Professional Documents
Culture Documents
Cardiac NSG Diagnosis
Uploaded by
Shreyas Walvekar0 ratings0% found this document useful (0 votes)
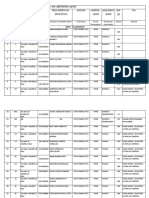
44 views5 pages1) The document discusses several potential nursing diagnoses for patients recovering from cardiac surgery or with cardiac conditions including risks for decreased cardiac output, acute pain, ineffective breathing patterns, impaired skin integrity, and deficient knowledge.
2) It also discusses nursing diagnoses for conditions like thromboembolism including ineffective peripheral tissue perfusion, acute pain, and impaired gas exchange.
3) For COPD patients, nursing diagnoses addressed include ineffective airway clearance, impaired gas exchange, imbalanced nutrition, and ineffective self-health management.
4) For heart failure, nursing diagnoses include decreased cardiac output, activity intolerance, and excess fluid volume. The document provides risk factors and desired outcomes for each diagnosis.
Original Description:
imp
Original Title
Cardiac Nsg Diagnosis
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Document1) The document discusses several potential nursing diagnoses for patients recovering from cardiac surgery or with cardiac conditions including risks for decreased cardiac output, acute pain, ineffective breathing patterns, impaired skin integrity, and deficient knowledge.
2) It also discusses nursing diagnoses for conditions like thromboembolism including ineffective peripheral tissue perfusion, acute pain, and impaired gas exchange.
3) For COPD patients, nursing diagnoses addressed include ineffective airway clearance, impaired gas exchange, imbalanced nutrition, and ineffective self-health management.
4) For heart failure, nursing diagnoses include decreased cardiac output, activity intolerance, and excess fluid volume. The document provides risk factors and desired outcomes for each diagnosis.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
44 views5 pagesCardiac NSG Diagnosis
Uploaded by
Shreyas Walvekar1) The document discusses several potential nursing diagnoses for patients recovering from cardiac surgery or with cardiac conditions including risks for decreased cardiac output, acute pain, ineffective breathing patterns, impaired skin integrity, and deficient knowledge.
2) It also discusses nursing diagnoses for conditions like thromboembolism including ineffective peripheral tissue perfusion, acute pain, and impaired gas exchange.
3) For COPD patients, nursing diagnoses addressed include ineffective airway clearance, impaired gas exchange, imbalanced nutrition, and ineffective self-health management.
4) For heart failure, nursing diagnoses include decreased cardiac output, activity intolerance, and excess fluid volume. The document provides risk factors and desired outcomes for each diagnosis.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 5
CARDIAC SURGERY: POSTOPERATIVE CARE—CORONARY ARTERY BYPASS GRAFT (CABG), MINIMALLY
INVASIVE DIRECT CORONARY ARTERY BYPASS (MIDCAB), CARDIOMYOPLASTY, VALVE REPLACEMENT
NURSING DIAGNOSIS: risk for decreased Cardiac Output Risk Factors
May Include Altered contractility recent Altered preload—hypovolemia; altered afterload—systemic
vascular resistance Altered heart rate/rhythm
Possibly Evidenced By (Not applicable; presence of signs and symptoms establishes an actual
diagnosis)
Desired Outcomes/Evaluation Criteria—Client Will
Tissue Perfusion: Cardiac Display hemodynamic stability, such as stable blood pressure, cardiac
output. Report and display decreased episodes of angina and dysrhythmias. Demonstrate an
increase in activity tolerance. Participate in activities that maximize and enhance cardiac function.
NURSING DIAGNOSIS: acute Pain
May Be Related To
Injuring physical agents—surgical incisions, tissue inflammation, edema formation, intraoperative nerve trauma
Possibly Evidenced By
Verbal/coded reports of pain
Guarding behavior
Expressive behaviors—restlessness, irritability
Changes in heart rate, blood pressure, respiratory rate
Desired Outcomes/Evaluation Criteria—Client Will
Pain Level
Verbalize relief or absence of pain.
