness ranging from mild wheezing to severe
bronchoconstriction
PULMONARY DISORDERS IN functional result of acute bronchospasm
Pregnancy ⚜ airway obstruction
⚜ decreased airflow
⚜ work of breathing progressively increases
Patient present with
Pulmonary Disorders ⚜ chest tightness
ASTHMA ⚜ wheezing
most common ⚜ breathlessness
affects up to 4 percent of women Distribution of airway narrowing is uneven
CA-PNA + Asthma alterations in oxygenation Ventilation–Perfusion
accounts for 10% of nonobstetrical antepartum Mismatching
HYPOXIA
hospitalizations in one managed care plan
⚜ MILD
advanced pregnancy may intensify the Initially compensated by hyperventilation
pathophysiological effects of some lung diseases normal arterial pO2, decreased pCO2
disparate number of maternal deaths during the Respiratory Alkalosis
influenza pandemics of 1918 and 1957 ⚜ PROGRESSION
poor tolerance for pregnancy of women with severe As airway narrowing worsens
ventilation–perfusion defects arterial
chronic lung disease
hypoxemia ensues
With severe obstruction
Asthma ⚜ Ventilation impaired because fatigue causes
common in young women and therefore is seen early CO2 retention
frequently during pregnancy. Because of hyperventilation, this may only
asthma prevalence during pregnancy: 4 and 8 percent be seen initially as an arterial pCO2
Chronic inflammatory airway disorder returning to the normal range
PATHOPHYSIOLOGY
Major hereditary component
⚜ airway responsiveness and persistent
subacute inflammation a/w:
Chromosomes 5, 11, and 12
Cytokine gene clusters
β-adrenergic and glucocorticoid receptor
genes
T-cell antigen receptor gene
environmental allergic stimulant
⚜ influenza
⚜ cigarette smoke
Hallmarks of asthma:
⚜ Reversible airway obstruction from
bronchial smooth muscle contraction
Vascular congestion
Tenacious mucus
Mucosal edema
Airway inflammation
⚜ d/t responsiveness to stimuli
irritants
viral infections
aspirin
cold air
exercise
⚜ Inflammatory response caused by:
mast cells
eosinophils
lymphocytes
bronchial epithelium
Inflammatory Mediators:
⚜ Histamine
changes are generally reversible and well tolerated
⚜ Leukotrienes
by the healthy nonpregnant individual
⚜ Prostaglandins
However, even early stages of asthma may be
⚜ Cytokines
dangerous for the pregnant woman and her fetus
⚜ IgE
⚜ Because the smaller functional residual capacity
F-series prostaglandins and ergonovine
and increased effective shunt render the woman
⚜ Exacerbate asthma
more susceptible to hypoxia and hypoxemia
⚜ commonly used obstetrical drugs
⚜ should be avoided if possible
2 Williams Obstetrics 23rd Edition
Surgery Block
SECTION VIII: MEDICAL & SURGICAL COMPLICATIONS
2012
direct relationship with birthweight
inverse relationship with rates of
gestational hypertension and preterm
delivery
Life-threatening complications from status
asthmaticus include
muscle fatigue with respiratory arrest
pneumothorax
pneumomediastinum
acute cor pulmonale
cardiac arrhythmias
Maternal and perinatal mortality rates are
substantively increased when mechanical
ventilation is required
⚜ FETAL EFFECTS
No significant adverse neonatal sequelae
from asthma
But when respiratory alkalosis develops
EFFECTS OF PREGANCY ON ASTHMA fetal hypoxemia develops well before
the alkalosis compromises maternal
no evidence that pregnancy has a predictable effect
oxygenation
on underlying asthma Fetal Compromise results from
⚜ baseline severity correlated with asthma uterine blood flow
morbidity during pregnancy decreased maternal venous return
MILD disease: alkaline induced shift to the left of the
12% w/ exacerbation oxyhemoglobin dissociation curve
2.3 % require admission Fetal response to Maternal hypoxemia:
MODERATE disease: umbilical blood flow
26% w/ exacerbation systemic and pulmonary vascular
7% require admission resistance
SEVERE Disease: cardiac output
52% w/ exacerbation incidence of fetal-growth restriction
27% require admission
increases with asthma severity
⚜ 1/3 each: improved, remained unchanged or
worsened hence, need for aggressive
⚜ 20% w/ Intrapartum Exacerbation among management
women w/ MILD to MODERATE asthma CLINICAL EVALUATION
⚜ 18 fold increased risk of exacerbation following ⚜ subjective severity of asthma frequently does
caesarean vs vaginal delivery not correlate with objective measures of airway
function or ventilation
Asthma & Pregnancy
⚜ Clinical examination
ASTHMA Exacerbation (%) Admission (%)
Mild 13-20 2.3
inaccurate as a predictor of severity
Moderate 26 7 Useful clinical signs include
Severe 50 27 labored breathing
tachycardia
PREGNANCY OUTCOMES pulsus paradoxus
⚜ MATERNAL & PERINATAL OUTCOMES prolonged expiration
slightly increased incidence of use of accessory muscles
preeclampsia Signs of a potentially fatal attack
☀ risk in moderate to severe central cyanosis
asthma, regardless of treatment altered consciousness.
preterm labor ⚜ Arterial blood gas analysis
☀ increased about twofold in severe provides objective assessment of maternal:
asthma oxygenation
low-birthweight infants ventilation
perinatal mortality acid–base status.
placental abruption severity of an acute attack can be assessed
preterm rupture of membranes ROUTINE arterial blood gas analysis
most obstetrical complications were not did not help to manage most pregnant
higher in asthmatic women vs women who required admission for
nonasthmatics, except: asthma control.
depression If used, the results must be interpreted in
miscarriages relation to normal values for pregnancy
cesarean delivery pCO2 > 35 mm Hg with a pH < 7.35
significantly increased morbidity is linked to ☀ consistent with hyperventilation
progressively more severe disease and CO2 retention in a pregnant
poor control woman.
combination of both ⚜ Pulmonary function testing
baseline pregnancy forced expiratory should be routine in the management of
volume at 1 second (FEV1) chronic and acute asthma.
