Professional Documents
Culture Documents
Maat 07 I 3 P 269
Uploaded by
turi gauOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Maat 07 I 3 P 269
Uploaded by
turi gauCopyright:
Available Formats
Emergency Medicine
Management of Respiratory Distress in the Newborn
Surg Cdr SS Mathai*, Col U Raju+, Col M Kanitkar#
MJAFI 2007; 63 : 269-272
Key Words : Respiratory distress; Newborn
Introduction Pathophysiology Unique to Newborn
R espiratory distress is a common emergency
responsible for 30-40% of admissions in the neonatal period
Prolonged and unattended distress leads to
hypoxaemia, hypercarbia and acidosis. These
[1]. A working diagnosis should be made in the first few causes lead to pulmonary vasoconstriction and
minutes of seeing the baby and immediate life-saving
measures should be undertaken till further persistence of foetal circulation with right to left
management plans are drawn up. shunting through the ductus and foramen ovale,
Respiratory distress in the neonate is diagnosed when thereby aggravating hypoxaemia which leads to
one or more of the following is present; tachypnoea or multi system organ dysfunction.
respiratory rate of more than 60/minute, retractions or An audible grunt (forced expiratory sound) is an
increased chest in drawings on respirations (subcostal, important sign of pulmonary pathology in the newborn
intercostal, sternal, suprasternal) and noisy respiration in indicating that the baby has a low lung volume or
the form of a grunt, stridor or wheeze[1]. The distress functional residual capacity (FRC). Breathing against a
may or may not be associated with cyanosis and partially closed glottis increases the FRC of the baby and
desaturation on pulse oximetry. The common causes of helps keep the alveoli patent. This is characteristically
respiratory distress in the neonate are: seen in a baby with HMD where surfactant deficiency
1. Hyaline Membrane Disease (HMD) tends to keep the alveoli collapsed during expiration.
Indiscriminately inserting an endotracheal (ET) tube
2. Meconium Aspiration Syndrome (MAS) without giving positive end expiratory pressure (PEEP)
3. Transient Tachypnoea of the Newborn (TTNB) to a neonate who is grunting will deprive the baby of this
4. Congenital or acquired pneumonia physiological effect and worsen rather than improve his
5. Persistent Pulmonary Hypertension of the condition. Hence any baby who is grunting should either
Newborn (PPHN) be given continuous positive airway pressure (CPAP) or
intubated and put on ventilator support, but never left to
6. Air leaks
breathe spontaneously with a tube in situ.
7. Congenital anomalies of upper airway (choanal
atresia), gut (tracheoesophageal fistula, congenital
diaphragmatic hernia) or lungs (lobar emphysema,
Grading of Distress Severity
congenital cystic adenomatoid malformation, cysts) The severity of respiratory distress is assessed by
8. Cardiac shock or Congenital Heart Disease (CHD). Silverman- Anderson Score and Downes’ Score. While
the Silverman Anderson Retraction Score is more suited
9. Haematological causes (severe anaemia, for preterms with HMD, the Downes’ Score is more
polycythaemia) comprehensive and can be applied to any gestational age
10. Neurological causes leading to hyperventilation and condition. Scoring should be done at half hourly
like seizures intervals and a chart maintained to determine progress
11. Metabolic causes- Inborn Errors of Metabolism (Tables 1,2). A progressively increasing FiO 2
(IEM) requirement to maintain a saturation of 90-92% in a
preterm and 94-96% in a term baby is also a sensitive
indicator of the severity and progress of distress.
*
Associate Professor, # Professor and Head (Department of Paediatrics ), Armed Forces Medical College, Pune. +Senior Advisor (Paediatrics
& Neonatology), Command Hospital (Southern Command), Pune.