Demonstrate relaxed body posture and ability to rest and sleep appropriately.
Pain Control
Differentiate surgical discomfort from angina or preoperative heart pain.
NURSING DIAGNOSIS: risk for ineffective Breathing Pattern
Risk Factors May Include
Pain
Musculoskeletal impairment
Possibly Evidenced By
(Not applicable; presence of signs and symptoms establishes an actual diagnosis)
Desired Outcomes/Evaluation Criteria—Client Will
Respiratory Status: Ventilation
Maintain an effective respiratory pattern free of cyanosis and other signs and symptoms of hypoxia, with breath sounds equal
bilaterally, lung fields clearing.
Display complete reexpansion of lungs with absence of pneumothorax and hemothorax.
NURSING DIAGNOSIS: impaired Skin/Tissue Integrity
May Be Related To
Mechanical factors (e.g., surgery)
Possibly Evidenced By
Disruption of skin surface/damaged tissue [surgical incisions, puncture wounds]
Desired Outcomes/Evaluation Criteria—Client Will
Wound Healing: Primary Intention
Demonstrate behaviors and techniques to promote healing and prevent complications.
Display timely wound healing.
NURSING DIAGNOSIS: deficient Knowledge [Learning Need] regarding condition,
postoperative care, self-care, and discharge needs
May Be Related To
Lack of exposure or recall
Information misinterpretation
Possibly Evidenced By
Reports the problem
Inaccurate follow-through of instructions
Desired Outcomes/Evaluation Criteria—Client Will
Self-Management: Cardiac Disease
Participate in learning process.
Assume responsibility for own learning.
Begin to ask questions and look for information.
Knowledge: Treatment Regimen
Verbalize understanding of condition, prognosis, and potential complications.
THROMBOPHLEBITIS: VENOUS
THROMBOEMBOLISM (INCLUDING
PULMONARY EMBOLI CONSIDERATIONS)
NURSING DIAGNOSIS: ineffective peripheral tissue Perfusion
May Be Related To
Deficient knowledge of aggravating factors—sedentary lifestyle/immobility, trauma, smoking, obesity
Possibly Evidenced By
Edema, extremity pain
Diminished pulses, capillary refill >3 seconds
Altered skin characteristics—color, temperature
Desired Outcomes/Evaluation Criteria—Client Will
Tissue Perfusion: Peripheral
Demonstrate improved perfusion as evidenced by peripheral pulses present, equal skin color, and temperature normal and
absence of edema.
Engage in behaviors or actions to enhance tissue perfusion.
Display increasing tolerance to activity.
NURSING DIAGNOSIS: acute Pain
May Be Related To
Injury agent—physical (inflammatory process); chemical (accumulation of lactic acid in tissues)
Possibly Evidenced By
Reports pain
Guarding behavior
Expressive behaviors—restlessness
Desired Outcomes/Evaluation Criteria—Client Will
Pain Control
Report that pain or discomfort is alleviated or controlled.
Verbalize methods that provide relief.
Display relaxed manner; be able to sleep or rest and engage in desired activity.
NURSING DIAGNOSIS: impaired Gas Exchange (in presence of Pulmonary
Embolus)
May Be Related To
Ventilation-perfusion imbalance [altered blood flow to alveoli or to major portions of the lung]
Alveolar-capillary membrane changes
Possibly Evidenced By
Dyspnea, restlessness, [apprehension], somnolence
Abnormal arterial blood gases, hypoxemia, hypercapnia
Desired Outcomes/Evaluation Criteria—Client Will
Respiratory Status: Gas Exchange
Demonstrate adequate ventilation and oxygenation by ABGs within client’s normal range.
Report or display resolution or absence of symptoms of respiratory distress.
NURSING DIAGNOSIS: deficientKnowledge [Learning Need] regarding condition,
treatment program, self-care, and discharge needs
May Be Related To
Lack of exposure or recall
Misinterpretation of information
Unfamiliarity with information resources
Possibly Evidenced By
Reports the problem
Inaccurate follow-through of instructions
Desired Outcomes/Evaluation Criteria—Client Will
Knowledge: Thrombus Prevention
Verbalize understanding of disease process, treatment regimen, and limitations.