3 Williams Obstetrics 23rd Edition
Surgery Block
SECTION VIII: MEDICAL & SURGICAL COMPLICATIONS
2012
Sequential measurement of the FEV1 or the STEPWISE THERAPY OF CHRONIC ASTHMA DURING PREGNANCY
peak expiratory flow rate—PEFR SEVERITY STEPWISE THERAPY
best measures of severity MILD INTERMITTENT Inhaled β-agonists (ALBUTEROL) as needed
Low-dose inhaled corticosteroids
FEV1 (BUDESONIDE)
☀ If < 1 L or < 20% of predicted value MILD PERSISTENT
ALTERNATIVE: Cromolyn, leukotriene
❧ correlates with severe disease antagonists, or theophylline
defined by Low-dose inhaled corticosteroids and long-
acting β-agonists (SALMETEROL) or
☘ hypoxia medium-dose inhaled steroids and long-
☘ poor response to therapy MODERATE PERSISTENT acting β-agonist if needed
☘ high relapse rate Alternative—low-dose (or medium if
needed) inhaled steroids and either
PEFR theophylline or leukotriene antagonists
☀ correlates well with the FEV1 High-dose inhaled corticosteroids and long-
☀ can be measured reliably with acting β-agonist and oral steroids if needed
SEVERE PERSISTENT ALTERNATIVE: high-dose inhaled
inexpensive portable meters
corticosteroids and theophylline and oral
☀ Each woman determines her own steroids
baseline when asymptomatic—
personal best ⚜ ALTERNATIVE DRUGS
❧ compared with values when Theophylline
symptomatic Methylxanthine
☀ PEFR did not change during the bronchodilators and possibly anti-
course of pregnancy in normal inflammatory agents
women. used less frequently since inhaled
MANAGEMENT OF CHRONIC ASTHMA corticosteroids became available
⚜ Management Guidelines on Asthma & Some theophylline derivatives are
Pregnancy: considered useful for oral maintenance
Objective assessment of pulmonary therapy if the initial response is not
function & fetal well being optimal to inhaled corticosteroids and
monitor with PEFR or FEV1 β-agonists
Environmental precipitating factors Leukotriene modifiers
Avoidance or control of triggers inhibit their synthesis and include
Pharmacological drugs ☀ zileuton
to provide baseline control and treat ☀ zafirinkast
exacerbations ☀ montelukast
Patient education given orally or by inhalation for
general asthma management and its
prevention
effect on pregnancy
☀ not effective for acute disease
⚜ women with moderate to severe asthma
For maintenance
should measure and record either their
☀ used in conjunction with inhaled
FEV1 or PEFR twice daily
corticosteroids to allow minimal
FEV1
dosing
☀ Ideally >80 percent of predicted.
not as effective as inhaled
PEFR
corticosteroids
☀ predicted values range from 380 to Cromolyn and nedocromil
550 L/min inhibit mast cell degranulation
☀ Each woman has her own baseline ineffective for acute asthma
value, & therapeutic adjustments taken chronically for prevention
can be made using this not as effective as inhaled
⚜ Treatment depends on the severity of disease corticosteroids
β-agonists been replaced by leukotriene modifiers
help to abate bronchospasm omalizumab
corticosteroids no experience in pregnant women
treat the inflammatory component a recombinant humanized monoclonal
For mild asthma anti-IgE antibody
inhaled β-agonists binds circulating IgE to deactivate it
☀ as needed are usually sufficient MANAGEMENT OF ACUTE ASTHMA
For persistent asthma ⚜ Similar to that for the nonpregnant asthmatic
inhaled corticosteroids Except for those w/ lowered threshold for
☀ administered every 3 to 4 hours. hospitalization
☀ Goal: ⚜ Intravenous hydration may help clear
❧ to the use of β-agonists for pulmonary secretions
symptomatic relief ⚜ Supplemental oxygen is given by mask
☀ hospitalizations by 80 percent ⚜ THERAPEUTIC AIM:
55% in readmissions for severe Maintain the pO2 > 60 mm Hg to NORMAL
exacerbations in pregnant asthmatics with 95-% oxygen saturation
given maintenance inhaled ⚜ Baseline pulmonary function testing:
corticosteroids along with β-agonist Includes FEV1 or PEFR
therapy ⚜ Continuous pulse oximetry and electronic fetal
monitoring
4 Williams Obstetrics 23rd Edition
Surgery Block
SECTION VIII: MEDICAL & SURGICAL COMPLICATIONS
2012
⚜ First-line therapy ⚜ Maintenance medications are continued
β-adrenergic agonist through delivery
given SQ, oral or inhaled ⚜ Give anesthesia preferably EPIDURAL
EXAMPLES ANESTHESIA
☀ Terbutaline ⚜ Stress-dose corticosteroids
☀ Albuterol administered with systemic steroid therapy
☀ Isoetharine within the preceding 4 weeks
☀ Epinephrine Usual dose is 100 mg of HYDROCORTISONE
IV q 8 hours during labor and for 24 hours
☀ Isoproterenol
after delivery
☀ Metaproterenol
⚜ PEFR or FEV1
bind to specific cell-surface receptors
determined on admission
activate adenylyl cyclase
serial measurements taken
intracellular cyclic AMP modulate
⚜ Oxytocin or prostaglandins E1 or E2
bronchial smooth muscle relaxation
Used for cervical ripening and induction of
Long-acting preparations are used for
labor
outpatient therapy
⚜ Fentanyl:
Maintenance drug
Nonhistamine-releasing narcotic
Inhaled corticosteroids intensive β-
May be preferable to meperidine for labor,
agonist therapy
and epidural analgesia is ideal
For Severe exacerbations:
⚜ Conduction analgesia
Inhaled Ipratropium Bromide is given
For surgical delivery
Corticosteroids
preferred because tracheal intubation can
☀ should be given early to all
trigger severe bronchospasm
patients with severe acute asthma
⚜ Postpartum hemorrhage
☀ Given orally or parenteral Treated with oxytocin or prostaglandin E2.