Received : 04.08.2006; Accepted : 25.01.2007
270 Mathai, Raju and Kanitkar
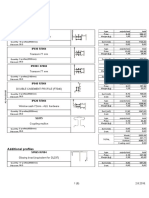
Table 1 For babies presenting later with distress we have
Silverman Anderson retraction score [2] to ask a few other questions :-
Score Upper Lower Xiphoid Nasal Grunt a) Is the distress associated with feed refusal and
chest chest retraction dilatation
retraction retraction lethargy? (sepsis, pneumonia)
0 Synch None None None None b) Did the distress appear slowly after starting
1 Lag on Just Just Minimal Stethoscope feeds? (IEM).
inspiration visible visible only
c) Is there a family history of early neonatal
2 See-Saw Marked Marked Marked Naked ear
deaths? (CHD, IEM).
A score of >6 is indicative of impending respiratory failure.
The algorithm shown in Fig.1, helps in reaching a
Table 2 working aetiological diagnosis [4].
Downes’ score [3] Clinical Examination
Score Respiratory Cyanosis Air Grunt Retraction Clues to the likely aetiology can be picked up on
rate entry
examination of the neonate
0 <60/min Nil Normal None Nil
1 60- In room Mild Ausc Mild
1. A preterm baby weighing <1500 gms with
80/min air with retractions and grunt is likely to have HMD.
stethoscope
2. A term baby born through meconium stained
2 >80/min In >40% Marked Audible Moderate
with amniotic fluid with an increase in the anterior-
naked ear posterior diameter of the chest (full chest) is
A score of >6 is indicative of impending respiratory failure. likely to be suffering from MAS.
3. A depressed baby with poor circulation is likely
Besides assessing the severity of the distress it is to have neonatal sepsis with or without
essential to determine the underlying pathology for congenital pneumonia.
further management. For a new born baby (within 4. A near term baby with no risk factors and mild
few hours of birth) with respiratory distress, a quick distress may have TTNB.
review of the following antenatal and peripartum 5. An asphyxiated baby may have PPHN.
events including the condition at birth is a must :-
6. A growth retarded baby with a plethoric look
a) Were there any risk factors in the antepartum
may have polycythaemia.
period or evidence of foetal distress prior to
delivery? (Birth asphyxia or PPHN) 7. A baby with respiratory distress should be
checked for an air leak by placing a cold light
b) Did the mother receive antenatal steroids if it
source over the chest wall in a darkened room.
was a preterm delivery? (Antenatal steroids
8. A baby presenting with tachypnoea and a cardiac
decrease the incidence of HMD by 50%)
murmur may have a congenital heart disease.
c) Was there a history of premature rupture of
9. Inability to pass an 5F catheter through the nostril of
membranes and fever? (congenital pneumonia
or sepsis) a term baby is suggestive of choanal atresia.
d) Was there meconium stained amniotic fluid? Investigations
(MAS is a possibility) Essential investigations for all cases of neonatal
e) A look at the antenatal ultrasonography (USG) for Respiratory
the amount of amniotic fluid would tell us the status Distress
(tachypnoea, retractions, grunt
of the foetal lung. (congenital anomalies of lung)
f) Was resuscitation required at birth? Preterm Term
(resuscitation trauma/PPHN/ acidosis)
g) Did the distress appear immediately or a few hours < 6hrs old > 6hrs old < 6hrs old > 6hrs old
after birth? (HMD appears earlier than pneumonia)
HMD Pneumonia TTNB Pneumonia
h) Was it related to feeding or frothing at the mouth? Pneumonia CHD MAS/PPHN Polycythaemia
Lung Pulmonary Asphyxia, Shock CHD
(tracheo-esophageal fistula or aspiration) Anamoly Haemorrhage Lung Anamoly
Shock Air leak
i) Does the distress decrease with crying? (choanal
atresia).
Fig. 1 : Diagnostic approach to respiratory distress
MJAFI, Vol. 63, No. 3, 2007
Respiratory Distress In The Newborn 271
respiratory distress include chest radiograph with an 4. Fluid and electrolyte management: Electrolyte
orogastric tube in situ, arterial blood gas (ABG) analysis balance, fluids, calcium and glucose homeostasis are
(Table 3), sepsis screen including C-reactive protein, all equally important. Fluids are usually started at a
µ ESR, white blood cell count, peripheral smear for toxic minimum of 60ml/kg/day of 10% D or three fourth
granules, blood culture, surface swab culture (where of daily maintenance whichever is more. This will
indicated), maternal vaginal swab, blood glucose, serum ensure a glucose infusion rate of about 4 mg/kg/min
calcium and central haematocrit assessment. which is the minimum required for adequate glucose
A score of 3 or more on the ABG indicates the need homeostasis. Calcium in the dose of 6-8 ml/kg/day
for CPAP or mechanical ventilation. A pH of <7.2 with of calcium gluconate should be added to the fluid in
hypercarbia (pCO2>60mm) or a pO2<50mm Hg in FiO2 all preterms and term babies.