Participate in learning process.
Identify signs and symptoms requiring medical evaluation.
Correctly perform therapeutic actions and explain reasons for actions.
COPD
NURSING DIAGNOSIS: ineffective Airway Clearance
May Be Related To
Chronic obstructive pulmonary disease
Airway spasm, allergic airways
Excessive mucus, retained secretions, exudates in the alveoli
Smoking/secondhand smoke
Possibly Evidenced By
Dyspnea, difficulty vocalizing
Changes in depth and rate of respirations
Diminished/adventitious breath [wheezes, rhonchi, crackles]
Absent/ineffective cough
Restlessness, cyanosis
Desired Outcomes/Evaluation Criteria—Client Will
Respiratory Status: Airway Patency
Maintain patent airway with breath sounds clear or clearing.
Demonstrate behaviors to improve airway clearance.
NURSING DIAGNOSIS: impaired Gas Exchange
May Be Related To
Ventilation-perfusion imbalance [retained secretions, bronchospasm, air-trapping]
Alveolar-capillary membrane changes
Possibly Evidenced By
Dyspnea
Confusion, restlessness
Abnormal breathing (e.g., rate, rhythm, depth); tachycardia
Abnormal ABGs—hypoxia, hypercapnia
Nasal flaring; abnormal skin color (e.g., pale, dusky)
Reduced tolerance for activity
Desired Outcomes/Evaluation Criteria—Client Will
Respiratory Status: Gas Exchange
Demonstrate improved ventilation and adequate oxygenation of tissues by ABGs within client’s normal range and be free
of symptoms of respiratory distress.
Participate in treatment regimen within level of ability and situation.
NURSING DIAGNOSIS: imbalanced Nutrition: less than body requirements
May Be Related To
Biological factors—dyspnea; medication side effects; anorexia, nausea or vomiting; fatigue
Possibly Evidenced By
Body weight 20% or more under ideal; poor muscle tone
Reported altered taste sensation, aversion to eating, lack of interest in food
Desired Outcomes/Evaluation Criteria—Client Will
Nutritional Status
Display progressive weight gain toward goal as appropriate.
Demonstrate behaviors and lifestyle changes to regain and maintain appropriate weight
NURSING DIAGNOSIS: ineffective Self-Health Management
May Be Related To
Deficient knowledge; complexity of therapeutic regimen
Economic difficulties
Perceived benefits/seriousness
Possibly Evidenced By
Reports difficulty with prescribed regimen
Failure to include treatment regimens in daily living
Failure to take action to reduce risk factors
Self-Management: Chronic Obstructive Pulmonary Disease/Asthma Management
Verbalize understanding of condition and disease process and treatment.
Identify relationship of current signs and symptoms to the disease process and correlate these with causative factors.
Initiate necessary lifestyle changes and participate in treatment regimen.
HEART FAILURE: CHRONIC
NURSING DIAGNOSIS: decreased Cardiac Output
May Be Related To
Altered contractility (such as valvular defects and ventricular aneurysm)
Altered heart rate, rhythm
Altered afterload (vascular resistence)
Possibly Evidenced By
Tachycardia, arrhythmias, ECG changes
Variations in blood pressure readings (hypotension, hypertension)
Decreased peripheral pulses
S3, S4 heart sounds
Orthopnea, crackles, jugular vein distension, edema, weight gain
Skin color changes, clammy skin
Oliguria
Desired Outcomes/Evaluation Criteria—Client Will
Cardiac Pump Effectiveness
Display vital signs within acceptable limits, dysrhythmias absent or controlled, and no symptoms of failure, for example,
hemodynamic parameters within acceptable limits and urinary output adequate.
Report decreased episodes of dyspnea and angina.
Cardiac Disease Self-Management
Participate in activities that reduce cardiac workload.