☀ IV methylprednisolone Prostaglandin F2α or ergotamine derivatives
❧ 40 to 60 mg, every 6 hours CONTRAINDICATED
☀ Hydrocortisone by infusion may cause significant bronchospasm
☀ Prednisone orally.
☀ Give along w/ beta agonists for Acute Bronchitis
acute asthma Infection of the large airways
☀ onset of action is several hours MANIFESTATION
For acute asthma cough without pneumonitis
Corticosteroids β-agonists common in adults, especially in winter months
⚜ If initial therapy with β-agonists is a/w Infections are usually caused by viruses commonly:
improvement of FEV1 or PEFR >70 % of baseline influenza A and B
discharge can be considered parainfluenza
Some may benefit from observation.
respiratory syncytial
coronavirus
⚜ for the woman with obvious respiratory distress,
adenovirus
or if the FEV1 or PEFR <70% of predicted after rhinovirus
three doses of β-agonist Bacterial agents causing community-acquired pneumonia
admission is advisable are rarely implicated.
Intensive therapy includes cough
inhaled β-agonists persists for 10 to 20 days (mean 18 days)
occasionally lasts for a month or longer
intravenous corticosteroids
routine antibiotic treatment is not justified
close observation for worsening
respiratory distress or fatigue in Pneumonia
breathing TYPES OF PNA
woman is cared for in the delivery unit or an Community Acquired PNA
intermediate or intensive care unit ⚜ encountered in otherwise healthy young
STATUS ASTHMATICUS AND RESPIRATORY FAILURE women, including during pregnancy
⚜ Severe asthma of any type NOT responding after ⚜ relatively common in pregnant women
30 to 60 minutes of intensive therapy ⚜ caused by a number of bacterial or viral
⚜ Managed in ICU pathogens
⚜ Management of nonpregnant patients in an Healthcare-Associated PNA
intensive care setting good outcome in most ⚜ in patients in outpatient care facilities
cases ⚜ more closely resembles hospital-acquired
⚜ Consider Early intubation when maternal pneumonia (HAP)
respiratory status worsens despite aggressive nursinghome-acquired pneumonia (NHAO)
treatment ventilator-associated pneumonia (VAP).
Indications for mechanical ventilation: accounts for 4.2% of antepartum admissions for
Fatigue nonobstetrical complications
Carbon dioxide retention Mortality from pneumonia
Hypoxemia infrequent in young women
LABOR & DELIVERY
5 Williams Obstetrics 23rd Edition
Surgery Block
SECTION VIII: MEDICAL & SURGICAL COMPLICATIONS
2012
during pregnancy severe pneumonitis with ⚜ Outpatient or 23-hour observation is reasonable
appreciable loss of ventilatory capacity is not as well if home care & follow up are optimal
tolerated
Hypoxemia and acidosis
⚜ poorly tolerated by the fetus
⚜ frequently stimulate preterm labor after
midpregnancy. B
⚜ worsening or persistence of symptoms may
represent developing pneumonia.
Any pregnant woman suspected of having
pneumonia should undergo chest radiography.
BACTERIAL PNEUMONIA
Many bacteria that cause community-acquired
pneumonia, such as Streptococcus pneumoniae, are
part of the normal resident flora
Some Factors that perturb the symbiotic relationship
b/w colonizing bacteria and mucosal phagocytic
defenses include
⚜ acquisition of a virulent strain
⚜ bacterial infections following a viral infection
Cigarette smoking and chronic bronchitis favor
colonization of:
⚜ S. pneumonia CHEST RADIOGRAPHS in a pregnant woman with RIGHT LOWER LOBE
PNEUMONIA. A. Complete opacification of the right lower lobe (arrows)
⚜ Haemophilus influenza is consistent with the clinical suspicion of pneumonia
⚜ Legionella species
Risk factors include: CRITERIA FOR SEVERE COMMUNITY ACQUIRED PNEUMONIA
⚜ Asthma CRITERIA VALUES
⚜ binge drinking RESPIRATORY RATE ≥30/min
⚜ human immunodeficiency virus (HIV) infection PaO2/FiO2 ratio ≤250
INCIDENCE AND CAUSES LUNG INFILTRATES MULTILOBULAR infiltrates
⚜ Pregnancy itself DOES NOT predispose to LEVEL OF CONSCIOUSNESS Confusion/disorientation
pneumonia UREMIA UREMIA
⚜ Hospitalization for pneumonia to be 1.5 per Leukopenia—WBC <4000/µL
1000 deliveries CBC Thrombocytopenia—platelets
<100,000/µL
⚜ > 50% of adult PNA are bacterial
TEMPERATURE Hypothermia—core temperature <36°C
⚜ 75% of the Causes of PNA are:
Hypotension requiring aggressive fluid
S. pneumoniae (37%) BLOOD PRESSURE
resuscitation
most common bacterial & overall cause
of PNA ⚜ If w/ SEVERE PNA
AKA: Pneumococci admission to an intensive care or
Influenza A (14%) intermediate care unit is advisable
MC viral cause of PNA common cause of acute respiratory distress
Chlamydophila pneumonia (10%) syndrome during pregnancy
H. Influenza (5%) mechanical ventilation maybe necessary
Mycoplasma pneumoniae (2%) ⚜ Antimicrobial treatment is empirical