of 0.8 is suggestive of frank respiratory failure. 5. Maintenance of adequate haemoglobin: Any neonate
Treatment with respiratory distress should have a packed cell
1. Clearing of airway, ensuring adequate breathing and volume (PCV) above 40% (but less than 75%).
circulation are the first line of management. A baby 6. All preterm babies with respiratory distress should be
in obvious respiratory distress needs to be on started on broad spectrum antibiotics. In term babies,
continuous pulse oximeter monitoring to decide decision to start antibiotics would depend on the
when intubation and ventilation is required. clinical situation, but the threshold should be low.
2. Warm, humidified oxygen is given with a head box, Role of Surfactant
preferably with a FiO2 meter and pulse oximeter Surfactant is the drug of choice in a baby with HMD.
monitoring to determine the amount of oxygen This may be given either prophylactically if the baby is
required. Soft nasal cannulae may also be used to less than 28 weeks of gestation or within the first two
give oxygen. Small changes in FiO2 are made and hours of onset of symptoms in older babies [7,8].
monitored on the pulse oximeter. Oxygen should be Prophylactic surfactant is given in the labour room after
given in the correct dose, as it is toxic to preterm the baby has been stabilized. Rescue therapy is most
neonates and the suggested guidelines are given in effective if given within the first two hours of birth.
Table 4. The “30-60-90” rule is a useful bedside Presently both natural and synthetic surfactants are being
indicator when using the pulse oximeter. This means marketed in India. Surfactant is given in a dose of 100
that at a saturation of 90% the paO2 is around mg/kg through the endotracheal tube in small aliquots
60mmHg and at 60% it is around 30 mmHg in a with intermittent bagging to prevent desaturation during
newborn. This is due to high HbF in neonatal blood administration and it should be followed by ventilatory
which causes the left shift of oxygen dissociation support.
curve. At saturation of 90-95%, the paO 2 may be Respiratory Support
between 60 to 98mm Hg and above 95% saturation,
Respiratory support is given in the form of continuous
paO2 is well above 100mmHg. positive airway pressure (CPAP) or intermittent
3. Maintenance of correct temperature is essential. mandatory ventilation (IMV). Short nasal or longer
HMD and PPHN are aggravated by hypothermia. nasopharyngeal prongs are preferred to endotracheal
CPAP as latter markedly increases the work of breathing
Table 3 and tires the infant. CPAP should be started early in a
ABG score preterm with HMD. Indications for starting CPAP are a
Points Downes’ or Silvermann score of >6 at birth or a FiO 2
0 1 2 3 requirement of >0.4 to maintain an acceptable saturation
paO2 mmHg > 60 50-60 < 50 < 50 on pulse oximeter. ABG score of more than 3 is also
pH > 7.3 7.20-7.29 7.1-7.19 < 7.1 acceptable. CPAP is a gentler form of non-invasive
paCO2 mmHg < 50 50-60 61-70 > 70 ventilatory support as compared to IMV [6].
Score of > 3 suggestive of ventilatory support requirement IMV: Time cycled pressure limited ventilation is the
modality of choice for ventilation of a neonate in
Table 4
respiratory failure. If patient triggered ventilation is used
Guidelines for monitoring oxygen saturation levels by pulse
oximetry it is given as synchronized intermittent mandatory
ventilation (SIMV) or assist control mode ventilation
>95% Term baby, pulmonary hypertension (PPHN)
88-94% 28-34 weeks preterm
(ACMV). For best outcomes this should be given to
85-92% Below 28 weeks gestational age babies in impending respiratory failure or failed CPAP
MJAFI, Vol. 63, No. 3, 2007
272 Mathai, Raju and Kanitkar
rather than in complete respiratory failure [5]. Resistant
apnoea is also an absolute indication. CPAP is said to
have failed when the FiO 2 requirement is >0.6 or the
pressure required to maintain oxygenation exceeds 7-8
cm of H2O. Respiratory failure is defined a paCO 2
>60mm or paO2 < 50 mm or saturation < 85% in 100%
O2 with or without a pH of <7.25. A working algorithm
for ventilatory support is given in Fig. 2.