NURSING DIAGNOSIS: Activity Intolerance
May Be Related To
Imbalance between oxygen supply and demand
Generalized weakness
Sedentary lifestyle
Possibly Evidenced By
Reports fatigue, feeling weak
Abnormal blood pressure/heart rate in response to activity
Exertional dyspnea
Desired Outcomes/Evaluation Criteria—Client Will
Endurance
Participate in desired activities; meet own self-care needs.
Achieve measurable increase in activity tolerance, evidenced by reduced fatigue and weakness and by vital signs within
acceptable
limits during activity.
NURSING DIAGNOSIS: excess Fluid Volume
May Be Related To
Compromised regulatory mechanism (reduced glomerular filtration rate, increased antidiuretic hormone [ADH] production, and
sodium and water retention)
Excess sodium intake
Possibly Evidenced By
Orthopnea, S3 heart sound
Oliguria, edema, JVD, positive hepatojugular reflex
Weight gain over short period of time
Blood pressure changes
Pulmonary congestion, adventitious breath sounds
Desired Outcomes/Evaluation Criteria—Client Will
Fluid Overload Severity
Demonstrate stabilized fluid volume with balanced intake and output, breath sounds clear or clearing, vital signs within
acceptable
range, stable weight, and absence of edema.
Verbalize understanding of individual dietary and fluid restrictions.
NURSING DIAGNOSIS: risk for impaired Gas Exchange
Risk Factors May Include
Alveolar-capillary membrane changes such as fluid collection and shifts into interstitial space or alveoli
Possibly Evidenced By
(Not applicable; presence of signs and symptoms establishes an actual diagnosis)
Desired Outcomes/Evaluation Criteria—Client Will
Respiratory Status: Gas Exchange
Demonstrate adequate ventilation and oxygenation of tissues by ABG values and oximetry within client’s normal ranges and be
free of symptoms of respiratory distress.
Participate in treatment regimen within level of ability and situation.
NURSING DIAGNOSIS: risk for chronic Pain
Risk Factors May Include
Chronic physical disease or condition
Altered ability to continue previous activities
Possibly Evidenced By
(Not applicable; presence of signs and symptoms establishes an actual diagnosis)
Desired Outcomes/Evaluation Criteria—Client Will
Pain Control
Verbalize and demonstrate relief or control of pain or discomfort.
Demonstrate and initiate behavioral modifications of lifestyle and appropriate use of therapeutic interventions
NURSING DIAGNOSIS: risk for Impaired Skin Integrity
Risk Factors May Include
Impaired circulation
Possibly Evidenced By
(Not applicable; presence of signs and symptoms establishes an actual diagnosis)
Desired Outcomes/Evaluation Criteria—Client Will
Tissue Perfusion: Peripheral
Maintain skin integrity.
Demonstrate behaviors or techniques to prevent skin breakdown.
NURSING DIAGNOSIS: ineffective Self-Health Management
May Be Related To
Complexity of therapeutic regimen
Perceived seriousness/susceptibility
Deficient knowledge
Economic difficulties
Possibly Evidenced By
Reports difficulty with prescribed regimen
Failure to include treatment regimen in daily living
Failure to take action to reduce risk factors
Unexpected acceleration of illness symptoms
Desired Outcomes/Evaluation Criteria—Client Will
Self-Management: Heart Failure
Identify relationship of ongoing therapies (treatment program) to reduction of recurrent episodes and prevention of
complications.
List signs and symptoms that require immediate intervention.
Identify own stress and risk factors and some techniques for handling them.
Initiate necessary lifestyle and behavioral changes.