Legionella pneumophila (2%) MOST ADULT PNA are caused by
⚜ CA-MRSA Pneumococci
Cause Necrotizing pneumonia Mycoplasma
DIAGNOSIS Chlamydophilia
⚜ Typical Symptoms include: Monotherapy initially is with a MACROLIDE:
Cough Azithromycin
Dyspnea Clarithromycin
Sputum production Erythromycin
Pleuritic chest pain ☀ Given intravenously and then
⚜ Mild upper respiratory symptoms and malaise orally, was effective in 99% of
Precededs above symptoms women w/ uncomplicated PNA
⚜ Diagnostic Tests If w/ SEVERE disease:
CBC: Respiratory Fluoroquinolone
Mild leukocytosis ☀ DRUGS
Chest radiography
❧ Levofloxacin
Essential to establish dx & help monitor
disease ❧ Moxifloxacin
Does not accurately predict etiology ❧ Gemifloxacin
⚜ Other Recommended Tests ☀ Teratogenicity risk: LOW
Rapid Serological Testing (RAST) ❧ given if indicated
Test for Influenza A & B β-Lactam + Macrolide
MANAGEMENT ☀ Preferred β-Lactams:
⚜ Hospitalize all pregnant women w/ ❧ high-dose amoxicillin
radiographically proven PNA ❧ amoxicillin-clavulanate
6 Williams Obstetrics 23rd Edition
Surgery Block
SECTION VIII: MEDICAL & SURGICAL COMPLICATIONS
2012
☀ Alternatives for MACROLIDE
resistant Pneumococci (25%)
❧ Ceftriaxone
❧ Cefpodoxime
❧ Cefuroxime
❧ Levofloxacin
CA-MRSA
vancomycin
⚜ RESOLUTION OF PNA
Clinical improvement is usually evident in
48 to 72 hours
Resolution of fever in 2 to 4 days
Resolution of X-ray abnormalities takes up
to 6 weeks
⚜ Worsening disease
poor prognostic feature
follow-up radiography is recommended
if fever persists
20% of women develop a pleural effusion
⚜ FACTOR that increase the risk of death or
complications w/ CA PNA CHEST RADIOGRAPH of a 30-week pregnant woman with INFLUENZA A
PNEUMONIA. Extensive right lower lung field opacification (arrows),
Coexisting chronic conditions
which represents parenchymal infiltrate and pleural effusion, obscures
Clinical Findings the right hemidiaphragm
RR > 30
Hypotension
quickly infects ciliated columnar
Tachycardia: PR > 125 bpm
Hypothermia epithelium, alveolar cells, mucus gland
Temp <36ᵒC or > 40ᵒC cells, and macrophages
ALOC ONSET
Extrapulmonary dse ⚜ 1-4 days after exposure
LABS FLU shots recommended in pregnancy
Leukopenia or leukocytosis Infection is self-limited
PREGNANCY OUTCOME PRIMARY INFLUENZA PNEUMONITIS
rd
⚜ Without antibiotics, 1/3 pregnant women with ⚜ Most severe
pneumonia died ⚜ CHARACTERISTICS
⚜ maternal mortality rate was 0.8 percent of 632 sparse sputum production
women. radiographic interstitial infiltrates
⚜ 7% required intubation and mechanical SECONDARY PNEUMONIA
ventilation. ⚜ More Common
⚜ COMMON COMPLICATIONS of PNA during ⚜ Develops from bacterial superinfection by
Pregnancy: Streptococci or Staphylococci after 2 to 3 days
Prematurely ruptured membranes of initial clinical improvement
Preterm delivery MANAGEMENT
low-birthweight infants ⚜ RECOMMENDED for UNCOMPLICATED PNA
PREVENTION Supportive treatment
⚜ Pneumococcal vaccine Antipyretics
60-70% protective against its 23 serotypes Bed rest
Emergence of drug-resistant ⚜ influenza A
pneumococci H3N2 strains
Not recommended for otherwise healthy Has rapid resistance to
pregnant women ☀ AMANTADINE
Recommended for: ☀ RIMANTADINE
Immunocompromised H1N1 strain
HIV infection Resistant to OSELTAMIVIR
Significant smoking history ⚜ DRUGs for CHEMOPROPHYLAXIS & TREATMENT
Diabetes Neuraminidase inhibitors
Cardiac, pulmonary, or renal disease given within 2 days of symptoms onset
Asplenia (sickle-cell disease) for influenza A and B infection
INFLUENZA PNEUMONIA MOA
Respiratory infection ☀ interfere with the release of
⚜ PNEUMONITIS progeny virus from infected host
PNA cells and thus prevent infection of
MC complication new host cells
Caused by RNA viruses of which influenza A and B Effective for early influenza
form one genus DRUGS
⚜ Influenza A ☀ Oseltamivir
Serious, epidemic in winter months ❧ oral, 75 mg BID
MOA ☀ Zanamivir
⚜ aerosolized droplets ❧ inhalation, 10 mg BID
7 Williams Obstetrics 23rd Edition
Surgery Block
SECTION VIII: MEDICAL & SURGICAL COMPLICATIONS
2012
shorten the course of illness by 1 to 2 Should NOT BE GIVEN to women who may
days become pregnant during the month
may reduce the risk for pneumonitis following each vaccine dose
PREVENTION Attenuated vaccine virus is not secreted in
⚜ Vaccination for influenza A breast milk
⚜ Prenatal vaccination affords protection for a Postpartum vaccination MUST NOT be
third of infants for at least 6 months delayed
EFFECTS ON PREGNANCY FUNGAL & PARASITIC PNA
⚜ Severe viral pneumonitis is life-threatening Greatest consequence in immunocompromised
during pregnancy hosts, especially in women with acquired
FETAL EFFECTS: immunodeficiency syndrome (AIDS).