Fig. 2 : Algorithm for ventilatory support
Outcome
With good intensive care in a neonatal intensive care 4. Greenough A, Roberton NRC. Acute respiratory disease in the
unit the outcome of neonates with respiratory distress has newborn. In: JM Rennie editors.Textbook of Neonatology. 4th
ed. China:Churchill Livingstone, 2005: 512-7.
improved remarkably in the past decade with a survival
5. Goldsmith JP, Karotkin EH. Introduction to mechanical
rate of > 60% in babies weighing > 1 kg [9].
ventilation. . In : Goldsmith JP, Karotkin EH, editors. Assisted
Conflicts of Interest Ventilation of the Newborn. 3rd ed. Philadelphia: WB
Saunders, 2003:161-72.
None identified
6. Upadhyay A, Deorari AK. Continuous positive airway
References pressure - a gentler approach to ventilation. Indian Pediatr
1. NNF Recommended Basic Perinatal-Neonatal Nomenclature. 2004 ;41:459-69.
In: DK Guha, editors. Neonatology- Principles and Practice. 7. Suresh GK, Soll RF. Current surfactant use in premature
1st ed. New Delhi : Jaypee Brothers, 1998: 131-2. infants. Clin Perinatol 2001; 28: 671-93.
2. Silverman WC, Anderson DH. Controlled clinical trial on 8. Stevens TP, Blennow M, Soll RF. Early surfactant
effects of water mist on obstructive respiratory signs, death administration with brief ventilation vs. selective surfactant
rate and necropsy findings among premature infants. and continued mechanical ventilation for preterm infants with
Pediatrics 1956; 17: 1-4. or at risk for respiratory distress syndrome. Cochrane
3. Wood DW, Downes’ JJ, Locks HI. A clinical score for the Database Syst Rev 2004; 3:CD003063.
diagnosis of respiratory failure. Amer J Dis Child 1972; 123: 9. Mathur NB, Garg P, Mishra TK. Predictors of fatality in
227-9. neonates requiring mechanical ventilation. Indian Pediatrics
2005; 42:645-51.
MJAFI, Vol. 63, No.
3, 2007
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Football Trading StrategyDocument27 pagesFootball Trading StrategyChem100% (2)
- MCQ On ErgonomicsDocument4 pagesMCQ On Ergonomicszoom milind67% (3)
- ENVSOCTY 1HA3 - Lecture 01 - Introduction & Course Overview - Skeletal NotesDocument28 pagesENVSOCTY 1HA3 - Lecture 01 - Introduction & Course Overview - Skeletal NotesluxsunNo ratings yet
- QUARTER 3, WEEK 9 ENGLISH Inkay - PeraltaDocument43 pagesQUARTER 3, WEEK 9 ENGLISH Inkay - PeraltaPatrick EdrosoloNo ratings yet
- A User's Guide To Capitalism and Schizophrenia Deviations From Deleuze and GuattariDocument334 pagesA User's Guide To Capitalism and Schizophrenia Deviations From Deleuze and Guattariapi-3857490100% (6)
- Daftarr PustakaDocument1 pageDaftarr Pustakaturi gauNo ratings yet
- The Evolution of Interventional RadiologyDocument4 pagesThe Evolution of Interventional Radiologyturi gauNo ratings yet
- The Evolution of Interventional RadiologyDocument4 pagesThe Evolution of Interventional Radiologyturi gauNo ratings yet
- 27e99e17d7fe8d43b1cad5c342b7c41aDocument5 pages27e99e17d7fe8d43b1cad5c342b7c41aturi gauNo ratings yet
- Varying Response Effort in The Treatment of Pica Maintained by Automatic ReinforcementDocument14 pagesVarying Response Effort in The Treatment of Pica Maintained by Automatic Reinforcementturi gauNo ratings yet