You might also like
- Guide For Writing NotesDocument10 pagesGuide For Writing Notesiamsera100% (1)
- Normal Lab ValuesDocument54 pagesNormal Lab ValuesShreyas Walvekar100% (3)
- Nursing Management of Patient With Disorders of Ent Third YrDocument26 pagesNursing Management of Patient With Disorders of Ent Third YrShreyas Walvekar100% (3)
- Maternal Health: Ekta Modi 2 MPT in RehabDocument368 pagesMaternal Health: Ekta Modi 2 MPT in RehabMihir_Mehta_5497100% (1)
- Dark Souls 5eDocument17 pagesDark Souls 5ebite_clown_437074191No ratings yet
- Bats MagicDocument5 pagesBats MagicANDROMEDA1974No ratings yet
- Neonatal Sepsis: CausesDocument3 pagesNeonatal Sepsis: CausesGeraldine BirowaNo ratings yet
- Chapter 3 Client PresentationDocument4 pagesChapter 3 Client PresentationEllePeiNo ratings yet
- FULL Download Ebook PDF Fundamentals of Human Neuropsychology 7th Edition PDF EbookDocument41 pagesFULL Download Ebook PDF Fundamentals of Human Neuropsychology 7th Edition PDF Ebookjennifer.lawver532100% (44)
- Intravenous FluidsDocument2 pagesIntravenous FluidsShreyas WalvekarNo ratings yet
- Management of Tuberculosis: A guide for clinicians (eBook edition)From EverandManagement of Tuberculosis: A guide for clinicians (eBook edition)No ratings yet
- Medical EnglishDocument133 pagesMedical EnglishKristina TomakNo ratings yet
- ABCDs During A Code Blue Response in An Adult PatientDocument23 pagesABCDs During A Code Blue Response in An Adult PatientChakra PuspitaNo ratings yet
- Form 7 Mental Capacity AssessmentDocument3 pagesForm 7 Mental Capacity Assessmenttexasranger770No ratings yet
- Problem-based Approach to Gastroenterology and HepatologyFrom EverandProblem-based Approach to Gastroenterology and HepatologyJohn N. PlevrisNo ratings yet
- Cancer of LarynxDocument3 pagesCancer of LarynxShreyas WalvekarNo ratings yet
- Bowel ObstructionDocument6 pagesBowel ObstructionKryza Dale Bunado BaticanNo ratings yet
- Teacher Preparation Seminar 11Document33 pagesTeacher Preparation Seminar 11Shreyas Walvekar60% (5)
- Viral Exanthem (Main)Document94 pagesViral Exanthem (Main)Starlet Rhonadez Bito-onon OrielNo ratings yet
- Timed Up and Go Test RalanDocument1 pageTimed Up and Go Test RalanBagus Andi PramonoNo ratings yet
- Trauma Team UMDocument13 pagesTrauma Team UMMohamad Hasnol HayatNo ratings yet
- Chronic Kidney DiseaseDocument7 pagesChronic Kidney DiseaseLardel Balbiran LafortezaNo ratings yet
- Choking: by Jawad AhmedDocument25 pagesChoking: by Jawad Ahmedjawad_ahmedNo ratings yet
- Kode Penjelasan Keterangan: ObgynDocument14 pagesKode Penjelasan Keterangan: Obgynanon_507132438No ratings yet
- NCP Poststreptococcal GlomerulonephritisDocument12 pagesNCP Poststreptococcal GlomerulonephritisScarlet ScarletNo ratings yet
- Typhoid FeverDocument38 pagesTyphoid FeverRonelenePurisimaNo ratings yet
- Case Presentation On LrtiDocument17 pagesCase Presentation On LrtiNewtan DebNo ratings yet
- Exudative Pleural Effusions - UpToDateDocument2 pagesExudative Pleural Effusions - UpToDateAsif IqbalNo ratings yet
- Toaz - Info Case Study Pneumonia PRDocument41 pagesToaz - Info Case Study Pneumonia PRTrixNo ratings yet
- Grand Case DengueDocument14 pagesGrand Case DengueShell BalangueNo ratings yet