⚜ No firm evidence causes congenital Pneumocystis Pneumonia
malformations ⚜ Lung infection with Pneumocystis jiroveci
⚜ Increased neural-tube defects in neonates aka Pneumocystis carinii
(possibly associated with early hyperthermia) ⚜ Common complication in women with AIDS
⚜ May predispose to schizophrenia in later life ⚜ Causes INTERSTITIAL PNA characterized by:
VARICELLA PNEUMONIA Dry cough
AGENT Tachypnea
⚜ Varicella Zoster Virus Dyspnea
Double-stranded DNA herpesvirus Diffuse radiographic infiltrates
Attack rate in seronegative individual is 90% ⚜ Management:
PRIMARY INFECTION Trimethoprim-sulfamethoxazole
Chickenpox or Varicella Pentamidine
☀ CLINICAL MANIFESTATIONS Tracheal intubation and mechanical
ventilation
❧ 1- to 2-day flulike prodrome
⚜ Prophylaxis
❧ pruritic maculopapular
Double-strength TRIMETHOPRIM-
vesicular lesions that crust
SULFAMETHOXAZOLE tablet
over in 3 to 7 days
daily for some HIV-infected pregnant
☀ MORTALITY d/t Varicella PNA women
❧ More severe in adulthood Fungal Pneumonia
especially during pregnancy ⚜ Usually seen in women with HIV infection
10% of Pregnancy PNA ⚜ Who are otherwise immunocompromised
Risk of developing PNA ⚜ Organisms:
⚜ Smoking Histoplasmosis & Blastomycosis
⚜ >100 skin lesions not common
Clinical Manifestations: more severe during pregnancy
⚜ Symptoms of pneumonia (appear 3 to 5 days) (+) erythema nodosum
characterized: ☀ symptomatic infection
Fever, tachypnea, dry cough, dyspnea, and
☀ better overall prognosis
pleuritic pain
Cryptococcosis
Nodular infiltrates are similar to other viral
manifest as MENINGITIS
pneumonias
⚜ Management:
Fever and compromised pulmonary
ITRACONAZOLE
function may persist for weeks
PREFERRED therapy for disseminated
Diagnosis:
fungal infections
⚜ Performing a Tzanck smear
INTRAVENOUS AMPHOTERICIN B OR
Fetal and Neonatal Varicella Infection:
KETOCONAZOLE
⚜ Fetus may develop Congenital Varicella
Amphotericin B
Syndrome
☀ used extensively in pregnancy with
Chorioretinitis
no embryo-fetal effects
Microphthalmia
FLUCONAZOLE, ITRACONAZOLE, AND
Cerebral cortical atrophy
KETOCONAZOLE
Growth restriction
embryotoxic in large doses in early
Hydronephrosis
pregnancy
Skin or bone defects
ITRACONAZOLE
Management
⚜ Supportive care ☀ reasonable later in pregnancy
⚜ Intravenous ACYCLOVIR therapy
For Invasive candidiasis
2
500 mg/m or 10 to 15 mg/kg every 8 hours CASPOFUNGIN, MICAFUNGIN, AND
⚜ Serious maternal infection w/sepsis of varicella
ANIDULAFUNGIN
PNA is a/w PRETERM DELIVERY ☀ Embryotoxic and teratogenic in
VACCINATION laboratory animals
⚜ Attenuated live-virus vaccine—VARIVAX SEVERE ACUTE RESPIRATORY DISTRESS SYNDROME
2 doses, given 4 to 8 weeks apart CORONAVIRUS respiratory infection
recommended for adolescents and adults ATYPICAL Pneumonitis
with no history of varicella case-fatality rate :
NOT RECOMMENDED for pregnant women ⚜ NONPREGNANT: ~ 5%
⚜ PREGNANT: 25%
8 Williams Obstetrics 23rd Edition
Surgery Block
SECTION VIII: MEDICAL & SURGICAL COMPLICATIONS
2012
PLACENTAL EFFECT: ⚜ Cycloserine
⚜ abnormal intervillous or subchorionic fibrin ⚜ Para-aminosalicylic acid
deposition TUBERCULOSIS AND PREGNANCY
⚜ extensive fetal thrombotic vasculopathy OUTCOMES
⚜ dependent on the site of infection and timing of
Tuberculosis diagnosis in relation to delivery
MOT active pulmonary tuberculosis associated with
inhalation of Mycobacterium tuberculosis incidences:
⚜ incites a granulomatous pulmonary reaction ⚜ preterm delivery: 2x
In 90% of patients, infection contained and dormant for ⚜ low-birthweight: 2x
long periods ⚜ growth-restricted infants
reactivated in IMMUNOCOMROMISED patients ⚜ perinatal mortality: 6x
MANIFESTATIONS:
⚜ Preeclampsia: 2x
Cough with minimal sputum production
Adverse outcomes correlate with
Low-grade fever
Hemoptysis ⚜ Late diagnosis
Weight loss. ⚜ Incomplete or irregular treatment
Mediastinal lymphadenopathy ⚜ Advanced pulmonary lesions
LABORATORY FINDINGS CDC GUIDELINES FOR TB
Culture ⚜ SKIN TESTING of pregnant women who are in
⚜ Ziehl-Neelsen acid-fast staining any of the high-risk groups
(+) Acid Fast Bacilli on stained smears of Purified Protein Derivative (PPD)
sputum preferred antigen
Chest radiograph intermediate strength of 5 tuberculin
⚜ Variety of infiltrative pattern units.
intracutaneously applied
⚜ Cavitation
If NEGATIVE
EXTRAPULMONARY TB
Middle ear ☀ no further evaluation is needed.