- Pica in An Adolescent With Autism Spectrum Disorder Responsive To AripiprazoleDocument3 pagesPica in An Adolescent With Autism Spectrum Disorder Responsive To Aripiprazoleturi gauNo ratings yet
- Upanikhat-I Garbha A Mughal Translation PDFDocument18 pagesUpanikhat-I Garbha A Mughal Translation PDFReginaldoJurandyrdeMatosNo ratings yet
- Radio Protection ChallengesDocument31 pagesRadio Protection ChallengesJackssonNo ratings yet
- MNT-Notes Pt. 2Document58 pagesMNT-Notes Pt. 2leemon.mary.alipao8695No ratings yet
- K Unit 1 SeptemberDocument2 pagesK Unit 1 Septemberapi-169447826No ratings yet
- XS2 Pharma 0512 103 UK U-NiDocument2 pagesXS2 Pharma 0512 103 UK U-NiMilan MilovanovicNo ratings yet
- The Christ of NankingDocument7 pagesThe Christ of NankingCarlos PérezNo ratings yet
- Kingdom AnimaliaDocument13 pagesKingdom AnimaliaAryanNo ratings yet
- 580 People vs. Verzola, G.R. No. L-35022Document2 pages580 People vs. Verzola, G.R. No. L-35022Jellianne PestanasNo ratings yet
- Rosa Chavez Rhetorical AnalysisDocument7 pagesRosa Chavez Rhetorical Analysisapi-264005728No ratings yet
- The Passive Aggressive Disorder PDFDocument13 pagesThe Passive Aggressive Disorder PDFPhany Ezail UdudecNo ratings yet
- Manasvi Lingam, Avi Loeb - Life in The Cosmos - From Biosignatures To Technosignatures-Harvard University Press (2021)Document1,082 pagesManasvi Lingam, Avi Loeb - Life in The Cosmos - From Biosignatures To Technosignatures-Harvard University Press (2021)Shahwaiz NiaziNo ratings yet
- Songs of KabirDocument342 pagesSongs of KabirSant MatNo ratings yet
- The Court of Heaven 1Document2 pagesThe Court of Heaven 1Rhoda Collins100% (7)
- The Interplay of Religion and PoliticsDocument10 pagesThe Interplay of Religion and PoliticsThompson mercyNo ratings yet
- Simple Past Story 1Document7 pagesSimple Past Story 1Ummi Umarah50% (2)
- Assignment in Legal CounselingDocument4 pagesAssignment in Legal CounselingEmmagine E EyanaNo ratings yet
- Sepulveda v. de Las CasasDocument2 pagesSepulveda v. de Las CasasNova GaveNo ratings yet
- A Terence McKenna Audio Archive - Part 1Document203 pagesA Terence McKenna Audio Archive - Part 1BabaYagaNo ratings yet
- Lista Materijala WordDocument8 pagesLista Materijala WordAdis MacanovicNo ratings yet
- Remo Vs DevanaderaDocument2 pagesRemo Vs DevanaderaZymon Andrew MaquintoNo ratings yet
- t10 2010 Jun QDocument10 pagest10 2010 Jun QAjay TakiarNo ratings yet
- Deborah Schiffrin .Tense Variation in NarrativeDocument19 pagesDeborah Schiffrin .Tense Variation in Narrativealwan61No ratings yet
- A Scoping Literature Review of The Provision of Orthoses and Prostheses in Resource-Limited Environments 2000-2010. Part Two: Research and OutcomesDocument20 pagesA Scoping Literature Review of The Provision of Orthoses and Prostheses in Resource-Limited Environments 2000-2010. Part Two: Research and OutcomesGufron Abu MufadholNo ratings yet
- Pi 100 Book ReviewDocument10 pagesPi 100 Book ReviewBianca CacnioNo ratings yet
- NUR 200 Week 7 Practice Case StudyDocument2 pagesNUR 200 Week 7 Practice Case StudyJB NicoleNo ratings yet