- Pathological Changes of DM - 2023Document53 pagesPathological Changes of DM - 2023Visura PrabodNo ratings yet
- Health Teachings On CHFDocument6 pagesHealth Teachings On CHFfLOR_ZIANE_MAENo ratings yet
- IM Clinics History 2Document4 pagesIM Clinics History 2LucyellowOttemoesoeNo ratings yet
- Guada A. Dumapit RN, ManDocument18 pagesGuada A. Dumapit RN, ManAnne B. BuenvenidaNo ratings yet
- Community-Acquired Pneumonia: Bello, Mickaela Bianca A. Gumiran, NomerDocument37 pagesCommunity-Acquired Pneumonia: Bello, Mickaela Bianca A. Gumiran, NomerKristine-Joy Legaspi FrancoNo ratings yet
- HISTORY TAKING - FINAL - Sumanyu258@gmail - Com - 01092014 PDFDocument111 pagesHISTORY TAKING - FINAL - Sumanyu258@gmail - Com - 01092014 PDFRashmi RanjanNo ratings yet
- Case Presentation OF Acute Tonsillitis: Nueva Ecija University of Science andDocument38 pagesCase Presentation OF Acute Tonsillitis: Nueva Ecija University of Science andBeverly DatuNo ratings yet
- CarePlan Clinical Log Summary1Document4 pagesCarePlan Clinical Log Summary1Cherie L. MilburnNo ratings yet
- COPD Case Presentation 1Document19 pagesCOPD Case Presentation 1Praveena Mogan100% (1)
- Management of Asthma ExacerbationDocument13 pagesManagement of Asthma ExacerbationAini Shofa HaniahNo ratings yet
- Background: Viral Mumps InfectionDocument5 pagesBackground: Viral Mumps InfectionAgustin UyNo ratings yet
- Case StudyNursing AssessmentDocument7 pagesCase StudyNursing AssessmentArindomNo ratings yet
- Tuberculosis: Dr.V. Gangadharan Professor & Hod Department of Respiratory Medicine Saveetha Medical College HospitalDocument58 pagesTuberculosis: Dr.V. Gangadharan Professor & Hod Department of Respiratory Medicine Saveetha Medical College HospitalJoanna RachelNo ratings yet
- Drug StudyDocument9 pagesDrug StudyShiara Ruth EdrosoloNo ratings yet
- NursingCare PlanDocument8 pagesNursingCare PlanSunSearra Kennedy RuffinNo ratings yet
- Dengue Fever Case StudyDocument5 pagesDengue Fever Case StudyNadine PollescasNo ratings yet
- Dengue Breakbone Fever Case StudyDocument53 pagesDengue Breakbone Fever Case StudyLeilani Rodriguez AmpoNo ratings yet
- Nursing Education Department: Patient AssessmentDocument34 pagesNursing Education Department: Patient AssessmentSitti Mardiya SariolNo ratings yet
- Coughs and Colds Nurse Management of Upper Respiratory Tract InfectionDocument3 pagesCoughs and Colds Nurse Management of Upper Respiratory Tract InfectionMichael Anthony ErmitaNo ratings yet
- Case AppendicitisDocument30 pagesCase AppendicitisSarahNo ratings yet
- Case Presentation - GASTRODocument46 pagesCase Presentation - GASTROalidudeNo ratings yet
- Article On DengueDocument6 pagesArticle On Dengueاحمد احمدNo ratings yet
- Chest Pain.Document53 pagesChest Pain.Shimmering MoonNo ratings yet
- PnuemoniaDocument102 pagesPnuemoniaRegineCuasSulibNo ratings yet
- Case Presentation: Patient Chart - Mary JohnsonDocument12 pagesCase Presentation: Patient Chart - Mary Johnsonivoneeh_16100% (1)
- Case Presentation Laryngitis TB 70 TahunDocument21 pagesCase Presentation Laryngitis TB 70 TahunMegan Shanzu100% (1)
- Nursing Care Plan Case StudyDocument2 pagesNursing Care Plan Case StudyHANIM0% (1)
- Pat 2 Medsurg1Document20 pagesPat 2 Medsurg1api-300849832No ratings yet
- PNEUMONIA Case 2 PDFDocument49 pagesPNEUMONIA Case 2 PDFRed OrangeNo ratings yet