Tonsils IF POSITIVE
Lungs ☀ (+) skin test measures > 5 mm in
Pericardium diameter
CNS ☀ requires evaluation for active
Bones, spine, psoas mm disease, including a chest
Pelvic TB radiograph
⚜ Common ☀ VERY HIGH-RISK patients:
⚜ Amenorrhea, ascites, adhesions ❧ HIV-positive
Intestine ❧ abnormal chest radiography
Genitals ❧ recent contact with an active
⚜ especially epididymis case— > 5 mm
Liver,spleen, peritoneum, ☀ HIGH RISK patients
Adrenal glands ❧ Foreign-born individuals
Ureter ❧ intravenous drug users who
Bladder are HIV-negative
Adnexa
❧ low-income populations
Prostate, seminal vesicles
❧ medical conditions that
MILIARY TB
increase the risk for
40%of affected HIV-positive patients have
tuberculosis— >10 mm
disseminated disease
TREATMENT ☀ For persons with no risk factors but
Cure rates with 6-month short-course DIRECTLY w/ > 15 mm or greater is defined
OBSERVED THERAPY (DOT) as requiring treatment
Multidrug-resistant tuberculosis (MDR-TB)
⚜ rapidly as TB incidence fell during the 1990s
FOUR-DRUG REGIMEN for initial empirical treatment:
Isoniazid
Rifampin
Pyrazinamide
Ethambutol
Extensively Drug-Resistant Tuberculosis—XDR-TB
st
Resistance in vitro to at least the 1 -line drugs
⚜ Isoniazid
⚜ Rifampin
ND
Resistance to >3 of the 6 main classes of 2 -LINE
DRUGS
⚜ Aminoglycosides
⚜ Polypeptides
⚜ Fluoroquinolones
⚜ Thioamides
9 Williams Obstetrics 23rd Edition
Surgery Block
SECTION VIII: MEDICAL & SURGICAL COMPLICATIONS
2012
⚜ In Vitro Quantiferon-TB Gold Test NEONATAL TUBERCULOSIS
same indications as skin testing Tubercular bacillemia can infect the
useful in identifying patients with latent ⚜ Placenta
TB and at risk for progression to active ⚜ Fetus
disease. Congenital Tuberculosis
distinguish between immune responses d/t aspiration of infected secretions at
delivery
due to infection and responses resulting
simulates other congenital infections
from bacille Calmette-Guérin (BCG) MANIFESTATIONS
vaccination ☀ Hepatosplenomegaly
TREATMENT
☀ respiratory distress
⚜ Principles are similar in pregnant & nonpregnant
☀ fever
except STREPTOMYCIN NOT ALLOWED in
pregnancy ☀ lymphadenopathy
unlikely if the mother with active disease has been
⚜ LATENT INFECTION
treated before delivery or if her sputum culture is
ISONIAZID:
negative
For Nonpregnant; (+) Tuberculin; < 35
recommend isolation from the mother suspected of
Years; (-) Evidence Of Active Disease
having active disease
☀ 300 mg orally daily for 1 year
⚜ contradicts EINT
Considered safe in pregnancy st
After delivery, NORMALLY, the 1 thing you
COMPLIANCE is a major problem
is do place the baby on top on mother’s
Delayed administration until after
chest w/ baby wrapped & dried,
delivery:
wait for the cord to stop pulsating (around
☀ For possibly increased isoniazid- 2 minutes) before clamping
induced hepatitis risk in Allows more blood to flow to baby
postpartum women After 2 mintues, double clamp & cut
☀ Withholding treatment until 3 to 6 umbilical cord
months after delivery Wait for the baby to crawl & look for nipple
☀ Exceptions to delayed treatment in & latch naturally
pregnancy: Occurs ~ 20-30 minutes after delivery
❧ Known recent skin-test ⚜ So if mother is w/ tuberculosis
convertors Recommend to still follow EINT but
❧ Skin-test-positive women MOTHER MUST WEAR MASK FIRST
exposed to active infection If untreated, the risk of disease in the infant
❧ HIV-positive women born to a woman with active infection is
⚜ ACTIVE INFECTION 50% in the first year
Recommended initial treatment:
Three-drug regimen
☀ ISONIAZID
☀ RIFAMPIN
☀ ETHAMBUTOL
Prevalence of isoniazid-resistant
tuberculosis
☀ PYRAZINAMIDE
If organism is susceptible:
☀ Regimen is given for 9 months
Breast feeding is not prohibited
To decrease hepatic toxicity:
ISONIAZID PYRIDOXINE (25 mg/day
orally)
HIV-INFECTED WOMEN:
Rifampin or Rifabutin
☀ CONTRAINDICATED If certain
protease inhibitors or non-
nucleoside reverse transcriptase
inhibitors are being administered
Resistance to rifabutin or rifampin:
☀ Pyrazinamide therapy is given
Second-line regimens
CONTRAINDICATED
ototoxic to the fetus
Aminoglycosides
☀ Streptomycin
☀ Kanamycin
☀ Amikacin
☀ Capreomycin
10 Williams Obstetrics 23rd Edition
You might also like
- Physiology of PregnancysDocument10 pagesPhysiology of PregnancysadiNo ratings yet
- Physiology of Pregnancy: Learning ObjectivesDocument3 pagesPhysiology of Pregnancy: Learning ObjectivesadiNo ratings yet
- Maternal Adaptations in Pregnancy and Fetal MorphologyDocument51 pagesMaternal Adaptations in Pregnancy and Fetal Morphologykira santosNo ratings yet
- Perubahan Fisiologi KehamilanDocument32 pagesPerubahan Fisiologi Kehamilandmandatari7327No ratings yet
- Anatomical and Physiological ChangesDocument10 pagesAnatomical and Physiological Changesyosua simarmataNo ratings yet
- Acute Conditions of The NeonatesDocument8 pagesAcute Conditions of The Neonatesjillmonicadaquipil7No ratings yet
- NU403 Simulation PrepDocument8 pagesNU403 Simulation Prephaleykatherine.sandersNo ratings yet
- Prone VentilationDocument25 pagesProne VentilationHazel AsperaNo ratings yet
- 9.anesthesia For Obstetrics. Pediatric Anesthesia. Geriatric Anesthesia.Document52 pages9.anesthesia For Obstetrics. Pediatric Anesthesia. Geriatric Anesthesia.karim hassanNo ratings yet
- 5.1 OB-Pulmonary Disorders in Pregnancy (Dr. Bautista)Document10 pages5.1 OB-Pulmonary Disorders in Pregnancy (Dr. Bautista)Monique BorresNo ratings yet
- Physiology of Pregnancy: Learning ObjectivesDocument5 pagesPhysiology of Pregnancy: Learning ObjectivesBaiiqDelaYulianingtyasNo ratings yet
- NU403 Simulation PrepDocument8 pagesNU403 Simulation Prephaleykatherine.sandersNo ratings yet
- Physiology of PregnancyDocument5 pagesPhysiology of PregnancyLorena Garcia PatiñoNo ratings yet
- Patient Anita NCPDocument15 pagesPatient Anita NCPJoshoua MalanaNo ratings yet
- Respiratory PhysiologyDocument5 pagesRespiratory PhysiologyRaul A UrbinaNo ratings yet
- NCP Impaired Gas Exchange STROKEDocument2 pagesNCP Impaired Gas Exchange STROKEMa. Elaine Carla TatingNo ratings yet
- Disease, Most Often Occurs In: Respiratory Distress SyndromeDocument6 pagesDisease, Most Often Occurs In: Respiratory Distress Syndromejoyrena ochondraNo ratings yet
- Lung Parenchymal DiseaseDocument21 pagesLung Parenchymal DiseaseCamille KayeNo ratings yet
- CASE 1: Manipac Yao: Cmmatias (Cmed 2022)Document3 pagesCASE 1: Manipac Yao: Cmmatias (Cmed 2022)Charm MatiasNo ratings yet
- Asma Dalam KehamilanDocument33 pagesAsma Dalam KehamilanAnonymous wztrzkVnNo ratings yet
- Lap Abdominal Surg-1Document4 pagesLap Abdominal Surg-1Rizwan AhmedNo ratings yet
- Respiratory PhysiologyDocument42 pagesRespiratory PhysiologyvtnvmycdvgNo ratings yet
- Uia34 Obstetric and Foetal Physiology - Implications For Clinical Practice in Obstetric Analgesia and AnaesthesiaDocument4 pagesUia34 Obstetric and Foetal Physiology - Implications For Clinical Practice in Obstetric Analgesia and AnaesthesiaadiNo ratings yet
- Imprint CPRDocument27 pagesImprint CPRStanford AnesthesiaNo ratings yet
- The NewbornDocument114 pagesThe NewbornKing kakaNo ratings yet
- Rle 8 4 21Document6 pagesRle 8 4 21Sheryhan Tahir BayleNo ratings yet
- Featl Transition Togdwwdq HvawDocument55 pagesFeatl Transition Togdwwdq HvawmunshiNo ratings yet
- Lecture Notes Surgery in Pregnancy Dr. BonleonDocument5 pagesLecture Notes Surgery in Pregnancy Dr. BonleonMonica Dianne AdtoonNo ratings yet
- Obstetric AnesthesiaDocument31 pagesObstetric AnesthesiaChosenNo ratings yet
- PULMO OB TransDocument8 pagesPULMO OB TransMichelle Vera GabunNo ratings yet
- Physiology of PregnancyDocument5 pagesPhysiology of PregnancyAlejandra RequesensNo ratings yet
- Biophysical Profile& Color Doppler Ultrasound in The High Risk PregnancyDocument56 pagesBiophysical Profile& Color Doppler Ultrasound in The High Risk Pregnancykhadzx100% (4)
- Airway: Nursing Care PlanDocument3 pagesAirway: Nursing Care PlanPhoebe Kyles CammaNo ratings yet
- ARDS Prone PositionDocument22 pagesARDS Prone PositionIhteshamNo ratings yet
- Surgery Trans 2a - Fluid and Electrolyte Management of The Surgical PatientDocument14 pagesSurgery Trans 2a - Fluid and Electrolyte Management of The Surgical PatientJoan Caacbay De GuzmanNo ratings yet
- Diagnosis Evaluation of The Patient That Who Is Having Oxygen InsufficiencyDocument5 pagesDiagnosis Evaluation of The Patient That Who Is Having Oxygen InsufficiencyesakkiammalNo ratings yet
- LESSON-PLAN-ON-PHYSIOLogical Changes During PregnancyDocument22 pagesLESSON-PLAN-ON-PHYSIOLogical Changes During PregnancyV.srivaniNo ratings yet
- Physiological Changes During Pregnancy 2-1Document32 pagesPhysiological Changes During Pregnancy 2-1PATRICK ROSHAN ANo ratings yet
- Community Acquired Pneumonia Nursing Care Plan: Demonstrate Pursed-Lip and Diaphragmatic Breathing To The PatientDocument4 pagesCommunity Acquired Pneumonia Nursing Care Plan: Demonstrate Pursed-Lip and Diaphragmatic Breathing To The PatientKrisianne Mae Lorenzo Francisco100% (1)
- 0900 - Friday - Hypoxemic Respiratory Failure - SesslerDocument69 pages0900 - Friday - Hypoxemic Respiratory Failure - Sesslertechang1No ratings yet
- Changes in Maternal Physiology During PregnancyDocument4 pagesChanges in Maternal Physiology During PregnancyTina Ong SinagaNo ratings yet
- Edema PulmonumDocument39 pagesEdema Pulmonumnilvany100% (1)
- PDF Document 4Document76 pagesPDF Document 4Suji MerlineNo ratings yet
- Physiological Changes in PregnancyDocument16 pagesPhysiological Changes in PregnancyKinshuk DhaliwalNo ratings yet
- Adjustments of The Infant To Extrauterine LifeDocument11 pagesAdjustments of The Infant To Extrauterine LifeAntoine TimmermansNo ratings yet
- CPR in Pregnancy 2Document3 pagesCPR in Pregnancy 2Fatmasari Perdana MenurNo ratings yet
- Ventilator Parameter & Its Normal RangeDocument8 pagesVentilator Parameter & Its Normal RangeTmanoj Praveen0% (1)
- Neonatal Resuscitation: Ryan D. Kearney Mark D. LoDocument12 pagesNeonatal Resuscitation: Ryan D. Kearney Mark D. LoAuliaNo ratings yet