- Reye's SyndromeDocument11 pagesReye's SyndromeChristine Go100% (1)
- Nursing Case Presentation For A Patient With CABG: Subject: Medical Surgical Nursing-IIDocument10 pagesNursing Case Presentation For A Patient With CABG: Subject: Medical Surgical Nursing-IIanamika sharmaNo ratings yet
- Chronic GastritisDocument7 pagesChronic GastritisDivina AquinoNo ratings yet
- Asthma in PregnancyDocument18 pagesAsthma in Pregnancyms khan0% (1)
- Case Study On Ibd17Document2 pagesCase Study On Ibd17api-381128376No ratings yet
- Acute TonsillopharyngitisDocument39 pagesAcute TonsillopharyngitisCin AtianzarNo ratings yet
- HIV:AIDS Determinants and Control of The EpidemicDocument4 pagesHIV:AIDS Determinants and Control of The EpidemicahiNo ratings yet
- Abdominal Distension: Common Causes: - (Five F'S) 1. 2. 3. 4. 5. History of Present Illness 1Document3 pagesAbdominal Distension: Common Causes: - (Five F'S) 1. 2. 3. 4. 5. History of Present Illness 1Maxamed DananNo ratings yet
- Reflection On Blood Transfusion ErrorDocument3 pagesReflection On Blood Transfusion ErrorSana LaraibNo ratings yet
- AKI CASE NishaDocument64 pagesAKI CASE NishaSurkhali Bipana100% (1)
- MeaslesDocument32 pagesMeaslesYum C100% (2)
- Welcome To Our Presentation - Subject:Dermatology - Facilitator: Ustad Hamdi A Hussein - Title: Chickenpox - Class:019 - Group 3Document17 pagesWelcome To Our Presentation - Subject:Dermatology - Facilitator: Ustad Hamdi A Hussein - Title: Chickenpox - Class:019 - Group 3knowledge chanall chanallNo ratings yet
- Case Scenerio Nephrotic SyndromeDocument4 pagesCase Scenerio Nephrotic SyndromeEllen AngelNo ratings yet
- Addison's DiseaseDocument9 pagesAddison's Diseaseash ashNo ratings yet
- A Study of the Lack of Hiv/Aids Awareness Among African American Women: a Leadership Perspective: Awareness That All Cultures Should Know AboutFrom EverandA Study of the Lack of Hiv/Aids Awareness Among African American Women: a Leadership Perspective: Awareness That All Cultures Should Know AboutRating: 5 out of 5 stars5/5 (1)
- 1st Year Basic BSC Nursing Anatomy Word Notes in DetailsDocument2 pages1st Year Basic BSC Nursing Anatomy Word Notes in DetailsShreyas WalvekarNo ratings yet
- Nursing Management of PatientDocument30 pagesNursing Management of PatientShreyas WalvekarNo ratings yet
- Palliative Care Lecture 2022Document20 pagesPalliative Care Lecture 2022Shreyas WalvekarNo ratings yet
- Assessment of SkinDocument11 pagesAssessment of SkinShreyas WalvekarNo ratings yet
- Warfarin DietDocument4 pagesWarfarin DietShreyas Walvekar0% (1)
- Possible Nursing Diagnosis According To Needs of Cancer Bedridden PatientDocument2 pagesPossible Nursing Diagnosis According To Needs of Cancer Bedridden PatientShreyas WalvekarNo ratings yet
- ACNEDocument20 pagesACNEShreyas WalvekarNo ratings yet
- MACROLIDESDocument14 pagesMACROLIDESShreyas WalvekarNo ratings yet
- Conflict ManagementDocument22 pagesConflict ManagementShreyas Walvekar100% (1)
- Staff Nurse PVTDocument7 pagesStaff Nurse PVTShreyas WalvekarNo ratings yet
- Cancer of The UterusDocument5 pagesCancer of The UterusShreyas WalvekarNo ratings yet
- CEPHALOSPORINSDocument8 pagesCEPHALOSPORINSShreyas WalvekarNo ratings yet