- Proceedings of The 16th Italian Association of Equine Veterinarians CongressDocument8 pagesProceedings of The 16th Italian Association of Equine Veterinarians CongressCabinet VeterinarNo ratings yet
- Lesson Plan On PhysiologicalDocument22 pagesLesson Plan On PhysiologicalruchiNo ratings yet
- Practical Application of CPAP: Dr. Srinivas MurkiDocument8 pagesPractical Application of CPAP: Dr. Srinivas MurkiRaji MohanNo ratings yet
- Ventilation in ARDS: Mechanical Ventilation For COVID-19Document13 pagesVentilation in ARDS: Mechanical Ventilation For COVID-19Praveen TagoreNo ratings yet
- OXYTOCINDocument3 pagesOXYTOCINJaye Aprile Adrianne KuizonNo ratings yet
- Anaesthetics NotesDocument15 pagesAnaesthetics NotesnaNo ratings yet
- Pregnancy Induced Hypertension Joseph JanDocument11 pagesPregnancy Induced Hypertension Joseph JanJan Joseph BanzuelaNo ratings yet
- P I H J A NDocument14 pagesP I H J A NJan Joseph BanzuelaNo ratings yet
- From Liquid To Air: Breathing After Birth: A B. P, MD, P G. D, MD, S B. H, P D, C J. M, MDDocument5 pagesFrom Liquid To Air: Breathing After Birth: A B. P, MD, P G. D, MD, S B. H, P D, C J. M, MDmaria jose amayaNo ratings yet
- CPCR NewDocument30 pagesCPCR NewPhil PhilipsNo ratings yet
- Adaptasi Fisiologi Selama KehamilanDocument39 pagesAdaptasi Fisiologi Selama KehamilanKevin NugrohoNo ratings yet
- Respiratory Monitoring in Mechanical Ventilation: Techniques and ApplicationsFrom EverandRespiratory Monitoring in Mechanical Ventilation: Techniques and ApplicationsJian-Xin ZhouNo ratings yet
- Abnormal Labor, Dystocia IIDocument9 pagesAbnormal Labor, Dystocia IIIke RilleraNo ratings yet
- "A Fun Hazily Snail Barn-Aftermaster": Neisseria Gonorrhea and Chlamydia TrachomatisDocument3 pages"A Fun Hazily Snail Barn-Aftermaster": Neisseria Gonorrhea and Chlamydia TrachomatisIke Rillera100% (1)
- JaundiceDocument25 pagesJaundiceIke RilleraNo ratings yet
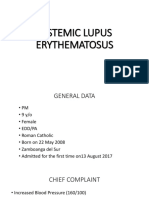
- Systemic Lupus ErythematosusDocument89 pagesSystemic Lupus ErythematosusIke RilleraNo ratings yet
- Treatment For Central Pain Syndrome 2007Document0 pagesTreatment For Central Pain Syndrome 2007Merari Lugo OcañaNo ratings yet
- Praktikum Epid AriDocument119 pagesPraktikum Epid AriFaisal Ahmad100% (1)
- Chiropractic and Physical Therapies (PDFDrive)Document279 pagesChiropractic and Physical Therapies (PDFDrive)Pierre NotserNo ratings yet
- SurvivalDocument61 pagesSurvivalsgod34No ratings yet
- DialogDocument2 pagesDialogolga millatNo ratings yet
- Clinical Guidelines For The Use of Granulocyte TransfusionsDocument13 pagesClinical Guidelines For The Use of Granulocyte Transfusionssm19790% (1)
- Microbiologist: 3.1.5 Isolation & Gram StainingDocument5 pagesMicrobiologist: 3.1.5 Isolation & Gram Stainingapi-534896073No ratings yet
- El Papiro de Edwin Smith y Su TrascendenDocument6 pagesEl Papiro de Edwin Smith y Su TrascendenSebastian PintoNo ratings yet
- AnesthesiaDocument26 pagesAnesthesiaezkina14No ratings yet
- International Journal of Pediatric Research Ijpr 9 113Document4 pagesInternational Journal of Pediatric Research Ijpr 9 113VsbshNo ratings yet
- The Mental Workload of Nurses in The Role of Nursing Care ProvidersDocument8 pagesThe Mental Workload of Nurses in The Role of Nursing Care ProvidersDede NunuNo ratings yet
- Elobest Kporon 2019Document88 pagesElobest Kporon 2019JENNIFER ENEKWECHINo ratings yet
- PROBIÓTICOSDocument5 pagesPROBIÓTICOSstephanielopes2020No ratings yet
- Hajj Health Requirements English LanguageDocument8 pagesHajj Health Requirements English Languageelis suryaniNo ratings yet
- Romano Et Al-2024-Cochrane Database of Systematic ReviewsDocument111 pagesRomano Et Al-2024-Cochrane Database of Systematic Reviewsaraujoaoh07No ratings yet
- Shortage of Medication ArgumentDocument5 pagesShortage of Medication Argumentapi-543490444No ratings yet
- Epid 1.1Document194 pagesEpid 1.1devtarioNo ratings yet
- Jurnal 1Document8 pagesJurnal 1meira audriNo ratings yet
- HerbalismDocument15 pagesHerbalismTee R Taylor100% (1)
- ResumeDocument5 pagesResumeJuvie Dawn MaquilanNo ratings yet
- Gotthard Bulau Closed Water-Seal Drainage For Empyema,: John A. MeyerDocument3 pagesGotthard Bulau Closed Water-Seal Drainage For Empyema,: John A. Meyerputri aprilianiNo ratings yet
- NCAA Concussion Fact SheetDocument2 pagesNCAA Concussion Fact Sheetelijah edwardsNo ratings yet
- KOREA Magazine (MARCH 2012 VOL. 9 NO. 3)Document29 pagesKOREA Magazine (MARCH 2012 VOL. 9 NO. 3)Republic of Korea (Korea.net)100% (1)
- Intravenous InfusionDocument9 pagesIntravenous InfusionMarina MuradNo ratings yet
- Putney Rehab Centre TimetableDocument2 pagesPutney Rehab Centre Timetableapi-280584977No ratings yet
- Hypersensitivity 2Document3 pagesHypersensitivity 2kuldip.biotechNo ratings yet
- Zhang 2021Document8 pagesZhang 2021Magna Fitriani HutasuhutNo ratings yet
- Orientation ResidenecyDocument18 pagesOrientation ResidenecyReeMii AngeLa100% (1)
- Parents Consent AY 2022 2023Document2 pagesParents Consent AY 2022 2023Jayloid AlteaNo ratings yet
- MO Durable Power of AttorneyDocument16 pagesMO Durable Power of Attorneytlayton223No ratings yet