- GENITO URINARY SYSTEM 2nd Year BSC NursingDocument8 pagesGENITO URINARY SYSTEM 2nd Year BSC NursingShreyas WalvekarNo ratings yet
- Yashwant Shikshan Prasarak MandalDocument1 pageYashwant Shikshan Prasarak MandalShreyas WalvekarNo ratings yet
- Unit Iv Nursing Management of Patient With Gi DisordersDocument1 pageUnit Iv Nursing Management of Patient With Gi DisordersShreyas WalvekarNo ratings yet
- First Degree Atrioventricular BlockDocument3 pagesFirst Degree Atrioventricular BlockShreyas WalvekarNo ratings yet
- Krishna Institute of Medical Science and Deemed To Be' University, Karad. Krishna Institute of Nursing SciencesDocument2 pagesKrishna Institute of Medical Science and Deemed To Be' University, Karad. Krishna Institute of Nursing SciencesShreyas WalvekarNo ratings yet
- Who Day Celebration 2018Document25 pagesWho Day Celebration 2018Shreyas WalvekarNo ratings yet
- Gold Awards: Organization Name Title of InnovationDocument10 pagesGold Awards: Organization Name Title of Innovationchek86351No ratings yet
- People vs. BonoanDocument6 pagesPeople vs. BonoannellafayericoNo ratings yet
- What Is Rheumatoid ArthritisDocument16 pagesWhat Is Rheumatoid ArthritisDurge Raj GhalanNo ratings yet
- Ob Osce.04 CTG ReadingDocument6 pagesOb Osce.04 CTG ReadingDasha VeeNo ratings yet
- Assis 2017Document19 pagesAssis 2017widyadariNo ratings yet
- Group 4 Environmental Pollution and Impacts On Public HealthDocument10 pagesGroup 4 Environmental Pollution and Impacts On Public HealthBen KuNo ratings yet
- Garcia. Act 1 and 2 NUR103Document4 pagesGarcia. Act 1 and 2 NUR103Frances Katherine GarciaNo ratings yet
- Illich 1982Document5 pagesIllich 1982CsscamposNo ratings yet
- Osteoporosis - PathophysiologyDocument2 pagesOsteoporosis - PathophysiologyMary April MendezNo ratings yet
- Maui Medical Dispensary Application Redacted Sec3Document541 pagesMaui Medical Dispensary Application Redacted Sec3melipasaNo ratings yet
- Sub - PG Dissertation Title Registration With KNR UHS, WarangalDocument7 pagesSub - PG Dissertation Title Registration With KNR UHS, WarangalPradeep VunnamNo ratings yet
- Mekong TMBO 02 Maret 2021Document14 pagesMekong TMBO 02 Maret 2021Yolanda RahayuNo ratings yet
- San Marcelino Campus San Marcelino, Zambales: Ramon Magsaysay Technological UniversityDocument33 pagesSan Marcelino Campus San Marcelino, Zambales: Ramon Magsaysay Technological UniversityKristine Grace CachoNo ratings yet
- New Microsoft Word DocumentDocument3 pagesNew Microsoft Word Documentnew one10% (1)
- NMAT Biology Practice Questions Set 1Document6 pagesNMAT Biology Practice Questions Set 1Nurshayma JalilNo ratings yet
- Lesson 10: Sexual Aspect of Self: Name: Ramil D Malapo Course: BEEDDocument15 pagesLesson 10: Sexual Aspect of Self: Name: Ramil D Malapo Course: BEEDJOANA MANAOGNo ratings yet
- Causes of Metabolic AcidosisDocument10 pagesCauses of Metabolic AcidosisKimberly Anne SP PadillaNo ratings yet
- Analytical Case Study of Bmiof Mildly Symptomatic Covid-19 Patients With Reference To MizajDocument7 pagesAnalytical Case Study of Bmiof Mildly Symptomatic Covid-19 Patients With Reference To MizajyusufNo ratings yet
- Nutrition For Pregnant WomenDocument3 pagesNutrition For Pregnant WomenKeff MundaNo ratings yet
- Euthanasia ThesisDocument11 pagesEuthanasia ThesisAyush MathurNo ratings yet